Abstract
A patient with no conventional cardiovascular risk factors presented with inferior ST-elevation myocardial infarction which was finally diagnosed as a case of essential thrombocytosis. This case demonstrated that thrombectomy alone was sufficient for the treatment of his coronary occlusion. Furthermore, this case report highlights the importance of evaluating rare causes of myocardial infarction other than atherosclerosis and that internists and cardiologists should be aware of essential thrombocytosis as a known cause of myocardial infarction, particularly in patients with no underlying cardiovascular risk factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Case presentation
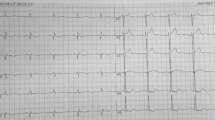
A 40-year-old man without significant medical history presented to the emergency department with retrosternal chest pain associated with nausea and vomiting started 3 h prior to his admission. He had no cardiovascular risk factors. His HbA1c was in normal range. His initial blood pressure and pulse rate were 95/70 mmHg and 60 beats/min, respectively. The remainders of his physical examination were unremarkable. Initial ECG revealed normal sinus rhythm, ST-segment elevation in leads II, III, AVF and V3R-V6R, consistent with inferior and right ventricular (RV) ST-elevation myocardial infarction (STEMI).
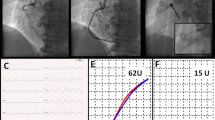
Aspirin 325 mg and clopidogrel 600 mg were administered and the patient was transferred to the cardiac catheterization laboratory for primary percutaneous coronary intervention (PCI). His angiogram showed large amount of thrombus in the mid-portion of right coronary artery (RCA) with 100 % occlusion of distal posterior descending artery (PDA). Left coronary angiography revealed no significant stenosis (Fig. 1). After administration of 5000 units IV heparin, PCI was started with aspiration thrombectomy using 6F Export catheter (Medtronic C. Ltd.). After thrombectomy, TIMI flow grade 2 was established. Due to a large thrombus burden, the decision was made to aggressively treat him with antithrombotic therapy before stenting was attempted to reduce the risk of persistent no reflow as the patient was asymptomatic at that time. Intravenous heparin, 600 units/h, was continued to maintain a plasma thromboplastin time (PTT) at 1.5 times of control. Ebtifibatide 2 mg/kg/h was also given for 24 h. Visible thrombus could be seen after removal of intracoronary thrombus in the aspiration catheter.
The patient was free of symptoms with ST-segment resolution in his ECG. Furthermore, the patient was treated with Aspirin (80 mg/daily), clopidogrel (75 mg/daily), valsartan (40 mg/daily) and atorvastatin (40 mg/daily). Trans-thoracic echocardiography revealed ejection fraction of 40–45 % with akinesia of the inferior and base of inferoseptal wall. Initial laboratory data showed: hemoglobin of 14.9 g/dL, white cell count of 16.4 th/mm3, platelet count of 1,056,000 µL, TG = 167 mg/dl, LDL = 135 mg/dl, HDL = 45 mg/dl, CKMB of 200 mg/dL, CPK of 1094 U/L and Troponin-I (TnI) level of 86.4 ng/mL. During his entire hospital course, platelet count remained highly elevated. His peripheral blood smear examination confirmed the diagnosis of essential thrombocytosis (Fig. 2). His genetic testing showed JAK-2 and BCR/AB mutations confirming the diagnosis of essential thrombocytosis. He was stable after his PCI with no complications such as arrhythmia, angina, or heart failure during his hospitalization. Three days later, the patient underwent repeated coronary angiography to evaluate RCA patency and any potential need of stenting. Coronary angiography revealed patent RCA and PDA with no residual stenosis with the presence of TIMI 3 flow (Fig. 3). Hydroxyurea (1000 mg twice daily) was added to his treatment and he was discharged in a stable condition after 5 days. Sixteen days later, his platelet counts were 850,000 µL, with no cardiac symptoms.
Discussion
ST-segment elevation MI due to non–atherosclerotic origin is a rare condition that needs to be considered in younger population. Thrombocytosis is one of these rare conditions that classifies into essential thrombocytosis and reactive thrombocytosis [1, 2].
Essential thrombocytosis (ET) is a myeloproliferative disease that predisposes affected patients to a variety of complications, including thrombosis [3]. Due to high platelet counts, essential thrombocytosis can lead to myocardial infarction [4–7]. The incidence of acute coronary events reported to be near 9.4 % which increases with aging [5, 8]. The median age of these patients with ET is 60 years and 10–25 % of patients are <40 years of age while one-third of patients are asymptomatic [9]. The relationship of the disease with the JAK2 V617F mutation is prominent. This mutation is present in 50–60 % of ET cases. This disorder may lead to the formation of thrombus and acute arterial occlusion, as well as hemorrhagic complications, probably as a result of platelet dysfunction. Therefore, stenting in these patients can complicate the treatment as these patients are at higher risk for thrombosis and bleeding at the same time [2–4, 8, 9]. The incidence of thrombosis is usually increased when platelet count is more than 6,000,000/µL [2]. Scheffer et al. [10] reported that all patients under 50 years of age with thrombocythemia and acute MI had normal coronary arteries or one-vessel disease; The LAD artery was occluded in most of the patients presenting with MI and ET. It has been reported that hypertension and smoking are risk factors for thrombosis development in these patients. It is important that every effort should be made to reduce large thrombus burden in these patients. If mechanical thrombectomy fails to clear the thrombus within the vessel wall, local thrombolysis given directly into the coronary can be effective in refractory cases that can lead to restoration of the coronary. Intensive antithrombotic treatment of these patients with administration of GPIIb/IIIa inhibitors can facilitate thrombolysis.
We presented a patient with no conventional cardiovascular risk factors, who developed STEMI and was finally diagnosed as a case of ET. Furthermore, our case demonstrated that thrombectomy alone can be sufficient treatment in these patients. This case report highlights the importance of evaluation of rare causes of myocardial infarction other than atherosclerosis. Internists and cardiologists should be informed of essential thrombocytosis as a known cause of myocardial infarction, particularly in the setting of no underlying cardiovascular risk factors. No intracoronary imaging was performed during this procedure. Certainly, intracoronary imaging such as intravascular ultrasound or optical coherence tomography could be helpful for evaluating endothelial structure and presence of any atherosclerosis.
There is not enough data about long-term treatment and follow-up of these patients [11, 12]. Aggressive treatment with antiplatelet agents in the presence of ET is recommended to minimize the risk of thromboembolic events. In patients with high vascular risk including those with the history of previous thrombosis, persistent platelet counts >1,500,000 and age >60 years, aspirin is beneficial. In the absence of the above factors, patients can be divided into low risk (age < 40 years) and intermediate risk (age 40–60 years) population. The effect of clopidogrel or/and statin treatment in this patient population remains unknown.
References
Kumagai N1, Mitsutake R, Miura S, Kawamura A, Takamiya Y, Nishikawa H, et al. Acute coronary syndrome associated with essential thrombocythemia. J Cardiol. 2009;54(3):485–489.
Douste-Blazy P, Taudou MJ, Delay M, Pris J, Sie P, Ribaut L, et al. Essential thrombocythaemia and recurrent myocardial infarction. Lancet. 1984;2(8409):992.
Sanchez S, Ewton A. Essential thrombocythemia. Arch Pathol Lab Med. 2006;130:1144–50.
Daya SK, Gowda RM, Landis WA, Khan IA. Essential thrombocythemia-related acute ST-segment elevation myocardial infarction. A case report and literature review. Angiology. 2004;55(3):319–23.
Mizuta E1, Takeda S, Sasaki N, Miake J, Hamada T, Shimoyama M, et al. Acute myocardial infarction in a patient with essential thrombocythemia: successful treatment with percutaneous transluminal coronary recanalization. Circ J. 2005;69(8):1000–1002.
Bildirici U, Celikyurt U, Ural E. Essential thrombocythemia: a case of acute ST-segment elevation myocardial infarction in a young female. Clin Cardiol. 2009;32(2):104–5.
Pande S, Joshi R, Pande R. Essential thrombocythemia in a young man treated for myocardial infarction. BMJ Case Rep. 2010. doi:10.1136/bcr.09.2009.2234.
Cortelazzo S, Viero P, Finazzi G, D’Emilio A, Rodeghiero F, Barbui T. Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J Clin Oncol. 1990;8(3):556–62.
Alvarez-Larrán A, Cervantes F, Bellosillo B, Giralt M, Juliá A, Hernández-Boluda JC, et al. Essential thrombocythemia in young individuals: frequency and risk factors for vascular events and evolution to myelofibrosis in 126 patients. Leukemia. 2007;21(6):1218–23.
Scheffer MG, Michiels JJ, Simoons ML, Roelandt JRTC. Thrombocythemia and coronary artery disease. Am Heart J. 1991;122:573–6.
Tefferi A, Fonseca R, Pereira DL, Hoagland HC. A long-term retrospective study of young women with essential thrombocythemia. Mayo Clin Proc. 2001;76(1):22–8.
Landolfi R, Di Gennaro L. Prevention of thrombosis in polycythemia vera and essential thrombocythemia. Haematologica. 2008;93(3):331–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khaheshi, I., Memaryan, M., Taherkhani, M. et al. Acute ST-segment elevation myocardial infarction as the first manifestation of essential thrombocytosis successfully treated with thrombectomy alone. Cardiovasc Interv and Ther 31, 275–278 (2016). https://doi.org/10.1007/s12928-015-0347-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-015-0347-z