Abstract
Involvement of para-aortic nodes (PAN) has been detected at pathological examination in 10–25% of locally advanced gastric cancer. Based on these data of nodal diffusion, the lymphadenectomy of para-aortic stations would be desirable in locally advanced gastric cancer. However, the debate on the oncological benefit of para-aortic nodes dissection is still not solved. A review of the literature was performed and papers reporting either the rate of para-aortic nodal metastases or the long-term survival outcomes after D2+ para-aortic nodes dissection (PAND) or D3 lymphadenectomy were descriptively reported. The literature survey yielded 14 studies. Most of the papers show the outcome of series of advanced gastric cancer treated with surgery alone, while starting from 2012, 3 articles report the outcomes of D2 + PAND or D3 lymphadenectomy after preoperative chemotherapy. The rate of PAN metastases ranges between 8.5 and 28% in surgical series. Survival outcomes largely improved in series of patients treated with multimodal approach compared to those of surgery alone. In patients with clinically detected para-aortic nodal metastases, preoperative chemotherapy followed by PAND is indicated. More data are needed to clarify the indication to prophylactic PAND in the era of multimodal treatment, anyway super-extended lymphadenectomies have to be performed by experienced surgeons in dedicated centres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the declining incidence and the therapeutic improvements achieved in the last decades, gastric cancer (GC) is still a major cause of cancer death worldwide [1]. Therefore, further improvements in treatment through more tailored strategies are essential.
Surgery remains the cornerstone of curative intent therapy. As such, the extent of surgical resection, especially the extent of lymphadenectomy, is one of the key elements that needs to be personalized according to patients and tumours characteristics to get the best outcome for each patient by balancing post-operative complications and oncological benefits.
Involvement of para-aortic nodes (PAN) has been detected at pathological examination in 10–25% of locally advanced GCs [2, 3] when considering also the incidence of micrometastases, Natsugoe et al. reported a positivity rate up to 64% [4].
Based on the data of nodal diffusion, the lymphadenectomy of para-aortic stations would be desirable in locally advanced gastric cancer. However, the debate on the oncological benefit of para-aortic nodes dissection is still not solved. Indeed, on the other hand, para-aortic nodal involvement is considered as expression of a metastatic disease both by the 8th edition of TNM staging [5] and the 3rd Japanese Classification of gastric cancer [6], while on the other hand some authors [7], suggest considering the cases of gastric cancer harbouring metastases to the para-aortic nodes as borderline resectable rather than metastatic tumours as the long-term outcomes observed in such patients are much more better compared with other metastatic tumours [8]. In the present review, based on the available literature data, we will describe the current indications to para-aortic nodal dissection as well as the open questions on this topic.
Methods
VM searched PubMed for papers using the key words “para-aortic” AND “gastric cancer” AND “lymphadenectomy”. Only studies in English language reporting either the rate of para-aortic nodal metastases or the long-term survival outcomes after D2+ PAND or D3 lymphadenectomy were included. Results of literature review were descriptively reported.
Results
The literature survey yielded 14 studies [9] (Table 1). Most of the papers show the outcome of series of advanced gastric cancer treated with surgery alone [9], while starting from 2012, 3 articles report the outcomes of D2+ para-aortic or D3 lymphadenectomy after preoperative chemotherapy [20]. The rate of PAN metastases ranges between 8.5 and 26.1% in surgical series where no selection of patients based on tumour site was made [11]. The rate of PAN metastases was 28% in a surgical series including only upper third tumours [9]. Survival outcomes largely improved in series of patients treated with multimodal approach compared to those with surgery alone (Table 1).
Discussion
History of para-aortic nodal dissection in gastric cancer
D2 lymphadenectomy is the standard of care in Japan and South Korea since decades [23, 24], more recently also in Europe the guidelines recommend the extended D2 dissection in case of curative intent treatment of GC [25,26,27,28].
The benefit of further extending the lymphadenectomy beyond the D2 is controversial.
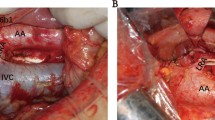
The para-aortic area is considered as the outmost nodal station before the systemic lymphatic flow. Based on this consideration and according to retrospective data reporting a high rate (10–30%) of PAN pathological involvement [29], D2+ para-aortic nodal dissection (PAND) or super-extended D3 lymphadenectomy have been routinely performed for advanced gastric cancer in Japan as well as in dedicated Western centres in the past decades.
Both Eastern and European authors reported satisfying long-term outcomes in patients with pathological positivity of PAN (pPAN+) after super-extended dissection (Table 1). Tokunaga et al. showed that in pPAN+ patients, if excluding cases with linitis plastica or with more than 15 positive lymph nodes, 5-year overall survival was 28.6% after D3 dissection [15]. Similarly, in a study of the Italian Research Group for Gastric Cancer (GIRCG), the 5-year overall survival in pPAN+ after D3 lymphadenectomy was 17% [30].
However, since the publication of the Japan Clinical Oncology Group (JCOG) 9501 trial [11], showing no survival benefit of prophylactic D2+ PAND compared to D2 lymphadenectomy alone in advanced gastric cancer, the routine PAND is no more indicated.
Of note, that trial excluded cases with clinically detected PAN metastases, leading to a lower rate of PAN metastases retrieved at pathological examination (8.5%) compared to previous studies. Nevertheless, Sasako et al. reported a not negligible 5-year overall survival rate of 18.2% in patients with PAN metastases after prophylactic PAN dissection. Moreover, that trial [11], although not finding any significant survival advantage after PAN dissection with respect to simple D2 in the whole sample, highlighted significant interactions between T or N status and extension of lymphadenectomy (p = 0.004 and p = 0.003, respectively): paradoxically, patients with less advanced cancer (subserosal and node-negative tumours) showed a significant benefit from PAN dissection.
Taken together, these considerations suggest the possibility that the D2+ PAND can offer a chance of cure in selected patients with advanced GC without clinically detectable PAN metastases [31].
All the above-mentioned evidences suggest the need of further investigations on the role of PAN dissection in advanced GC, especially if considering the increasing efficacy of chemotherapy regimens either in neo-adjuvant or in metastatic setting.
Both, the role of PAND in patients with clinically positive PAN and the role of prophylactic PAND should be reconsidered in the era of multimodal treatment.
Para-aortic nodal dissection in the era of multimodal treatment
Interesting findings arise from recent studies exploring the role of para-aortic dissection after preoperative chemotherapy [20,21,22] (Table 1). A phase II Japanese trial demonstrated that in patients with clinically detected extensive nodal metastases (bulky nodes in the D2 stations) with or without lymphadenopathy in the para-aortic (No. 16 a2–b1) regions, a multidisciplinary treatment including two courses of neo-adjuvant chemotherapy with S-1+ cisplatin followed by D2 plus PAND lead to a 5-year survival rate of 53% [21].
Specifically, in patients with clinically bulky nodes in the second-level perigastric stations without preoperative evidence of PAN metastases, the 5-year overall survival was 68%, while in patients with clinically detected PAN metastases without bulky N2 nodes, the 5-year overall survival was 57%, while in patients with both initial bulky N2 and PAN metastases the 5-year overall survival was 17%.
Interestingly, only 15 (31%) of patients included in the trial were pathologically staged as pN3, including PAN metastases: according to the clinical node status in 48 eligible patients who underwent surgery, pN3 disease was found in 5 of 24 patients with bulky N2 disease only, 4 of 14 with bulky PAN involvement alone, and 5 of 10 with both bulky N2 and PAN-positive tumours.
Of note, in that trial, peritoneal metastasis as well as the peritoneal cytology status had to be ruled out by staging laparoscopy prior to registration. The results of this Japanese trial are very relevant and confirm that in the era of multimodal treatment the role of PAN dissection is beneficial in patients with clinically detected PAN metastases after chemotherapy unless peritoneal cytology or peritoneal metastases are detected at staging laparoscopy. But also a role of “prophylactic” PAND after preoperative chemotherapy in locally advanced gastric cancer is suggested. In this case, the prophylactic PAND after chemotherapy was demonstrated highly beneficial (5-year OS 68%) in patients with bulky N2, i.e., one node ≥ 3 cm or two adjacent nodes ≥ 1.5 cm in the second-level perigastric stations. Moreover, also other patients with locally advanced gastric cancer may benefit from the prophylactic extension of lymphadenectomy to the para-aortic area. Indeed, a recent Korean study, by analysing 2618 patients who had undergone gastrectomy with D2 lymphadenectomy for gastric cancer very rarely (1.3% of cases) extended to PAN [32], reported a loco-regional relapse rate of 8.5% 5 years after surgery, this was most often seen outside the D2 dissected area (90,4%) in particular in the stations 16 a2 and 16 b1 (46 and 60%, respectively). These findings further support the hypothesis that some subgroups of patients with advanced gastric cancer have PAN micrometastases or metastases that are not detectable trough the current available preoperative imaging examinations. It could be hypothesized that prophylactic PAND would prevent loco-regional relapse in these patients, especially if there is a good clinical response to preoperative chemotherapy.
How to select patients for prophylactic PAND in the era of multimodal treatment?
Based on the consideration that patients with clinically detectable PAN metastases treated with preoperative chemotherapy followed by PAND have a good prognosis [21], the same treatment option should not be denied to those patients who have clinically negative but pathological positive PAN. Indeed, even if a good accuracy of CT scan has been reported both by Eastern and Western authors [33, 34] in some cases of locally advanced gastric cancer with diffuse histotype, pathological nodal metastases were found also in clinically negative cases. Moreover, as stated above, the possible role of PAND on preventing cancer relapse by blocking lymphatic channels from the stomach or removing PAN micrometastases, is basically unknown.
Of course, the problem is how to identify the patients with locally advanced gastric cancer at high risk of PAN metastases [18] that may benefit from PAND.
Interestingly, in a previous study by our group, by analysing a series of patients with advanced gastric cancer including those with PAN metastases, we found that the rate of loco-regional relapse was comparable after D2 or D3 lymphadenectomy (16.4% vs. 17%) in the whole series. However, we found a significantly higher risk of locoregional recurrence in the diffuse histotype after D2 compared with D3 [16]. It is likely that a more extended lymphadenectomy had played a better local control of those tumours that have a higher lymphotropism, and both patients with clinical positive PAN and those with pathological positive, but clinical negative PAN or with PAN micrometastasis could have benefit from D3.
Considering the high proportion of Laurèn diffuse type especially of signet ring cell tumours that is currently observed in the West [35], the benefit of prophylactic PAND need to be evaluated through a dedicated trial comparing D2 versus D2+ PAND or D3 in tumours with Laurèn diffuse/WHO poorly cohesive and SRC tumours after neo-adjuvant chemotherapy.
Of course, the possible oncological benefit of super-extended lymphadenectomy should be balanced with the risk of post-operative complications and mortality. Therefore, super-extended lymphadenectomies should be performed in dedicated high-volume hospitals.
Conclusion
In patients with clinically detected para-aortic nodal metastases, preoperative chemotherapy followed by PAND is indicated. Prophylactic PAND after neo-adjuvant treatment could also be of benefit in some subgroups of locally advanced gastric cancer at high risk of PAN metastases such as cases with bulky nodes in the second level perigastric nodal stations or with Laurèn diffuse/WHO poorly cohesive and SRC tumours. More data are needed to clarify the indication TP prophylactic PAND, anyway super-extended lymphadenectomies have to be performed by experienced surgeons in dedicated centres.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386
Kunisaki C, Shimada H, Yamaoka H et al (1999) Significance of para-aortic lymph node dissection in advanced gastric cancer. Hepatogastroenterology 46:2635–2642
Liang H, Deng J (2016) Evaluation of rational extent lymphadenectomy for local advanced gastric cancer. Chin J Cancer Res. 28(4):397–403
Natsugoe S, Nakashima S, Matsumoto M et al (1999) Paraaortic lymph node micrometastasis and tumor cell microinvolvement in advanced gastric carcinoma. Gastric Cancer 2:179–185
Amin MBES, Greene F et al (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Association Japanese Gastric Cancer (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Kodera Y, Kobayashi D, Tanaka C, Fujiwara M (2014) Gastric adenocarcinoma with para-aortic lymph node metastasis: a borderline resectable cancer? Surg Today 45:1082–1090
Park IH, Kim SY, Kim YW et al (2011) Clinical characteristics and treatment outcomes of gastric cancer patients with isolated para-aortic lymph node involvement. Cancer Chemother Pharmacol 67(1):127–136
Baba M, Hokita S, Natsugoe S, Miyazono T, Shimada M, Nakano S et al (2000) Paraaortic lymphadenectomy in patients with advanced carcinoma of the upper-third of the stomach. Hepatogastroenterology 47:893–896
Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA et al (2006) Comparison of surgical results of D2 versus D3 gastrectomy (para-aortic lymph node dissection) for advanced gastric carcinoma. A multi-institutional study. Ann Surg Oncol. 13:659–667
Sasako M, Sano T, Yamamoto S et al (2008) D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med 359:453–462
Yonemura Y, Wu CC, Fukushima N et al (2008) Randomized clinical trial of D2 and extended paraaortic lymph- adenectomy in patients with gastric cancer. Int J Clin Oncol 13:132–137
Fujimura T, Nakamura K, Oyama K, Funaki H, Fujita H, Kinami S, Ninomiya I, Fushida S, Nishimura G, Kayahara M, Ohta T (2009) Selective lymphadenectomy of para-aortic lymph nodes for advanced gastric cancer. Oncol Rep 22(3):509–514
Roviello F, Pedrazzani C, Marrelli D et al (2010) Super-extended (D3) lymphadenectomy in advanced gastric cancer. Eur J Surg Oncol 36(5):439–446
Tokunaga M, Ohyama S, Hiki N, Fukunaga T, Aikou S, Yamaguchi T (2010) Can superextended lymph node dissection be justified for gastric cancer with pathologically positive para-aortic lymph nodes? Ann Surg Oncol 17(8):2031–2036
de Manzoni G, Verlato G, Bencivenga M et al (2015) Impact of super- extended lymphadenectomy on relapse in advanced gastric cancer. Eur J Surg Oncol 41(4):534–540
Morita S, Fukagawa T, Fujiwara H, Katai H (2016) The clinical significance of para-aortic nodal dissection for advanced gastric cancer. Eur J Surg Oncol 42(9):1448–1454
Marrelli D, Ferrara F, Giacopuzzi S, Morgagni P, Di Leo A, De Franco L, Pedrazzani C, Saragoni L, De Manzoni G, Roviello F (2017) Incidence and prognostic value of metastases to “Posterior” and para-aortic lymph nodes in resectable gastric cancer. Ann Surg Oncol 24(8):2273–2280
Kumagai K, Sano T, Hiki N, Nunobe S, Tsujiura M, Ida S, Ohashi M, Yamaguchi T (2017) Survival benefit of ‘‘D2-plus’’ gastrectomy in gastric cancer patients with duodenal invasion. Gastric Cancer. https://doi.org/10.1007/s10120-017-0733-6
Oyama K, Fushida S, Kinoshita J, Makino I, Nakamura K, Hayashi H et al (2012) Efficacy of pre-operative chemotherapy with docetaxel, cisplatin, and S-1 (DCS therapy) and curative resection for gastric cancer with pathologically positive para-aortic lymph nodes. J Surg Oncol 105:535–541
Tsuburaya A, Mizusawa J, Tanaka Y, Fukushima N, Nashimoto A, Sasako M, Stomach Cancer Study Group of the Japan Clinical Oncology Group (2014) Neoadjuvant chemotherapy with S-1 and cisplatin followed by D2 gastrectomy with para-aortic lymph node dissection for gastric cancer with extensive lymph node metastasis. Br J Surg 101(6):653–660
Fujiwara Y, Omori T, Demura K, Miyata H, Sugimura K, Ohue M, Kobayashi S, Takahashi H, Doki Y, Yano M (2015) A multidisciplinary approach for advanced gastric cancer with paraaortic lymph node metastasis. Anticancer Res 35(12):6739–6745
Kajitani T (1981) The general rules for the gastric cancer study in surgery and pathology. Part I. Clinical classification. Jpn J Surg 11:127–139
Lee JH, Kim JG, Jung HK, Kim JH, Jeong WK, Jeon TJ, Kim JM, Kim YI, Ryu KW, Kong SH, Kim HI, Jung HY, Kim YS, Zang DY, Cho JY, Park JO, Lim DH, Jung ES, Ahn HS, Kim HJ (2014) Clinical practice guidelines for gastric cancer in Korea: an evidence-based approach. J Gastric Cancer 14(2):87–104
Allum WH, Blazeby JM, Griffin SM, Cunningham D, Jankowski JA, Wong R, Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, the British Society of Gastroenterology and the British Association of Surgical Oncology (2011) Guidelines for the management of oesophageal and gastric cancer. Gut 60:1449–1472
Roviello F, Marrelli D, Morgagni P, de Manzoni G, Di Leo A, Vindigni C, Saragoni L, Tomezzoli A, Kurihara H (2002) Survival benefit of extended D2 lymphadenectomy in gastric cancer with involvement of second level lymph nodes: a longitudinal multicenter study. Ann Surg Oncol 9:894–900
Meyer HJ, Hölscher AH, Lordick F, Messmann H, Mönig S, Schumacher C, Stahl M, Wilke H, Möhler M (2012) Current S3 guidelines on surgical treatment of gastric carcinoma. Chirurg 83:31–37
Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D (2013) Gastric cancer: ESMO-ESSO-ESTRO Clinical 55 Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl. 6):57–63
Verlato G, Giacopuzzi S, Bencivenga M, Morgagni P, De Manzoni G (2014) Problems faced by evidence-based medicine in evaluating lymphadenectomy for gastric cancer. World J Gastroenterol 20(36):12883–12891
De Manzoni G, Baiocchi GL, Framarini M et al (2014) The SIC-GIRCG 2013 Consensus Conference on gastric cancer. Updates Surg 66(1):1–6
Zhang C, He Y, Schwarz RE et al (2014) Evaluation of para- aortic nodal dissection for locoregionally advanced gastric cancer with 1–3 involved para-aortic nodes. Chin Med J (Engl) 127:435–441
Chang JS, Kim KH, Yoon HI, Hyung WJ, Rha SY, Kim HS, Lee YC, Lim JS, Noh SH, Koom WS (2017) Locoregional relapse after gastrectomy with D2 lymphadenectomy for gastric cancer. Br J Surg 104(7):877–884
Marrelli D, Mazzei MA, Pedrazzani C, Di Martino M, Vindigni C, Corso G, Morelli E, Volterrani L, Roviello F (2011) High accuracy of multislices computed tomography (MSCT) for para-aortic lymph node metastases from gastric cancer: a prospective single-center study. Ann Surg Oncol 18(8):2265–2272
Lee JH, Paik YH, Lee JS, Song HJ, Ryu KW, Kim CG et al (2006) Candidates for curative resection in advanced gastric cancer patients who had equivocal para-aortic lymph node metastasis on computed tomographic scan. Ann Surg Oncol 13:1163–1167
Henson DE, Dittus C, Younes M et al (2004) Differential trends in the intestinal and diffuse types of gastric carcinoma in the United States, 1973–2000: increase in the signet ring cell type. Arch Pathol Lab Med 128:765–770
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
The research does not involve Human Participants and/or Animals.
Informed consent
There was no need to get informed consent.
Additional information
The article is part of topical collection on Gastric Cancer Surgery.
Rights and permissions
About this article
Cite this article
Mengardo, V., Bencivenga, M., Weindelmayer, J. et al. Para-aortic lymphadenectomy in surgery for gastric cancer: current indications and future perspectives. Updates Surg 70, 207–211 (2018). https://doi.org/10.1007/s13304-018-0549-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0549-x