Abstract
We used national survey data to (1) determine the extent to which individuals trust the sources from which they are most likely to receive information about cancer-related genetic tests (BRCA1/2, Lynch syndrome), (2) examine how level of trust for sources of genetic information might be related to cancer-related genetic testing uptake, and (3) determine whether key factors, such as cancer history and numeracy, moderate the latter association. We used cross-sectional data from the Health Information National Trends Survey. Our study sample included individuals who responded that they had heard or read about genetic tests (n = 1117). All analyses accounted for complex survey design. Although respondents trusted information from health professionals the most, they were significantly less likely to report hearing about genetic testing from such professionals than via television (p < 0.01). Regardless of source, higher levels of trust in the information source from which participants heard about genetic tests were associated with increased odds of genetic testing uptake, particularly among those with a personal cancer history. Numeracy was not associated with genetic testing uptake. Because health professionals were among the most trusted health information sources, they may serve as important brokers of genetic testing information for those with a personal cancer history.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Targeted screening and treatment using genetic technologies are becoming increasingly common in this era of precision medicine. For individuals with a family or personal history of disease, genetic testing may be used to identify individuals at especially high risk. Identifying those with high-penetrance genes could be a promising public health application of whole genome or gene panel sequencing [3]. Overall, about 1% of the US population (~3,220,000 people) is estimated to carry a clinically actionable and highly penetrant genetic mutation [3, 37]. Indeed, clinical guidelines around BRCA1/2-attributed breast and ovarian cancers and Lynch Syndrome, among others, have been developed and can be implemented upon discovery of a genetic mutation. This is important, for example, as 45–65 and 11–39% of women with known BRCA1 or BRCA2 mutations develop breast and ovarian cancers, respectively [6]. Conversely, 12 and 1.3% of women in the general population develop breast and ovarian cancers, respectively [6].
Genetic testing for those at increased lifetime risk of a genetic disease, such as those with extensive family or personal cancer histories, could improve current cancer prevention efforts. Preventive protocols for such diseases including enhanced screening (e.g., earlier age of screening initiation, more frequent screening, or more sensitive screening modalities) and prophylactic treatments (e.g., prophylactic surgical procedures or chemoprevention) have been developed [9] that reduce mortality and cost [18, 11, 2]. For those with a personal cancer history, genetic testing may also lead to targeted cancer treatment regimens in addition to enhanced screening protocols [30].
However, use of genetic tests remains suboptimal among individuals who are eligible [14]. For example, among families with known BRCA1/2 mutations, uptake of genetic testing remained low [14]; this is particularly true among black women [31]. Not all cancers are hereditary (only 5–10%) [17] and not everyone who is eligible for genetic testing undergoes testing. Understanding why individuals do not obtain testing is important for maximizing the utility of these tests. Although there are many legitimate reasons why an individual may decide not to pursue genetic testing, one possibility is that individuals may not feel they have received reliable and trustworthy information necessary to move the process forward.
Studies demonstrate that patients learn about health information from many different sources. In particular, when patients do not receive health information from providers, they turn to alternative information sources, which often are perceived as less trustworthy [7, 24]. Information sources with low perceived credibility are less persuasive than sources with high perceived credibility [29]. Thus, individuals who receive information about genetic testing from trusted sources may be more likely to accept and act upon this credible information about genetic tests. Trusting the information source may be particularly important among racial/ethnic minorities and low socioeconomic populations; for example, evidence has shown that blacks are more likely to harbor lower levels of trust about genetic testing and the medical community more broadly [8, 32] and to have lower health literacy [28]. Evidence suggests that preferences for health information sources vary by health literacy level [33, 32]. For instance, patients with low functional health literacy report preferences to receive health information from face-to-face clinical interactions with a trusted provider and may be less likely to seek information beyond the provider encounter and report the lowest preference for written information in print or online [16]. The latter is not true for those with adequate health literacy or numeracy (the ability to interpret and act upon numerical information [21]).
Although research findings indicate that health communication (e.g., health care provider communication), demographics (e.g., race/ethnicity, numeracy, age), and health history factors (e.g., cancer history) may be associated with genetic test uptake [38], to date no studies have explicitly examined the association between receiving genetic information from trusted sources and genetic test uptake within a national sample of US adults. That is, do people trust the sources from which they are getting their information about genetic testing, and is level of trust in these sources associated with test uptake? This question is particularly relevant as screening and treatment become more targeted and as genetic testing becomes more common. The objectives of this study were to determine the extent to which individuals trust the sources from which they receive information about cancer-related genetic tests (i.e., BRCA1/2, Lynch syndrome) and to examine how level of trust in genetic information might be related to the uptake of cancer-related genetic testing. We also examined whether other key factors, including cancer history and numeracy, play a role in the latter association.
Materials and Methods
Data Source
We used the data from the Health Information National Trends Survey (HINTS 4, Cycle 3), a population-based survey administered by the National Cancer Institute [36]. Because few studies have examined genetic testing outside of a research context, these data provide a unique opportunity to examine public perceptions about genetic testing. Prior research with this data set has examined the prevalence and sociodemographic and psychosocial correlates (but not trust in information sources) of having had BRCA1/2 or Lynch syndrome genetic testing and sharing this information with health professionals and family members [34]. The survey was mailed to non-institutionalized, civilian adults, ages 18 and older, between September and December of 2013. African Americans and Hispanics were oversampled. HINTS 4, Cycle 3 data are de-identified and publicly available [36]. Of the 3185 respondents, our study sample included individuals who responded “yes” to the following survey item: “Genetic tests that analyze your DNA, diet, and lifestyle for potential health risks are currently being marketed by companies directly to consumers. Have you heard or read about these genetic tests?” (n = 1117, 35.1%). We excluded individuals who answered a follow-up question (“From which of the following sources did you read or hear anything about genetic tests?”) with “have not heard” (i.e., a commission error) (n = 5) or “missing” (n = 9) “not sure” (n = 26) or “other only” (n = 27).
Measures
Dependent Variables
The key dependent variable for this study was uptake of a cancer-related genetic test, which was self-reported and included reporting ever having “BRCA1/2 testing: to determine if a person has more than an average chance of developing breast cancer or ovarian cancer” and “Lynch Syndrome testing: to determine if a person has more than an average chance of developing colon cancer.” Participants were asked, “Have you ever had any of the following type(s) of genetic tests?” and instructed to mark all that apply. For the sake of comparison, we also included uptake of non-cancer-related genetic testing, which included paternity testing, ancestry testing, DNA fingerprinting, and cystic fibrosis carrier testing.
Primary Independent Variables
Trust in Genetic Testing Information Sources
The key independent variable was mean level of trust in sources from which participants learned about genetic testing. This variable integrated two survey questions. First, respondents reported “how much [they] trust information about health or medical topics” from seven information sources (i.e., a doctor, family or friends, online newspapers, print newspapers, special health or medical magazines or newsletters, radio, internet, local television, national or cable television news programs, government health agencies, charitable organizations, religious organizations and leaders) on 4-point Likert scales (not at all, a little bit, some, a lot). Second, respondents reported their information source for genetic testing by answering “from which of the following sources did [they] read or hear anything about genetic tests?” with the option to select one or more information sources (i.e., newspaper, magazine, radio, health professional, family member, social media, television, internet, other). Because survey response categories across these two questions were not identical, we collapsed categories (e.g., online newspapers and print newspapers were collapsed to “newspapers”) and we matched information sources across the two survey items (Appendix 1). Receiving information from a health professional specifically was included as a primary independent variable, as studies indicate that this may be an important factor in genetic testing uptake. Because patients often overestimate their risk for hereditary cancer, discussions with providers about genetic testing may actually lower patients’ risk perceptions and thus be associated with lower genetic test uptake [22].
Personal and Family Cancer Histories
We included self-reported personal and family cancer histories as primary independent variables, as those with a personal and/or family cancer history are more likely to be clinically eligible for Lynch syndrome testing and BRCA1/2 testing [9, 20]. Having a personal cancer history and family history of cancer, respectively, were defined as responding “yes” to the following questions: “Have you ever been diagnosed as having cancer?” and “Have any of your family members ever had cancer?”
Demographics
We included numeracy as a primary independent variable using an adapted measure from the Newest Vital Signs measure [40] in the survey in which respondents could score 0 (lowest numeracy) through 4 (highest numeracy). Numeracy was skewed towards high numeracy and as such was dichotomized as high (numeracy score = 4) and low (numeracy score < 4) consistent with prior research [1]. Finally, we included age as a categorical primary independent variable (i.e., 18–34, 35–49, 50–64, 65–74, or 75+ years), as age and numeracy level may be inversely associated [4].
Covariates
We controlled for several other key demographic and socioeconomic factors. Race was dichotomized as black (i.e., African American) or non-black (White, American Indian, or Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean Vietnamese, Other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, Other Pacific Islander) because we were interested in identifying potential disparities between black and non-black groups, as blacks are less likely to receive genetic testing [31] and have lower levels of trust about genetic testing [32]; we did not have power to further disentangle the non-black subgroup. Ethnicity was defined as Hispanic (Mexican, Mexican American, Chicano/a, Puerto Rican, Cuban, another Hispanic, Latino/a, or Spanish Origin) or non-Hispanic (not of Hispanic, Latino/a, or Spanish origin). Insurance was defined as a binary variable “insured” (i.e., private, Medicare, Medicaid, Tricare, VA, Indian Health Service) or “uninsured.” We used an imputed income variable which was categorized into nine categories (i.e., $0–9999, 10–14,999, 15–19,999, 20–34,999, 35,000–49,999, 50–74,999, 75,000–99,999, 100–199,999, 200,000+). The imputed income variable was made available in the HINTS 4, Cycle 3 data set, as 14% of the unweighted income values was missing. The imputed variable was derived using several socioeconomic status variables, including education level, race/ethnicity, whether home is rented/owned, whether born in the USA, and self-rated ability to speak English [36]. Marital status was dichotomized as “married or living as married” or “divorced, widowed, separated or single (never married).” Education was a categorical variable (i.e., <8 grade, 8–11 grades, 12 grade or GED, post high school, some college, college graduate, post graduate). Gender was self-reported as male or female.
Analyses
We conducted a complete case analysis. Overall, individuals with missing data for the dependent variable and primary independent variables had lower education and income and were black, Hispanic, or female (data not shown). To account for the complex probability sampling design and jackknife replicate weights, all analyses were weighted to obtain nationally representative results. We used bivariate weighted linear regression (for continuous variables) and weighted chi-square testing (for binary and categorical variables) to examine descriptive differences between those who did and did not report having cancer-related genetic testing.
Using weighted multivariate logistic regression analyses, we examined the association between level of trust in genetic information sources and test uptake. A full model, which included all variables of interest (i.e., trust in genetic testing information sources, personal cancer history, family cancer history, numeracy, race, age) as well as covariates (i.e., race, ethnicity, insurance status, income level, marital status, education, and gender) was developed, and backwards elimination was used to identify covariates that were statistically significant and influenced the regression estimates: accordingly, we included only primary independent variables that were significant in this initial model in our final model. Potential interactions among primary independent variables were examined; specifically, we examined two-way interactions among trust in genetic information sources, personal cancer history, family cancer history, numeracy, age, and receiving genetic testing information from a health professional within a single multivariable logistic regression model. We identified an interaction between personal cancer history and level of trust in genetic information sources; all other potential interactions were null, including interactions between numeracy and other primary independent variables. As a result, our final model included all primary independent variables and an interaction term between personal cancer history and level of trust for genetic information sources. For the sake of comparison, associations between these variables with non-cancer-related genetic testing were also examined, as we would not expect a personal cancer history to be associated with uptake of non-cancer-related genetic testing. We plotted predicted probabilities of genetic testing by personal cancer history across levels of trust in genetic information sources, accounting for survey design.
Results
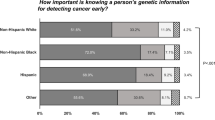
Demographic population characteristics have been reported elsewhere [1]. Of note, 53% of the sample was male, white (78.5%), non-Hispanic (87.4%), employed (66%), had health insurance (85.4%), and had high numeracy (62.5%, 4/4 numeracy items correct). Almost two thirds of the respondents (62.7%) learned about genetic testing from more than one source (SE = 0.022, 95% CI = 0.58, 0.67). Interestingly, although respondents were most likely to hear about genetic testing from the television (53%, 95% CI = 0.48, 0.58) (Table 1), they had the lowest trust in health information from this source (1.69, 95% CI = 0.62, 2.76) (Table 2). Conversely, respondents were significantly less likely to report hearing about genetic testing from health professionals (16%, 95% CI = 0.13, 0.20), despite reporting significantly higher levels of trust in health information from health professionals than from the television (see Tables 1 and 2 for statistics). Few respondents (12.4%) learned about genetic testing only from the television (SE = 0.01, 95% CI = 0.100, 0.015). Of those who learned about genetic testing from a health professional, fewer than half also reported learning about genetic testing from the television (data not shown).
Individuals who did and did not receive cancer-related genetic testing did not significantly differ in the sources from which they learned about genetic testing. In terms of demographic factors, those receiving cancer-related genetic testing tended to be female and were more likely to have a personal history of cancer compared to those who did not receive testing (Table 3). A higher proportion of respondents who had genetic testing reported a family history of cancer (83.1%) than those who did not receive testing (65.5%); however, this difference was not statistically significant (p = 0.07).
We observed a significant interaction between having a personal history of cancer and level of trust for the source of genetic testing information (OR = 7.497, p = 0.015, 95% CI = 1.499, 37.481.622) (Table 4). Specifically, among those with a personal history of cancer, increased trust was associated with increased predicted probability of receiving genetic testing. This was not true among those without a personal history of cancer (see Fig. 1).
As one would expect, such a pattern did not emerge for uptake of non-cancer-related genetic testing (see Fig. 2). Family cancer history, numeracy, and receiving information about genetic testing from a health professional were not associated with non-cancer-related or cancer-related genetic testing uptake (see Table 4).
Discussion
Our results suggest that individuals who have heard or read about genetic tests are most likely to receive this information about genetic testing from the very health information sources they trust the least. A previous study supports our finding that health information is most trusted from health professionals compared to other information sources [7]; however, we also found that respondents were less likely to report hearing or reading information about genetic testing from trusted health professionals compared to other sources, such as the television or the internet. Of particular concern, only 26.9% of those who received cancer-related genetic testing heard or read about genetic testing from a provider, possibly suggesting that patients are not receiving genetic counseling prior to testing. Of note, direct-to-consumer (DTC) genetic testing for cancer-related genes was available until November 2013, when the Food and Drug Administration (FDA) sent a warning letter to a DTC genetic testing company [12]. This may partially contribute to our results, as a cohort study of DTC genomic testing consumers in 2010 indicated that only 26.5% discussed their test results with their provider [10]. Today, DTC genetic testing is still an issue, as the public can order health-related carrier testing through direct-to-consumer test companies as of February 2015 [13].
Level of trust for genetic information sources as well as the source of information itself did not vary between those who received cancer-related genetic testing versus those who did not. However, when controlling for other factors, increased levels of trust for genetic information sources were associated with an increased predicted probability that individuals received cancer-related genetic testing, only if they had a personal history of cancer. In other words, for those who are more likely to be eligible for genetic testing (e.g., to inform future screening and/or treatment), level of trust for the genetic testing information source was associated with uptake of genetic testing. Higher levels of trust were associated with increased odds of receiving cancer-related genetic testing. This association was not observed for non-cancer-related genetic testing, suggesting that the factors driving cancer-related genetic testing differ for non-cancer-related genetic testing, such as ancestry—which is commonly advertised through less trusted information sources such as the television and internet [5]. These results may point to the importance of disseminating information about cancer-related genetic testing through trusted channels, such as health professionals, particularly for individuals with a personal cancer history.
Despite this need, other studies show that health professionals report feeling unprepared to deliver information about genetic testing [15] and are overburdened with other tasks during the health care visit [39]. Thus, it may in fact be beneficial for information about genetic testing to be disseminated through other information channels. Additional research is necessary to better understand which trusted information source should be leveraged to increase uptake of genetic testing among those who are both eligible and interested in pursuing genetic testing.
We did not observe an interaction between family cancer history and trust, perhaps because the majority of those with a family history of cancer (as defined in our study) may not be eligible for genetic testing according to clinical guidelines [27, 20, ]. Surprisingly, we did not find that receiving information about genetic testing from a provider versus other sources was associated with uptake of cancer-related genetic testing, perhaps suggesting that trust in information source is more important than the information source itself. Additional research is necessary to determine whether individuals are truly obtaining BRCA1/2 and Lynch syndrome testing without consulting or going through providers: the data obtained here suggest that this may be the case. Alternatively, it is possible that some individuals interpreted the question as asking about which information source they first heard about genetic testing from and may not have marked all that apply, resulting in underrepresentation of hearing about genetic testing from health professionals.
Although numeracy may not be associated with uptake of genetic testing, a previous review of the literature suggests that low numeracy may be associated with lower ability to interpret and apply genetic information [19, 25]. Similarly, there does not appear to be an association between age and gender with cancer-related genetic testing [35, 26]. Our divergent findings could be due to power limitations, as small cell sizes resulted when all covariates were included in the model.
Limitations
This study has several limitations. First, although HINTS data originate from a nationally representative sample, awareness of genetic testing remains relatively low [1] and genetic testing remains a rare occurrence. Consequently, a small sample size and unequal sample sizes between those who did and did not obtain testing may have limited our ability to observe associations between covariates and the uptake of genetic testing. This small sample size, as well as the cross-sectional nature of the data set, limited our ability to examine mediators of demographic characteristics and genetic testing uptake (i.e., causal beliefs and cognitive and emotional processes). Because HINTS data were collected through a self-administrated mailed survey, we have limited knowledge of exactly who has completed each survey item and whether the respondent received help responding to items, which has implications for measures such as numeracy. Furthermore, because these data are cross-sectional, we are unable to assess temporality or causality in our analyses, specifically between trust and genetic testing uptake. We were unable to assess the appropriateness of genetic testing uptake for any given respondent or to determine how many individuals who did not undergo testing were in fact eligible (e.g., we could not assess type of personal cancer diagnosis or age of onset). This has implications concerning the source from which individuals learn about genetic testing, as providers would be less likely to discuss genetic testing with patients who are ineligible for testing. Future studies should further examine whether causal beliefs and cognitive/emotional processes mediate genetic testing uptake to better establish the relationship between trust in genetic testing information and genetic test uptake.
Conclusions
Overall, these results suggest that trust in the source of one’s information about genetic testing is associated with greater uptake of cancer-related genetic testing among individuals with a personal cancer history. Because providers were among the most trusted sources of health information, providers may be important brokers for genetic testing information. In one study, fewer than half of the patients who reported interest in genetic testing had a discussion with providers about testing [22]. Furthermore, providers report that they have insufficient training with regard to communicating about genetic testing [15, 23]. As such, provider-level interventions that improve communication about genetic testing to patients may be important. Additional research is necessary to better understand the most effective mode of communication about genetic testing to the public and to those with a personal cancer history for whom higher levels of trust for genetic information sources are associated with genetic testing uptake.
References
Agurs-Collins T, Ferrer R, Ottenbacher A, Waters EA, O'Connell ME, Hamilton JG (2015) Public awareness of direct-to-consumer genetic tests: findings from the 2013 U.S. Health Information National Trends Survey. J Cancer Educ 30(4):799–807. doi:10.1007/s13187-014-0784-x
Anderson K, Jacobson JS, Heitjan DF, Zivin JG, Hershman D, Neugut AI, Grann VR (2006) Cost-effectiveness of preventive strategies for women with a BRCA1 or a BRCA2 mutation. Ann Intern Med 144(6):397–406
Berg JS, Khoury MJ, Evans JP (2011) Deploying whole genome sequencing in clinical practice and public health: meeting the challenge one bin at a time. Genet Med 13(6):499–504. doi:10.1097/GIM.0b013e318220aaba
Bruine de Bruin W, McNair SJ, Taylor AL, Summers B, Strough J (2015) “Thinking about numbers is not my idea of fun”: need for cognition mediates age differences in numeracy performance. Med Decis Mak 35(1):22–26. doi:10.1177/0272989X14542485
Caulfield T, Ries NM, Ray PN, Shuman C, Wilson B (2010) Direct-to-consumer genetic testing: good, bad or benign? Clin Genet 77(2):101–105. doi:10.1111/j.1399-0004.2009.01291.x
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25(11):1329–1333. doi:10.1200/JCO.2006.09.1066
Clarke MA, Moore JL, Steege LM, Koopman RJ, Belden JL, Canfield SM, Meadows SE, Elliott SG, Kim MS (2015) Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: a literature review. Health Inform J. doi:10.1177/1460458215602939
Cuevas AG, O'Brien K, Saha S (2016) African American experiences in healthcare: "I always feel like I'm getting skipped over". Health Psychol. doi:10.1037/hea0000368
Daly, Mary B., et al. (2016) "Genetic/familial high-risk assessment: breast and ovarian, version 2.2015." Journal of the National Comprehensive Cancer Network 14(2):153–162
Darst BF, Madlensky L, Schork NJ, Topol EJ, Bloss CS (2014) Characteristics of genomic test consumers who spontaneously share results with their health care provider. Health Commun 29(1):105–108. doi:10.1080/10410236.2012.717216
Dinh TA, Rosner BI, Atwood JC, Boland CR, Syngal S, Vasen HF, Gruber SB, Burt RW (2011) Health benefits and cost-effectiveness of primary genetic screening for Lynch syndrome in the general population. Cancer Prev Res (Phila) 4(1):9–22. doi:10.1158/1940-6207.CAPR-10-0262
Federal Drug Administration (2013) Warning letter. In: No. GEN1300666, ed. Federal Drug Administration. Silver Spring, MD
Federal Drug Administration (2015) FDA permits marketing of first direct-to-consumer genetic carrier test for Bloom syndrome. FDA News Release.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm435003.htm. Accessed 2016
Finlay E, Stopfer JE, Burlingame E, Evans KG, Nathanson KL, Weber BL, Armstrong K, Rebbeck TR, Domchek SM (2008) Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test 12(1):81–91. doi:10.1089/gte.2007.0037
Freedman AN, Wideroff L, Olson L, Davis W, Klabunde C, Srinath KP, Reeve BB, Croyle RT, Ballard-Barbash R (2003) US physicians’ attitudes toward genetic testing for cancer susceptibility. Am J Med Genet A 120A(1):63–71. doi:10.1002/ajmg.a.10192
Gaglio B, Glasgow RE, Bull SS (2012) Do patient preferences for health information vary by health literacy or numeracy? A qualitative assessment. J Health Commun 17(Suppl 3):109–121. doi:10.1080/10810730.2012.712616
Garber JE, Offit K (2005) Hereditary cancer predisposition syndromes. J Clin Oncol 23(2):276–292. doi:10.1200/JCO.2005.10.042
Guillem JG, Wood WC, Moley JF, Berchuck A, Karlan BY, Mutch DG, Gagel RF et al (2006) ASCO/SSO review of current role of risk-reducing surgery in common hereditary cancer syndromes. J Clin Oncol 24(28):4642–4660. doi:10.1200/JCO.2005.04.5260
Hanoch Y, Miron-Shatz T, Rolison JJ, Ozanne E (2014) Understanding of BRCA1/2 genetic tests results: the importance of objective and subjective numeracy. Psychooncology 23(10):1142–1148. doi:10.1002/pon.3537
Hegde M, Ferber M, Mao R, Samowitz W, Ganguly A, Genetics Working Group of the American College of Medical, and Committee Genomics Laboratory Quality Assurance (2014) ACMG technical standards and guidelines for genetic testing for inherited colorectal cancer (Lynch syndrome, familial adenomatous polyposis, and MYH-associated polyposis). Genet Med 16(1):101–116. doi:10.1038/gim.2013.166
Institute of Medicine Committee on Health Literacy (2004) Health literacy: a prescription to end confusion. Institute of Medicine. The National Academies Press: Institute of Medicine, Washington DC
Jagsi R, Griffith KA, Kurian AW, Morrow M, Hamilton AS, Graff JJ, Katz SJ, Hawley ST (2015) Concerns about cancer risk and experiences with genetic testing in a diverse population of patients with breast cancer. J Clin Oncol 33(14):1584–1591. doi:10.1200/JCO.2014.58.5885
Klitzman R, Chung W, Marder K, Shanmugham A, Chin LJ, Stark M, Leu CS, Appelbaum PS (2013) Attitudes and practices among internists concerning genetic testing. J Genet Couns 22(1):90–100. doi:10.1007/s10897-012-9504-z
Kowalczyk N, Draper LJ (2012) Trends in patient information preferences and acquisition. Radiol Technol 83(4):316–324
Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW (2011) Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics 14(4–5):279–289. doi:10.1159/000294191
Lerman C, Daly M, Masny A, Balshem A (1994) Attitudes about genetic testing for breast-ovarian cancer susceptibility. J Clin Oncol 12(4):843–850
Nelson HD, Fu R, Goddard K, Mitchell JP, Okinaka-Hu L, Pappas M, Zakher B (2013) Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer: systematic review to update the U.S. Preventive Services Task Force recommendation. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews, Rockville (MD)
Paasche-Orlow MK, Wolf MS (2010) Promoting health literacy research to reduce health disparities. J Health Commun 15(Suppl 2):34–41. doi:10.1080/10810730.2010.499994
Petty RE, Wegener DT (1998) Attitude change: multiple roles for persuasion variables. In: Fiske ST, Gilbert DT, Lindzey G (eds) The handbook of social psychology. McGraw-Hill, New York, NY, pp 323–390
Schwartz MD, Lerman C, Brogan B, Peshkin BN, Halbert CH, DeMarco T, Lawrence W et al (2004) Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol 22(10):1823–1829. doi:10.1200/JCO.2004.04.086
Simon MS, Petrucelli N (2009) Hereditary breast and ovarian cancer syndrome: the impact of race on uptake of genetic counseling and testing. Methods Mol Biol 471:487–500. doi:10.1007/978-1-59745-416-2_25
Singer E, Antonucci T, Van Hoewyk J (2004) Racial and ethnic variations in knowledge and attitudes about genetic testing. Genet Test 8(1):31–43. doi:10.1089/109065704323016012
Suri VR, Majid S, Chang YK, Foo S (2016) Assessing the influence of health literacy on health information behaviors: a multi-domain skills-based approach. Patient Educ Couns 99(6):1038–1045. doi:10.1016/j.pec.2015.12.017
Taber JM, Chang CQ, Lam TK, Gillanders EM, Hamilton JG, Schully SD (2015) Prevalence and correlates of receiving and sharing high-penetrance cancer genetic test results: findings from the Health Information National Trends Survey. Public Health Genomics 18(2):67–77. doi:10.1159/000368745
Tambor ES, Rimer BK, Strigo TS (1997) Genetic testing for breast cancer susceptibility: awareness and interest among women in the general population. Am J Med Genet 68(1):43–49
The National Cancer Institute (2015) HINTS 4 Cycle 3. http://hints.cancer.gov/. Accessed 2016
United States Census Bureau (2016) US and world population clock.http://www.census.gov/popclock/. Accessed 2016
Waters EA, Muff J, Hamilton JG (2014) Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genet Med 16(12):913–921. doi:10.1038/gim.2014.49
Watson EK, Shickle D, Qureshi N, Emery J, Austoker J (1999) The ‘new genetics’ and primary care: GPs’ views on their role and their educational needs. Fam Pract 16(4):420–425
Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA (2005) Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med 3(6):514–522. doi:10.1370/afm.405
Acknowledgements
This work was funded by intramural National Cancer Institute funds. The authors have no conflicts of interest. The views and opinions expressed in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health or any other governmental agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study includes the secondary data analysis of human subject research, as such informed consent was not applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Roberts, M.C., Taber, J.M. & Klein, W.M. Engagement with Genetic Information and Uptake of Genetic Testing: the Role of Trust and Personal Cancer History. J Canc Educ 33, 893–900 (2018). https://doi.org/10.1007/s13187-016-1160-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1160-9