Abstract
A 56-year-old male was admitted to our hospital complaining of chest pain. The patient had chronic kidney disease requiring a minimum contrast procedure when performing percutaneous coronary intervention. A jailed wire technique is known to reduce the risk of side branch occlusion. We report a case measuring the presence of ischemia in the side branch (SB) by a jailed Opto Wire (Opsens, Quebec) after implantation of a stent in the main vessel for the treatment of a bifurcation lesion. This method provides for a decrease in usage of contrast without leaving the side branch at risk of ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous coronary intervention (PCI) for coronary bifurcation lesions is common in daily practice [1, 2]. Following stenting in the main vessel (MV), ostial stenosis or total occlusion of the side branch (SB) occasionally occurs [3–5]. As a result, procedures involving bifurcation lesions tend to be complex, resulting in increased contrast volume usage. Contrast induced nephropathy (CIN) is an important complication following exposure to iodinated contrast [6]. There is a threshold of the rate of contrast volume to estimated glomerular filtration rate (CV/eGFR) above which increases the occurrence of CIN [7, 8]. Therefore, minimum contrast procedures are ideal even for complex PCI of patients with chronic kidney disease (CKD). A jailed wire technique is known to reduce the risk of SB occlusion. The original method is described previously [9, 10].
It is cumbersome to know if there is ischemia in the jailed SB after the treatment of a coronary bifurcation lesion with a stent deployed in the MV. We report a case of the measurement of the presence of ischemia in the SB by a jailed Opto Wire. Theoretical less drift and improved coating with this wire might make this wire suitable for use in such a tough condition.
In this case report, we undertook a minimum contrast procedure in a complex bifurcation lesion.
Case report
A 56-year-old male was admitted to our hospital complaining of chest pain.
Coronary risk factors of this patient were hypertension, hyperlipidemia, and diabetes. Blood tests revealed increased creatinine (1.75 mg/dl), decreased estimated glomerular filtration rate (eGFR) (33.1 GFR/1.73 m2), a slightly elevated serum troponin-T level (0.709 ng/ml), and an elevated N terminal-pro brain natriuretic peptide level (4432.0 pg/ml). The electrocardiogram (ECG) showed a slight depletion of the ST segment in leads V4–6, I, aVL, II, III and aVF. A coronary angiography (CAG) showed severe stenosis in the coronary tree (#1 75 %, #2 75 %, #6 50 %, #7 90 %, #9 75-90 %, #13 99 %, #14 75 %) (Fig. 1a–c). PCI to the left circumflex artery (LCX) was performed. A 3.0 × 38 mm Resolute Integrity stent (Medtronic, Minneapolis, MN, USA) was deployed (Fig. 1d). Since it was an emergency operation, the information about the increased creatinine level was reported to the operator near the end of the procedure resulting in a total of 80 ml of contrast media usage to complete the procedure. Fortunately, CIN was not observed after the PCI. A few days later during rehabilitation, the patient complained of slight chest pain and an ECG monitor showed a deep depression of the ST segment.
A CAG was performed to confirm the cause of the depression of the ST segment. Following the confirmation of no stent thrombosis in the implanted stent in the LCX, fractional flow reserve (FFR) measurement of the lesion in the RCA was performed. The lesion of RCA was diagnosed as an intermediate stenosis because the value of FFR was 0.79. Next, FFR measurement of the lesion in the LAD was attempted, but the wiring of the lesion with a pressure wire was difficult due to the severity of the lesion. A PCI to the LAD at the bifurcation point with severe stenosis of the diagonal branch (Medina classification 1.1.1) was then performed without FFR measurement despite presence of CKD and the short duration (4 days) after the initial PCI.
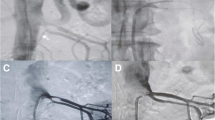
A blood test just before the second PCI revealed rather improved creatinine (1.57 mg/dl) and estimated glomerular filtration rate (eGFR) (37.3 GFR/1.73 m2). There was severe stenosis just distal of the diagonal branch in the MV; therefore, the formation of stenosis at the ostium of the diagonal branch was expected due to plaque shift. Access was obtained via the right radial artery, using a 6-French PB 3.5 guide catheter (Asahi Intecc Co., Aichi, Japan). A SION blue wire (Asahi Intecc Co., Aichi, Japan) was advanced to the distal LAD. A pressure wire was then advanced into the diagonal branch with the pressure sensor placed beyond the ostium of the diagonal branch (Fig. 2a). Pre-FFR of the diagonal branch was 0.90. An intravascular ultrasound (IVUS) catheter (Terumo, Tokyo, Japan) was advanced to the distal LAD. The IVUS showed an eccentric fibrous plaque in the lesion. A 3.5 × 18 mm Resolute Integrity stent (Medtronic, Minneapolis, MN, USA) was deployed at 9 atm in the MV with the pressure wire in the diagonal branch jailed by the stent (Fig. 2b). Following a post-dilatation with the stent delivery system at 18 atm, IVUS was performed. It revealed a malposition of the stent and additional dilatation was, therefore, performed with a 4.25 × 13 mm RAIDEN balloon (Kaneka Medix, Osaka, Japan) at 18 atm. The second FFR measurement was performed, while the pressure wire was jailed under the implanted stent and the value was 0.86 (Fig. 2c). No further diagonal branch intervention was performed. The jailed pressure wire was carefully removed. The pressure wire was brought back to the distal tip of the guiding catheter confirming the presence of zero drift. FFR of the main vessel after PCI was 0.95.
a Percutaneous coronary intervention to the left anterior descending coronary artery (LAD). Black arrows a pressure wire in the diagonal branch. Asterisk a SION blue wire in the LAD. b Implantation of stent in the main vessel. Black arrows a pressure wire in the diagonal branch jailed by the stent. Asterisk 3.5 × 18 mm Resolute Integrity stent in the main vessel. c The FFR measurement after an additional dilatation with a 4.25 × 13 mm RAIDEN balloon at 18 atm, while the pressure wire was jailed under the implanted stent. The value was 0.86 and the lesion at the diagonal branch ostium was functionally insignificant. d A final coronary angiogram: Well-dilated main vessel and preserved diagonal branch flow
A final CAG revealed a well-dilated MV and preserved diagonal branch flow (Fig. 2d). Only 10 ml of contrast media was necessary to complete the procedure. A blood test revealed unchanged creatinine (1.64 mg/dl) and estimated glomerular filtration rate (eGFR) (35.6 GFR/1.73 m2) 2 days after the second PCI. CIN was prevented with the minimum contrast procedure.
His chest pain disappeared after PCI.
Discussion
CIN is one of the important complications in PCI, and the prognosis of patients with CIN is sometimes poor [11–13]. Special attention should be paid particularly when patients with eGFR <45 ml/min/1.73 m2 undergo PCI [14]. The safety threshold for a safe CV/eGFR is reported to be 1.0–3.0 [7, 15]. When CV/eGFR ≤1.0, the occurrence of CIN is reported to be especially low [16]. However, contrast volume often exceeds this rate for a complex PCI [17]. PCI to a coronary bifurcation is one of the complex PCI procedures. During MV stenting in coronary bifurcation lesions, ostial stenosis or total occlusion of SB occurs frequently. The mechanisms for this SB narrowing or occlusion are carina shift, plaque shift, dissection, spasm, and bifurcation angle changes [18, 19]. Re-wiring of the narrowed or occluded SB can be difficult and the prolonged flow disturbance of the SB might cause a peri-procedural myocardial infarction [20, 21].
On the other hand, it is reported that the difference in 9-month target vessel revascularization for treatments of SB was comparable between the FFR-guided group and the angiography-guided group [22]. Therefore, following MV stenting if the FFR is higher than 0.75 in the SB, no further SB intervention is necessary and results in a decrease in contrast usage. If the FFR is ≤0.75, the SB is rewired with a third guidewire without removing the jailed pressure wire (JPW). After the JPW is removed carefully with the third wire remaining in the SB, a kissing balloon technique can be performed. This jailed wire technique is a very user-friendly technique [9, 10]. Jailing a pressure wire with a stent may cause difficulty with removing the wire and can be a cause of drift. The new Opto Wire has an improved hydrophilic coating and theoretically has less drift by using optical fibers. These features of this new wire might be ideal for jailed pressure wire technique. This minimum contrast procedure was safely performed in a complex bifurcation lesion using the jailed wire technique in a patient with CKD.
If the removal of the JPW is difficult, we should avoid the forceful pull out of the pressure wire to avoid a fracture of the pressure wire. A ballooning with a low-profile balloon over the JPW may facilitate the removal of the wire.
Conclusion
The jailed pressure wire technique is an effective method to minimize the amount of contrast in the treatment of a complex bifurcation lesion treatment.
The new Opto Wire has several unique advantageous features for the application in jailed pressure wire technique.
References
Melikian N, Airoldi F, Di Mario C. Coronary bifurcation stenting, current techniques outcome and possible future developments. Minerva Cardioangiol. 2004;52:365–78.
Lassen JF, Holm NR, Stankovic G, et al. Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European Bifurcation Club meetings. EuroIntervention. 2014;10(5):545–60.
Tanabe K, Hoye A, Lemos PA, et al. Restenosis rates following bifurcation stenting with sirolimus-eluting stents for de novo narrowings. Am J Cardiol. 2004;94:115–8.
Kralev S, Poerner TC, Basorth D, et al. Side branch occlusion after coronary stent implantation in patients presenting with ST-elevation myocardial infarction: clinical impact and angiographic predictors. Am Heart J. 2006;151:153–7.
Hahn JY, Chun WJ, Kim JH, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (Coronary Bifurcation Stenting). J Am Coll Cardiol. 2013;62(18):1654–9.
Rudnick M, Feldman H. Contrast-induced nephropathy: what are the true clinical consequences? Clin J Am Soc Nephrol. 2008;3(1):263–72.
Laskey WK, Jenkins C, Selzer F, Marroquin OC, Wilensky RL, Glaser R, Cohen HA. A pharmacokinetically based risk factor for prediction of early creatinine increase after percutaneous coronary intervention. J Am Coll Cardiol. 2007;50(7):584–90.
Gurm HS, Dixon SR, Smith DE, Share D, Lalonde T, Greenbaum A, Moscucci M. Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2011;58(9):907–14.
Brunel P, Lefevre T, Darremont O, et al. Provisional T-stenting and kissing balloon in the treatment of coronary bifurcation lesions: results of the French multicenter “TULIPE” study. Catheter Cardiovasc Interv. 2006;68:67–73.
Burzotta F, Trani C, Sianos G. Jailed balloon protection: a new technique to avoid acute side-branch occlusion during provisional stenting of bifurcated lesions. Bench test report and first clinical experience. EuroIntervention. 2010;5(7):809–13.
Goldenberg I, Chonchol M, Guetta V. Reversible acute kidney injury following contrast exposure and the risk of long-term mortality. Am J Nephrol. 2009;29:136–44.
Gruberg L, Mintz GS, Mehran R, Gangas G, Lansky AJ, Kent KM, Pichard AD, Satler LF, Leon MB. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol. 2000;36:1542–8.
Senoo T, Motohiro M, Kamihata H, Yamamoto S, Isono T, Manabe K, Sakuma T, Yoshida S, Sutani Y, Iwasaka T. Contrast-induced nephropathy in patients undergoing emergency percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol. 2010;105:624–8.
Owen RJ, Hiremath S, Myers A, Fraser-Hill M, Barrett BJ. Canadian Association of Radiologists consensus guidelines for the prevention of contrast-induced nephropathy: update 2012. Can Assoc Radiol J. 2014;65(2):96–105.
Gurm HS, Dixon SR, Smith DE, Share D, Lalonde T. Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2011;58(9):907–14.
Ogata N, Ikari Y, Nanasato M, Okutsu M, Kametani R, Abe M, Uehara Y, Sumitsuji S. Safety margin of minimized contrast volume during percutaneous coronary intervention in patients with chronic kidney disease. Cardiovasc Interv Ther. 2014;29(3):209–15.
Kawase Yoshiaki, Matsuo Hitoshi, Teramoto Tomohiko, Matsuda Osamu, Suzuki Yoriyasu, Tsuchikane Etsuo, Suzuki Takahiko. The achievability of minimum contrast procedures for the prevention of contrast Induced nephropathy in patients with chronic kidney disease: a prospective, multicentre trial. J Cardiovasc Dis Diagn. 2014;2:183.
Kang SJ, Mintz GS, Kim WJ, et al. Preintervention angiographic and intravascular ultrasound predictors for side branch compromise after a single-stent crossover technique. Am J Cardiol. 2011;107(12):1787–93.
Singh J, Patel Y, Depta JP, et al. A modified provisional stenting approach to coronary bifurcation lesions: clinical application of the “jailed-balloon technique”. J Interv Cardiol. 2012;25(3):289–96.
Colombo A, Moses JW, Morice MC, et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004;109:1244–9.
Chaudhry EC, Dauerman KP, Sarnoski CL, et al. Percutaneous coronary intervention for major bifurcation lesions using the simple approach: risk of myocardial infarction. J Thromb Thrombolysis. 2007;24:7–13.
Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, Chae IH, Choi DJ, Tahk SJ, Oh BH, Park YB, Kim HS. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29(6):726–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflict of interest to disclose with respect to this paper.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revision. All institutional and national guidelines for the care and use of laboratory animals were followed.
Informed consent
Informed consent or substitute for it was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Omori, H., Kawase, Y., Tanigaki, T. et al. The utility of a jailed pressure wire technique for the treatment of coronary bifurcation lesion in a patient with chronic kidney disease. Cardiovasc Interv and Ther 32, 269–273 (2017). https://doi.org/10.1007/s12928-016-0413-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-016-0413-1





