Abstract
To increase the uptake of the human papillomavirus (HPV) vaccine, understanding the determinants of vaccination intentions for various groups is important. Three studies examining theoretical determinants of college-aged women’s (study 1: n = 286), parents’ of daughters (study 2: n = 230) and parents’ of sons (study 3: n = 137) HPV vaccination intentions were conducted. Participants completed questionnaires assessing constructs of protection motivation theory (PMT) and the theory of planned behaviour (TPB). Results indicate that both PMT and TPB constructs predict intentions for the different groups. Focusing on the response efficacy of the vaccine rather than the severity of contracting HPV may be an effective way to increase vaccination intentions among all groups. Focusing on vulnerability to HPV may only increase intentions among college-aged women and parents of sons, and increasing self-efficacy may only increase intentions among college-aged women and parents of daughters. Findings have implications for understanding differences among groups considering HPV vaccination and tailoring interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Canada, the human papillomavirus (HPV) vaccine has been approved for women and recently for men aged 9 to 26 [13]. However, there are concerns about rates of vaccine uptake in all potential target groups including young girl, boys and college-aged women [6, 9, 16]. For example, the uptake of the government’s HPV vaccination programme that provides the vaccine for free to all grade 8 girls has been low. In some provinces, uptake has been as low as 49 % [9]. Furthermore, hypothetical studies investigating Canadian parents’ intentions to have their son vaccinated indicate that uptake of government vaccination programmes also will be low [15, 16]. Investigations of young Canadian women’s uptake of the HPV vaccine are currently underway [11, 12]. College-aged Canadian women’s access to the HPV vaccine differs from parents of daughters due to the absence of a subsidised school-based vaccination programme for college-aged women and the high cost of the HPV vaccine. Therefore, it has been suggested that the uptake of the HPV vaccine among Canadian women is likely to be even lower than that of parents considering vaccination for their child [11].
Understanding the determinants of HPV vaccine acceptability among specific target groups is necessary to inform future vaccination programmes and campaigns as well as to increase the uptake of the HPV vaccine in Canada. A priori predictions of potential factors that may increase the uptake of the HPV vaccine can be informed by theories of health behaviour [5] such as the health belief model [4], protection motivation theory (PMT, [18]) and the theory of planned behaviour (TPB, [2]).
A systematic review by Brewer and colleagues [5] used the constructs of the health belief model to investigate theory-informed determinants of HPV vaccine acceptability among parents considering the HPV vaccine for their children and adults considering the HPV vaccine for themselves who reside in USA [5]. The health belief model postulates that perceived risk of HPV infection, perceived effectiveness of the vaccine, perceived barriers to vaccination and cues to action are determinants of vaccination behaviour [4]. Within the context of HPV vaccination, perceived risk is comprised of a person’s belief that an HPV infection is likely to occur (perceived vulnerability) and that an HPV infection will result in serious negative consequences for health and well-being (perceived severity). Perceived effectiveness represents a person’s belief that the HPV vaccine will reduce the perceived severity or vulnerability of HPV (response efficacy), and cues to action refers to situational factors such as a doctor’s recommendation that may prompt a person to be vaccinated [4]. Review findings indicated that perceived vulnerability to HPV and response efficacy of the HPV vaccine are key determinants of HPV vaccine acceptability among parents considering vaccination for their child and adults considering vaccination for themselves. Physician recommendations have also been found to be a key cue to action among successful vaccination programmes. Conversely, the review found that perceived severity of HPV was not related to vaccine acceptance, and common barriers among adults and parents for vaccination were not identified.
While the review by Brewer and colleagues [5] provides an indication of the theoretical determinants of HPV vaccination acceptability among adults and parents residing in USA, the findings may not necessarily translate to a Canadian context. In Canada, government-funded HPV vaccination programmes exist for all girls in grade 8. However, similar vaccination programmes do not exist for boys or college-aged women. Therefore, access to the HPV vaccine varies among target groups. Furthermore, a slew of controversy has surrounded the release of the HPV vaccine in Canada. Both scientific and main stream articles questioned the seriousness of HPV infections and cervical cancer, the validity of the HPV vaccine trials and the overall cost and necessity of a vaccination programme [10, 12]. Therefore, the present paper aims to build on the work of Brewer and colleagues [5] by investigating the determinants of vaccination within a Canadian context. In particular, we conducted three studies investigating the determinants of HPV vaccination among three distinct audiences for HPV vaccination campaigns: (a) college-aged women, (b) parents of daughters and (c) parents of sons.
To further build on the work of Brewer and colleagues [5], the second objective of the present paper was to test the applicability of a theoretical framework integrating two alternative health behaviour theories: PMT [18] and the TPB [2] (see Table 1). The protection motivation theory constructs of perceived vulnerability, perceived severity and response efficacy were included in the theoretical framework because their similarity to health belief model constructs allows us to test whether Brewer and colleagues’ [5] findings extend to a Canadian context. In addition, we tested the PMT and TPB construct of self-efficacy/perceived behavioural control which in the context of HPV vaccination represents people’s confidence in their ability to get the vaccine or have their child vaccinated. Finally, we included the TPB construct of subjective norms which allows us to test Brewer and colleagues’ specific findings that important others such as doctors are important cues to action for vaccination.
Given Brewer and colleagues’ [5] findings, we hypothesized that the majority of the determinants of vaccination would likely be similar among all three groups. In particular, we hypothesized that in the present analysis, perceived vulnerability, response efficacy and subjective norms would predict vaccination intentions among all the three groups and that perceived severity would not predict vaccination intentions among any of the three groups. Due to the differences in access to the HPV vaccine among the three groups, we hypothesized that differences in vaccination determinants would also exist among the three groups. Specifically, we hypothesized that self-efficacy would only be a determinant of vaccination among parents of daughters because at the time of the study, a government vaccination programme had only been established for girls in grade 8.
Method
In this study, we report a secondary analysis of data from a series of experiments examining effective messages for promoting the HPV vaccine. The full description of these experiments is reported elsewhere [Gainforth, Cao & Latimer, In Press; 8]. In brief, all participants completed the study online and at one time point. Each participant completed the demographic questionnaire, received a message about HPV and the vaccine and then completed a questionnaire evaluating the theoretical determinants of HPV vaccination. Prior to completing questionnaires, HPV was defined for participants. The message either described the benefits of being vaccinated against HPV or the costs of not being vaccinated against HPV. Only data collected after reading the messages were included in the models presented here. To account for the effects of the messages, experimental condition was used as a covariate in all statistical analyses. All studies reported were approved by the Queen’s University General Research Ethics Board, and all participants consented to participate in the research.
Study 1: Determinants of College-Aged Women’s Intentions to be Vaccinated Against HPV
Participants
A convenience sample of 286 women attending a mid-size, Canadian university participated in the study in exchange for a chance to win gift certificates. Participants were recruited through on-campus flyers and word of mouth. All participants consented to participate in the study. In order to be eligible to participate, women could not have been previously vaccinated against the HPV. The mean age of women who participated in the study was 21.77 years (SD = 2.29), and 46 % of the women had not previously received a pap test. The majority of the women had completed 4 years or less of university (67 %). The majority of the participants were white (80 %, 12 % Chinese, 3 % South Asian, 5 % other). Five participants identified themselves as an aboriginal person.
Measures
Demographic Questionnaire
Participants indicated their sex, age, programme year, ethnicity and aboriginal status.
Sexual Health Questionnaire
Participants indicated ‘yes’ or ‘no’ as to whether they had already received the HPV vaccine and whether they had been pap tested. No specific timeline for screening was indicated. Participants also were asked to respond on a scale ranging from 1 (strongly disagree) to 7 (strongly agree) as to whether they had beliefs against the HPV vaccine.
Self-efficacy
To assess the participants’ confidence in their ability to obtain the HPV vaccine in the next 3 months, a six-item measure adapted from Ajzen’s recommendations [3] was used. Items were rated on a seven-point scale and included (a) ‘I believe that I have the ability to get vaccinated against HPV in the next 3 months (definitely do not/definitely do)’, (b) ‘For me, getting vaccinated against HPV in the next three months will be… (extremely easy/extremely difficult)’, (c) ‘How confident are you that over the next 3 months that you will be able to get vaccinated against HPV? (not at all confident/very confident)’, (d) ‘If it were entirely up to me, I am confident that I would be able to be vaccinated against HPV in the next 3 months (strongly agree/strongly disagree)’, (e) ‘How confident are you over the next 3 months that you could overcome obstacles that prevent you from getting the HPV vaccine? (completely confident/not at all confident)’ and (f) ‘How confident are you over the next 3 months that you could get vaccinated against HPV if you wanted to do so? (completely confident/not at all confident). This scale demonstrated an acceptable internal reliability with a Cronbach’s alpha of .85 [15].
Perceived Response Efficacy
A 12-item measure adapted from Ajzen’s recommendations [3] as well as Neuwirth, Dunwoody and Griffin’s [14] and Courneya and Hellsten’s [7] measures was used to assess the participants’ perceived response efficacy of the HPV vaccine. Items began with a stem of ‘Being vaccinated against HPV…’ and were rated on a seven-point scale ranging from 1 (strongly agree) to 7 (strongly disagree). Items included ‘Being vaccinated against HPV…’ (a) ‘… leads to feelings of relief’, (b) ‘… would reassure me’, (c) ‘… leads to serious side effects’, (d) ‘… leads to certainty about my health status’, (e) ‘… would be extremely effective in protecting me against genital warts’, (f) ‘… would be extremely effective in protecting me against cervical cancer’, (g) ‘… would be extremely effective in protecting me against HPV’, (h) ‘… would be inconvenient for me’, (i) ‘… would be expensive for me’, (j) ‘… would be unpleasant for me’, (k) ‘… would result in serious side effects (e.g. death)’ and (l) ‘… would be embarrassing for me’. This measure showed an acceptable internal reliability with a Cronbach’s alpha of .78 [15].
Perceived Severity
To assess the participants’ beliefs about the severity of HPV, a three-item measure adapted from Courneya and Hellsten’s measure [7] was used. Participants responded using a scale that ranged from 1 (very likely) to 7 (very unlikely). Items included (a) ‘I feel that HPV is a serious infection for me to contract’, (b) ‘I feel that cervical cancer is a serious disease for me to develop’ and (c) ‘I feel that genital warts are a serious disease for me to develop’. This scale had a good internal reliability with a Cronbach’s alpha of .91 [15].
Perceived Vulnerability
To assess the participants’ beliefs about their vulnerability to HPV, a two-item measure adapted from Neuwirth and colleagues [14] was used. Participants responded using a scale that ranged from 1 (very likely) to 7 (very unlikely). Items included (a) ‘Considering your personal circumstances, how likely is it that you will be affected by the HPV?’ and (b) ‘Considering your personal circumstances, how likely is it that you will get genital warts?’ This measure had a good internal reliability with a Cronbach’s alpha of .74 [15].
Subjective Norms
A three-item measure adapted from Ajzen’s recommendations [3] assessed participants’ beliefs as to whether significant others believed they should or should not be vaccinated against HPV. Items were rated on a Likert scale ranging from 1 (strongly agree) to 7 (strongly disagree) and included items such as ‘People in my life whose opinions I value would approve of me being vaccinated against HPV’. This scale had a Cronbach’s alpha of .69, and the internal reliability was deemed acceptable [15].
Intentions
To assess the participants’ intentions to get vaccinated against HPV, a three-item questionnaire adapted from Ajzen’s [3] recommendations was used. Items began with one of three stems (‘I intend’, ‘I will’ and ‘I plan’) and captured intentions, within the next 3 months, to be vaccinated against HPV. Responses were rated using a scale ranging from 1 (strongly disagree) to 7 (strongly agree). This scale’s internal reliability was deemed acceptable with a Cronbach’s alpha of .98 [15].
Study 2: Parents’ Intentions to Have Their Daughters Vaccinated Against HPV
Participants
A convenience sample of 230 parents of daughters in grade 5, 6 or 7 participated in the study in exchange for a chance to win one of ten $25 gift certificates. The majority of the participants (83 %) were recruited face-to-face at various child-centred community and sporting events in Ontario, Canada. If a parent indicated that their daughter in grade 5, 6 or 7 had not been vaccinated, the parent was included in the study. The study was approved by the university’s general research ethics board, and all participants consented to participate in the study.
The mean age of the participants was 42.52 years (SD = 4.73); 83 % of the sample was female. The majority of participants had two (49 %) or three (31 %) children with an average age of 11.35 (SD = 2.52) years. Most of the participants were either Protestant Christian or Roman Catholic, highly educated and Caucasian. The majority of the sample was married and belonged to a dual-income family that had an income equal to or greater than $75,000 a year. Eleven percent of participants had a family history of HPV-related diseases (e.g. cervical cancer, anal cancer). Regarding vaccination, 15 % of participants had personal beliefs against vaccination and 13.5 % of the participants had at least one of their daughters already vaccinated against HPV. Approximately, half of the participants had previously received information about the HPV vaccine. Of the participants who received information, the overall tone was perceived to be positive (M = 5.05, SD = 1.19). In terms of the vaccination decision, 55 % of the sample will be making the decision with their spouse and 41 % will be the primary decision maker.
Measures
Demographic Questionnaire
Participants indicated their sex, age, ethnicity, religion, education, marital status and household income.
Family History Questionnaire
In a measure adapted from Abhyankar and colleagues[1], participants were asked yes or no questions relating to whether or not they had personal beliefs against vaccination in general and whether or not their family has a medical history of HPV-related diseases (e.g. cervical cancer, penile cancer). Participants were asked whether or not they had previously received information about the HPV vaccine and if they had received information. They were asked to rate on a seven-point scale (1 = extremely negative to 7 = extremely positive), the overall tone of the information they received. Participants were also asked who would be the primary person deciding whether or not their child would be receiving the HPV vaccination.
Perceived Severity of HPV
This three-item measure adapted from Courneya and Hellsten’s [7] measure captured the participants’ beliefs about the seriousness of their child developing HPV and/or HPV-related diseases. Items included (a) ‘HPV is a serious infection for my son/daughter to contract’, (b) ‘cervical, penile and anal cancer is a serious disease for my son/daughter to develop’ and (c) ‘genital warts is a serious disease for my son/daughter to develop’. Parents responded using a Likert scale ranging from 1 (strongly agree) to 7 (strongly disagree). This scale demonstrated a good internal reliability with a Cronbach’s alpha of 0.92 in this study [15].
Perceived Response Efficacy
This measure was adapted from Abhyankar and colleagues [1] and includes four items assessing the participants’ perception of the HPV vaccine’s effectiveness. The scale used the stem ‘the HPV vaccination leads to’ (a) certainty about my son/daughter’s health, (b) relief, (c) reassurance and (d) serious side effects and ranged from 1 (strongly disagree) to 7 (strongly agree). This scale had a good internal reliability with a Cronbach’s alpha of .87 [15].
Self-efficacy
This four-item measure was adapted from Ajzen’s [3] recommendations and assessed the participants’ confidence in their ability to have their son/daughter vaccinated and their perception of the ease of doing so. All items used a scale ranging from 1 to 7 and began with a statement holding motivation as a positive constant (e.g. ‘If I was really motivated…’). Sample items included (a) ‘How confident are you that you will be able to have your son/daughter vaccinated against HPV (very unconfident/very confident)’ and (b) ‘For me to be able to have my son/daughter vaccinated against HPV would be (very difficult/very easy)’. This scale had an acceptable internal reliability with a Cronbach’s alpha of 0.86 [15].
Subjective Norms
This four-item measure assessed participants’ beliefs as to whether significant others believed they should or should not have their son/daughter vaccinated. Items were created using Ajzen’s [3] recommendations and were rated on a Likert scale ranging from 1 (strongly agree) to 7 (strongly disagree). Sample items included (a) ‘People in my life whose opinions I value would approve of me having my son/daughter vaccinated against HPV’ and (b) ‘my son/daughter thinks that he/she should get the HPV vaccine’. This scale had a good internal reliability with a Cronbach’s alpha of 0.84 [15].
Perceived Vulnerability
To capture the parents’ feelings about their child being vulnerable to HPV, we used a three-item measure to assess the participants’ anxiety about their child contracting HPV [1]. Participants responded using a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). Items began with the stem ‘Thinking about the possibility of my son/daughter getting HPV when he/she grows up makes me feel’ and is followed by the end points ‘anxious’, ‘fearful’ and ‘worried’. This scale had an acceptable internal reliability with a Cronbach’s alpha of .95 [15].
Intentions
This two-item questionnaire was created using Ajzen’s [3] recommendations. Items were rated on a Likert scale ranging from 1 (strongly agree) to 7 (strongly disagree). Items began with one of two stems (‘I intend’ or ‘I will’) and captured parents’ intentions within the next 3 years to have their daughters vaccinated against HPV. This measure had a good internal reliability with a Cronbach’s alpha of .90 [15].
Study 3: Parents’ Intentions to Have Their Sons Vaccinated Against HPV
Participants
A convenience sample of 137 parents of sons in grade 5, 6 or 7 participated in the study in exchange for a chance to win one of ten $25 gift certificates. The majority of the participants (94.2 %) were recruited face-to-face at various child-centred community and sporting events in Ontario, Canada. If a parent indicated that their son in grade 5, 6 or 7 had not been vaccinated, the parent was included in the study. The study was approved by the university’s general research ethics board, and all participants consented to participate in the study.
The mean age of the participants was 42.58 years (SD = 4.75); 77 % of the sample was female. The majority of participants had two (49 %) or three (29 %) children with an average age of 11.27 (SD = 2.75) years. Most of the participants were either Protestant Christian or Roman Catholic, highly educated and Caucasian. The majority of the sample was married and belonged to a dual-income family that had an income equal to or greater than $75,000 a year. Eight percent of participants had a family history of HPV-related diseases (e.g. cervical cancer, anal cancer). Regarding vaccination, 16 % of the participants had personal beliefs against vaccination and 14 % of the participants had at least one of their daughters already vaccinated against HPV. Approximately, half of the participants had previously received information about the HPV vaccine. Of the participants who received information, the overall tone was perceived to be positive (M = 4.75, SD = 1.29). In terms of the vaccination decision, 66 % of the sample will be making the decision with their spouse and 30 % will be the primary decision maker.
Measures
The measures for study 3 were identical to study 2 except the wording was changed to reflect sons rather than daughters.
Results
Analysis
To test our hypotheses, we tested three separate regression models for each of study. For study 1, beliefs against vaccination and experimental message condition were controlled for in the model. Self-efficacy, response efficacy, perceived severity, perceived vulnerability and subjective norms were entered into the model as potential determinants of intentions to vaccinate. For studies 2 and 3, beliefs against vaccination, experimental message condition and sex of the parent were controlled for in the model to account for the effects observed in the primary analysis. Self-efficacy, response efficacy, perceived severity, HPV anxiety and subjective norms were entered into the model as potential determinants of intentions to vaccinate.
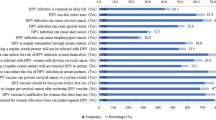
Study 1
The model was significant: F(8, 262) = 32.04 and p < .001. Theoretical determinants accounted for 50 % of the variance in HPV vaccination intentions. Independent theoretical determinants of college-aged women’s intentions to be vaccinated against HPV included response efficacy, self-efficacy, perceived vulnerability to HPV and subjective norms (Table 2). Perceived severity of HPV was not an independent determinant of HPV vaccination intentions (p > .05).
Study 2
The model was significant: F(7, 218) = 34.22 and p < .001. Theoretical determinants accounted for 56 % of the variance in the parent’s HPV vaccination intentions. Independent theoretical determinants of the parents’ intentions to have their daughter vaccinated against HPV included response efficacy, self-efficacy and subjective norms (Table 2). Perceived severity of HPV and perceived anxiety of a daughter contracting HPV were not independent determinants of HPV vaccination intentions (p > .05).
Study 3
The model was significant: F(8, 120) = 10.82 and p < .001. Theoretical determinants accounted for 42 % of the variance in the parent’s HPV vaccination intentions. Independent theoretical determinants of the parents’ intentions to have their son vaccinated against HPV included response efficacy, anxiety about their son contracting HPV and subjective norms (Table 2). Perceived severity of HPV and self-efficacy to have their son vaccinated against HPV were not independent determinants of HPV vaccination intentions (p > .05).
Discussion
The purpose of the present study was to investigate the determinants of HPV vaccination among the three Canadian target groups that have differing levels of access to the HPV vaccine: college-aged women, parents of daughters and parents of sons. Results of the three independent studies revealed that some theoretical constructs are determinants of HPV vaccination among all the three target groups while other constructs are only determinants among certain target groups. Our hypotheses regarding response efficacy, subjective norms and perceived severity were confirmed. Response efficacy of the HPV vaccine and the approval of important others such as doctors were found to be important determinants of HPV vaccination intentions among all the three target groups. Perceived severity of HPV was not a determinant of HPV vaccination intentions among any of the three target groups. Our hypotheses regarding self-efficacy and perceived vulnerability were only partially confirmed. Self-efficacy was found to be a determinant of vaccination intentions among college-aged women and parents of daughters whereas perceived vulnerability, operationalized as HPV anxiety for the studies of parents, was only found to be a determinant of vaccination intentions among college-aged women and parents of sons. These findings provide insight into the potential cognitive variables that could be used to target messages within an HPV vaccination campaign. Specifically, results could be used to ensure that the content of the messages addresses the determinants of a particular target groups’ vaccination intentions.
In general, our findings indicate that the determinants of HPV vaccination within Canada may be similar to those reported among samples of American women and parents. Consistent with the review of theoretical determinants conducted by Brewer and colleagues, we found that across all the three groups, response efficacy and subjective norms predicted vaccination intentions but perceived severity did not. While there were many consistencies between our study and Brewer and colleagues review, our findings contribute the field by highlighting differences in vaccination determinants between the three audiences that had not been reported or explored previously.
The variation in determinants between target groups observed in the current study may be indicative of the context in which each target group makes a vaccination decision. The finding that self-efficacy was not a determinant of vaccination among parents of sons may be attributed to the novelty and recent release of the HPV vaccine for boys at the time the study was conducted. Parents of sons may have been unsure of how a vaccination programme for their sons would be implemented and what steps they would need to be taken to vaccinate. Furthermore, parents of sons would not have had friends or counterparts that had their son previously vaccinated. Thus, modelling behaviours, a key source of self-efficacy, would not be available to parents of sons to draw upon when making a vaccination decision. In contrast, parents of daughters and college-aged women may be aware of the steps that need to be taken to be vaccinated and likely have friends that have vaccinated themselves or their daughters. The finding that indicators of perceived vulnerability to HPV did not predict parents’ intentions to have their daughter vaccinated but did predict intentions among parents of sons and college-aged women may be the result of parents’ inability to accurately assess their daughter’s vulnerability to HPV. Compared to parents of sons, parents of daughters may be less willing to consider their daughters becoming sexually active in the future. Along these lines, they may not be able to accurately report how they feel about their daughter getting HPV because they do not see this as a possibility. Conversely, parents of sons and college-aged women may have more concrete opinions of their personal or child’s vulnerability to HPV.
Our findings indicating that the majority of theoretical constructs are determinants of HPV vaccination among all three target groups while a few constructs are only determinants among certain target groups reflect the need for different types of messages about the HPV vaccine. There is a potential to use both mass media messages about the HPV vaccine that are delivered to the general public and targeted messages that are delivered to specific target groups. In particular, messages that are delivered to all target groups should emphasise the safety and effectiveness of the HPV vaccine and positive recommendations for vaccination from important others rather than focusing on the severity of the virus itself. Conversely, some messages may need to be tailored to specific audience. Messages for college-aged women and parents of daughters should specifically aim to increase recipients’ confidence in their ability to vaccinate. For example, these messages could highlight the ease of vaccination. Furthermore, messages for college-aged women and parents of sons should highlight the likelihood of an HPV infection.
While the results of these three studies provide insight into the determinants of HPV vaccination within a Canadian context, limitations of these studies must be addressed. First, neither the theory of planned behaviour nor the protection motivation theory was measured in their entirety. Future research should consider measuring identical models that contain all variables from both theoretical approaches. Second, we only assessed the intentions to vaccinate and not vaccination behaviour. Third, we did not assess whether participants’ thoughts about future transmission of HPV to potential partners affected the intention to vaccinate. Given that Olshen and colleagues have found that parents’ consideration of their son’s likelihood of transmitting HPV to a future partner affects their acceptance of the HPV vaccine [17], researchers should consider this determinant of vaccination among varying target groups. Fourth, in the study of college women, we only assessed vulnerability to the proximal outcomes of HPV. We did not assess vulnerability to more distal outcomes such as cervical cancer. Examining vulnerability to both proximal and distal outcomes might have strengthened the vulnerability–intentions relationship. Finally, since the vaccination for young boys was still relatively novel at the time of this study, the determinants of HPV vaccination among parents of sons may change as HPV vaccination for young boys becomes mainstream. Therefore, it would be valuable for future research to continue to track vaccination determinants, particularly among parents of sons.
Despite the limitations, this paper is the first to consider HPV vaccination among the three target groups within a Canadian context. This comparison of vaccination intention determinants is further strengthened by the similar measures and methodologies used within the three studies. The findings from these comparisons have important implications for understanding key messages that could be adopted in future Canadian vaccination campaigns and programmes and for tailoring HPV vaccine interventions to specific audiences.
References
Abhyankar P, O’Connor DB, Lawton R (2008) The role of message framing in promoting MMR vaccination: evidence of a loss-frame advantage. Psychol Health Med 13(1):1–16
Ajzen I (1988) Attitudes, personality and behavior. Open University Press, Milton Keynes, pp 179–211
Ajzen I (2002) Constructing a TPB questionnaire: conceptual and methodological considerations. http://people.umass.edu/aizen/pdf/tpb.measurement.pdf. September 2009
Becker MH (1974) The health belief model and personal health behavior. Heal Educ Monogr 2:324–508
Brewer NT, Fazekas KI (2007) Determinants of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med 45(2–3):107–114
Caskey R, Lindau ST, Alexander GC (2009) Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey. J Adolesc Health Off Publ Soc Adolesc Med 45(5):453–462. doi:10.1016/j.jadohealth.2009.04.021
Courneya KS, Hellsten LM (2001) Cancer prevention as a source of exercise motivation: an experimental test using protection motivation theory. Psychol Health Med 6(1):59–64
Gainforth HL, Latimer A (2011) Risky business: risk information and the moderating effect of message frame and past behaviour on women’s perceptions of the human papillomavirus vaccine. J Health Psychol. doi:10.1177/1359105311431173
Graveland B (2009) HPV vaccine tough sell in parts of Canada, The Toronto Star. Accessed 2 March 2009
Gulli K (2007) Our girls are not guinea pigs. Is an upcoming mass inoculation of a generation unnecessary and potentially dangerous? Macleans
Kliewer EV, Demers AA, Brisson M, Severini A, Lotocki R, Elias B, Hammond G, Wurtak G, Manitoba HPV Research Group (2010) The Manitoba human papillomavirus vaccine surveillance and evaluation system. Health Rep 21(3):37–42
Lippman A, Melynchuck R, Shimmin C, Boscoe M (2007) Human papillomavirus, vaccines and women’s health: questions and cautions 177(5):484–487
Merck (2010) Consumer Information: gardasil. Quebec. Merck Frost: Canada
Neuwirth K, Dunwoody S, Griffin R (2000) Protection motivation and risk communication. Risk Anal 20(5):721–734
Nunally J (1978) Psychometric theory, 2nd edn. McGraw-Hill, New York
Ogilvie G, Anderson M, Marra F, MCNeil S, Pielak K, Dawar M, McIvor M et al (2010) A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med 7(5):1–10
Olshen E, Woods ER, Austin SB, Luskin M, Bauchner H (2005) Parental acceptance of the human papillomavirus vaccine. J Adolesc Heal 37(3):248–251
Rogers RW (1975) A protection motivation theory of fear appeals and attitude change. J Psychol 91(1):93
Acknowledgments
The authors would like to thank the Social Science and Humanities Research Council of Canada (SSHRC) for funding this research.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Gainforth, H.L., Cao, W. & Latimer-Cheung, A.E. Determinants of Human Papillomavirus (HPV) Vaccination Intent Among Three Canadian Target Groups. J Canc Educ 27, 717–724 (2012). https://doi.org/10.1007/s13187-012-0389-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-012-0389-1