Abstract
Treatment options to gastric cancer (GC) have been changing in recent years from a standard to a tailored approach. Different individualized procedures can range from endoscopic resection, D2 with open or minimally invasive approach, to neo-adjuvant therapy followed by extended surgery. In more advanced stages, a combined approach with the inclusion of intraperitoneal chemo-hyperthermia (HIPEC) may represent a new advanced option. The inclusion of histological type according to Laurén classification in the flowchart of treatment could increase both accuracy and effectiveness of such tailored approach. New molecular classifications of GC have been introduced recently and translational clinical studies are ongoing. These classifications are expected to be included in multidisciplinary treatment of GC. In particular, in the group with microsatellite instability a less extended lymphadenectomy may be proposed. Also tailored neo-adjuvant treatment may be proposed according to molecular classifications. The group of patients with epithelial-to-mesenchymal transition shows very high propensity to peritoneal dissemination, as well as N-metastases, and may benefit from prophylactic HIPEC and extended lymphadenectomy when confirmed in prospective trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC), despite the general decreasing incidence, is still one of the main causes of death for cancer worldwide [1, 2]. Radical surgery is still the main therapeutic option, and the extent of lymphadenectomy is an index of surgical quality and a crucial step to increase the chance of cure, above all in advanced forms (T2 and over) [3,4,5,6]. D2 lymphadenectomy is now considered the standard treatment in most therapeutic guidelines for GC all over the world [3,4,5,6].
A more extended dissection (D2plus) has been also proposed in some selected cases to further improve prognosis [7,8,9,10,11,12].
However, advanced stages of GC are still associated with poor survival expectance despite an aggressive surgery; cases with serosal infiltration and/or extensive lymph nodal spread poorly respond to surgical treatment only [13,14,15].
As such, new therapeutic options, in addition to surgery, have been proposed, in order to increase the chance of cure in such cases. Neo-adjuvant treatments, as demonstrated in recent randomized trials, are of particular importance in this way, and have been now adopted in most guidelines as part of standard treatment of locally advanced, resectable GC [16,17,18].
Advanced multimodality treatments, as intraperitoneal chemohyperthermia (HIPEC) are also under study, in order to prevent peritoneal recurrence of the tumor, which now represents the main cause of failure of GC treatment in the West [19, 20].
All these procedures are now part of the modern multimodality approach to GC, which has the target to tailor the most potentially effective treatment to tumor- and patient-related characteristics [1]. Tailored treatment, which is now considered the most modern and advanced approach for several diseases, is particularly important for GC, because for such neoplasm therapeutic options could range from minimally invasive procedures (such as endoscopic resections) to very extended and aggressive therapies (combined resections, HIPEC) [1].
To date, tumor stage is the main factor considered in the selection process to properly address the appropriate therapeutic option. However, the histological type of GC could also play an important role in this field. Recently, novel molecular classifications of GC have been introduced, and an extensive and flourishing research is now ongoing, in order to find clinical applications to these important findings [21, 22].
The aim of this review is to summarize the clinical relevance of the histological and molecular characteristics of GC, with special reference to their potential utility in the selection process to tailor the multimodal therapeutic options to different cases of GC.
Clinical features of different histotypes of gastric cancer and their impact on multimodality treatment
According to Laurén classification, gastric cancer (GC) can be divided in three histological types: intestinal (IT), diffuse (DT) and mixed (MT). Besides histomorphometrical characteristics, IT and DT histotypes show evident differences in their epidemiological, clinical and molecular features [23]. The IT, in its pathogenesis, usually follows the sequence chronic atrophic gastritis, intestinal metaplasia, and dysplasia. It is more common in males and older patients and is generally linked to environmental factors. On the contrary, the DT usually affects younger females, and is more related to genetic factors.
The different pathogenesis is probably at the basis of the divergent epidemiological trend of IT and DT Lauren histotypes. It has been reported that the declining incidence of GC is due to the decreasing number of IT located in the distal stomach, in consequence of the changed methods of food preservation and the decreased prevalence of Helicobacter pylori infection. On the contrary, the incidence of DT and also of IT of the proximal stomach, which has a different pathogenesis than distal IT, are generally stable [24,25,26]. As a consequence of this different trend, the DT neoplasms show a relative increase with time.
In addition, also the proportion of signet ring cell gastric cancer has been reported to be increasing in recent years [26], particularly in younger patient population [27].
These epidemiological trends are related to potential clinical implications. It is well known that proximal tumors, including those involving the esophago-gastric junction (EGJ), are associated with greater clinical aggressiveness and poor prognosis [28,29,30,31].
Regarding the histological types, it is recognized that the risk of lymph node metastases is notably higher in the DT, compared with IT, at the same pT stage. This regards both early forms than advanced types of GC [32]; DT is associated with higher general incidence node-positive cases, and also overall number of involved nodes [1]. Furthermore, the DT is also a strong risk factor for lymph node metastases in extra-regional nodal stations, with special reference to para-aortic nodes, but a recent report from the Italian Research Group for Gastric Cancer (GIRCG) group indicates that even subgroups of IT tumors have a propensity to spread to “posterior” node stations (8p, 12b/p, 13) [12, 33, 34]. According to these characteristics of nodal spread, indications to super-extended lymphadenectomy may differ according to histotype. A recent retrospective study of the GIRCG group indicate that a potential survival benefit, with a reduction in the rate of locoregional recurrence after surgery, may be obtained with super-extended para-aortic lymphadenectomy in the diffuse-mixed types of GC, when compared with a D2 procedure [35]. In our opinion, histotype of GC may have a role, in addition to other factors such as tumor stage, tumor location and patient’s general conditions, in tailoring the extent of lymphadenectomy for GC.
The higher risk of nodal metastases may also influence the indications to neo-adjuvant chemotherapy according to histotype of GC. Indeed, current indications to neo-adjuvant chemotherapy for non-cardia GC, according to the GIRCG guidelines, are: T3 and/or N positive clinical stage, and patients fit for chemotherapy [6]. However, clinical staging of nodal metastases of GC is still challenging, because, despite the increasing accuracy of CT scan, and different criteria of clinical node positivity are used from different groups. It has been reported that in the DT the size of involved nodes may be smaller than the commonly used cut-off values [33]. As such, indications to neo-adjuvant treatment may be probably more extensive in the DT, due to the higher risk of node-positivity even in cases with clinically favorable tumor stages.
Besides the lymph node involvement, another clinical characteristic of DT tumors is the propensity to peritoneal spread. A much higher risk of peritoneal recurrence after potentially curative surgery has been reported in diffuse/mixed histotypes, above when the serosa is involved [23, 36]. The extent of lymphadenectomy seems to have no role in reducing such risk of recurrence [37, 38]. A late evolution of the DT of the stomach is the “linitis plastica”, a diffuse infiltration, thickening and stiffening of the gastric wall with reactive fibrosis, with a notable propensity to massive lymph node metastasis and peritoneal spread, which make the rate of radical resection very low and the prognosis generally very poor even after surgical resection [39].
The chance of cure in patients with peritoneal recurrence of GC is very low, as demonstrated in several cohort studies. As such, prevention of peritoneal recurrence, more than treatment after its occurrence, may be the only potential chance of cure in high-risk cases [40]. The most important factors associated with the risk of peritoneal recurrence of GC are: positive peritoneal cytology (cy+), serosal involvement and diffuse histotype. Patients with these characteristics associated with primary tumor may potentially benefit from prophylactic HIPEC [20].
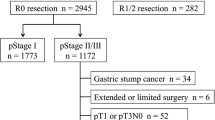
In summary, the current proposed model of multimodality approach to resectable non-cardia GC may be integrated with histological type according to Lauren. In particular, diffuse-mixed types, cT3/N+ and over should be treated by neo-adjuvant chemotherapy (NAC) followed by super-extended lymphadenectomy. In addition, serosally exposed tumors of diffuse-mixed type, as well as cT4b and cy+ may be treated by NAC, super-extended lymphadenectomy and HIPEC (Fig. 1).
New molecular classifications of GC
In the last few years, many new GC classifications were proposed. They are based on anatomical side, histopathology, gene expression, gene amplification, DNA methylation, numerous cancer-relevant aberrations and also on the oncogenic pathways [21, 22, 41,42,43,44,45,46,47].
Last few years gave us a better understanding of GC by proposing two independent molecular classifications by TCGA and Asian Cancer Research Group (ACRG) [21, 22]. Both of these classifications showed a simple 4 groups division of GC opening new possibilities to treat the disease in a tailored way. The TCGA classification presents four groups: Epstein–Barr virus (EBV), microsatellite instability (MSI), chromosomal instability (CIN) and genomically stable (GS) [21]. The ACRG divided the GC into MSI and microsatellite stable (MSS) types. Then secondary the MSS was divided into epithelial–mesenchymal transition (EMT), TP53+ and TP53− groups [22].
The MSI represents the group with elevated mutations rate, with Gastric-CIMP, MLH1 silencing, and mitotic pathways. The EBV group represents a group with a high rate of PIK3CA mutation, PD_L1/2 overexpression what is especially important in the light of new research targeting successfully that part of immunologic therapy. Additionally, in this group, we have EBV-CIMP, CDKN2A silencing, and immune cell signaling. The group represented by CIN has in majority intestinal histology, TP53 mutation and RTK-RAS activation. The last group GS tumors in majority presents diffuse histology and also CDH1, RHOA mutation, CLDN18-ARHGAP fusion and elevated expression o cell adhesion pathways.
The ACRG groups also are described by specific molecular characterization [22]. The MSI subtype represents hypermutations of such genes as KRAS, PI3K–PTEN–mTOR pathway, ALK, and ARID1A. They also found that the subtype of PIK3CA mutation of H1047R is common in MSI and the other subtypes of that mutation namely E542K and E545K are common in MSS tumors. The EMT is a group that presents a very little number of mutations. The MSS/TP53− presents a widespread TP53 mutation, and MSS/TP53+ shows a high rate of APC, ARID1A, KRAS, PIK3CA and SMAD4 mutations.
Clinical impact of molecular classifications of GC
Following the introduction of molecular classifications, great research efforts have been conducting, in order to clarify their potential impact in clinical decision-making and treatment of GC. This is particularly true for ACRG classification, because in such study some clinically relevant features were attributed to molecular subgroups [22]. Distinct groups, indeed, showed peculiar clinical–pathological characteristics (such as age, tumor location, invasion and stage). Importantly, different prognosis was attributed to the four groups, with MSI showing the best survival rate, and EMT the worse prognosis. The following are the most important molecular subgroups according to these classifications, and their main clinical characteristics identified or suggested to date.
MSI group (TGCA and ACRG classifications)
The subgroup of GC with microsatellite instability is probably the better studied to date. It is present in both TGCA and ACRG classifications, and was previously extensively investigated and results reported in several papers, although with heterogeneous and somewhat conflicting results [48]. These were mainly due to different characteristics of patient populations and various tests used for the assessment of MSI status. A recent meta-analysis was performed by our group in 48 studies with a total of 18.612 patients [48]. In mean, the MSI group accounts for about 9% of the total cases (but in some series it overcomes 20%). The pooled analysis indicated that women had a significantly increased risk of MSI compared with men, and the mean age of patients with MSI was 66 years vs. 60 years for MSS group. Most of MSI tumors were of the intestinal type according to Lauren, and were located in the distal stomach. Importantly, the risk of nodal metastases was lower than MSS cases (OR 0.70, 95 per cent c.i. 0.57–0.86), and also tumor stage was less advanced. It was also confirmed that overall survival was better for patients with MSI gastric cancer (HR 0.69, 95 per cent c.i. 0.56–0.86, p < 0.001). These results confirmed previous investigations from our group. In a recent paper including 472 patients, cancer-related 5-year survival was significantly higher in MSI-H versus MSS group (67.6% vs. 35%), and this prognostic impact was confirmed by multivariate Cox regression analysis [49]. However, the stratified analysis revealed a significant impact of MSI on prognosis in non-cardia tumors of intestinal type or tubular/poorly differentiated histology. No prognostic value of MSI in the diffuse-mixed type and signet ring cell/mucinous histotypes was observed. Other studies from our group were conducted matching MSI status and age in GC patients. In a recent large series, we observed a linear correlation between advanced age and the rate of MSI; indeed, the percentage of MSI increases gradually with increasing age, accounting for 48% of patients over the age of 85 years [50]. Furthermore, the prognostic effect of MSI status was more evident in elderly compared to younger patients. The highest difference in survival was seen between MSI and MSS groups of patients older than 65 years, while no statistical difference was seen for younger groups, and multivariate analysis confirmed MSI status has a significant factor in patients aged over 70 years (HR 1.82, P = 0.013) [50]. These findings confirm that MSI may act as a significant predictor of better prognosis above all in the elderly.
In a recent study, a detailed analysis of lymph nodal spread in MSI vs. MSS GC was performed in a total of 361 patients [51]. All patients were submitted to an extended (D2) or super-extended (D2plus) lymphadenectomy; the different lymph node stations were divided and classified according to the Japanese Society for Gastric Cancer (JGCA) criteria, and single nodes retrieved in the fresh specimen. The MSI tumors showed: a lower rate of lymph node metastases (46% vs. 70% of MSS group), a lower median number of involved nodes (1 vs. 5), a lower number of involved node stations, and a lower propensity to spread to second and third compartment nodes. Furthermore, no skip metastases were observed in MSI group. These data, when validated in other experiences and in preoperative endoscopic biopsies, could be useful in tailoring lymphadenectomy for GC, allowing a less extended dissection in MSI tumors, above all when facing with high-risk patients with relevant co-morbidities [51].
Finally, an interesting recent paper reported a post hoc analysis of patients included in the MAGIC trial; patients were treated with surgery alone or perioperative chemotherapy plus surgery for operable gastroesophageal cancer, and the association between MSI status and long-term survival was investigated [52]. Results revealed that MSI status was associated with a positive prognostic effect in patients treated with surgery alone, whereas in patients treated with neo-adjuvant chemotherapy the prognostic effect was negative. If confirmed, these results could change indications to NAC in the subgroup of patients with MSI.
MSS/EMT group (ACRG classification)
The group of tumors with MSS and epithelial-to-mesenchymal transition (EMT) according to ACRG classification is also very interesting from a clinical point of view. EMT is a process where epithelial cells are transformed into cells with mesenchymal phenotypes, characterized by lost cellular polarity and adhesion and enhanced invasive and migratory properties [53]. Epithelial markers, such as E-cadherin, are repressed, and mesenchymal markers, such as vimentin and fibronectin, are up-regulated. These alterations, together with microenvironment remodeling, facilitates GC aggressiveness, invasion, migration, metastasis and chemo-resistance.
Some reports suggest that EMT phenotype correlates, in addition to the diffuse type and poorly differentiated histology, with an advanced TNM stage and poor prognosis [53,54,55]. Most information regarding clinical characteristics of this subtype of GC come from the ACRG report [22]. It accounts for about 15% of cases, and is associated with younger age (53 years in median), location in the middle third (45.6%) or the whole stomach (6.5%), diffuse histotype (80.4%) and signet ring cell histology (43.5%); more than 50% of signet ring cell cases belong to MSS/EMT group. In addition, this subgroup is associated with more advanced pT stage, lymph node metastasis, TNM stage and perineural invasion. Importantly, this group of GC showed the worse prognosis when compared with other groups, and when analyzing the pattern of relapse, 77% of MSS/EMT cases in the ACRG cohort recurred in the peritoneum (vs. less than 20% of other groups); none of the cases had liver metastases [22]. These data are indicative of a special propensity of this molecular group to spread to the peritoneum. If confirmed in further studies, this could lead to indications for prophylactic HIPEC in such patients, to attempt to prevent peritoneal recurrence after radical surgery.
Chromosomal instability (CIN) group (TGCA classification)
The CIN subtype represents about 50% of total GC cases. About 80% of cases in this group are of the intestinal type, and main location is fundus/body or EGJ/cardia [21]. This group is particularly interesting in the view of a potential targeted therapy; indeed, CIN tumors present amplification in oncogene pathways such as RTK/RAS/MAPK signaling, including HER2, BRAF, epidermal growth factor (EGFR), MET, FGFR2, RAS [56]. Further studies are necessary to elucidate the clinical implications of this group, with special reference to multimodality approach.
Genomic stability (GS) group (TGCA classification)
The molecular with GS represents about 20% of cases in the TCGA report. Most of these tumors are of diffuse histotype (about 60% of diffuse type cases are included in this group), and a peculiar characteristic is the predominance of poorly cohesive type tumors in this group. Tumors are equally distributed in the stomach portions. The main somatic genomic alterations involve CDH1, ARID1A and RHOA [56]. CDH1 mutations have been reported, also from our group, to be a significant predictor of poor prognosis after radical surgery for GC [57], and this may have clinical implications that deserve further studies.
EBV-associated group (TGCA classification)
The molecular with EBV represents about 9% of cases according to the TCGA report [21]. The molecular analysis showed that this subtype represents PD-L1/2 overexpression, PIK3CA mutation, EBV-CIMP, CDKN2A silencing and additionally immune cell signaling [21]. In the ACRG classification, EBV in the majority is presented in the MSS/TP53+ subgroup [22]. The largest international pooled analysis on 4599 gastric cancer patients by Camargo et al. proved that this group is strongly overrepresented by males [58]. Additionally, positive EBV GCs were early stage gastric cancer, cardia localization, diffuse histotype according to Laurén classification, poorer differentiation. The median survival for EBV GC was 8.5 years vs. 5.3 years for no-EBV GC (p = 0.0006). In multivariate analysis, EBV status was one of the statically significant predictors of survival. Currently, ongoing trials try to find a group of patients that will respond to the immunological therapy. Especially PD-L1/2 expression represented in this subgroup of GC is an important target for such a medication. The response to this treatment is not only limited to the presence of the antigen, but also other factors may play an important role. One of them seems to be EBV infection probably because of its immune cell signaling [59]. Prospective trials are awaited.
Conclusions
Treatment options to GC have been changing in recent years from a standard to a tailored approach. Different individualized procedures can range from endoscopic resection, D2 with open or minimally invasive approach, to neo-adjuvant therapy followed by extended surgery. In more advanced stages, a combined approach with the inclusion of HIPEC may represent a new advanced option. The inclusion of histological type in treatment flowchart could increase both accuracy and effectiveness of such tailored approach. New molecular classifications of GC are expected to be included in multidisciplinary treatment of this aggressive disease (Fig. 2), in particular when their clinical and therapeutic implications will be clarified in the near future in a flourishing scientific context of precision medicine.
Multimodal approach to non-cardia gastric cancer with introduction of histotype and molecular features to flowchart. JGCA Japanese Gastric Cancer Association, MSI Microsatellite instability, MSS Microsatellite stable, EMT Epithelial-to-mesenchymal transition, HIPEC Hyperthermic intraperitoneal chemotherapy
References
Marrelli D, Polom K, de Manzoni G, Morgagni P, Baiocchi GL, Roviello F (2015) Multimodal treatment of gastric cancer in the west: where are we going? World J Gastroenterol 21(26):7954
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917. https://doi.org/10.1002/ijc.25516
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–19
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D, ESMO Guidelines Committee (2016) Gastric cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 27(suppl 5):v38–v49
Lee JH, Kim JG, Jung HK et al (2014) Clinical practice guidelines for gastric cancer in Korea: an evidence-based approach. J Gastric Cancer 14:87–104
De Manzoni G, Marrelli D, Baiocchi GL et al (2017) The italian research group for gastric cancer (GIRCG) guidelines for gastric cancer staging and treatment: 2015. Gastric Cancer 20:20–30
Tokunaga M, Ohyama S, Hiki N, Fukunaga T, Aikou S, Yamaguchi T (2010) Can superextended lymph node dissection be justified for gastric cancer with pathologically positive para-aortic lymph nodes? Ann Surg Oncol 17:2031–2036
Roviello F, Pedrazzani C, Marrelli D, Di Leo A, Caruso S, Giacopuzzi S, Corso G, de Manzoni G (2010) Super-extended (D3) lymphadenectomy in advanced gastric cancer. Eur J Surg Oncol 36:439–446
Eom BW, Joo J, Kim YW, Park B, Park JY, Yoon HM, Lee JH, Ryu KW (2013) Is there any role of additional retropancreatic lymph node dissection on D2 gastrectomy for advanced gastric cancer? Ann Surg Oncol 20:2669–2675
Kodera Y, Kobayashi D, Tanaka C, Fujiwara M (2015) Gastric adenocarcinoma with para-aortic lymph node metastasis: a borderline resectable cancer? Surg Today 45(9):1082–1090
Morita S, Fukagawa T, Fujiwara H, Katai H (2016) The clinical significance of para-aortic nodal dissection for advanced gastric cancer. Eur J Surg Oncol 42:1448–1454
Marrelli D, Ferrara F, Giacopuzzi S, Morgagni P, Di Leo A, De Franco L, Pedrazzani C, Saragoni L, De Manzoni G, Roviello F (2017) Incidence and prognostic value of metastases to “posterior” and para-aortic lymph nodes in resectable gastric cancer. Ann Surg Oncol 24(8):2273–2280. https://doi.org/10.1245/s10434-017-5857-8
Han DS, Suh YS, Kong SH, Lee HJ, Choi Y, Aikou S, Sano T, Park BJ, Kim WH, Yang HK (2012) Nomogram predicting long-term survival after d2 gastrectomy for gastric cancer. J Clin Oncol 30:3834–3840
Marrelli D, Morgagni P, de Manzoni G, Marchet A, Baiocchi GL, Giacopuzzi S, Coniglio A, Mocellin S, Saragoni L, Roviello F, Italian Research Group for Gastric Cancer (2015) External validation of a score predictive of recurrence after radical surgery for non-cardia gastric cancer: results of a follow-up study. J Am Coll Surg 221:280–290
Marrelli D, Morgagni P, de Manzoni G, Coniglio A, Marchet A, Saragoni L, Tiberio G, Roviello F; Italian Research Group for Gastric Cancer (IRGGC) (2012) Prognostic value of the 7th AJCC/UICC TNM classification of noncardia gastric cancer: analysis of a large series from specialized Western centers. Ann Surg 255(3):486–491. https://doi.org/10.1097/SLA.0b013e3182389b1a
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR; Upper Gastrointestinal Clinical Studies Group of the National Cancer Research Institute of the United Kingdom (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358:36–46. https://doi.org/10.1056/NEJMoa073149
Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, Ducourtieux M, Bedenne L, Fabre JM, Saint-Aubert B, Genève J, Lasser P, Rougier P (2011) Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol 29:1715–1721. https://doi.org/10.1200/JCO.2010.33.0597
Al-Batran SE, Hofheinz RD, Pauligk C et al (2016) Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol 17(12):1697–1708. https://doi.org/10.1016/S1470-2045(16)30531-9
Polom K, Marano L, Roviello G, Petrioli R, Piagnerelli R, de Franco L, Marrelli D, Roviello F (2016) Evolution and emerging future of cytoreductive surgery and hyperthermic intraperitoneal chemoperfusion in gastric cancer: from treating the incurable to preventing recurrence. Int J Hyperth 32(2):173–179. https://doi.org/10.3109/02656736.2015.1111432
Glehen O, Passot G, Villeneuve L, Vaudoyer D, Bin-Dorel S, Boschetti G, Piaton E, Garofalo A (2014) GASTRICHIP: d2 resection and hyperthermic intraperitoneal chemotherapy in locally advanced gastric carcinoma: a randomized and multicenter phase III study. BMC Cancer 14:183. https://doi.org/10.1186/1471-2407-14-183
Cancer Genome Atlas Research Network (2014) Comprehensive molecular characterization of gastric adenocarcinoma. Nature 513(7517):202–209. https://doi.org/10.1038/nature13480
Cristescu R, Lee J, Nebozhyn M et al (2015) Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med 21(5):449–456. https://doi.org/10.1038/nm.3850
Marrelli D, Roviello F, de Manzoni G, Morgagni P, Di Leo A, Saragoni L, De Stefano A, Folli S, Cordiano C, Pinto E, Italian Research Group for Gastric Cancer (2002) Different patterns of recurrence in gastric cancer depending on Lauren’s histological type: longitudinal study. World J Surg 26(9):1160–1165. https://doi.org/10.1007/s00268-002-6344-2
Wu H, Rusiecki JA, Zhu K, Potter J, Devesa SS (2009) Stomach carcinoma incidence patterns in the United States by histologic type and anatomic site. Cancer Epidemiol Biomarkers Prev 18(7):1945–1952. https://doi.org/10.1158/1055-9965.EPI-09-0250
Laurén PA, Nevalainen TJ (1993) Epidemiology of intestinal and diffuse types of gastric carcinoma. A time-trend study in Finland with comparison between studies from high- and low-risk areas. Cancer 71(10):2926–2933
Henson DE, Dittus C, Younes M, Nguyen H, Albores-Saavedra J (2004) Differential trends in the intestinal and diffuse types of gastric carcinoma in the United States, 1973-2000: increase in the signet ring cell type. Arch Pathol Lab Med 128(7):765–770
Anderson WF, Camargo MC, Fraumeni JF Jr, Correa P, Rosenberg PS, Rabkin CS (2010) Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA 303(17):1723–1728. https://doi.org/10.1001/jama.2010.496
Marrelli D, Pedrazzani C, Morgagni P, de Manzoni G, Pacelli F, Coniglio A, Marchet A, Saragoni L, Giacopuzzi S, Roviello F and Italian Research Group for Gastric Cancer (2011) Changing clinical and pathological features of gastric cancer over time. Br J Surg 98(9):1273–1283. https://doi.org/10.1002/bjs.7528
Marrelli D, De Stefano A, de Manzoni G, Morgagni P, Di Leo A, Roviello F (2005) Prediction of recurrence after radical surgery for gastric cancer: a scoring system obtained from a prospective multicenter study. Ann Surg 241(2):247–255. https://doi.org/10.1097/01.sla.0000152019.14741.97
Kattan MW, Karpeh MS, Mazumdar M, Brennan MF (2003) Postoperative nomogram for disease-specific survival after an R0 resection for gastric carcinoma. J Clin Oncol 21(19):3647–3650. https://doi.org/10.1200/JCO.2003.01.240
Han DS, Suh YS, Kong SH, Lee HJ, Choi Y, Aikou S, Sano T, Park BJ, Kim WH, Yang HK (2012) Nomogram predicting long-term survival after d2 gastrectomy for gastric cancer. J Clin Oncol 30(31):3834–3840. https://doi.org/10.1200/JCO.2012.41.8343
Roviello F, Rossi S, Marrelli D, Pedrazzani C, Corso G, Vindigni C, Morgagni P, Saragoni L, de Manzoni G, Tomezzoli A. (2006) Number of lymph node metastases and its prognostic significance in early gastric cancer: a multicenter Italian study. J Surg Oncol 94:275–280; discussion 4
Marrelli D, Mazzei MA, Pedrazzani C, Di Martino M, Vindigni C, Corso G, Morelli E, Volterrani L, Roviello F (2011) High accuracy of multislices computed tomography (MSCT) for para-aortic lymph node metastases from gastric cancer: a prospective single-center study. Ann Surg Oncol 18(8):2265–2272. https://doi.org/10.1245/s10434-010-1541-y
de Manzoni G, Di Leo A, Roviello F, Marrelli D, Giacopuzzi S, Minicozzi AM, Verlato G (2011) Tumor site and perigastric nodal status are the most important predictors of para-aortic nodal involvement in advanced gastric cancer. Ann Surg Oncol 18(8):2273–2280. https://doi.org/10.1245/s10434-010-1547-5
de Manzoni G, Verlato G, Bencivenga M, Marrelli D, Di Leo A, Giacopuzzi S, Cipollari C, Roviello F (2015) Impact of super-extended lymphadenectomy on relapse in advanced gastric cancer. Eur J Surg Oncol 41(4):534–540. https://doi.org/10.1016/j.ejso.2015.01.023
Roviello F, Marrelli D, de Manzoni G, Morgagni P, Di Leo A, Saragoni L, De Stefano A; Italian Research Group for Gastric Cancer (2003) Italian research group for gastric cancer. prospective study of peritoneal recurrence after curative surgery for gastric cancer. Br J Surg 90(9):1113–1119. https://doi.org/10.1002/bjs.4164
Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, Okajima K; Japan Clinical Oncology Group (2008) D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med 359(5):453–462. https://doi.org/10.1056/NEJMoa0707035
Roviello F, Pedrazzani C, Marrelli D, Di Leo A, Caruso S, Giacopuzzi S, Corso G, de Manzoni G (2010) Super-extended (D3) lymphadenectomy in advanced gastric cancer. Eur J Surg Oncol 36(5):439–446. https://doi.org/10.1016/j.ejso.2010.03.008
Pedrazzani C, Marrelli D, Pacelli F, Di Cosmo M, Mura G, Bettarini F, Rosa F, de Manzoni G, Roviello F (2012) Gastric linitis plastica: which role for surgical resection? Gastric Cancer 15(1):56–60. https://doi.org/10.1007/s10120-011-0063-z
Roviello F, Caruso S, Neri A, Marrelli D (2013) Treatment and prevention of peritoneal carcinomatosis from gastric cancer by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: overview and rationale. Eur J Surg Oncol 39(12):1309–1316. https://doi.org/10.1016/j.ejso.2013.10.010.]
Wang G, Hu N, Yang HH, Wang L, Su H, Wang C, Clifford R, Dawsey EM, Li JM, Ding T, Han XY, Giffen C, Goldstein AM, Taylor PR, Lee MP (2013) Comparison of global gene expression of gastric cardia and noncardia cancers from a high-risk population in China. PLoS ONE 8(5):e63826
Shah MA, Khanin R, Tang L, Janjigian YY, Klimstra DS, Gerdes H, Kelsen DP (2011) Molecular classification of gastric cancer: a new paradigm. Clin Cancer Res 17(9):2693–2701
Tan IB, Ivanova T, Lim KH, Ong CW, Deng N, Lee J, Tan SH, Wu J, Lee MH, Ooi CH, Rha SY, Wong WK, Boussioutas A, Yeoh KG, So J, Yong WP. Tsuburaya A. Grabsch H, Toh HC, Rozen S, Cheong JH, Noh SH, Wan WK, Ajani JA, Lee JS, Tellez MS, Tan P. (2011) Intrinsic subtypes of gastric cancer, based on gene expression pattern, predict survival and respond differently to chemotherapy. Gastroenterology 141(2):476–485; 485.e1–11
Deng N, Goh LK, Wang H, Das K, Tao J, Tan IB, Zhang S, Lee M, Wu J, Lim KH, Lei Z, Goh G, Lim QY, Tan AL, Sin Poh DY, Riahi S, Bell S, Shi MM, Linnartz R, Zhu F, Yeoh KG, Toh HC, Yong WP, Cheong HC, Rha SY, Boussioutas A, Grabsch H, Rozen S, Tan P (2012) A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut 61(5):673–684
Zouridis H, Deng N, Ivanova T, Zhu Y, Wong B, Huang D, Wu YH, Wu Y, Tan IB, Liem N, Gopalakrishnan V, Luo Q, Wu J, Lee M, Yong WP, Goh LK, Teh BT, Rozen S, Tan P (2012) Methylation subtypes and large-scale epigenetic alterations in gastric cancer. Sci Transl Med 4(156):156ra140. https://doi.org/10.1126/scitranslmed.3004504
Wang K, Yuen ST, Xu J, Lee SP, Yan HH, Shi ST, Siu HC, Deng S, Chu KM, Law S, Chan KH, Chan AS, Tsui WY, Ho SL, Chan AK, Man JL, Foglizzo V, Ng MK, Chan AS, Ching YP, Cheng GH, Xie T, Fernandez J, Li VS, Clevers H, Rejto PA, Mao M, Leung SY (2014) Whole-genome sequencing and comprehensive molecular pro ling identify new driver mutations in gastric cancer. Nat Genet 46(6):573–582
Liu J, McCleland M, Stawiski EW, Gnad F, Mayba O, Haverty PM, Durinck S, Chen YJ, Klijn C, Jhunjhunwala S, Lawrence M, Liu H, Wan Y, Chopra V, Yaylaoglu MB, Yuan W, Ha C, Gilbert HN, Reeder J, Pau G, Stinson J, Stern HM, Manning G, Wu TD, Neve RM, de Sauvage FJ, Modrusan Z, Seshagiri S, Firestein R, Zhang Z. (2104) Integrated exome and transcriptome sequencing reveals ZAK isoform usage in gastric cancer. Nat Commun 5: 3830
Polom K, Marano L, Marrelli D, De Luca R, Roviello G, Savelli V, Tan P, Roviello F (2018) Meta-analysis of microsatellite instability in relation to clinicopathological characteristics and overall survival in gastric cancer. Br J Surg 105(3):159–167. https://doi.org/10.1002/bjs.10663
Marrelli D, Polom K, Pascale V, Vindigni C, Piagnerelli R, De Franco L, Ferrara F, Roviello G, Garosi L, Petrioli R, Roviello F (2016) Strong prognostic value of microsatellite instability in intestinal type non-cardia gastric cancer. Ann Surg Oncol 23(3):943–950. https://doi.org/10.1245/s10434-015-4931-3
Polom K, Marrelli D, Roviello G, Pascale V, Voglino C, Rho H, Marini M, Macchiarelli R, Roviello F (2017) Molecular key to understand the gastric cancer biology in elderly patients—the role of microsatellite instability. J Surg Oncol 115(3):344–350. https://doi.org/10.1002/jso.24513
Polom K, Marrelli D, Pascale V, Ferrara F, Voglino C, Marini M, Roviello F (2017) The pattern of lymph node metastases in microsatellite unstable gastric cancer. Eur J Surg Oncol 43(12):2341–2348. https://doi.org/10.1016/j.ejso.2017.09.007
Smyth EC, Wotherspoon A, Peckitt C, Gonzalez D, Hulkki-Wilson S, Eltahir Z, Fassan M, Rugge M, Valeri N, Okines A, Hewish M, Allum W, Stenning S, Nankivell M, Langley R, Cunningham D (2017) Mismatch repair deficiency, microsatellite instability, and survival: an exploratory analysis of the medical research council adjuvant gastric infusional chemotherapy (MAGIC) trial. JAMA Oncol 3(9):1197–1203. https://doi.org/10.1001/jamaoncol.2016.6762
Huang L, Wu RL, Xu AM (2015) Epithelial-mesenchymal transition in gastric cancer. Am J Transl Res 7(11):2141–2158
Zheng HX, Cai YD, Wang YD, Cui XB, Xie TT, Li WJ, Peng L, Zhang Y, Wang ZQ, Wang J, Jiang B (2013) Fas signaling promotes motility and metastasis through epithelial-mesenchymal transition in gastrointestinal cancer. Oncogene 32(9):1183–1192. https://doi.org/10.1038/onc.2012.126
Okubo K, Uenosono Y, Arigami T, Yanagita S, Matsushita D, Kijima T, Amatatsu M, Uchikado Y, Kijima Y, Maemura K, Natsugoe S (2017) Clinical significance of altering epithelial-mesenchymal transition in metastatic lymph nodes of gastric cancer. Gastric Cancer 20(5):802–810. https://doi.org/10.1007/s10120-017-0705-x
Garattini SK, Basile D, Cattaneo M, Fanotto V, Ongaro E, Bonotto M, Negri FV, Berenato R, Ermacora P, Cardellino GG, Giovannoni M, Pella N, Scartozzi M, Antonuzzo L, Silvestris N, Fasola G, Aprile G (2017) Molecular classifications of gastric cancers: novel insights and possible future applications. World J Gastrointest Oncol 9(5):194–208. https://doi.org/10.4251/wjgo.v9.i5.194
Corso G, Carvalho J, Marrelli D, Vindigni C, Carvalho B, Seruca R, Roviello F, Oliveira C (2013) Somatic mutations and deletions of the E-cadherin gene predict poor survival of patients with gastric cancer. J Clin Oncol 31(7):868–875. https://doi.org/10.1200/JCO.2012.44.4612 Epub 2013 Jan 22
Camargo MC, Kim WH, Chiaravalli AM, Kim KM, Corvalan AH, Matsuo K, Yu J, Sung JJ, Herrera-Goepfert R, Meneses-Gonzalez F, Kijima Y, Natsugoe S, Liao LM, Lissowska J, Kim S, Hu N, Gonzalez CA, Yatabe Y, Koriyama C, Hewitt SM, Akiba S, Gulley ML, Taylor PR, Rabkin CS (2014) Improved survival of gastric cancer with tumour Epstein-Barr virus positivity: an international pooled analysis. Gut 63(2):236–243. https://doi.org/10.1136/gutjnl-2013-304531
Almhanna, K, and Scott A. (2017). PD-L1 antibodies for EBV-positive gastric cancer, Going beyond PD-L1 expression and microsatellite instability. JNCI (accepted to print)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures followed were in accordance with the Ethical Standards of the Responsible Committee on Human Experimentation (independent Scientific Committe of Siena University) and with the Helsinki declaration of 1975 and revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study. Additional written informed consent for the treatment of personal and sensible data was obtained from all patients prior to the data collection and evaluation.
Additional information
The article is part of topical collection on Gastric Cancer Surgery.
Rights and permissions
About this article
Cite this article
Marrelli, D., Polom, K., Neri, A. et al. Clinical impact of molecular classifications in gastric cancer. Updates Surg 70, 225–232 (2018). https://doi.org/10.1007/s13304-018-0546-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0546-0