Abstract
Obesity is a risk factor for vascular endothelial cell dysfunction characterized by low-grade, chronic inflammation. Increased levels of arginase I and concomitant decreases in l-arginine bioavailability are known to play a role in the pathogenesis of vascular endothelial cell dysfunction. In the present study, we focused on changes in the systemic expression of arginase I as well as l-arginine metabolism in the pre-disease state of early obesity prior to the onset of atherosclerosis. C57BL/6 mice were fed a control diet (CD; 10% fat) or high-fat diet (HFD; 60% fat) for 8 weeks. The mRNA expression of arginase I in the liver, adipose tissue, aorta, and muscle; protein expression of arginase I in the liver and plasma; and systemic levels of l-arginine bioavailability and NO2 − were assessed. HFD-fed mice showed early obesity without severe disease symptoms. Arginase I mRNA and protein expression levels in the liver were significantly higher in HFD-fed obese mice than in CD-fed mice. Arginase I levels were slightly increased, whereas l-arginine levels were significantly reduced, and these changes were followed by reductions in NO2 − levels. Furthermore, hepatic arginase I levels positively correlated with plasma arginase I levels and negatively correlated with l-arginine bioavailability in plasma. These results suggested that increases in the expression of hepatic arginase I and reductions in plasma l-arginine and NO2 − levels might lead to vascular endothelial dysfunction in the pre-disease state of early obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence and prevalence of obesity have increased worldwide in recent decades and reached epidemic proportions [2, 13]. The development of obesity is closely associated with additional metabolic complications, including insulin resistance, type 2 diabetes, cardiovascular disease, fatty liver disease, airway disease, and some cancers [8, 10]. Therefore, obesity and its related disorders are a global health issue, and their effective prevention is urgently needed.
l-Arginine (Arg) metabolism is important in normal homeostasis and is altered by various diseases. Arg is utilized by arginase and nitric oxide (NO) synthase (NOS) [16, 22, 40]. Arginase metabolizes the hydrolysis of Arg into l-ornithine (Orn) and urea and consists of two isoforms. Arginase I is localized in the cytoplasm and mainly expressed in the liver, but is present at lower levels in various extrahepatic organs. Arginase II is localized in mitochondria and expressed at low levels in extrahepatic tissues and cells [4, 16]. NOS converts Arg to NO and l-citrulline (Cit) [16]. Previous studies reported that arginase I levels in serum/plasma and lung tissue were elevated in a murine asthmatic model [25, 36, 41] and asthmatic patients [21, 28]. Furthermore, the inhibition of arginase increased the production of NO in asthmatic lungs and ameliorated allergic airway inflammation [26, 35]. Animals with obesity and its related metabolic disorders, including diabetes, atherosclerosis, and hypertension, were found to have increased levels of arginase I, and these symptoms were ameliorated by the inhibition of arginase [5, 6, 9, 14, 19, 34]. Decreased NO production has been implicated in the pathogenesis of these disorders [16, 18, 38]. Therefore, increased levels of arginase I may decrease NO production due to competitive consumption of Arg between arginase I and NOS and may also promote the pathogenesis of vascular endothelial dysfunction.
Our population studies on healthy Japanese individuals revealed that serum arginase I was associated with inflammation and oxidative stress [27, 29, 30]. Based on the negative independent association of serum levels of arginase I with serum levels of Arg in a healthy population [29, 30], serum levels of arginase I have been suggested to regulate Arg and tissue NO generation in pre-disease and disease states. Therefore, arginase I may not only be a biomarker for the early prediction of vascular endothelial dysfunction but also a target protein for the prevention of vascular endothelial dysfunction-related diseases. However, the organ or cell contributing to the increase in arginase I levels in the circulation has not yet been identified.
Obesity and its related disorders are characterized by low-grade, chronic inflammation [8, 10]. Obesity is related to the onset and development of fatty liver, leading to the more severe inflammatory state of non-alcoholic steatohepatitis [8] and liver cancer [1]. Since arginase I is mainly expressed in the liver [4, 18] and induced by inflammatory factors and its related pathways [23, 31, 32], early obesity may induce the upregulation of arginase I in the liver, which contributes to systemic changes in arginase and Arg metabolites.
High-fat diet (HFD) feeding is widely used in rodents to induce obesity and its related metabolic disorders, which resemble metabolic syndrome in humans [3, 12, 24]. In the present study, using HFD-fed obese mice, we investigated alterations in the systemic expression of arginase and Arg metabolism in the pre-disease state of early obesity prior to the onset of vascular endothelial disease.
Materials and methods
Animals
Three-week-old male C57BL/6 mice were obtained from Charles River Laboratories Japan (Yokohama, Japan). They were acclimatized for 1 week before experiments. The care and handling of animals were in accordance with the Guidelines for the Care and Use of Laboratory Animals at the Shikata Campus of Okayama University. This animal study was approved by the Okayama University Institutional Animal Care and Use Committee (OKU-2014322).
Experimental design
After acclimation for 1 week, mice were fed either a control diet (CD; 10% fat, D12450B, Research Diets Inc., New Brunswick, NJ, USA, CD group) or high-fat diet (HFD; 60% fat, D12492, Research Diets Inc., HFD group) for 8 weeks. Body weight and food intake were measured twice a week. Blood glucose levels were measured using the Glutest Neo Sensor (Sanwa Kagaku, Nagoya, Japan). After 8 weeks, all mice were killed by exsanguination under anesthesia with ketamine and xylazine. Blood was collected from the inferior vena cava and immediately centrifuged, and separated plasma was stored at − 80 °C. After the collection of blood, the liver, adipose tissue, aorta, and muscle were harvested. A portion of liver tissue was fixed in 10% neutral phosphate-buffered formalin for histological examinations. Other parts of the liver and other tissue samples were rapidly frozen using liquid nitrogen and stored at − 80 °C for further analyses.
Histological evaluation
Fixed liver tissues were embedded in paraffin. Liver sections were sliced and stained with hematoxylin and eosin and microscopically evaluated for hepatic steatosis according to a scoring system described previously by Kleiner et al. [15]. Sections were observed under an Olympus IX70 light inverted microscope (Olympus, Tokyo, Japan).
RNA extraction and real-time polymerase chain reaction
Total RNA from the liver, adipose tissue, aorta, and muscle was extracted with ISOGEN (Nippon Gene, Tokyo, Japan). Complementary DNA (cDNA) was reverse-transcribed from total RNA using the PrimeScript 1st strand cDNA Synthesis Kit (Takara Bio Inc., Shiga, Japan), according to the manufacturer’s instructions. cDNA was subjected to quantitative real-time polymerase chain reaction (PCR) using SYBR Premix Ex Taq (Tli RNaseH Plus, Takara Bio Inc.) with ROX Reference Dye on the StepOnePlus Real-Time PCR System (Applied Biosystems, Foster City, CA, USA). The following primers were used: Arg1, forward 5′-CTCCAAGCCAAAGTCCTTAGAG-3′ and reverse 5′-AGGAGCTGTCATTAGGGACATC-3′; Arg2, forward 5′-TCCTCCACGGGCAAATTCC-3′ and reverse 5′-GCTGGACCATATTCCACTCCTA-3′; and Gapdh, forward 5′-AGGTCGGTGTGAACGGATTTG-3′ and reverse 5′-TGTAGACCATGTAGTTGAGGTCA-3′. Relative mRNA expression levels were calculated using the comparative Ct (ΔΔCt) method [17], with the Gapdh gene as an internal control. Data are shown as relative expression.
Western blot analysis
A Western blot analysis was performed as previously described [26, 35, 41]. Liver tissue was homogenized in a buffer containing 20 mM Tris-HCl, pH 7.5, 150 mM NaCl, and complete protease inhibitor mixture tablets (Roche, Mannheim, Germany) and then centrifuged. Protein concentrations in the supernatant were measured using a BCA protein assay reagent kit (Pierce Biotechnology, Rockford, IL, USA). Equal amounts of protein from the liver or equal volumes of plasma were subjected to 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and proteins were subsequently transferred onto polyvinylidene fluoride membranes (Millipore, Bedford, MA, USA). After blocking, these membranes were incubated with antibodies to arginase I (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA), arginase II (Santa Cruz Biotechnology Inc.), or β-actin (Abcam, Cambridge, UK) as an internal control in the liver. Corresponding horseradish peroxidase-conjugated secondary antibodies (DakoCytomation Inc., Carpinteria, CA, USA) were used as the second antibody. Membranes were incubated with an enhanced chemiluminescence Western blot detection system (Perkin-Elmer, Boston, MA, USA), and bands were visualized using an MXJB-PLUS medical X-ray film (Kodak, Rochester, NY, USA). Each band was quantified using ImageJ software (National Institutes of Health, USA). The expression level of arginase I and arginase II in liver tissue was normalized to that of β-actin. Data are shown as relative expression.
High-performance liquid chromatography analysis
The plasma concentrations of amino acids such as Arg, Cit, and Orn were quantified using high-performance liquid chromatography (HPLC) with fluorescence detection, as previously described [41]. In brief, 10 μl of plasma was mixed with 50 μl of 1.5 M HClO4. After 2 min, 1 ml of H2O, 25 μl of 2 M K2CO3, and 125 μl of 100 μM monomethyl-l-arginine, an internal standard, were added. This mixture was vortexed and centrifuged. The supernatant was mixed with an equal amount of derivatization reagent (1 mg/ml ortho-phthalaldehyde, 2% methanol, and 0.1% 3-mercaptopropionic acid in 200 mM borate buffer, pH 8.5) and injected into a HPLC system consisting of a solvent delivery system and fluorometer (HITACHI Ltd., Tokyo, Japan). Ascentis® C18 (15 cm × 4.6 mm, 3 μm; Supelco Inc., Bellefonte, PA, USA) and Ascentis® C18 Supelguard™ (2 cm × 4.0 mm, 3 μm; Supelco Inc.) were used as the analytical column and guard column, respectively. Separation was performed by mobile phase A (0.1 M sodium acetate, pH 7.2, containing 9% methanol and 0.5% tetrahydrofuran) and mobile phase B (100% methanol). Fluorescence excitation and emission wavelengths were 340 and 455 nm, respectively.
Measurement of NO
In order to estimate NO production in plasma, the concentration of nitrite (NO2 −) was measured by the ozone-chemiluminescence method using an NO analyzer (Model-280i NOA with a Purge Vessel; Sievers, Boulder, CO, USA), as previously described [26, 41].
Statistical analysis
All data are given as the mean ± standard error of the mean (SEM). Comparisons between CD and HFD groups were performed using an unpaired Student t test or Mann-Whitney test after analyzing Gaussian distribution with the Shapiro-Wilk normality test or Kolmogorov-Smirnov test. Correlation analyses were assessed using Pearson’s correlation coefficients. Differences were considered to be significant when P < 0.05. All analyses were performed with GraphPad Prism 6 for Windows (GraphPad Software, Inc., San Diego, CA, USA).
Results
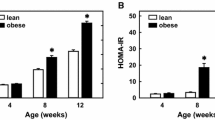
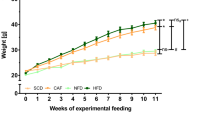
Characteristics of early obese mice induced by HFD
Body weights after 8 weeks of feeding were significantly higher in the HFD group (31.0 ± 0.9, n = 8) than in the CD group (25.4 ± 0.4, n = 7) (P < 0.001, Fig. 1a). The average energy of food intake (Kcal/week/mouse) was significantly higher in the HFD group (79.9 ± 1.7, n = 8) than in the CD group (63.1 ± 1.2, n = 7). However, no significant differences were observed in blood glucose levels between the CD group (177.7 ± 12.3, n = 7) and HFD group (173.0 ± 10.4, n = 8) (Fig. 1c). We assessed histological changes in the liver. Pathologically, fat deposition in the liver was approximately 5% in the HFD group, which indicates mild steatosis without microvascular steatosis and ballooning degeneration, but was negligible in the CD group (Fig. 1d). These results suggest that HFD causes early and mild, but not severe obesity in the pre-disease state prior to the onset of metabolic disorders.
Characteristics of HFD-fed early obese mice. Body weight (a), average calorie intake (b), and blood glucose levels (c) in CD- and HFD-fed mice. ***P < 0.001 vs. CD-fed mice (n = 7). d Representative images of hematoxylin and eosin-stained liver tissue from CD- and HFD-fed mice. All analyses were performed after 8 weeks of feeding. Bars indicate 200 μm
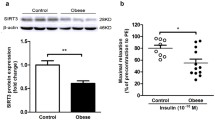
The mRNA and protein expression of arginase I and arginase II in the liver of HFD-fed early obese mice
We examined the mRNA expression of arginase isoforms in the liver by real-time PCR. The mRNA expression of arginase I was significantly stronger in the HFD group (relative values, 1.38 ± 0.09, n = 7) than in the CD group (n = 6) (P < 0.05, Fig. 2a). No significant differences were observed in the mRNA expression of arginase IΙ between the HFD group (relative values, 0.81 ± 0.07, n = 7) and CD group (n = 7) (Fig. 2b). Furthermore, we confirmed protein levels using a Western blot analysis and found that the protein expression of arginase I and arginase II in the liver was significantly stronger in the HFD group (relative value of arginase I, 1.86 ± 0.34, n = 8; that of arginase II, 1.70 ± 0.12, n = 8) than in the CD group (n = 7) (P < 0.05, Fig. 2c). These results indicate that early obesity induces the expression of arginase I in the liver.
Arginase I mRNA and protein expression levels are increased in the liver of HFD-fed early obese mice. Quantification after normalization to Gapdh in real-time PCR for Arg1 (a) and Arg2 mRNA (b) in the liver of CD and HFD-fed mice. Representative images and quantification after normalization to β-actin in a Western blot analysis for arginase I (c) and arginase II (d) protein levels in the liver of CD- and HFD-fed mice. *P < 0.05 vs. CD-fed mice (n = 7)
The mRNA expression of arginase I and arginase II in the adipose tissue, aorta, and muscle of HFD-fed early obese mice
We then measured the mRNA expression of the arginase isoforms in adipose, aortic, and muscle tissue by real-time PCR (Fig. 3a–f). No significant differences were noted in the mRNA expression of arginase I in the aorta between the HFD group (relative value of arginase I, 1.63 ± 0.99, n = 5; that of arginase II, 3.12 ± 1.16, n = 5) and CD group (n = 6) or in the muscle between the HFD group (relative value of arginase I, 0.29 ± 0.16, n = 5; that of arginase II, 1.02 ± 0.69, n = 5) and CD group (n = 5). However, although the mRNA expression of arginase I in adipose tissue was not significantly different between the HFD group (relative value of arginase I, 1.79 ± 0.47, n = 6) and CD group (n = 6), a significant difference was observed for the mRNA expression of arginase II between the HFD group (relative value of arginase II, 1.49 ± 0.12, n = 5) and CD group (n = 5).
Arginase I mRNA expression levels remain unchanged in adipose tissue, the aorta, and muscle of HFD-fed early obese mice. Quantification after normalization to Gapdh in real-time PCR for Arg1 (a–c) and Arg2 mRNA (d–f) in adipose tissue (a, d), the aorta (b, e), and muscle (c, f) of CD- and HFD-fed mice (n = 5–7)
The protein expression of arginase I in the plasma of HFD-fed early obese mice
We measured protein levels of arginase I in plasma using a Western blot analysis. Plasma arginase I levels were slightly higher in the HFD group (relative value of arginase I, 1.44 ± 0.19, n = 7) than in the CD group (n = 7) (P = 0.0870, Fig. 4a). We also assessed the relationship for arginase I between the liver and plasma. Pearson’s correlation analysis showed that the expression of arginase I in the liver positively correlated with that in the plasma (P = 0.0197, r = 0.6131, Fig. 4b). These results suggest that an elevated systemic level of arginase I is related to the obesity-induced increased expression of arginase I in the liver.
Plasma arginase I levels slightly increased and correlated with hepatic arginase I levels in HFD-fed early obese mice. a Representative images and quantification of a Western blot analysis for arginase I protein levels in the plasma of CD- and HFD-fed mice (n = 7). b Correlation analysis for arginase I between the plasma and liver (n = 14, 7 in each group)
Systemic Arg metabolism in HFD-fed early obese mice
We measured the plasma concentrations of Arg metabolites using HPLC. The concentrations of Arg and Cit were significantly lower in the HFD group (38.4 ± 1.4, n = 7, and 20.9 ± 0.9, n = 7, respectively) than in the CD group (63.6 ± 3.1, n = 7, and 35.3 ± 1.9, n = 7, respectively) (Fig. 5a, b). No significant difference was observed in the concentration of Orn between the HFD (38.0 ± 3.4, n = 7) and CD groups (35.9 ± 4.7, n = 7) (Fig. 5c). The ratio of Orn/Cit was significantly higher in the HFD group (1.8 ± 0.2, n = 7) than in the CD group (1.0 ± 0.2, n = 7) (Fig. 5d), suggesting the metabolism of Arg by arginase than by NOS. Furthermore, the Arg bioavailability ratio [Arg/(Orn + Cit)] [20, 37] was significantly lower in the HFD group (0.7 ± 0.1, n = 7) than in the CD group (0.9 ± 0.1, n = 7) (Fig. 5e). We also measured the plasma concentration of NO2 −, a metabolite of NO. The plasma concentration of NO2 − was significantly lower in the HFD group (176.7 ± 31.0, n = 7) than in the CD group (282.0 ± 16.1, n = 7) (Fig. 5f). These results suggest systemic changes in Arg metabolism including decreases in Arg bioavailability and NO production in the early stage of obesity.
Relationship between hepatic arginase I and plasma Arg metabolites
Pearson’s correlation coefficients between hepatic arginase I protein levels in the liver or plasma and Arg metabolites in the plasma are shown in Table 1. Hepatic arginase I levels positively correlated with the Orn/Cit ratio and negatively correlated with Arg and Cit levels as well as the Arg bioavailability ratio in plasma. A strong correlation was observed between hepatic arginase I levels and Arg bioavailability. However, no correlations were found between arginase I levels and Arg metabolites in plasma. These results suggest that arginase I expression in the liver contributes to systemic changes in Arg metabolism in early obesity.
Discussion
The results of the present study demonstrate that the expression of arginase I increased in the livers of early obese, pre-diseased, HFD-fed mice. We also showed the induction of hepatic arginase I in HFD-fed obese mice, which was followed by a decrease in Arg bioavailability and NO production. Furthermore, hepatic arginase I expression was associated with arginase I expression, Arg, Cit, the Orn/Cit ratio, and the Arg bioavailability ratio in plasma.
HFD-fed mice are a useful model for obesity and its related metabolic diseases. However, the obesity-induced onset or offset of metabolic syndrome varies depending on the duration of feeding, the fat content in the diet, the composition of dietary fat, and the rodent strain [3, 12, 24]. Since mice after 8 weeks of HFD feeding showed mild obesity without overt symptoms of metabolic disorders, such as hyperglycemia and severe fatty liver, HFD feeding in this study may be the pre-disease state of early obesity, prior to the onset of vascular endothelial dysfunction.
The results of the present study revealed increases in the expression of arginase I in the liver without obvious steatosis in early obesity. In contrast, arginase I mRNA levels remained unchanged in adipose tissue, the aorta, and muscle. Based on increases in arginase I levels after the onset of metabolic diseases [5, 6, 8, 14, 19, 34], arginase I in the liver may be more susceptible to early obesity-induced changes than that in other tissues. Furthermore, plasma arginase I levels slightly increase in early obesity. Previous studies reported that arginase is released from injured livers into the circulation [11, 33]. The positive correlation for arginase I levels between the liver and plasma in our HFD-fed mice indicates that increases in arginase I levels in the liver during pre-disease obesity partly contribute to elevated arginase I levels in the circulation.
Increasing evidence shows a reduction in Arg bioavailability in patients [30, 37, 39] and animals with metabolic disorders [6, 14]. Additionally, decreased NO production is a common feature of vascular endothelial cell dysfunction and the subsequent onset of atherosclerosis [14, 16, 38]. We found that systemic Arg bioavailability and NO production decreased even in the early pre-disease state of obesity. Our results suggest that elevated arginase I levels in the liver and plasma are responsible for these systemic changes.
Hepatic arginase I levels correlated with systemic levels of Arg and Cit as well as the Orn/Cit and Arg bioavailability ratios. These correlations may be explained by the release of arginase I from the liver into the circulation. Moreover, changes in Arg metabolites by arginase I within the liver and their release into the circulation may contribute to systemic changes in Arg metabolites. Systemic changes in Arg metabolism may predict the onset and development of subsequent obesity-related liver diseases. A correlation was not observed between arginase I and Arg metabolites in plasma in the present study; however, plasma levels of arginase I were slightly elevated. Although the reason for this currently remains unclear, arginase I levels in plasma may reflect differences in its release from the liver depending on the degree of obesity and its related inflammation.
The results of the present study showing increased levels of arginase and decreased Arg bioavailability in the pre-diseased state of early obesity support the negative relationship between arginase and Arg in a healthy Japanese population [30]. Therefore, our results indicate that systemic changes in Arg metabolism including those in arginase I and their relationship with Arg bioavailability are early signs of the onset and development of subsequent diseases. Although further studies are needed in order to assess and compare systemic changes in Arg metabolism in pre-obesity (prior to increases in body weight) and disease states after the onset and development of metabolic diseases, in addition to early obesity of the pre-disease state, monitoring these systemic changes in Arg metabolism may be effective for the early diagnosis and prevention of obesity-associated metabolic disorders.
The mechanisms underlying the upregulation of arginase I in the liver induced by HFD feeding are unclear. The expression of arginase I is inducible by various factors, including interleukin (IL)-4, IL-10, IL-13, tumor necrosis factor-α, reactive oxygen species, and glucose. The intracellular signaling pathways responsible for the induction of arginase I are the protein kinase C/RhoA/Pho kinase pathway and mitogen-activated protein kinase. This upregulation of arginase I is controlled by transcription factors, including signal transducer and activator of transcription-6, CAAT-enhancer binding protein, purine box factor 1, and peroxisome proliferator-activated receptor [23, 31, 32]. Furthermore, our previous population studies revealed a relationship between arginase I expression with increases in oxidative stress [27, 29, 30]. Previous studies showed that obesity is related to increased oxidative stress [7, 10]. Therefore, our results demonstrated that the upregulation of arginase I may be due to mild obesity-related inflammation in the liver induced by HFD; however, further experiments are needed in order to elucidate the mechanisms by which obesity induces the expression of arginase I in the liver in more detail.
In conclusion, the present study proposes that HFD feeding-induced early obesity may lead to the upregulation of arginase I expression in the liver, and this may be related to systemic changes in Arg metabolism. Although further studies are needed in order to clarify the contribution of arginase I and Arg metabolism to obesity and its related metabolic diseases, arginase I and Arg metabolites have potential as biomarkers for the early diagnosis and prevention of obesity and its related metabolic disorders.
References
Aleksanrrova K, Stelmach-Mardas M, Schlesinger S (2016) Obesity and liver cancer. Recent Results Cancer Res 208:177–198
Bastien M, Poirier P, Lemieux I, Despres JP (2014) Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 56:369–381
Buettner R, Scholmerich J, Bollheimer LC (2007) High-fat diets: modeling the metabolic disorders of human obesity in rodents. Obesity 15:798–808
Caldwell RB, Toque HA, Narayanan SP, Caldwell RW (2015) Arginase: an old enzyme with new tricks. Trends Pharmacol Sci 36:395–405
Chung JH, Moon J, Lee YS, Chung HK, Lee SM, Shin MJ (2014) Arginase inhibition restores endothelial function in diet-induced obesity. Biochem Biophys Res Commun 451:179–183
Erdely A, Kepka-Lenhart D, Salmen-Muniz R, Chapman R, Hulderman T, Kashon M, Simeonova PP, Morris SM Jr (2010) Arginase activities and global arginine bioavailability in wild-type and ApoE-deficient mice: responses to high fat and high cholesterol diets. PLoS One 5:e15253
Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761
Gregor MF, Hotamisligil GS (2011) Inflammatory mechanisms in obesity. Annu Rev Immunol 29:415–445
Gronros J, Jung C, Lundberg JO, Cerrato R, Ostenson CG, Pernow J (2011) Arginase inhibition restores in vivo coronary microvascular function in type 2 diabetic rats. Am J Physiol Heart Circ Physiol 300:H1174–H1181
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Ikemoto M, Tsunekawa S, Toda Y, Totani M (2001) Liver-type arginase is a highly sensitive marker for hepatocellular damage in rats. Clin Chem 47:946–948
Ito M, Suzuki J, Tsujioka S, Sasaki M, Gomori A, Shirakura T, Hirose H, Ito M, Ishihara A, Iwaasa H, Kanatani A (2007) Longitudinal analysis of murine steatohepatitis model induced by chronic exposure to high-fat diet. Hepatol Res 37:50–57
Johnson AR, Milner JJ, Makowski L (2012) The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev 249:218–238
Johnson FK, Peyton KJ, Liu XM, Azam MA, Shebib AR, Johnson RA, Durante W (2015) Arginase promotes endothelial dysfunction and hypertension in obese rats. Obesity 23:383–390
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrel LD, Liu YC, Torbenson MS, Unalp-Arida A, Yeh M, McCullough AJ, Sanyal AJ (2005) Design and vasodilation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41:1313–1324
Litvinova L, Atochin DN, Fattakhov N, Vasilenko M, Zatolokin P, Kirienkova E (2015) Nitric oxide and mitochondria in metabolic syndrome. Front Physiol 6:20
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and 2−∆∆CT method. Methods 25:402–408
Luiking YC, Ten Have GA, Wolfe RR, Deutz NE (2012) Arginine de novo and nitric oxide production in disease states. Am J Physiol Endocrinol Metab 303:E1177–E1189
Moon J, Do HJ, Cho Y, Shin MJ (2014) Arginase inhibition ameliorates hepatic metabolic abnormalities in obese mice. PLoS One 9:e103048
Morris CR, Kato GJ, Poljakovic M, Wang X, Blackwelder WC, Sachdev V, Hazen SL, Vichinsky EP, Morris SM Jr, Gladwin MT (2005) Dysregulated arginine metabolism, hemolysis-associated pulmonary hypertension, and mortality in sickle cell disease. JAMA 294:81–90
Morris CR, Poljakovic M, Lavrisha L, Machado L, Kuypers FA, Morris SM Jr (2004) Decreased arginine bioavailability and increased serum arginase activity in asthma. Am J Respir Crit Care Med 170:148–153
Morris SM Jr (2007) Arginine metabolism: boundaries of our knowledge. J Nutr 137:1602S–1609S
Munder M (2009) Arginase: an emerging key player in the mammalian immune system. Br J Pharmacol 158:638–651
Nakamura A, Terauchi Y (2013) Lessons from mouse models of high-fat diet-induced NAFLD. Int J Mol Sci 14:21240–21257
North ML, Khanna N, Marsden PA, Grasemann H, Scott JA (2009) Functionally important role for arginase 1 in the airway hyperresponsiveness of asthma. Am J Physiol Lung Cell Mol Physiol 296:L911–L920
Ogino K, Kubo M, Takahashi H, Zhang R, Zou Y, Fujikura Y (2013) Anti-inflammatory effect of arginase inhibitor and corticosteroid on airway allergic reactions in a dermatophogoides farinae-induced NC/Nga mouse model. Inflammation 36:141–151
Ogino K, Murakami I, Wang DH, Tsukiyama Y, Takahashi H, Kubo M, Sakano N, Setiawan H, Bando M, Ohmoto Y (2013) Evaluation of serum arginase I as an oxidative stress biomarker in a healthy Japanese population using a newly established ELISA. Clin Biochem 46:1717–1722
Ogino K, Obase Y, Takahashi N, Shimizu H, Takigawa T, Wang DH, Ouchi K, Oka M (2011) High serum arginase I levels in asthma: its correlation with high-sensitivity C-reactive protein. J Asthma 48:1–7
Ogino K, Takahashi N, Takigawa T, Obase Y, Wang DH (2011) Association of serum arginase I with oxidative stress in a healthy population. Free Radic Res 45:147–155
Ogino K, Wang DH, Kubo M, Obase Y, Setiawan H, Yan F, Takahashi H, Zhang R, Tsukiyama Y, Yoshida J, Zou Y (2014) Association of serum arginase I with L-arginine, 3-nitrotyrosine, and exhaled nitric oxide in healthy Japanese workers. Free Radic Res 48:137–145
Pernow J, Jung C (2013) Arginase as a potential target in the treatment of cardiovascular disease: reversal of arginine steal? Cardiovasc Res 98:334–343
Pourcet B, Pineda-Torra I (2013) Transcriptional regulation of macrophage arginase 1 expression and its role in atherosclerosis. Trends Cardiovasc Med 23:143–152
Reid KM, Tsung A, Kaizu T, Jeyabalan G, Ikeda A, Shao LF, Wu GY, Murase N, Geller DA (2007) Liver I/R injury is improved by the arginase inhibitor, N-omega-hydroxy-nor-L-arginine (nor-NOHA). Am J Physiol-Gastr L 292:G512–G517
Romero MJ, Platt DH, Tawfik HE, Labazi M, El-Remessy AB, Bartoli M, Caldwell RB, Caldwell RW (2008) Diabetes-induced coronary vascular dysfunction involves increased arginase activity. Circ Res 102:95–102
Takahashi N, Ogino K, Takemoto K, Hamanishi S, Wang DH, Takigawa T, Shibamori M, Ishiyama H, Fujikura Y (2010) Direct inhibition of arginase attenuated airway allergic reactions and inflammation in a Dermatophagoides farinae-induced NC/Nga mouse model. Am J Physiol Lung Cell Mol Physiol 299:L17–L24
Takemoto K, Ogino K, Shibamori M, Gondo T, Hitomi Y, Takigawa T, Wang DH, Takaki J, Ichimura H, Fujikura Y, Ishiyama H (2007) Transiently, paralleled upregulation of arginase and nitric oxide synthase and the effect of both enzymes on the pathology of asthma. Am J Physiol Lung Cell Mol Physiol 293:L1419–L1426
Tang WH, Wang Z, Cho L, Brennan DM, Hazen SL (2009) Diminished global arginine bioavailability and increased arginine catabolism as metabolic profile of increased cardiovascular risk. J Am Coll Cardiol 53:2061–2067
Toda N, Okamura T (2013) Obesity impairs vasodilatation and blood flow increase mediated by endothelial nitric oxide: an overview. J Clin Pharmacol 53:1228–1239
Tripolt NJ, Meinitzer A, Eder M, Wascher TC, Pieber TR, Sourij H (2012) Multifactorial risk factor intervention in patients with type 2 diabetes improves arginine bioavailability ratios. Diabet Med 29:e365–e368
Wu G, Bazer FW, Davis TA, Kim SW, Li P, Marc Rhoads J, Carey Satterfield M, Smith SB, Spencer TE, Yin Y (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Zhang R, Kubo M, Murakami I, Setiawan H, Takemoto K, Inoue K, Fujikura Y, Ogino K (2015) l-Arginine administration attenuates airway inflammation by altering l-arginine metabolism in an NC/Nga mouse model of asthma. J Clin Biochem Nutr 56:201–207
Funding
This work was supported in part by JSPS KAKENHI, a Grant-in-Aid for Science Research (C) (No. 15K08775) to MK, and a Grant-in-Aid for Science Research (B) (No. 26293152) to KO.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The care and handling of animals were in accordance with the Guidelines for the Care and Use of Laboratory Animals at the Shikata Campus of Okayama University. This animal study was approved by the Okayama University Institutional Animal Care and Use Committee (OKU-2014322).
Rights and permissions
About this article
Cite this article
Ito, T., Kubo, M., Nagaoka, K. et al. Early obesity leads to increases in hepatic arginase I and related systemic changes in nitric oxide and l-arginine metabolism in mice. J Physiol Biochem 74, 9–16 (2018). https://doi.org/10.1007/s13105-017-0597-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-017-0597-6