Abstract
The objective of this study is to identify levels of risk awareness for breast, lung and cervical cancer, in a UK student population. A sample of male (N = 62) and female (N = 58) university students, mean age 21.62 years completed a questionnaire identifying which risk factors they knew for each cancer. Analysis of variance was used to compare differences in risk awareness across gender and cancer types. Risk factor awareness was highest for lung cancer (0.78), mid-range for breast cancer (0.61) and lowest for cervical cancer (0.47). Women had greater risk factor awareness (0.67) than males (0.57) across all three cancers. There is also significant belief in mythic risk factors such as stress (from 14 to 40 % across the three cancers). Previous research has demonstrated that risk factor awareness increases with educational status, yet even in a university student population, in which the majority of females would have been offered the HPV vaccination, risk factor awareness for cancers is variable. More health education is needed particularly around the risk factors for cervical cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In economically developed countries cancer is the most common cause of death [1]. The burden that cancer brings is worsening because of lifestyle choices that increase cancer causing behaviours, such as smoking, as well as a growing population age as life expectancy increases. The impact of lifestyle choices on cancer rates has the potential to be reduced through the translation of existing knowledge into prevention techniques, along with improvements in public health education.
Siegel et al. [2] report that men have a higher probability of developing invasive cancer in their lifetime (45 %) than women (38 %). Lung cancer is the most commonly diagnosed and the largest cause of cancer-related deaths globally, as well as being the leading cancer in males [1]. Breast cancer is the second most frequent cancer in the world [3] and the leading cause of cancer death among females [1]. Cervical cancer is the fourth most common cancer to affect women worldwide [4], although cases in developed countries are relatively low in comparison to developing countries thanks to comprehensive screening programmes. However, uptake of invitations for cervical screening in the UK is dropping, and this study seeks to investigate how risk awareness for cervical cancer compares to a gender neutral cancer (lung) and a predominantly female cancer (breast).
Previous research has investigated awareness of different cancer risk factors. For example, Breslow et al. [5] examined Americans' knowledge of risk factors for breast, cervical, bowel and prostate cancer, by obtaining data from the National Health Interview Survey in 1992 which included questions about cancer risk and survival. The majority of participants failed to identify several major risk factors when presented with a list. Two thirds could not identify age as a risk factor for breast cancer or multiple sexual partners as increasing an individual's risk of developing cervical cancer. It was concluded that Americans lack knowledge of the risk factors for several types of cancer and that knowledge of cervical cancer was particularly poor. However, female participants were only asked about cancers that affect females and male participants were only asked about cancers that affect males, even though both genders can be vigilant for partners’ behaviour. In addition, whilst cervical cancer is a female cancer, men play a role in the transmission of the human papillomavirus which causes cervical cancer.
Wardle et al. [6] examined British adults’ knowledge of the causes of breast, cervical, prostate, bowel and lung cancer, to see if they could distinguish between acknowledged risk factors and mythic risks of cancer. Participants were presented with a questionnaire containing questions about different cancers which comprised a list of scientifically found risks and mythic risks including food additives and living near power lines. Participants were asked to tick the relevant risk factors for each specific type of cancer. Out of 15 well-established associations with increased cancer risk, on average, only five were correctly identified, with the association between smoking and lung cancer the best identified risk. Women correctly identified more risk factors than men, whilst men believed more mythic risks to be actual risks than women. The researchers acknowledged that many risk factors can be linked to all types of cancer, but they focused on the risks associated with each specific cancer for example breast (age, family history, HRT and overweight), lung (age and smoking) and cervical cancer (smoking, a virus/infection and number of sexual partners), as these were widely accepted by epidemiologists although they did not compare knowledge between the different cancers.
Adlard and Hume [7] carried out surveys in two primary care settings in the UK, investigating if adults could identify the risk factors for common types of cancer from a list of true and false causes. They found most participants were able to distinguish between true and false causes, but in their literature review, they observed that patients often fail to identify specific symptoms for specific cancers. Females had greater awareness of cancer than males. In addition, 20 % of participants thought that mobile phones and overhead power lines caused cancer, despite there being no evidence to support these factors.
Previous research has highlighted both men and women in the UK to be most aware that smoking causes lung cancer, in comparison to other behaviours associated with cancer [6, 7]. Hammard et al. [8] propose that one reason for this is that cigarette warning labels make people more aware of the health consequences and are more effective in countries where they are mandatory, for example the UK. Sanderson et al. [9] suggest that this association may be well recognised because it makes logical sense that inhaling smoke causes problems with the lungs.
Men are targeted less in public health campaigns about breast cancer because it mainly affects women, and male breast cancer receives little attention from public health initiatives, because it is less common, often leaving men unaware they can get breast cancer and less aware of the risk factors of breast cancer than other cancers [10]. The majority of research and health campaigns regarding cervical cancer are also targeted at women [11]. Male respondents are therefore less likely to be aware of the risk factors for breast and cervical cancer than women respondents.
Although previous studies have explored the relative awareness of risk factors for different cancers, the most recent comparison was over 10 years ago. A more recent study focusing specifically on student awareness of risk factors for cancer in general has found that student knowledge is low, with 59 % identifying that they knew little to very little about cancer [12]. At least two significant events have occurred in the UK in recent years which might have influenced awareness for cervical cancer risk factors in particular, namely the introduction of the human papillomavirus (HPV) vaccination for schoolgirls in 2008 and the high profile death from cervical cancer of reality television celebrity Jade Goody in 2009. The present study therefore seeks to explore current risk awareness of cervical cancer in comparison with breast and lung cancer amongst university students.
Materials and Methods
Participants
Participants consisted of 120 students (62 males, 58 females) predominantly from Keele University with a mean age of 21.62 years (SD 1.43). Participants were recruited by opportunity sampling on Keele University campus and snowball sampling via personal contacts of the second author at other UK universities.
Materials
Participants were asked to complete a paper questionnaire adapted from Wardle et al.’s study [6]. The questionnaire consisted of four demographic questions (age, gender, year of study and course of study). A further three questions required participants to select the risk factors for each type of cancer from a list of 13 items by ticking the corresponding box. Nine of these items were risk factors that have been strongly linked with cancer, and four were mythic risk factors that are often believed to cause cancer.
Results
The percentage of participants who believed each risk factor to be a cause of breast, lung and cervical cancer were calculated and are presented in Table 1.
A mean awareness score was then calculated for each participant for each cancer based on the number of risk factors that they correctly identified for each cancer type (breast: age, family history, HRT and overweight; lung: age and smoking; cervical cancer: smoking, a virus/infection and number of sexual partners), and these are presented in Table 2.
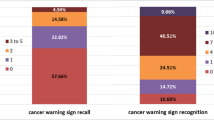
These scores were entered into a 2 (gender: male, female) × 3 (cancer type: breast, cervical, lung) mixed analysis of variance (ANOVA) and are presented in Fig. 1. There was a main effect of cancer type F (2, 236) = 51.04, MSe = .06, p < 0.001. Post hoc t-tests using a Bonferroni correction show that risk awareness of lung cancer (M = 0.78, SE = 0.02) was significantly higher than risk awareness for breast cancer (M = 0.61, SE 0.02) which was in turn significantly higher than risk awareness for cervical cancer (M = 0.47, SE = 0.03) (ps < 0.017).
There was a main effect of gender F (1, 118) = 8.36, MSe = .12, p < 0.01, with women having a better awareness of cancer risks (M = 0.67, SE = 0.03) than men (M = 0.57, SE = 0.03). There was no interaction between gender and cancer type F (2, 236) = 1.55, MSe = 0.06, p = 0.21.
Discussion
Overall, women showed more awareness of risk factors for the three cancers than men, and these findings are consistent with previous research [6, 7]. Both genders were more aware of the risk factors for lung cancer than for breast cancer and for breast cancer than for cervical cancer. The most consistently recognised risk factor was smoking in association with lung cancer, which replicates the findings from Wardle et al. [6]. Higher breast cancer awareness compared to cervical cancer is also consistent with Breslow et al. [5].
Relative to these previous studies, the current respondents demonstrate an improvement in awareness of risk factors, especially for cervical cancer. For example, previous research found 13 % of women believed smoking to increase their risk of cervical cancer and 35 % believed the number of sexual partners increased their risk [5]. In the current study, these figures were 38 and 74 %, respectively. However, since that study, the introduction of the human papillomavirus (HPV) vaccination for schoolgirls in the UK in 2008 and the high profile death from cervical cancer of reality television celebrity Jade Goody in 2009 have occurred. For the female student population tested in this study, most of whom would have been offered the HPV vaccination, it is worrying that their knowledge about a virus being a risk factor was only 50 %. Anecdotal evidence suggests that the information provided to girls about the HPV vaccination and why it is important is extremely variable. Studies are urgently needed to explore whether this is a missed opportunity to educate young women about cervical cancer and its risk factors.
Although there is little previous research exploring education interventions to increase awareness and knowledge about cancer in young people, two recent studies provide some indication that they can be effective. Adamowicz et al. [13] looked at four different health education strategies and how they increased pro-health attitudes in Polish young people under the age of 18 relative to no strategy being used. Both general knowledge about cancer and healthy lifestyles had improved after 2 months across all the education groups and 1 year later in three of the education groups, with the most effective methods being lectures accompanied by a discussion or a multimedia presentation. An obvious educational intervention would therefore be for schools to deliver lectures and discussions about HPV, cervical cancer and possibly cancer risk factors in general around the time that the HPV vaccination was offered to each cohort. Interventions at school would be more effective at widespread education of young people than interventions at university, since not all young people progress to university. For those who do attend university, at least in the UK, it is hard to see where such a lecture might take place, particularly for courses without a health component. Were it possible to identify an appropriate time for a university intervention to occur, Hwang [14] has demonstrated that undergraduate awareness of risk factors, prevention strategies and warning signs can also be increased by use of an educational intervention (in this case a 60-min lecture followed by a 30-min video). Educational interventions at an institutional level are warranted by Estaville et al.’s observation that 76 % of the students they surveyed ‘seldom, don’t remember, or never discuss cancer’ with family members whilst 85 % say the same for friends [12]. It is especially important since new diagnoses are increasing in women aged 25–34 (from 12.5 per 100,000 between 2000–2002 to 19.2 per 100,000 between 2009–2011) [15].
Conclusions
Previous research has demonstrated that risk factor awareness increases with educational status [16], yet even in a university student population, risk factor awareness for cancers is variable. Risk factor awareness for lung, breast and cervical cancer has increased relative to previous studies. However, awareness of cervical cancer risk factors lags behind that of breast and lung cancer. In light of the increasing number of cases of cervical cancer diagnosed in younger women, more health education is still needed about those risk factors.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62(1):10–29
Parkin DM (2001) Global cancer statistics in the year 2000. Lancet Oncol 2(9):533–543
World Cancer Research Fund International (2014) Cervical cancer. Retrieved 15th April 2014 from http://www.wcrf.org/cancer_statistics/data_specific_cancers/cervical_cancer_statistics.php
Breslow RA, Sorkin JD, Frey CM, Kessler LG (1997) Americans’ knowledge of cancer risk and survival. Prev Med 26(2):170–177
Wardle J, Waller J, Brunswick N, Jarvis M (2001) Awareness of risk factors for cancer among British adults. Publ Health 115(3):173–174
Adlard J, Hume M (2003) Cancer knowledge of the general public in the United Kingdom: survey in a primary care setting and review of the literature. Clin Oncol 15(4):174–180
Hammond D, Fong GT, McNeill A, Borland R, Cummings KM (2006) Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control 15(3):19–25
Sanderson SC, Waller J, Jarvis MJ, Humphries SE, Wardle J (2009) Awareness of lifestyle risk factors for cancer and heart disease among adults in the UK. Patient Educ Couns 74(2):221–227
Thomas E (2010) Men’s awareness and knowledge of male breast cancer. Am J Nurs 110(10):32–37
McPartland TS, Weaver BA, Lee S, Koutsky LA (2005) Men’s perceptions and knowledge of human papillomavirus (HPV) infection and cervical cancer. J Am Coll Heal 53(5):225–230
Estaville L, Trad M, Martinez G (2012) University student understanding of cancer: analysis of ethnic group variances. J Cancer Educ 27(3):580–584
Adamowicz K, Zalewska M, Majkowicz M, Zaucha JM (2014) Evaluation of the impact of different types of health education on the adoption and preservation of prohealth attitudes in preventing cancer in juveniles younger than 18 years. J Cancer Educ 1–7
Hwang LL (2013) Cancer awareness changes after an educational intervention among undergraduate students. J Cancer Educ 28(2):247–253
Cancer Research UK website: http://www.cancerresearchuk.org/cancer-info/cancerstats/types/cervix/incidence/#age. Retrieved 4th August 2014
Low EL, Simon AE, Lyons J, Romney-Alexander D, Waller J (2012) What do British women know about cervical cancer symptoms and risk factors? Eur J Cancer 48(16):3001–3008
Conflict of Interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sherman, S.M., Lane, E.L. Awareness of Risk Factors for Breast, Lung and Cervical Cancer in a UK Student Population. J Canc Educ 30, 660–663 (2015). https://doi.org/10.1007/s13187-014-0770-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-014-0770-3