Abstract
The role of N-methyl-D-aspartate receptor (NMDA-R) in heart is still unclear. For these ionotropic glutamate receptors is characteristic the necessity of both co-agonists, glutamate and glycine, for their activation, which primarily allows influx of calcium. The aim of the present study was to examine the effects of verapamil, as a calcium channel blocker, alone and its combination with glycine and/or glutamate on cardiac function, coronary flow, and oxidative stress in isolated rat heart or to examine the effects of potential activation of NMDA-R in isolated rat heart. The hearts of male Wistar albino rats were excised and perfused according to Langendorff technique, and cardiodynamic parameters and coronary flow were determined during the administration of verapamil and its combinations with glutamate and/or glycine. The oxidative stress biomarkers, including thiobarbituric acid-reactive substances, nitrites, superoxide anion radical, and hydrogen peroxide, were each determined spectrophotometrically from coronary venous effluent. The greatest decline in parameters of cardiac contractility and systolic pressure was in the group that was treated with verapamil only, while minimal changes were observed in group treated with all three tested substances. Also, the largest changes in coronary flow were in the group treated only with verapamil, and at least in the group that received all three tested substances, as well as the largest increase in oxidative stress parameters. Based on the obtained results, it can be concluded that NMDA-R activation allows sufficient influx of calcium to increase myocardial contractility and systolic pressure, as well as short-term increase of oxidative stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ionotropic glutamate receptor (iGLu-R) family is huge and it consists of three different types of receptors according to their sequence similarities, their electrophysiological properties, and their affinity to selective agonists: N-methyl-D-aspartate receptor (NMDA-R), α-amino-3-hydroxy-5-methyl-4-isoxazolepropionate receptor (AMPA-R), and kainite receptor (KA-R) [31, 50]. The NMDA-R is a protein complex, which may be built of three different subunits: GluN1, GluN2 (A-D), and GluN3 (A-B). NMDA-Rs are tetramer usually composed of two GluN1 and either two GluN2 subunits of the same or various subtype, or combination of GluN2 and GluN3 subunits, which form the channel [51]. Binding of glycine and glutamate is necessary for activation of this channel. Glutamate is released from presynaptic vesicles (concentration of glutamate is about 100 μmol/L) by Ca2+-dependent mechanism that involves N- and P/Q-type voltage-dependent Ca2+ channels [31]. The result of activation of this channel is influx of Ca2+ and Na+ ions and efflux of K+ ion [51]. Elevated intracellular concentration of free Ca2+ leads to depolarization of membrane and activation of Ca2+-sensitive channels [39]. NMDA-R activation in the brain induces Ca2+ overload, production of reactive oxygen species (ROS), and apoptotic cell death [34].
The most explored actions of this receptor are related to the function of the brain. They have a principal role in learning and memory, as well as in corticogenesis, neuronal migration, and synaptogenesis during the brain development. Besides the brain, these receptors are expressed in various non-neuronal cells and tissues such as pancreatic island cells, keratinocytes, and the heart [8]. Some of these GluN subunits were found in rat heart, but their function is still unknown. Presence of GluN1 subunit is proved in the adult heart [15, 26], while GluN2 subunit (type B) is only present in newborn rat heart [46].
Verapamil is a potent calcium channel blocker (CCB); its primary mechanism of action is blockade of L-type calcium channels [10]. Inhibition of these channels prevent excessive Ca2+ influx into cardiomyocytes (negative inotropic effects), as well as smooth muscle cells of the coronary vasculature. The result of this blockade is restriction of intracellular Ca2+ and relaxation of vascular smooth muscle cells. This blockade occurs in cells of the specialized sinoatrial and atrioventricular nodes, also causing its negative chronotropic effects. Verapamil is used in the treatment of hypertension, angina pectoris, and atrial fibrillation [30].
There are some claims that activation of NMDA-R in the heart has great impact at electrical activity of this organ and may play a role in cardiac arrhythmogenesis. Chronic administration of NMDA induces very important cardiac electrophysiological changes and increases a risk for ventricular arrhythmias and mild myocardial interstitial fibrosis [8]. The most common clinical situations where there is a simultaneous activation of NMDA receptors with the use of verapamil were found in patients who have elevated plasma levels of homocysteine and take verapamil, and some authors have investigated the effects of verapamil on experimentally induced hyperhomocysteinemia in humans [23, 42]. Kanani and coauthors in their study have investigated the effects of experimentally increased plasma homocysteine by methionine loading on endothelium, whereby they followed the reactivity of blood vessels during application of verapamil [23]. Similar investigation was done by Raghuveer and coworkers [42].
Knowing the all previously mentioned facts about NMDA receptor co-agonists glutamate and glycine and about potent calcium channel blocker verapamil, it would be of interest to assess their mutual influence on the myocardium and especially coronary circulation.
In that sense, the aim of the present study was to examine the effects of verapamil alone and its combination with glycine and/or glutamate on cardiac function, coronary flow, and oxidative stress in isolated rat heart or to examine the effects of potential activation of NMDA receptors in isolated rat heart.
Material and methods
Isolated rat heart preparation
Sixty male Wistar albino rats (12 rats per experimental group) are used in this study. Each of these rats was 8 weeks old and had a body mass 180–200 g (the rats were obtained from the Military Medical Academy, Belgrade, Serbia). After anesthetizing with ketamine (10 mg/kg) and xylazine (5 mg/kg), the animals were euthanized via cervical dislocation (Schedule 1 of the Animals/Scientific Procedures, Act 1986, UK). After euthanasia, a quick thoracotomy and rapid cardiac arrest by superfusion with ice-cold isotonic saline were performed and the hearts were promptly excised and attached to the Langendorff apparatus (Experimetria Ltd., 1062 Budapest, Hungary) via aortic cannulation. After removing left auricula and through an incision in the left atrium the sensor (transducer BS4 73–0184, Experimetria Ltd., Budapest, Hungary) was placed into the left ventricle for the continuous monitoring of cardiac function. The hearts were retrogradely perfused under a constant perfusion pressure (CPP) of 70 cmH2O with complex Krebs-Henseleit solution composed of the following (in mmol/L): NaCl 118, KCl 4.7, CaCl2·2H2O 2.5, MgSO4·7H2O 1.7, NaHCO3 25, KH2PO4 1.2, glucose 11, pyruvate 2, equilibrated with 95 % O2 plus 5 % CO2 at 37 °C (pH 7.4).
Experimental protocol
The hearts from all experimental groups were undergone to a 25-min stabilization period. During this period, each of the hearts was subjected to short-term occlusion (20 s) followed by simultaneous bolus injections of 5 mmol/l adenosine (60 μl at a flow of 10 ml/min to elicit maximal coronary flow) to test coronary vascular reactivity. If coronary flow (CF) did not increase by 100 % compared with control values, the hearts were disposed of. Coronary flow was determined flowmetrically. When the CF was stabilized (three repeatedly measurements of the same value), samples of coronary effluent were collected (control value), and the experimental protocol was initiated. Hearts were perfused with
-
1.
3 μmol/l verapamil
-
2.
3 μmol/l verapamil + 100 μmol/l glycine
-
3.
3 μmol/l verapamil + 100 μmol/l glutamate
-
4.
3 μmol/l verapamil + 100 μmol/l glycine + 100 μmol/l glutamate
In order to assess the potential role of glycine receptors (GlyR) in regulation of heart homeostasis, we also performed experiments with strychnine (10 μmol/l), which acts as a blocker of these receptors.
Each of the applied substances was administered for 5 min, followed by a wash-out period lasting for 10 min. In the last minute of substance application (effect) and in the last minute of the wash-out period (wash-out), the samples of coronary venous effluent were collected. Using the sensor within the left ventricle, the following parameters of myocardial function were determined:
-
1.
The maximum rate of pressure development in the left ventricle (dp/dt max)
-
2.
The minimum rate of pressure development in the left ventricle (dp/dt min)
-
3.
The systolic left ventricular pressure (SLVP)
-
4.
The diastolic left ventricular pressure (DLVP)
-
5.
The heart rate (HR)
All research procedures were carried out in accordance with European Directive for welfare of laboratory animals N° 86/609/EEC and principles of Good Laboratory Practice (GLP), approved by ethical committee of the Faculty of Medical Sciences, University of Kragujevac, Serbia.
Biochemical assays
The following oxidative stress parameters were determined spectrophotometrically (Shimadzu UV 1800, Japan) using collected samples of the coronary venous effluent:
-
1.
The index of lipid peroxidation, measured as thiobarbituric acid-reactive substances (TBARS)
-
2.
The level of nitrite (NO2 −)
-
3.
The level of the superoxide anion radical (O2 −) and
-
4.
The level of hydrogen peroxide (H2O2)
TBARS determination (index of lipid peroxidation)
The degree of lipid peroxidation in the coronary venous effluent was estimated by measuring TBARS, using 1 % thiobarbituric acid in 0.05 NaOH, which was incubated with the coronary effluent at 100 °C for 15 min and measured at 530 nm. Krebs–Henseleit solution was used as a blank probe [35].
Determination of the nitrite level
Nitric oxide decomposes rapidly to form stable nitrite/nitrate products. The nitrite level (NO2 −) was measured and used as an index of nitric oxide (NO) production, using Griess’s reagent. A total of 0.5 ml of perfusate was precipitated with 200 μl of 30 % sulpho-salicylic acid, vortexed for 30 min, and centrifuged at 3000 x g. Equal volumes of the supernatant and Griess’s reagent, containing 1 % sulphanilamide in 5 % phosphoric acid/0.1 % naphthalene ethylenediamine-dihydrochloride were added and incubated for 10 min in the dark and measured at 543 nm. The nitrite levels were calculated using sodium nitrite as the standard [17].
Determination of the level of the superoxide anion radical
The level of the superoxide anion radical (O2 −) was measured via a nitro blue tetrazolium (NBT) reaction in TRIS buffer with coronary venous effluent, at 530 nm. Krebs–Henseleit solution was used as a blank probe [5].
Determination of the hydrogen peroxide level
The measurement of the level of hydrogen peroxide (H2O2) was based on the oxidation of phenol red by hydrogen peroxide in a reaction catalyzed by horseradish peroxidase (HRPO) [40]. Two hundred microliters of perfusate was precipitated using 800 ml of freshly prepared phenol red solution; 10 μl of (1:20) HRPO (made ex tempore) was subsequently added. For the blank probe, an adequate volume of Krebs–Henseleit solution was used instead of coronary venous effluent. The level of H2O2 was measured at 610 nm.
Drugs
All drugs used in this experimental protocol were provided by Sigma-Aldrich.
Statistical analysis
All values are expressed as mean ± SE. Paired t test, Wilcoxon test for paired samples and Kruskal-Wallis were used in statistical analysis and p values less than 0.05 were considered to be statistically significant.
Results
The effects of verapamil on the cardiodynamic parameters and coronary flow in isolated rat heart
(Fig. 1 and Table 1). The application of verapamil induced significant decrease of dp/dt max (−60.68 %), dp/dt min. (−57.21 %), SLVP (−54.18 %), and HR (−11.62 %) compared with control values. On the other hand, application of verapamil induced significant increase of CF (+32.95 %). Following the wash-out period dp/dt max (+37.22 %), dp/dt min (+38.29 %) and SLVP (+33.63 %) were significantly increased, while CF (−42.07 %) was significantly decreased. HR did not change significantly during wash-out period. The values of DLVP were not changed significantly during the application of verapamil. CF only reached initial values after the wash-out period (−9.12 %), while all the other parameters showed the statistically significant changes between control and wash-out period (dp/dt max: −23.46 %; dp/dt min: −18.92 %; SLVP: −20.55 %; HR: −13.81 %).
The effects of combined application of verapamil and glutamate on the cardiodynamic parameters and coronary flow in isolated rat heart
(Fig. 1 and Table 1). The simultaneous application of verapamil and glutamate induced significant decrease of dp/dt max (−44.66 %), dp/dt min (−47.96 %), SLVP (−34.45 %) and HR (−24.71 %) compared with control conditions. Following the wash-out period dp/dt max (+11.15 %) and SLVP (+10.14 %) were significantly increased, but did not reach the initial values (dp/dt max: -33.51 %; SLVP: -24.31 %). All the other previously mentioned parameters were not changed significantly during the wash-out period, and did not reach the initial values (dp/dt min: -38.21 %; HR: -29.25 %). The value of CF increased (+25.81 %) significantly during the administration of verapamil and glutamate, and after that significantly decreased (−52.11 %) during the wash-out period, but value after wash-out period was significantly lower compared to the control (−26.30 %). The value of DLVP was not significantly changed during the experiment.
The effects of combined application of verapamil and glycine on the cardiodynamic parameters and coronary flow in isolated rat heart
(Fig. 1 and Table 1). The simultaneous application of verapamil and glycin induced significant decrease of dp/dt max (−43.78 %), dp/dt min (−51.49 %) and SLVP (−37.93 %) compared with control conditions. Following the wash-out period all previously mentioned parameters were significantly increased (dp/dt max: +18.85 %; dp/dt min: +20.06 %; SLVP: -37.93 %), but neither of those parameters reached the initial values after the wash-out period (dp/dt max: −25.24 %; dp/dt min: −31.43 %; SLVP: −24.42 %). HR was significantly lower after wash-out period compared to control condition (−16.70 %). CF was significantly increased (+30.88 %) during application of verapamil and glycine and then significantly decreased (−59.85 %) during wash-out period. CF was significantly lower after wash-out period compared to initial state (−28.97 %). The value of DLVP was not significantly changed during the experiment.
The effects of combined application of verapamil, glutamate, and glycine on the cardiodynamic parameters and coronary flow in isolated rat heart
The simultaneous application of verapamil, glutamate and glycine induced significant decrease of dp/dt max (−40.10 %), dp/dt min (−44.85 %), and SLVP (−5 %) compared with control conditions, while CF was significantly increased (+24.69 %) compared with control. Following the wash-out period dp/dt max (+21.84 %), dp/dt min (+25.86 %) and SLVP (+9.21 %) were significantly increased, but did not reach the initial values (dp/dt max: −18.26 %; dp/dt min: -18.99 %; SLVP: -14.21 %), and CF was significantly decreased (−35.42 %), but also did not reach the initial values (−10.73 %). The value of HR significantly reduced (−13.47 %) after wash-out period compared with the effect of the applied substances as well as the initial values (−13.98 %). The value of DLVP was not significantly changed during the experiment (Fig. 1 and Table 1).
Comparisons of the values of cardiodynamic parameters between the experimental groups are shown on Table 2.
The effects of strychnine on cardiodynamic parameters and coronary flow in isolated rat heart
The application of strychnine in concentration of 10 μmol/l did not induce any significant change of observed cardiodynamic parameters or coronary flow (Fig. 2).
The effects of verapamil on the biomarkers of oxidative stress in isolated rat heart
(Fig. 3 and Table 3). Verapamil did not induce any significant change of the observed biomarkers of oxidative stress during experimental protocol.
The effects of combined application of verapamil and glutamate on the oxidative stress biomarkers in isolated rat heart
(Fig. 3 and Table 3). TBARS (−27.61 %), NO2 − (−30.84 %) and H2O2 (−24.28 %) significantly decreased during wash-out period, and values of these parameters were significantly lower (TBARS: −24.58 %; NO2 −: −26.14 %; H2O2: −26.81 %) after wash-out period compared to effect of the applied substances and control conditions. O2 − did not change significantly in any observed moment.
The effects of combined application of verapamil and glycine on the oxidative stress biomarkers in isolated rat heart
(Fig. 3 and Table 3). TBARS (−27.89 %), NO2 − (−30.71 %) and H2O2 (−34.40 %) were significantly decreased during wash-out period, and values of these parameters were significantly lower (TBARS: −23.67 %; NO2 −: −29.97 %; H2O2: −21.94 %) after wash-out period compared to effect of the applied substances and control conditions. O2 − did not change significantly in any observed moment.
The effects of combined application of verapamil, glycine, and glutamate on the oxidative stress biomarkers in isolated rat heart
The application of all three tested substances, verapamil, glycine, and glutamate, at the same time, induced significant increase of TBARS (+19.06 %), NO2 − (+19.09 %) and H2O2 (+41.86 %) compared with control conditions. Following the wash-out period TBARS (−34.64 %), NO2 − (−34.55 %) and H2O2 (−52.38 %) significantly dropped off. Only H2O2 of all previously mentioned parameters reached approximately initial value after the wash-out period (TBARS: −15.58 %; NO2 −: −15.46 %). O2 − did not change significantly in any observed moment (Fig. 3 and Table 3).
Comparisons of the values of oxidative stress biomarkers between the experimental groups are shown on Table 4.
The effects of strychnine on the oxidative stress biomarkers in isolated rat heart
The application of strychnine in concentration of 10 μmol/l did not induce any significant change of observed biomarkers of oxidative stress (Fig. 4).
The glutamate and glycine alone did not induce statistically significant change of any parameter of cardiac contractility or oxidative stress biomarkers. On the other hand, simultaneous application of glutamate and glycine induced significant decrease of dp/dt max, dp/dt min, heart rate, and coronary flow, as well as significant increase of NO2 −, O2 − and H2O2 levels. After the wash-out period all changed parameters returned to values that were not significantly different from controls. These data concerning the effects of glutamate or/and glycine are part of our preliminary research and have already been published [48].
Discussion
The aim of the present study was to assess the effects of verapamil and its combinations with glycine and glutamate on cardiac function, coronary flow and oxidative stress in isolated rat heart, in order to examine the potential role of NMDA receptors in regulation of cardiac function.
It is well known that verapamil blocks the entry of calcium into the cell through L-type calcium channels, prolonging the effective refractory period and reducing the conduction velocity of impulses through the AV node [10]. Acute application of verapamil in concentration of 3 μmol/L decreased significantly values of dp/dt max and dp/dt min, which reflect the contractile ability of the myocardium (Fig. 1a, b, Table 1). After the wash-out period these values were changed significantly again, namely dp/dt max and dp/dt min were increased, but parameters have not reached their initial values. These effects are consistent with the mechanism of action of verapamil, which includes a blockade of calcium influx and direct negative inotropic effects. In the study with human embryonic stem cell-derived cardiomyocytes, Hayakawa and coauthors verified the relationship between the intracellular concentration of Ca2+ and contractility [20]. Namely, in this study, verapamil decreased all of the observed parameters of Ca2+ transient and contractile motion. In the case of combined application of verapamil and glutamate dp/dt max and dp/dt min were also significantly reduced, but percentage reduction were considerably lower compared to verapamil alone (Fig. 1a, b, Table 1). Xie and coworkers in their study have investigated the role of metabotropic glutamate receptors, mGluR1/mGluR5, in regulation of connexin 43 (Cx43) phosphorylation and gap junctional intercellular communication [56]. They found that direct activation of mGluR1 in cardiomyoblast cells increases Cx43 phosphorylation level and suppresses gap junctional intercellular communication that might be the reason for less reduction of myocardial contractility parameters in this group. Furthermore, Liu and coworkers found that activation of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors by glutamate, besides other effects, induces calcium mobilization in cardiomyocytes [27]. As AMPA receptor belongs to the family of ionotropic glutamate receptors, it is a channel permeable to Ca2+, and these authors confirmed that treatment with AMPA in dose of 10−5 mol/L and 10−4 mol/L induced a Ca2+ transient in the cardiomyocytes that can be a potential explanation for the improvement of myocardial contractility in this experimental group. Similarly to the previous experimental group, combined application of verapamil and glycine induced significant decrease of dp/dt max and dp/dt min, and percentage reduction was similar (Fig. 1a, b, Table 1). Results of Qi and coauthors suggested the existence of glycine receptors (GlyR) in cardiomyocytes and their participation in cytoprotection from the damage induced by lipopolysaccharide and hypoxia/reoxygenation injury [41]. The GlyR represents a glycine-gated chloride channel whose activation is essential for certain functions of the nervous system as well as cells of the immune system [12, 43]. The proposed mechanism is that direct activation of GlyR by glycine prevents the excess calcium influx into the cardiomyocytes. The results of numerous studies also suggest the protective effects of glycine against oxidative damage in cardiovascular tissues [9, 44, 54]. However, the application of strychnine, GlyR blocker, did not induce any significant change in values of cardiodynamic parameters (Fig. 2), as well as application of glycine alone [48]. In investigation of Wang and coauthors, glycine induced significant reduction in the entry of Ca2+ into the cardiomyocytes induced by lipopolysaccharide [53]. Strychnine prevented this action of glycine, as well as increase of intracellular concentration of Ca2+ induced by potassium chloride. The potential cause of absence of effects during strychnine application could be the applied experimental protocol and the method or length of strychnine administration. Combined application of all three tested substances, verapamil, glutamate and glycine, also produced significant reduction of dp/dt max and dp/dt min, but percentage reduction in this experimental group was the least (Fig. 1a, b). Also in this experimental group, the values after the wash-out period were closest to the control values (Table 1). Some of previous data from our laboratory indicated that combined application of glutamate and glycine caused a decrease in myocardial contractility parameters, in contrast to their individual administration [48]. Taking into account the role of NMDA-R as Ca2+ channels and their distribution in many tissues, they are considered to be important for pathological processes in myocardium, in view of the significance of maintaining Ca2+ homeostasis for the proper functioning of the heart [8]. Some of the adverse effects of hyperhomocysteinemia are related with excessive stimulation of NMDA receptors by homocystein and increase intracellular and mitochondrial Ca2+ content [14, 52]. But in the case of concurrent administration of verapamil, a Ca2+ channel blocker, and glutamate and glycine, NMDA channel coactivators, activated NMDA channels may allow entry of sufficient amount Ca2+ which allows an increase in myocardial contractility.
Comparing values of dp/dt max and dp/dt min, as myocardial contractility parameters, between experimental groups, we get significant differences in dp/dt max after application of verapamil compared to the other three experimental groups (Table 2). After wash-out period, differences between these parameters were insignificant.
During verapamil application SLVP decreased significantly, and after wash-out period, this parameter was significantly increased but did not reach the control values (Fig. 1c, Table 1). DLVP insignificantly decreased during verapamil administration, and the decline continued during the wash-out period, but control values and values after wash-out period did not differ significantly (Fig. 1d, Table 1). Verapamil, as a Ca2+ channel blocker, is an important drug for the treatment of hypertension [10]. Xu and coworkers induced reduction of both systolic and diastolic blood pressure in rats, by verapamil in dose of 15 μg/100 g b.w. [57]. Cellular mechanism of action of verapamil, as well as other Ca2+ antagonists, includes binding to α1c subunit of the L-type calcium channel and thus block the entrance of extracellular Ca2+, resulting in decrease of contractility, systolic and diastolic pressures lowering and vascular smooth muscle relaxation [2, 10]. In other three experimental groups (verapamil in combination with glycine, glutamate, and glycine and glutamate), decrease of SLVP was also significant and percentage reductions were similar between groups (Table 1). After wash-out period, values of SLVP increased significantly, and the percentage difference between the control values and the values after a wash-out period was the lowest in the group treated with all three tested substances (Table 1). Diastolic pressure did not change significantly in any group (Fig. 1d, Table 1). Some of our previous data have shown that neither glutamate nor glycine, nor their combination, have impact on SLVP and DLVP [48]. The possible reason of relative increase of SLVP in group treated with combination of glutamate and verapamil, compared to verapamil only, could be the activation of AMPA receptors in the heart by glutamate [27]. Also, there are evidences of the presence of metabotropic glutamate receptors in cardiomyocytes that are assumed to have different roles [56, 58]. These receptors may be able to provide a certain transient Ca2+ inflow into cardiomyocytes which is enough to increase the force of myocardial contraction and SLVP. Similar to the combined administration of verapamil and glutamate, combination of verapamil and glycine induced relative increase of SLVP, compared to verapamil only (Table 1, Fig. 1c). We already have mentioned that activation of GlyR by glycine prevent the excessive inflow of Ca2+ and thus prevent the myocardial damage [41]. But, Mishra and coauthors found that glycine induces pressor responses in hypertensive rats and fall in mean arterial pressure in normotensive rats [33]. So the effects of glycine on systolic blood pressure are not clear. The smallest difference in the values between control and wash-out period in group treated with all three estimated substance could be the consequence of activation of NMDA-R. There are sufficient data that activation of NMDA-R in central nervous system induces increase in blood pressure, and vice versa [16, 49]. Our previous data also showed decrease of SLVP induced by NMDA-R inhibitor MK-801 [18]. So activation of these receptors by glutamate and glycine in heart may induce influx of Ca2+ sufficient to partially increase SLVP during simultaneous administration of verapamil.
Comparing the SLVP and DLVP parameters between the groups it can be observed that after the application of tested substances (effect), SLVP was significantly higher in experimental groups treated with all three substances and with verapamil and glutamate in comparison to groups treated with verapamil only (Table 2). After wash-out period, values of SLVP were not significantly differed, and also values of DLVP were similar between all groups in all observed situations (Table 2).
Verapamil induced significant decrease of HR, which also happened in groups in which verapamil have been applied in combination with glutamate or glycine (Fig. 1e, Table 1). Verapamil has suppressive effect on sinoatrial node resulting in decelerated atrioventricular conduction velocity and reduction of the heart rate [2, 10, 18]. On the other hand in the group treated with combination of verapamil, glutamate, and glycine, practically there were no changes in heart rate (Fig. 1e, Table 1). Also there are lots of data about activation of NMDA receptors in some regions of CNS and changes in heart rate. Santini and coauthors induced tachycardia by application of L-glutamate into the ventral hypothalamus [45]. In our previous work, we induced bradycardia by application of NMDA-R antagonist MK-801 [49]. During wash-out period HR was decreased significantly only in the group treated with combination of verapamil, glutamate and glycine (Fig. 1e, Table 1), and differences were significant between control and wash-out period in all experimental groups (Fig. 1e, Table 1).
HR was significantly higher after the administration of verapamil, glutamate and glycine in comparison to treatment with verapamil only or combination of verapamil and glutamate (Table 2). After wash-out period, values of HR were significantly higher in experimental group treated with all three tested substances compared to group treated with verapamil and glutamate, as well as in group treated with verapamil only compared to group treated with verapamil and glutamate.
Coronary flow was significantly increased in all experimental groups (Fig. 1f, Table 1). Increase of coronary flow by verapamil is used during surgical interventions on heart, such as percutaneous coronary intervention, in order to avoid no-reflow phenomenon [11]. The underlying mechanism could be the attenuation of Ca2+ inflow in vascular smooth muscle cells [36]. Elevation in coronary flow in group treated with all three tested substances could be explained by quantitatively insufficient amount of calcium that enters through NMDA-R in vascular smooth muscle cells to reduce the relaxing effect of verapamil. Increase of coronary flow also could be mediated by increased amount of nitric oxide. There are evidences that activation of NMDA-R in the rat cerebral parenchymal arterioles induce dilatation by activation of neuronal nitric oxide synthase (NOS) and increased production of superoxide and nitric oxide within the parenchymal arterioles [19]. In our results, values of nitrites that reflect nitric oxide were significantly increased in this group (Fig. 3b, Table 3). One of proposed mechanisms by which homocysteine induces adverse effects on cardiovascular system is prolonged activation of NMDA-R [13, 38]. Increase of coronary flow in other two experimental groups in probably mediated by dilatative effect of verapamil.
The values of CF were significantly higher in groups in which were applied verapamil only or all three tested substances, relative to other two experimental groups, and similar situation maintained during wash-out period (Table 2).
The next part of experimental protocol was referred to assessment of oxidative stress parameters during application of tested substances.
In experimental group treated with verapamil, there were no changes in any observed parameter (Fig. 3, Table 3). Abd Allah and coauthors examined the effect of verapamil on iron-overload induced oxidative stress and cardiac structural changes, and found that concomitant treatment with verapamil and ferrous sulfate induced increase in serum total antioxidant capacity and decline of serum total peroxide, in contrast to the group treated only with ferrous sulfate [1]. Also, verapamil exerted a protective effect on hepatic ischemia-reperfusion injury in rats, and significantly corrected the oxidative stress biomarkers, TBARS and reduced glutathione (GSH) in the liver, as well as myeloperoxidase (MPO) and total nitrate/nitrite (NOx) [32]. Truancy of protective effects of verapamil in our study could be the consequence of short verapamil treatment time or different experimental protocol.
In group treated with combination of verapamil and glutamate TBARS, nitrites (NO2 −) and hydrogen peroxide (H2O2) reduced significantly during wash-out period, while superoxide anion radical (O2 −) did not change significantly (Fig. 3, Table 3). King and coworkers in their study showed protective effect of glutamate on rat cardiomyocytes [24]. Namely, they have investigated the effect of glutamate upon ROS generation during various models of metabolic inhibition and wash-off or oxidative stress, as well as the relationship between glutamate and the glutathione-redox system, and showed that glutamate-loaded cardiomyocytes produced significantly less ROS than control cells under all the stressful conditions. The proposed mechanism for this action of glutamate is stimulation of glutathione peroxidase and consequent increased GSH-mediated removal of H2O2 in glutamate-loaded cells. In our previous work, glutamate alone did not induce significant changes in tested biomarkers of oxidative stress [48]. However, in this case, there may be a cumulative protective effect of verapamil and glutamate.
Combined application of verapamil and glycine induced decrease in values of TBARS, NO2 − and H2O2 during wash-out period, while O2 − did not change significantly (Fig. 3, Table 3). The protective role of glycine against oxidative stress is also linked to the production of glutathione. Some results showed that dietary supplementation with glutathione precursors, cysteine and glycine, in elderly population restores glutathione synthesis and concentrations and lowers levels of oxidative stress and oxidant damages [47]. We already mentioned above that some studies have demonstrated that cardiomyocytes exhibit glycine-gated chloride channel, whose activation resulting in chloride influx and hyperpolarization of the membrane, and that way prevent influx of extracellular Ca2+ [41]. In previous work from our laboratory, glycine, similarly to glutamate, did not induce significant changes in values of oxidative stress markers [48]. We also investigated the influence of GlyR blocker, strychnine on oxidative status of isolated rat heart, and there were no differences in any observed biomarker of oxidative stress (Fig. 4). In the study of Arora and coauthors found that strychnine did not have any effects in ischemia reperfusion-induced acute kidney injury (AKI) in rats [4]. As well as in the case of glutamate, we can assume a cumulative protective effect of verapamil and glycine.
In the last experimental group during administration of all tested substances (verapamil, glutamate, and glycine), values of TBARS, NO2 −, and H2O2 increased significantly, and after that significantly decreased during wash-out period. Values after wash-out period were significantly lower compared to control conditions (Fig. 3, Table 3). O2 − did not change significantly. Increase of measured biomarkers of oxidative stress is in accordance with our previous results [48]. Gao and coworkers showed that activation of NMDA-R in rat-cultured cardiomyocytes by NMDA induces ROS generation, which could be prevented by MK-801 or removal of extracellular free Ca2+, suggesting that the NMDA-R mediated generation of ROS in cardiomyocytes is Ca2+-dependent [14]. Later lowering of the observed oxidative stress parameters could be a consequence the protective effects of applied substances.
After the application of all three experimental substances values of TBARS, NO2 − and H2O2 were significantly higher in comparison to other groups, except in comparison to treatment with verapamil only for NO2 − and H2O2 (Table 4). Values of NO2 − and H2O2 were significantly higher in group in which was applied verapamil only in comparison to group treated with verapamil and glycine. After wash-out period TBARS, NO2 − and H2O2 were significantly higher in group treated with verapamil, glutamate and glycine relative to group treated to verapamil and glycine, and TBARS and NO2 − were higher compared to group treated with verapamil and glutamate. Also after wash-out period, the TBARS, NO2 − and H2O2 were higher in group treated with verapamil only relative to group treated with verapamil and glycine, and NO2 − was higher relative to group treated with verapamil and glutamate (Table 4).
A substantial number of data brought into connection variety of disorders of the cardiovascular system and oxidative stress, such as coronary artery disease, hypertension, and atherosclerosis [25, 29, 37]. Keeping in mind the role and mechanism of action of NMDA receptors, we were interested to assess the consequences of their activation in the heart and coronary circulation. Activation of NMDA-R will increase intracellular Ca2+ levels and mitochondrial Ca2+ levels, resulting in oxidative stress [14, 52]. There are several sources of ROS in cardiovascular tissues, including NADPH oxidase, nitric oxide (NO) synthase, xanthine oxidase, lipoxygenases, and the mitochondrial respiratory chain. Under physiological conditions, the main source of free radicals are mitochondria, but disturbances of Ca2+ content in cells could increase the mitochondrial ROS production [7, 28]. NADPH oxidase family contains several enzymes which are largely present in the cells that build tissues of the cardiovascular system, and some of them are regulated by Ca2+ [3, 6, 21, 22, 55].
On the basis of the obtained results, we can conclude that simultaneous application of glutamate and glycine, and the probable consequent activation of the NMDA-R, had the greatest impact on calcium channel blockade by verapamil, which was reflected in the degree of change of the observed cardiodynamic parameters. Furthermore, only in the experimental group treated with verapamil, glutamate, and glycine, oxidative stress parameters have increased, which in turn may be brought in connection with the activation of the NMDA-R, but these short-term changes probably did not adversely affect the function of the heart.
References
Abd Allah ES, Ahmed MA, Abdel Mola AF (2014) Comparative study of the effect of verapamil and vitamin D on iron overload-induced oxidative stress and cardiac structural changes in adult male rats. Pathophysiology 21:293–300
Abernethy DR, Schwartz JB (1999) Calcium-antagonist drugs. N Engl J Med 341:1447–1457
Ago T, Kitazono T, Ooboshi H, Iyama T, Han YH, Takada J, Wakisaka M, Ibayashi S, Utsumi H, Iida M (2004) Nox4 as the major catalytic component of an endothelial NAD(P)H oxidase. Circulation 109(2):227–233
Arora S, Kaur T, Kaur A, Singh AP (2014) Glycine aggravates ischemia reperfusion-induced acute kidney injury through N-methyl-D-aspartate receptor activation in rats. Mol Cell Biochem 393(1–2):123–131
Auclair C, Voisin E (1985) Nitroblue tetrazolium reduction. In: Greenvvald RA (ed) Handbook of methods for oxygen radical research. CRC Press Une, Boca Raton, pp. 123–132
Bedard K, Krause KH (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87(1):245–313
Boyman L, Williams GS, Lederer WJ (2015) The growing importance of mitochondrial calcium in health and disease. Proc Natl Acad Sci U S A 112(36):11150–11151
Bozic M, Valdivielso JM (2015) The potential of targeting NMDA receptors outside the CNS. Expert Opin Ther Targets 19:399–413
Díaz-Flores M, Cruz M, Duran-Reyes G, Munguia-Miranda C, Loza-Rodríguez H, Pulido-Casas E, Torres-Ramírez N, Gaja-Rodriguez O, Kumate J, Baiza-Gutman LA, Hernández-Saavedra D (2013) Oral supplementation with glycine reduces oxidative stress in patients with metabolic syndrome, improving their systolic blood pressure. Can J Physiol Pharmacol 91:855–860
Elliott WJ, Ram CV (2011) Calcium channel blockers. J Clin Hypertens (Greenwich) 13:687–689
Faruk Akturk I, Arif Yalcin A, Biyik I, Sarikamis C, Turhan Caglar N, Erturk M, Celik O, Uzun F, Murat Caglar I, Oner E (2014) Effects of verapamil and adenosine in an adjunct to tirofiban on resolution and prognosis of no reflow phenomenon in patients with acute myocardial infarction. Minerva Cardioangiol 62:389–397
Froh M, Thurman RG, Wheeler MD (2002) Molecular evidence for a glycine-gated chloride channel in macrophages and leukocytes. Am J Physiol Gastrointest Liver Physiol 283:856–863
Ganguly P, Alam SF (2015) Role of homocysteine in the development of cardiovascular disease. Nutr J 14:6
Gao X, Xu X, Pang J, Zhang C, Ding JM, Peng X, Liu Y, Cao JM (2007) NMDA receptor activation induces mitochondrial dysfunction, oxidative stress and apoptosis in cultured neonatal rat cardiomyocytes. Physiol Res 56:559–569
Gill SS, Pulido OM, Mueller RW, McGuire PF (1998) Molecular and immunochemical characterization of the ionotropic glutamate receptors in the rat heart. Brain Res Bull 46:429–434
Glass MJ, Wang G, Coleman CG, Chan J, Ogorodnik E, Van Kempen TA, Milner TA, Butler SD, Young CN, Davisson RL, Iadecola C, Pickel VM (2015) NMDA receptor plasticity in the hypothalamic paraventricular nucleus contributes to the elevated blood pressure produced by angiotensin II. J Neurosci 35:9558–9567
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15 N]nitrate in biological fluids. Anal Biochem 126:131–138
Grossman E, Messerli FH (2004) Calcium antagonists. Prog Cardiovasc Dis 47:34–57
Hama-Tomioka K, Kinoshita H, Nakahata K, Kondo T, Azma T, Kawahito S, Hatakeyama N, Matsuda N (2012) Roles of neuronal nitric oxide synthase, oxidative stress, and propofol in N-methyl-D-aspartate-induced dilatation of cerebral arterioles. Br J Anaesth 108:21–29
Hayakawa T, Kunihiro T, Ando T, Kobayashi S, Matsui E, Yada H, Kanda Y, Kurokawa J, Furukawa T (2014) Image-based evaluation of contraction-relaxation kinetics of human-induced pluripotent stem cell-derived cardiomyocytes: correlation and complementarity with extracellular electrophysiology. J Mol Cell Cardiol 77:178–191
Joseph LC, Barca E, Subramanyam P, Komrowski M, Pajvani U, Colecraft HM, Hirano M, Morrow JP (2016) Inhibition of NAPDH oxidase 2 (NOX2) prevents oxidative stress and mitochondrial abnormalities caused by saturated fat in cardiomyocytes. PLoS One 11(1):e0145750
Kalinina N, Agrotis A, Tararak E, Antropova Y, Kanellakis P, Ilyinskaya O, Quinn MT, Smirnov V, Bobik A (2002) Cytochrome b558-dependent NAD(P)H oxidase-phox units in smooth muscle and macrophages of atherosclerotic lesions. Arterioscler Thromb Vasc Biol 22(12):2037–2043
Kanani PM, Sinkey CA, Browning RL, Allaman M, Knapp HR, Haynes WG (1999) Role of oxidant stress in endothelial dysfunction produced by experimental hyperhomocyst(e)inemia in humans. Circulation 100(11):1161–1168
King N, McGivan JD, Griffiths EJ, Halestrap AP, Suleiman MS (2003) Glutamate loading protects freshly isolated and perfused adult cardiomyocytes against intracellular ROS generation. J Mol Cell Cardiol 35:975–984
Kurian GA, Rajagopal R, Vedantham S, Rajesh M (2016) The role of oxidative stress in myocardial ischemia and reperfusion injury and remodeling: revisited. Oxidative Med Cell Longev 2016:1656450
Leung JC, Travis BR, Verlander JW, Sandhu SK, Yang SG, Zea AH, Weiner ID, Silverstein DM (2002) Expression and developmental regulation of the NMDA receptor subunits in the kidney and cardiovascular system. Am J Physiol Regul Integr Comp Physiol 283:964–971
Liu Y, Zhou L, Xu HF, Yan L, Ding F, Hao W, Cao JM, Gao X (2013) A preliminary experimental study on the cardiac toxicity of glutamate and the role of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor in rats. Chin Med J 126:1323–1332
Madamanchi NR, Runge MS (2013) Redox signaling in cardiovascular health and disease. Free Radic Biol Med 61:473–501
Madisetty MK, Kumaraswami K, Katkam S, Saumya K, Satyanarayana Raju Y, Chandra N, Jyotsna M, Patnaik S, Kutala VK (2016) Assessment of oxidative stress markers and carotid artery intima-media thickness in elderly patients without and with coronary artery disease. Indian J Clin Biochem 31(3):278–285
Mandal R, Kutala VK, Khan M, Mohan IK, Varadharaj S, Sridhar A, Carnes CA, Kálai T, Hideg K, Kuppusamy P (2007) N-hydroxy-pyrroline modification of verapamil exhibits antioxidant protection of the heart against ischemia/reperfusion-induced cardiac dysfunction without compromising its calcium antagonistic activity. J Pharmacol Exp Ther 323:119–127
Meldrum BS (2000) Glutamate as a neurotransmitter in the brain: review of physiology and pathology. J Nutr 130:1007–1015
Messiha BA, Abo-Youssef AM (2015) Protective effects of fish oil, allopurinol, and verapamil on hepatic ischemia-reperfusion injury in rats. J Nat Sci Biol Med 6:351–355
Mishra RC, Tripathy S, Quest D, Desai KM, Akhtar J, Dattani ID, Gopalakrishnan V (2008) L-serine lowers while glycine increases blood pressure in chronic L-NAME-treated and spontaneously hypertensive rats. J Hypertens 26:2339–2348
Nakamichin N, Ohno H, Kuramoto N, Yoneda Y (2002) Dual mechanisms of Ca2+ increases elicited by N-methyl-D-aspartate in immature and mature cultured cortical neurons. J Neurosci Res 67:275–283
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Ok SH, Kwon SC, Kang S, Choi MJ, Sohn JT (2014) Mepivacaine-induced intracellular calcium increase appears to be mediated primarily by calcium influx in rat aorta without endothelium. Korean J Anesthesiol 67:404–411
Oyagbemi AA, Omobowale TO, Asenuga ER, Adejumobi AO, Ajibade TO, Ige TM, Ogunpolu BS, Adedapo AA (2016) Yakubu MA (2016) sodium fluoride induces hypertension and cardiac complications through generation of reactive oxygen species and activation of nuclear factor kappa beta. Environ Toxicol. doi:10.1002/tox.22306
Pang X, Liu J, Zhao J, Mao J, Zhang X, Feng L, Han C, Li M, Wang S, Wu D (2014) Homocysteine induces the expression of C-reactive protein via NMDAr-ROS-MAPK-NF-κB signal pathway in rat vascular smooth muscle cells. Atherosclerosis 236:73–81
Petersen OH (2002) Cation channels: homing in on the elusive CAN channels. Curr Biol 12:520–522
Pick E, Keisari Y (1980) A simple colorimetric method for the measurement of hydrogen peroxide produced by cells in culture. J Immunol Methods 38:161–170
Qi RB, Zhang JY, Lu DX, Wang HD, Wang HH, Li CJ (2007) Glycine receptors contribute to cytoprotection of glycine in myocardial cells. Chin Med J 120:915–921
Raghuveer G, Sinkey CA, Chenard C, Stumbo P, Haynes WG (2001) Effect of vitamin E on resistance vessel endothelial dysfunction induced by methionine. Am J Cardiol 88(3):285–290
Rajendra S, Lynch JW, Schofield PR (1997) The glycine receptor. Pharmacol Ther 73:121–146
Ruiz-Ramírez A, Ortiz-Balderas E, Cardozo-Saldaña G, Diaz-Diaz E, El-Hafidi M (2014) Glycine restores glutathione and protects against oxidative stress in vascular tissue from sucrose-fed rats. Clin Sci (Lond) 126:19–29
Santini CO, Fassini A, Scopinho AA, Busnardo C, Corrêa FM, Resstel LB (2013) The ventral hippocampus NMDA receptor/nitric oxide/guanylate cyclase pathway modulates cardiovascular responses in rats. Auton Neurosci 177:244–252
Seeber S, Becker K, Rau T, Eschenhagen T, Becker CM, Herkert M (2000) Transient expression of NMDA receptor subunit NR2B in the developing rat heart. J Neurochem 75:2472–2477
Sekhar RV, Patel SG, Guthikonda AP, Reid M, Balasubramanyam A, Taffet GE, Jahoor F (2011) Deficient synthesis of glutathione underlies oxidative stress in aging and can be corrected by dietary cysteine and glycine supplementation. Am J Clin Nutr 94:847–853
Srejovic I, Jakovljevic V, Zivkovic V, Jeremic N, Jevdjevic M, Stojic I, Djuric D (2015a) The effects of glycine, glutamate and their combination on cardiodynamics, coronary flow and oxidative stress in isolated rat heart. Curr Res Cardiol 2:63–68
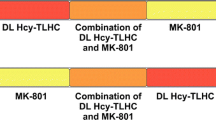
Srejovic I, Jakovljevic V, Zivkovic V, Barudzic N, Radovanovic A, Stanojlovic O, Djuric DM (2015b) The effects of the modulation of NMDA receptors by homocysteine thiolactone and dizocilpine on cardiodynamics and oxidative stress in isolated rat heart. Mol Cell Biochem 401:97–105
Stern JE, Potapenko ES (2013) Enhanced NMDA receptormediated intracellular calcium signaling in magnocellular neurosecretory neurons in heart failure rats. Am J Physiol Regul Integr Comp Physiol 305:414–422
Traynelis SF, Wollmuth LP, McBain CJ, Menniti FS, Vance KM, Ogden KK, Hansen KB, Yuan H, Myers SJ, Dingledine R (2010) Glutamate receptor ion channels: structure, regulation, and function. Pharmacol Rev 62:405–496
Vacek TP, Vacek JC, Tyagi SC (2012) Mitochondrial mitophagic mechanisms of myocardial matrix metabolism and remodelling. Arch Physiol Biochem 118:31–42
Wang HD, Lü XX, Lu DX, Qi RB, Wang YP, Fu YM, Wang LW (2009) Glycine inhibits the LPS-induced increase in cytosolic Ca2+ concentration and TNFalpha production in cardiomyocytes by activating a glycine receptor. Acta Pharmacol Sin 30(8):1107–1114
Wang W, Wu Z, Dai Z, Yang Y, Wang J, Wu G (2013) Glycine metabolism in animals and humans: implications for nutrition and health. Amino Acids 45:463–477
Xiao L, Pimentel DR, Wang J, Singh K, Colucci WS, Sawyer DB (2002) Role of reactive oxygen species and NAD(P)H oxidase in alpha(1)-adrenoceptor signaling in adult rat cardiac myocytes. Am J Physiol Cell Physiol 282(4):C926–C934
Xie F, Yi SL, Hao L, Zhang Y, Zhong JQ (2015) Role of group I metabotropic glutamate receptors, mGluR1/mGluR5, in connexin 43 phosphorylation and inhibition of gap junctional intercellular communication in H9c2 cardiomyoblast cells. Mol Cell Biochem 400:213–222
Xu YJ, Elimban V, Dhalla NS (2015) Reduction of blood pressure by store-operated calcium channel blockers. J Cell Mol Med. doi:10.1111/jcmm.12684
Zhu DY, Zhou LM, Zhang YY, Huang JQ, Pan X, Lou YJ (2012) Involvement of metabotropic glutamate receptor 5 in cardiomyocyte differentiation from mouse embryonic stem cells. Stem Cells Dev 21:2130–2141
Acknowledgments
This project was supported by Grant No. 175043 from the Ministry of Science and Technical Development of the Republic of Serbia and the Junior Project 04/2011, Faculty of Medical Sciences, University of Kragujevac, Serbia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Stojic, I., Srejovic, I., Zivkovic, V. et al. The effects of verapamil and its combinations with glutamate and glycine on cardiodynamics, coronary flow and oxidative stress in isolated rat heart. J Physiol Biochem 73, 141–153 (2017). https://doi.org/10.1007/s13105-016-0534-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-016-0534-0