Abstract
Rapid developments of biomedical science have initiated different fora to take stand on the protection of human rights and human dignity. In front of the new genomic era with the completion of the Human Genome Project in 2003, a plethora of instruments addressing human genetic testing emerged, some looking suspiciously like legal acts. The notion of genetic exceptionalism was characteristic to the normative reactions in the legal acts, but it can be questioned how justified this is. Despite the critique on genetic exceptionalism, it is argued that in certain situations detection of a serious genetic anomaly may cause extra anxiety in a person tested, if the knowledge has a great significance also to family members. Regulative needs should depend on the context and purpose of the test. This review examines the legal framework governing the use of genetic tests in the clinical setting in Western Europe. Five countries have enacted genetic specific laws, and three have comprehensive provisions pertaining genetic testing in their biomedical legislation. Central provisions cover informed consent, autonomy and integrity of the person tested, further uses of tests results, quality requirements of the personnel and facilities involved. Moreover, contemporary challenges related to whole genome sequencing, direct-to-consumer genetic tests and insurance are briefly discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Challenging regulatory target
The Human Genome Project was completed in 2003. At the time, the preface to World Health Organization report envisaged that “The International Human Genome Project (HGP) will rapidly make genetic information available on a worldwide scale previously impossible to imagine. All adults have a right, if they so choose, to know their genetic makeup and implications for the health of their potential offspring, to be educated about their own genetics, and to have the services available to act upon their knowledge.” (WHO 2003). The new genomic future seemed promising, but also frightening; thus regulation was demanded and guidelines were created. However, legal scholars argue that the regulatory response reflects unfounded genetic exceptionalism (Gostin and Hodge 1999; Laurie 2002; Knoppers and Saginur 2005; Rothstein 2005; Krajewska 2009). Gostin and Hodge (1999, p. 31) define genetic exceptionalism to refer to the societal practise of treating genetic data as different from other types of health data for the purposes of assessing privacy and security protections.
The codes of human beings have turned out to be much more complex than anticipated. And so-called junk-DNA was not that junk at all. Now, key focus of modern genetic research is in the epigenetics, the non-DNA-sequence-related hereditary, that is believed to control gene expression, impacting developmental events and diseases (Feinberg 2008). Lots of important findings have been made, but the risk estimates of underlying genetic contribution to most studied diseases are still regarded unstable (Kraft and Hunter 2009). Whole genome sequencing may soon be an option for a disease-specific genetic testing (Lifton 2010), but it raises new ethical and legal questions, such as what to do with all the additional information the significance of which is not clear at the time of testing, how to handle incidental findings, and the storage and future use of samples and data.
Genetic testing can be performed for many different purposes within and outside medical field. Thus, regulative needs depend on the context in which the test is being performed and for which purpose: medical-nonmedical purposes, tests to detect monogenic diseases, predispositions or carrier tests, predictive tests for late onset diseases, diagnostic and treatment purposes, drug response, family planning, population screening, forensics, and DNA profiling or research. Also stakeholders involved are many: individuals and their family members, biotechnological research and industry, criminal investigation, insurance, and employers. Hence, trying to make policies and govern the use of genetic information is a challenging mission since the basic question is what is we are trying to regulate and why and what are we trying to protect.
Furthermore, lack of generally approved definition of a genetic test makes the analysis of different regulations demanding. Many have tried to define the concept of genetic testing, but without generally approved results. A European Union (EU)-funded project, EuroGentest, had as one of its objectives to analyse definitions of genetic tests, and try to develop at least some key elements for a working definition (Pinto-Basto et al. 2010). Use of genetic information in different contexts is also challenged by the confusing and contradictory terminology in different regulatory instruments, a phenomen called ‘The Babel of genetic data terminology’ in a seminal article of Knoppers and Saginur (2005).
Regulation of medical practice is mostly based on long western medical ethics stemming from at least the Hippocrates Oath 500 aD, i.e. do good, avoid harm, keep professional secrecy. Modern medical ethics started rapidly developing after the Second World War along with human rights and birth of ethical codes and committees. A strong doctrine of informed consent to medical interventions was born, be it for clinical or research purposes. The outcome of Nurnberg Trials is considered the core of modern medical research ethics, and it paved the way for the World Medical Association’s Helsinki Declaration, which has de facto become institutionalised in national and EU legislation. Rapid development of biomedical science has initiated different fora to take stand on the protection of human rights and human dignity. As a consequence, a plethora of instruments addressing genetic testing has emerged, some looking suspiciously like a legal act. That said, the binding legal framework in Western Europe is, principally, composed of national laws, European Union law, and international law. Different forms of soft law complete the regulatory scenery and guide practices. Indeed, professional guidelines are interesting in this regard, as Article 4 the Biomedicine convention obligates to follow relevant professional obligations and standards in the interventions in the health field, research included. Also, the rulings of the European Court of Justice and European Court for Human Rights influence the legal situation.
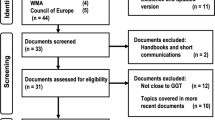
In this review, I will examine the legal framework governing the use of genetic tests in Western Europe. Footnote 1 I have examined national legal acts specific to genetic testing in the clinical setting, not in research, and not sporadic provisions in separate acts, nor recommendations and policies.
Transnational regulation and norm-setting instruments
European Union
According to Article 168 of the Treaty on the Functioning of the European Union (later referred to as TFEU), a high-level human health protection shall be ensured in the definition and implementation of all Union policies and activities. Still, the actions of the EU in the health field are, under EU law, complementary to those of the member states, and limited to the common safety concerns as defined in Article 168.4 TFEU, including setting high standards of quality and safety for medicinal products and devices for medical use. For instance, Directive (98/79/EC) on in vitro diagnostics devices stipulates essential requirements of genetic tests that are put on the market or on the service. It is not applied to in-house tests and tests only for research purposes. The IVD directive, however, focuses on the safety aspect of the genetic tests as a device, as a product, when used for medical purposes, while aspects related to the quality, validity and utility of such a test are not governed.
Moreover, Directive 98/44/EC on the legal protection of biotechnological innovations is applied to conditions under which genetic tests can be patented. For ethical and legal issues pertaining patenting and licencing in genetic testing, see Soini et al. (2008).
Data Protection Directive 95/46/EC is applicable on handling the genetic data. Under Article 8(1), data concerning health is regarded as ‘sensitive data’ in the directive, covering hence health-related genetic data. EU’s Article 29 Data Protection Working Party adopted a Working Document on Genetic Data on March 17, 2004, claiming that genetic data has extremely singular characteristics compared to health data and thus calls for reinforced legal protection. It was noticed, however, that genetic data should not be seen in a reductionist way, i.e. having a universal explanatory value of human life. All in all, many key challenges of the use of genetic testing are discussed in the document, even though the argumentation reveals strong genetic exceptionalism. Interestingly, at the same time, a working group invited by the European Commission gave 25 recommendations on the ethical, legal and social implications of genetic testing (EC Expert Group 2004) and stated that the notion of genetic exceptionalism is inappropriate and should thus be avoided. Instead, the EC Expert Group claimed equally high protection for all medical data.
In November 2010, European Commission made an initiative to start revisiting the legal framework for data protection. Amongst the issues is whether genetic data should be explicitly considered as ‘sensitive data’, widening it then to also to other than health information. The Commission is anticipated to give a proposal for a new legal framework in the early 2012. Given the current ambiguity of the EU stand, it will be interesting to see what kind of an input the Article 29 Data Protection Working Party is going to give on this round, and whether it will affect the treatment of genetic information in the EU.
In the primary law of EU, Article 3 of the EU Charter of fundamental rights (2010/C 83/02) captures the core rules on the right to the integrity of the person as follows:
-
1.
Everyone has the right to respect for his or her physical and mental integrity
-
2.
In the fields of medicine and biology, the following must be respected in particular:
-
The free and informed consent of the person concerned, according to the procedures laid down by law
-
The prohibition of eugenic practices, in particular those aiming at the selection of persons
-
The prohibition on making the human body and its parts as such a source of financial gain
-
The prohibition of the reproductive cloning of human beings
-
In addition, Article 21 of the Charter bans discrimination:
Any discrimination based on any ground such as sex, race, colour, ethnic or social origin, genetic features , language, religion or belief, political or any other opinion, membership of a national minority, property, birth, disability, age or sexual orientation shall be prohibited.
Despite the lack of specific genetic legislation at EU level, data protection and discrimination provisions are relevant when handling and using genetic data: genetic data pertaining health is ‘sensitive data’ under EU data protection directive, and is thus to be treated confidentially. Likewise, discrimination based on genetic features is prohibited in the EU member states.
UNESCO
The United Nations Educational, Scientific and Cultural Organisation (UNESCO) is concerned with moral issues in relation to science, and for that matter, it has developed international normative standards for the use of biomedical applications. Central instruments of UNESCO in the field of bioethics are Universal Declaration on Bioethics and Human Rights (2005), the International Declaration on Human Genetic Data (2003) and the Universal Declaration on the Human Genome and Human Rights (1997), the latter being endorsed also by the General Assembly of the United Nations in 1998.Footnote 2
Nevertheless, the approach of UNESCO pursues genetic exceptionalism. Article 4 of the International Declaration on Human Genetic Data attaches special importance to the human genetic data because they can be predictive of genetic predisposition; they may have a significant impact on the family members and group of persons; they may contain information the significance of which is not known; and they may have cultural significance. Despite this critique, the instruments that UNESCO has issued are helpful for policy makers as they can serve as benchmarks in front of the novel applications. In fact, they have been a stimulus for national legislation in many countries throughout the world even though they are not legally binding nor can they be ratified as such.
Council of Europe
The Council of Europe has been active in the bioethical arena since 1985. Both the Parliamentary Assembly and the Committee of Ministers have issued tens of recommendations in this field. The Committee of Ministers’ Recommendation No. R (97) 5 on the protection of medical data is applicable to the collection and automatic processing of medical data, genetic data included. The expression of genetic data is defined to ‘refer to all data, of whatever type, concerning the hereditary characteristics of an individual or concerning the patterns of inheritance of such characteristics within a related group of individuals’. It contains special provisions on collection, procession and use of genetic data, and on incidental findings of genetic analyses. All in all, approach to the use of genetic data in the recommendation is similar to other medical data, with a few exceptions. For instance, the recommendation states that the use of genetic data for forensic purposes shall be governed by law. Further, it is recommended that the person subjected to genetic analysis should be informed of unexpected findings, if this is not forbidden in the domestic law, the person has asked this information, and the information is not likely to cause serious harm on his or her health or to his or her close relatives. The Committee of Ministers’ Recommendations are not binding, but they often have impact as soft law instruments since they reflect the collective position of the governments of the member states (Benoît-Rohmer and Klebes 2005, p. 108-109). Indeed, the recommendation has been referred to at least in the Finnish legislative procedures.
The Council of Europe Convention on Human Rights and Biomedicine (ETS No. 164, 1997, later referred to as the Biomedicine Convention) is often claimed to be the first international legally binding instrument in the field of biomedicine. However, as subject to the international treaty law, it becomes a binding national law in a certain country only if the country ratifies it. For instance, Germany and the UK have not even signed the Biomedicine Convention, and France has only signed it. Yet, at the moment, 28 countries have ratified it.Footnote 3 The Biomedicine Convention has been later completed by various protocols. These protocols are subject to same ratification procedures as the Biomedicine Convention itself.
The Biomedicine Convention has relevant provisions on genetic testing. Article 12 of the Convention limits the use of predictive genetic tests to “tests which are predictive of genetic diseases or which serve either to identify the subject as a carrier of a gene responsible for a disease or to detect a genetic predisposition or susceptibility to a disease may be performed only for health purposes or for scientific research linked to health purposes, and subject to appropriate genetic counselling”. Thus, Article 12 is legally binding rule in the 28 countries that have ratified it.
According to article 23 of the Biomedicine Convention, countries bound by it shall provide appropriate judicial protection for infringements of the rights and principles of the convention.
The Council of Europe gave an additional protocol to the Biomedicine convention on genetic testing for health purposes (CETS No. 203, later referred to as the Protocol) in 2008. The general objective is to protect against improper use of genetic tests. Member states to the Council of Europe who have ratified the Biomedicine Convention can ratify this protocol to enforce it in their own jurisdiction.
Under article 2, the Protocol applies to tests, which are carried out for health purposes, involving analysis of biological samples of human origin and aiming specifically to identify genetic characteristics of a person, which are inherited or acquired during early prenatal development. Test fulfilling this definition are called genetic tests in the protocol. Central to the definition is that tests are performed for health purposes. Thus, tests to determine sports genes or other nonmedical conditions are not covered.
Article 5 requires that parties to the Protocol take the necessary measures to ensure that genetic services are of appropriate quality, scientifically and clinically valid, there are quality assurance programme, and persons providing these services have appropriate qualification. Article 6 sets clinical utility as an essential criterion for deciding to offer the test in the first place. Under the explanatory report, the assessment of the clinical utility of the genetic tests shall be assessed on an individual basis, and paying attention to social and cultural aspects. The point is then to consider if the test can guide the person to choose preventive or therapeutic strategies.
As regards the direct-to-consumer (DTCs) genetic tests, the Article 7 of the Genetic testing protocol is central: it sets forth that a genetic test for health purposes may only be performed under individualised medical supervision. This is the basic rule, and exemptions include a test that would not have important implications for the health of person concerned or members of their family or with important implications concerning procreation choices.
The Protocol also establishes an obligation to parties to facilitate access to objective general information on genetic tests, including their nature and the potential implications of their results. The Protocol thus offers an excellent framework to develop criteria and conditions for legislation regarding genetic tests in general, and direct-to-consumer tests in particular (of these DTC tests see later). So far, only five member states have signed the Protocol, Finland representing the only Nordic country, so the protocol is not yet in force. This is a pity, because the Protocol is thoroughly drafted and reflects considerations of a multidisciplinary expert working group during many years.
National legislation
First explicit law in the area of bioethics was enacted in France in 1994 (Loi 94-653 and 94-654, major revisions in 2004 and 2011). Biomedical regulation has also been adopted in Norway (Bioteknologilov 2003) and Spain (Ley 14/2007 de investigación biomedical). All these three acts contain several provisions related to genetic testing. As yet, most countries have applicable provisions for the genetic testing in the general legal framework governing activities and professionals in the health field, and other legislation, such as in vitro fertilization (IVF; e.g. conditions for PGD), data protection, patient rights, and penal code (e.g. discrimination). Lately, some countries have adopted specific laws on genetics, such as Austria, Germany, Portugal, Sweden and Switzerland (Table 1). In 2012, the Czeck Republic is also enforcing a special healthcare act that will provide a sound and modern legal framework for genetic testing. To the author’s knowledge, special provisions on genetic testing exist also in Bulgaria.
Austria
The Austrian Gene Technology Act (GTG, Gentechnikgesetzes BGBl. Nr. 510/1994, as revised later) came into force in 1995. It covers a wide range of genetic applications not limited to human medicine and stipulates also the use genetically modified organisms. GTG is completed by the Austria Book of Biotechnology (Gentechnikbuch)Footnote 4 published by the Advisory Board on Biotechnology. The normative status of the Gentechnikbuch is derived from the GTG, thus making it a legally valid normative instrument. The Gentechnikbuch presents the state of the art (‘der Stand von Wissenschaft und Technik’) of genetics and is updated by the Advisory Board of Biotechnology, also established by GTG. Chapter IV governs genetic testing and gene therapy on humans. Article 65 limits genetic testing on humans for medical purposes only to be performed in accordance with the established state of the art. The genetic tests are classified into four different types depending on the clinical purpose and availability of therapeutic measures. Article 67 prohibits explicitly employers and insurance companies to ask and access genetic information. Moreover, GTG sets requirements to the informed consent, qualification of the involved medical specialists and laboratories, and compulsory registers of the facilities providing services.
The Austrian Act regulates genetic activities in a rather strict and detailed manner. The institutions performing genetic services need to be licenced, and their staff and facilities shall comply with the legal requirements.
France
The French legislation governing genetic testing is based on the Bioethical Act that modified the Civil Code and Public Health Code in 2004 (Loi 2004-800 relative à la bioéthique modifying code civil and code de la santé publique). These codes were recently revised with an impact on genetic testing provisions (LOI n° 2011-267 du 14 mars 2011 d’orientation et de programmation pour la performance de la sécurité intérieure (1), Chapitre III: utilisation des nouvelles technologies, Section 1: identification d’une personne par ses empreintes genetiques and LOI n° 2011-814 du 7 juillet 2011 relative à la bioéthique). Article 16-10 of the civil code limits examination of a person’s genetic characteristics only for medical purposes or scientific research. An explicit written consent is required after the person is informed about the nature and finality of the examination. However, genetic ‘fingerprint’ of a person may be used for identification purposes under limited situations (Art 16-11). Article 1131-1 of the Public Health Code stipulates the use and communication of the person’s genetic information. Identification based on genetic information after death is in principle subject to the person’s consent given during lifetime. A violation of these norms may result in 1 year of imprisonment and fines of 15,000 Euros under penal code. The French provisions also set forth licencing and professional requirements on medical doctors operating who perform genetic tests.
In case a serious genetic anomaly is diagnosed that could pose a potential risk also to family members, the doctor is obliged to give the patient a written document informing of the risks, if the patient does not tell his family members who could benefit of preventive measures. A specific medical information process is available via the Biomedical Agency (l’Agence de la Biomédicine) in such cases, if the patient so prefers. It is specifically stated in the law that the patient cannot be charged with responsibility to give the information of his genetic anomaly to anybody. Thus, the information procedure is only an option in case the patient finds it difficult to give the information himself. This provision has been questioned by Francois Vialla (2006, p. 25) who asks why an HIV-positive patient hiding his condition from his or her partner can be charged with a civil and criminal responsibility while the opposite applies to a person with a serious genetic anomaly, who does not want to disclose the information to his or her close relatives even though a therapeutic or preventive cure exists to help dealing with the anomaly.
Germany
The German law is also very detailed and comprehensive (Gendiagnostikgesetz-GenDG 374/09).Footnote 5 The purpose of the Act under Article 1 is to determine the requirements for genetic examinations and genetic analyses, and to prevent discrimination and harm on the basis of genetic characteristics with a special regard to the protection of human dignity and right to self-determination. The scope of application of GenDG is for medical purposes, determination of descent, insurance and employment. The act does not apply to research and criminal procedure. The Act covers prenatal genetic examinations and genetic mass screenings. Under Article 7, diagnostic genetic examinations may primarily be conducted only by medical doctors who are certified specialists in human genetics. Article 18 prohibits the use of genetic information in the insurance context, but for certain types of insurance contracts, e.g. life insurance with a significant premium, the insurer may demand and use results of a previously conducted genetic test. In several provisions, the German lawmaker refers to ‘the generally accepted status of science and technology’. An Independent Genetic Diagnostics Commission at Robert Koch Institute, established under Article 23, is to assess this ‘generally accepted status of science and technology’. Like in Austria, this solution allows for the necessary flexibility in legislation when the regulatory target is so fluid.
Norway
Genetic testing in Norway is governed by Chapter 5 of the Biotechological Act (Lov om humanmedisinsk bruk av bioteknologi m.m 2003-12-05 nr 100). Genetic examinations are limited for medical purposes with diagnostic or therapeutic aims. The facilities performing tests shall be licenced. The Act contains provisions on consent, genetic counselling, testing of the children, and informing family members and relatives. Under Article 5-9, the patient decides if he or she wants to inform his or her relatives of the detected hereditary disease in the family. If the patient cannot or does not want to inform the relatives, the healthcare personnel can do that, provided that the condition in question is enlisted by the health department. In exceptional cases, the healthcare personnel can also inform the relatives if the patient cannot consent to the disclosure of the information.
Portugal
Portugal issued the Personal Genetic Information and Health Information Act in 2005 (Lei No 12/2005 de Janeiro). The Act governs performance of the genetic tests, use of genetic information and conduction of research in rather a detail in 22 articles. Genetic information may be obtained in many ways, but under Article 6, predictive tests to determine predispositions to common diseases, and presymptomatic tests for monogenic tests are excluded from the notion of genetic information. Genetic counselling shall accompany genetic testing. Insurance companies are not allowed to seek genetic information and employers only for justified health and safety purposes. Testing minors requires specific consideration as to the benefit of test. For instance, severe incurable late onset diseases shall not be tested.
Spain
Genetic testing in Spain is governed by the Act on Biomedical Investigations (Ley 14/2007 de Investigación Biomédica). The Aim of the Act is to protect dignity and identity as well as inherent rights of the human being. Under Article 1.2, the Act is applied to genetic analysis and handling of genetic data exclusively in the healthcare setting. Under Article 9, the genetic analysis shall fulfil the criteria of appropriateness, quality, equality and accessibility. Specific provisions are in Chapter II, Article 46-57. The patient shall be given written information on the nature and finality of the test, possibility of unexpected findings, and potential implications to the family members. Also, the consent to the test shall be express and specific in a written form. Further, it is stipulated that the patient has the right to know or not to know the personal genetic information obtained by the test. However, in case the patient has chosen not to know, his family members may be informed if the information is deemed necessary for them to avoid a serious harm. The Act contains provisions on handling the confidential data, genetic counselling and genetic screening. Finally, it also sets forth that performance of genetic tests as well as the genetic counselling shall be provided by qualified personnel in accredited centres.
Sweden
The Genetic Integrity Act came into force in 2006 (Lag om genetisk integritet m.m (2006:351)). It stipulates on the restrictions to certain uses of biotechical developments for medical purposes and on certain legal consequences related thereto. The aim of the Act is to safeguard person’s integrity. The Act was preceded by a thorough governmental proposal (Prop. 2005/06:64). Among the argumentation in the proposal regarding genetic integrity, the lawmaker discusses human dignity and genetic integrity, and concludes that the genetic code determines the uniqueness and identity of a human being. The mere risks of misuse and discrimination compose a threat to the integrity. It is the genetic component that is regarded unique. Moreover, self-determination is emphasised to be as one of the central ethical issues related to genetic integrity. The classic ‘right-to-know’ and ‘right-not-to-know’ are mentioned as a core to the principle of self-determination. Here again, genetic knowledge is deemed to require special provision.
The scope of application is the use of genetic analyses and information and gene therapy, genetic studies in general health examinations, PND and PGD, research and processing of ovocytes, insemination and IVF. Also, the Act contains provisions regarding responsibility for trade of human biological material.
A general principle set forth in Article 2:1 prohibits the use of or demanding genetic information without a support of legal provision as a precondition for any agreement. Genetic information can be used for risk evaluation in person insurance in certain cases (insured is over 18 years old and the insurance amount is significant). Genetherapy and research to develop therapies that have capacity to modify the human germ line is prohibited.
Sweden is the only Nordic country that has not ratified the Biomedicine Convention mostly due to difficulties to comply with some of its provisions (Rynning 2011). Nevertheless, Sweden seems to have followed the provisions of the Biomedicine Convention closely when drafting legal acts, such as Act on Genetic integrity, or when revising Biobank Act in 2011.
Switzerland
The scope of application of Federal Act on Human Genetic Analyse (Loi fédérale sur l’analyse génétique humaine (LAGH)i du 8 oct 2004 (1.4.2007)) is human genetic analyses performed in the field of medicine, employment, insurance. In addition, it addresses civil liability. Research is explicitly excluded. An authorisation to perform genetic analysis is required by a competent federal authority.
The purpose of LAGH is to assure protection of human dignity and personality, to prevent abusive genetic tests and abusive use of genetic information, and to guarantee the quality of genetic analyses and their intepretation.
Article 3 of LAGH contains a long list of definitions. It prohibits discrimination on the basis of genetic heritance. It contains provisions on consent, on the right not to know and protection of genetic information. Use of in vitro device outside a relevant professional practise is in principle prohibited save for some exceptions. Even then, the use of in vitro device shall always happen under medical control and all possibilities for misintepretations shall be excluded.
Similar to all the examined acts in this review, performance of genetic analyses is limited to medical purposes. Minors should not be tested unless his protection so requires. In exceptional cases when no other means exist to detect a serious hereditary diseases or a carriership to such a disease, the test may be performed. Article 12 sets specific conditions on genetic screening programmes.
According to article 13, a genetic analyses may only be prescribed by, or under surveillance of, a licenced doctor. Presymptomatic genetic analyses, prenatal genetic analyses or analyses for family planning may only be performed by, or under surveillance of, a doctor of appropriate post-graduate formation. The doctor prescribing the analyses shall take care that the patients receive genetic counselling.
Article 14 sets a general requirement for a genetic counselling prior to genetic analyses (presymptomatic, prenatal, family planning). Counselling shall be given by a non-directive manner by a qualified person. The article contains detailed requirements for the counselling in general, completed by following articles applicable in specific circumstances (e.g. PGD).
Article 19 concerns communicating the results of genetic analyses. As a principle, a doctor is not allowed to disclose the results of a genetic analyses to other than the person tested or his legal representative. With the consent of the person, the results can be disclosed to his family members, spouse or partner. If the person in question refuses to disclose such information to the persons mentioned above, even though the protection of their important interests would require such information, the doctor may ask the cantonal authority to be free from the professional secrecy obligation. This is a unique way of dealing with these delicate situations, and in my opinion, also an appropriate way from the point of view of a medical doctor to solve the ethical dilemma.
Re-use of biological material shall in principle according to Article 20 comply with the person’s consent. However, genetic analyses of such material may be performed for research uses if the material is anonymised and the person in question has been informed of his rights and he has not expressly opposed. Research regulations shall also be applied.
Article 21-25 concern genetic analyses in the employment field. As a main rule, when making, or during the course of, an employment contract, the employer or the doctor of the employer are not allowed to demand a presymptomatic genetic analysis, to demand results of such an analysis if already performed, or to demand a genetic analysis to determine the characteristics of an employee not relevant to health. Exemptions include occupational diseases relevant to a certain position.
Articles 26-28 concern use of genetic analyses in insurance. General principle is that an insurance company cannot require genetic analyses as a precondition for an insurance agreement. However, already performed genetic analyses can be taken into account in certain restricted cases.
Federal council appoints under article 35 of the act an independent expert commission for genetic analyses which shall, inter alia, elaborate norms for quality control of genetic analyses, give recommendations, opinions and follow scientific progress and practices, and take legislative initiatives, when deemed necessary. This solution to let an independent source to evaluate and follow scientific progress is similar to ones adopted by Austria and Germany.
Current challenges of regulation
Direct-to-consumers genetic tests
DTC-marketed genetic tests have escalated in recent years and raised a growing concern. They are marketed as to offer determination of an individual risk for many genetic conditions, and hence, the individual could pursue healthier life. A person could, for instance, discover whether he or she has an alcohol flush reaction or male pattern baldness. A child can be tested to find out if he has especially beneficial genes for sports. Risk for more serious conditions can also be tested. However, these tests are rarely diagnostic, i.e. confirm a certain genetic condition. Instead, they indicate risk based on predispositions for common complex diseases, the possible onset of which are influenced substantially by lifestyle and environmental factors. Also the quality and accuracy of these tests may be doubtful. While a total ban has not been demanded, more regulatory control is deemed necessary (Patch et al. 2009). It is generally held important that such tests are brought into some premarket scrutiny for transparent evidence on their validity and utility.
So far, legislation pertaining directly to genetic self-testing is lacking in the European Union. Traditional health laws and professional ethics do not reach this kind of a distance sales contract that consists of selling both device and service; service being the major deliverable. Consumer legislation may be effective against improper marketing within the EU, but most of the DTC companies operate outside the EU. European Group on Ethics in Science and New Technologies (EGE 2003) published a statement on advertising genetic tests via the Internet in 2003. The aim of the statement was to alert civil society and decision makers of the implications of direct-to-consumer genetic tests.
The In Vitro Diagnostic Directive (98/79/EC) is applied to genetic tests also, but because they are classified as a low-risk device, no prior market authorisation is currently needed in the European Union. A research team that explored policy issues around genetic tests for common, complex diseases published its briefing for competent authorities in 2007 (Hogarth and Melzer 2007). They highlighted some major problems in the In Vitro Diagnostics Directive and suggested certain policies for the Commission, i.e. revisiting the risk classification and independent premarket evaluation, introducing a provision of analytic and clinical validity and clarification of some key concepts.
Many instances have addressed the challenges posed by DTC, the Human Genetics Commission in the UK in the forefront. In August 2010, it issued standards for DTC tests called ‘the Common Framework of Principles’ (HGC 2010) which aim at ensuring that people who choose to buy genetic tests themselves can have confidence that the companies selling them follow basic principles of consent, data protection, truth in marketing, scientific rigour and balanced interpretation. The Society of Human Genetics (ESHG 2010) has also addressed this issue in its statement, concluding that DTC tests and the advertisement of genetic tests of unproven benefit or without adequate independent genetic counselling contradict with the professional standards the ESHG sustains. The statement contains a list of policy suggestions for DTC companies.
The additional protocol on genetic testing by the Council of Europe is currently the most important attempt to provide minimum standards also for DTC tests. For instance, demands for quality and clinical utility and for individualised supervision shall be applied to all genetic testing for health purposes, DTS testing included. Article 7 allows exemption for individualised supervision only if testing does not lead to important implications for the person concerned or his family, or for family-planning choices.
In my opinion, paternity tests should always require consent from both the parents and the child when possible. In addition, these tests should be limited to official paternity testing procedures and be performed in an accredited laboratory. Reasoning is that such a test touches immensely the core element of personal identity and family life, and has capacity to ruin the lives of the persons involved if the result is unexpected. Therefore, the performance of such tests should be absolutely controlled and provide accurate results.
To summarise the Western reflections on DTC testing, total ban has not been demanded. Instead, certain issues are considered important to safeguard the interests of the consumer: laboratories performing analyses should comply with quality assurance standards, and companies selling the tests should demonstrate clear privacy policies regarding processing and further uses of personal data and samples. Also, responsible authorities should provide rightful information concerning the tests for consumers in the public.
Whole genome sequencing
Whole genome sequencing (WGS) is anticipated to be soon a more pragmatic and economic alternative to establish a genetic condition behind a certain disease, instead of disease/mutation-specific genetic tests (Lifton 2010). This will evidently create new challenges for governance of genetic information. These include, incidental findings, testing minors, storing and further processing of the information. WGS will evidently result in excess of information. On one hand, it may reveal unexpected things, not related to the conditions examined. There may or may not be therapeutic or preventive measures available to deal with. Such a possibility should be discussed with the patient in advance and agree with him or her as how to handle with such an information. On the other hand, the significance of most information is not known at the time of performance of the test, and thus cannot be communicated to the patient. However, unknown data may later in the course of scientific progress gain significance. Should the patient then be contacted at the later stage with accumulating knowledge and whose responsibility would it be? These questions are particularly difficult when testing minors.
Insurance
The use of genetic information in the insurance context has raised worries. Currently, many insurance companies in Europe have agreed on a moratorium not to require genetic information when making insurance agreements. Nevertheless, one could ask how justified this is compared to other health information. Predictive information vis-à-vis already diagnosed symptomatic genetic diseases are likely to need different approaches. Insurance premiums are determined on pooling the risk among those insured based on the general and individual knowledge of risks at the time of the making the contract. For instance, it is known by public health research that life expectancy of older single males does not reach the level of married men, or that unhealthy lifestyle and obesity are likely to increase risk to cardio-vascular diseases and diabetes. Is using this kind of information discriminatory? Some countries, like Germany, Sweden and Switzerland, explicitly allow for using genetic information for risk evaluation if the insurance amount exceeds certain significant level. Usually this applies for life insurances, illness insurance or insurances to protect incomes in case of disabled to work. Also in the UK, the moratorium does not apply to predictive genetic information when the insurance amount exceeds a certain rather high level. Instead, Austria, France and Portugal explicitly prohibit the use of genetic information for the insurance purposes.
The Council of Europe decided to separate the use of genetic information in the context of insurance and employment from the Protocol on Genetic testing. It is currently working on this issue.
Discussion
The legislation presented above has certain similar characters: their scope of application is mostly limited to tests to establish a medical condition, they aim to protect the autonomy, integrity and privacy of the persons tested, they set requirement of the genetic counselling and they establish mechanisms to safeguard quality of the tests. Many of them pay attention to the interests of the family members. Some laws step further, and allow testing under certain conditions in the context of insurance, like in Germany, Sweden and Switzerland. Even in the absence of genetic-specific laws in other countries, a general legal framework in the health field pertaining the doctor-patient relationship, consent, professional ethics, healthcare performance, confidentiality and privacy is applied to genetic tests as well. Thus, genetic tests are hardly performed in a total legal vacuum in any country. A true legal comparative study would be needed to analyse the societal and cultural factors underlying regulatory responses in different countries.Footnote 6
The expression ‘geneticisation’ has been used to describe a kind of a genetic hype, over-emphasis of genetic component in human life and identity based on the perception that genomic knowledge is exceptional, and determines the course of one’s life, diseases, energy levels, happiness and career. For instance, as Rothstein (2005) points out, a mutation or other impairment in DNA may rather be a symptom of a disease, instead of being a cause for it. Thus, environment along with social conditions have also a huge impact on how our genes express themselves.
Many have argued against raising genetic data into stricter category of health data (Gostin and Hodge 1999; Laurie 2002; Rothstein 2005; Krajewska 2009). In an in-depth analysis, Gostin and Hodge (1999) argue that the hypothesis underlying genetic exceptionalism is flawed and it is not ethically and legally justified to distinct genetic data from other health data. Discrimination on other grounds may at least as devastating to a person. Clinical observations, lifestyle, family history and biometrics provide means to detect and predict a person’s current and future health. The basic rule about non-disclosure of sensitive personal data should apply here as well. Anna Krajewska has suggested that the term genetic information be replaced by the term biological information (Krajewska 2009 p. 25). Moreover, many acts stipulate the right-to-know and not-to-know about the results of genetic tests. The classic medical ethics and patient rights regimes govern the same issue, and I wonder why should there be a need for special provisions. If a person does not want to be informed of her medical condition, be it cancer diagnosis, HIV testing, or a genetic diagnosis, same approach and rules respecting the patient’s self-determination should apply.
Despite the critique regarding genetic exceptionalism, I argue that in certain situations genetic data has elements superseding other health conditions, and may thus generate more anxiety in a person tested. This is the case particularly in serious clear conditions that have great significance for the close relatives. Indeed, the need to pay attention to the interests of the kin is acknowledged in many of the examined legislations, while some stick to strict confidentiality and deny all access of third parties to information without a consent of the person tested.
Given the difficulty of defining the notion of ‘genetic testing’ and rapidly accumulating and sometimes also radically changing scientific knowledge, the regulatory task is not easy. Fear of eugenics is of course understandable cause for regulatory demands due to the rather recent eugenic policies in the beginning of twentieth century, and this history is clearly reflected in the regulation. However, claims of eugenics in the context of contemporary genetics seem to lack profound reasoning about the concept and its meaning (Harper 2008, p. 405-427). The purpose of today’s medical genetics is to alleviate individual suffering which is rather distinct from a coercive state policies targeted against certain groups and populations (WHO 2003, p. 10).
Genetic testing should, as any other healthcare measures, be of appropriate quality and utility. Clinical validity and utility of the research findings shall be held important before consideration of their clinical application (PGH Foundation 2010). This would also need improvement of legislation in this field, as currently research is strictly regulated in Europe, but introduction of genetic tests into clinical practice lack sufficient control. However, some balancing will be needed as a strict scrutiny would raise costs and delay introduction of tests in practice (Cassiman 2011). Appropriate mechanisms for approval of tests for clinical purposes and quality assurance for laboratories and personnel should take place along with oversight mechanisms. Still, regulation should not be too detailed to be flexible in the course of scientific progress. The approach adopted in the Austrian, German and Swiss legislation to leave assessment of the state-of-the-art to an independent multidisciplinary committee established by law seems to provide an evolutionary and responsive mechanism in front of rapidly developing science.
The role of the regulation can be seen as to facilitate practises and secure community interests by setting appropriate conditions and providing a structured framework for the activities in the field of genetics (Morgan and Yeung 2007, p. 4-7). Thus, it serves to provide public confidence.
Asymmetry on information regarding genetic information both among lay people and general practitioners should be given a due regard. This goal is mentioned, for instance in the OECD Guidelines (2007). Use of a parliamentary normative process is likely to ensure the democratic decision making that reflects national attitudes and values. It could be enhanced by deliberative democracy by involving citizens to open discourse at the early stage of the normative process. If norms are developed outside the democratic process, for instance, in the expert instances, the process is not necessarily transparent, the values may not meet those of the citizens, and consequently, they may not be welcomed. Awareness raising and accurate information are crucial for maintaining public trust in science in general and genetics in particular. Approval of genetic applications is hence also a matter of reception.
Notes
For an overview on US legislation, see Hudson 2011
For a timely list of ratifications, see www.coe.int/bioethics
An English translation is at http://www.eurogentest.org/professionals/ethical_and_legal/
Comparative law is a specific legal academic discipline that studies differences of legal systems, legal orders and laws of different countries. It aspires to go further into the local legal culture and history to be able to understand and explain normative structures and solutions in a given country.
References
Benoît-Rohmer and Klebes (2005) Council of Europe law. Towards a pan-European legal area, Council of Europe, Strasbourg
Cassiman J-J (2011) Some considerations about a report on ‘Public health in an era of genomic-based and personalized medicine’ from the Public Health Foundation, Cambridge. J Community Genet 2:107–109
EC Expert Group (2004) 25 recommendations on the ethical, legal and social implications of genetic testing. European Communities, Brussels
EGE - European Group on Ethics in Science and New Technologies (2003) Statement on advertising genetic tests via the internet
European Society of Human Genetics (ESHG) (2010) Statement of the ESHG on direct-to-consumer genetic testing for health-related purposes. Eur J Hum Genet 18(12):1271–1273
Feinberg AP (2008) Epigenetics at the epicenter of modern medicine. JAMA 299(11):1345–1350
PHG Foundation (2010) Public health in an era of genome-based and personalised medicine. ISBN 978-1-907198-06-9. Available at www.phgfoundation.org. Accessed on 15 Sept 2011
Gostin LO, Hodge JG Jr (1999) Genetic privacy and the law: an end to genetic exceptionalism. Jurimetrics 40:21–58
Harper PS (2008) A short history of medical genetics. Oxford University Press, Inc
HGC Human Genetics Commission (2010) The Common Framework of Principles 2010. www.hgc.gov.uk
Hogarth, Stuart and Melzer, David. IVD-directive and genetic testing. Problems and proposals. A briefing presented to the 20th meeting of Competent Authorities Lisbon, July 2007. Available at www.eshg.org. Accessed 27 August 2010
Hudson KL (2011) Genomics, health care, and society. NEJM 365(11):1033–1041
Knoppers BM, Saginur M (2005) The Babel of genetic data terminology. Nat Biotech 23(8):925–927
Kraft P, Hunter DJ (2009) Genetic risk prediction—are we there ye. NEJM 360(17):1701–1703
Krajewska A (2009) Conceptual quandaries about genetic data—a comparative perspective. Eur J Health Law 16:7–26. doi:10.1163/157180909X400204
Laurie, Graeme (2002) Genetic privacy: a challenge to medico-legal norms. Cambridge University Press
Lifton RP (2010) Individual genomes on the horizon. NEJM 362(13):1235–1236
Morgan, and Young (2007) An introduction to law and regulation. Cambridge University Press. Cambridge, UK
Organisation for Economic Co-operation and Development (2007) Guidelines for quality assurance in molecular genetic testing. OECD: Paris, France
Patch C, Sequieros J, Cornel MC (2009) Genetic horoscopes: is it all in the genes? Points for regulatory control of direct-to-consumer genetic testing. Eur J Hum Genet 17:857–859
Pinto-Basto J, Guimarães B, Rantanen E et al (2010) Scope of definitions of genetic testing: evidence from a EuroGentest Survey. J Community Genet 1:29–35
Rothstein MA (2005) Genetic exceptionalism and legislative pragmatism. Hastings Center Report 35(4):27–33
Rynning Elisabeth (2011) Still no Patients’ Act in Sweden—reasons and implications in Elisabeth Rynning & Mette Hartlev (Eds.) Nordic Health Law in a European Context—Welfare state perspectives on patients’ rights and biomedicine. Liber AB,Sweden
Soini S, Matthijs G, Aymé S (2008) Patenting and licensing in genetic testing. ethical, legal and social issues. Eur J Hum Genet 16:S10–S50
Vialla F (2006) La loi de 2004 au regard des évolutions en bioéthique in Dix and des lois de bioéthique en France. Revue générale de droit médical, Les Études Hospitalièrs Éditions, Bordeaux
WHO (2003) Review of Ethical Issues in Medical Genetics. Report of Consultants to WHO Professors D.C Wertz, J.C Fletcher and K. Berg. World Health Organisation
Conflict of interest
The author declares that she has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Western Europe, in this text, comprises the Nordic countries and German and French-speaking countries, as well as Spain and Portugal. The UK does not have specific genetic legislation. The choice of countries is based on language (Nordic, German, Latin, and English).
Rights and permissions
About this article
Cite this article
Soini, S. Genetic testing legislation in Western Europe—a fluctuating regulatory target. J Community Genet 3, 143–153 (2012). https://doi.org/10.1007/s12687-012-0078-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-012-0078-0