Abstract
Background
A proportion of patients with gastroesophageal reflux disease (GERD) do not respond to proton pump inhibitor (PPI) therapy.
Aim of the study
To determine the findings on high-resolution esophageal manometry (HREM) and 24-h pH recording in patients with typical GERD symptoms, refractory to PPI treatment.
Methods
Retrospective analysis of prospectively maintained database of patients referred for HREM and 24-h pH recording was done. We selected patients who were referred for evaluation of refractory GERD symptoms despite > 8 weeks of at least once-daily PPI treatment. Details noted were demographic profile, upper gastrointestinal endoscopy report, HREM findings and 24-h pH findings.
Results
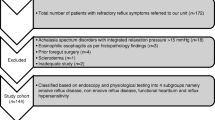
Ninety-six patients had symptoms of GERD that were refractory to PPI therapy. Seven patients (7.1%) were diagnosed having diseases mimicking GERD: eosinophilic esophagitis (n=2), supragastric belching (n=4) and rumination (n=1). After excluding these patients and those with insufficient data, the final study cohort included 82 cases. Fifty patients (61%) had normal motility. Major motility disorders were detected in 8 (9.75%) patients: achalasia cardia (6) and distal esophageal spasm (2). Ineffective esophageal motility was noted in 24 patients. A total of 74 patients underwent 24-h pH testing. Significant acid reflux with good symptom correlation was noted in 56 patients. Eighteen patients did not have significant acid reflux (Johnson-DeMeester score < 14.7): hypersensitive esophagus (12) and functional heartburn (6).
Conclusion
Fifty-six patients (68.3%) had definite diagnosis of GERD and 31.7% (26) had non-GERD conditions like motility disorders, functional heartburn and hypersensitive esophagus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Gastroesophageal reflux disease (GERD) is a common problem in the world with a prevalence of around 15% in North America and European countries [1, 2]. Population-based studies from India have noted variable prevalence [3,4,5]. The prevalence in India is almost comparable to that in the West and is higher than in many Asian countries [1, 2, 6].
Most patients respond well to lifestyle changes and medications. The recent task force constituted by the Indian Society of Gastroenterology to study GERD in India has reported that patients not responding to conventional 4-week proton pump inhibitor (PPI) therapy need to be investigated further [7]. These patients require detailed pathophysiological evaluation to rule out causes pertaining to persistent acid exposure, non-acid reflux, heartburn of other etiologies, esophageal motility disorders, functional heartburn and functional chest pain [8].
The present study was planned to determine the findings on pathophysiological tests, high-resolution esophageal manometry (HREM) and 24-h pH recording, in patients with typical GERD symptoms not responding to PPI treatment for > 8 weeks.
Methods
The present study is a retrospective analysis of prospectively maintained database of patients referred for HREM and 24-h pH recording between 2011 and 2019. We selected patients who were referred for evaluation of refractory GERD symptoms despite being on > 8 weeks of at least once a day PPI treatment. The demographic details included age, sex, symptoms, duration of disease and treatment details. Details of upper gastrointestinal (GI) endoscopy were noted. For some patients, endoscopic examination was repeated if static images were not available for interpretation or endoscopic examination was done > 6 months back. However, for most patients, endoscopy findings were noted from static images available from previous or outside endoscopy reports.
Manometry protocol
Prokinetics and anti-cholinergics were withdrawn for at least 14 days prior to the recording. Basal lower esophageal sphincter (LES) pressures and esophagogastric junction (EGJ) morphology were determined. Basal LES pressure was recorded after a period of quiet rest following introduction of the manometry catheter for 30 to 45 s at the start of HREM recording and during normal respiration. HREM recording was done following 10 swallows of 5 mL water each in supine posture, using a 16-channel water perfusion system (GS Hebbard, Australia) and reporting was done using Trace 1.3.3 software (GS Hebbard, Australia). All HREM records of patients were analyzed according to Chicago Classification 3.0 [9].
Twenty-four-hour pH recording
This was done while the patients were not taking PPI for at least 2 weeks using a single-sensor probe (Sandhill Scientific, Highland Ranch, USA). Location of LES was determined using HREM. The pH probe was passed into the stomach and using pull-through technique stationed at 5 cm above the LES. Relationship between the symptoms to meal and position was documented using symptom index. Interpretation was done using computerised software (Sandhill Scientific, Highland Ranch, USA). The pH-metry test was done only after HREM testing in all cases. This protocol is followed in our unit to determine the exact position of LES prior to probe placement and to rule out major motility disorders.
The study was approved by the Institutional Ethics Board.
Definitions used
Refractory GERD: defined as typical GERD symptoms (heartburn, regurgitation and/or chest pain) not responding to PPI (once or twice daily) for > 8 weeks [10].
Hypotensive LES: basal LES pressure less than 10 mmHg [11].
Type 1: no separation between the LES and the crural diaphragm.
Type 2: minimal separation (> 1 and < 2 cm) making a double-peaked pressure profile, which, however, is not indicative of a hiatus hernia.
Type 3: more than 2-cm separation between the LES and the crural diaphragm at inspiration so that two high-pressure zones can be clearly identified.
Type 3a: respiratory inversion point distal to the LES.
Type 3b: respiratory inversion point proximal to the LES.
Reflux esophagitis: diagnosed using the Los Angeles criteria [13].
Non-erosive reflux disease: negative endoscopic findings in the presence of pathological reflux but with Johnson-DeMeester score ≥ 14.7 or % of total time period pH below 4 ≥ 4.2% in ambulatory pH monitoring [14].
Hypersensitive esophagus: normal acid exposure and positive symptom association as defined by symptom index ≥ 50% [15].
Functional heartburn: burning retrosternal discomfort or pain with lack of symptom relief despite optimal antisecretory therapy in the absence of evidence of GERD, eosinophilic esophagitis, major esophageal motor disorder or structural abnormality [16].
Eosinophilic esophagitis: esophageal mucosal eosinophilic infiltrate of > 20 per high power field on histopathological examination and negative stool examination for parasites [17].
Rumination: diagnosed based on clinical symptoms, behavioral observations, normal structural tests like upper GI endoscopy and good response to behavioral treatment [18].
Supragastric belching: excessive belching caused by a rapid process of air entry by sucking air from the mouth or pharynx into the esophagus and then expelling it with abdominal straining. It is diagnosed based on clinical observation and response to behavioural therapy [19].
Statistical analysis
The data were entered in Microsoft Excel sheet. The data were represented as median and range for quantitative variables. For categorical variables, the data were reported as frequency and proportion.
Results
Seven hundred and ninety-six patients were referred for GI pathophysiological tests, HREM and 24-h pH testing, between 2011 and 2019. Of them, 96 (12%) had symptoms of GERD that were refractory to treatment with PPI for more than 8 weeks. On further evaluation, it was noted that 7 patients (7.1%) were diagnosed as having diseases mimicking GERD: eosinophilic esophagitis (2), supragastric belching (4) and rumination (1). The data were insufficient for analysis in further 7 cases and they were excluded from the final analysis. Thus, the final study cohort included 82 cases.
Demographic parameters (Table 1)
The patients were predominantly males (54, 65.8%). The median age was 48 years (20–82 years). Body mass index was > 25 kg/m2 in 32 patients (39%). History of tobacco use, smoking and alcohol intake was noted in 20 (24.4%), 12 (14.6%) and 14 (17%) patients, respectively.
Reflux esophagitis had been reported on upper GI endoscopy in 15 patients (18.3%). The predominant symptoms reported were heartburn (58, 70.3%), regurgitation (44, 53.6%) and chest pain or retrosternal discomfort (24, 29.6%).
HREM findings (Table 1)
Fifty patients (61%) had normal esophageal motility. Hypotensive LES was noted in 40 patients (48.8%)
Peristaltic abnormalities (Fig. 1)
Major motility disorders were detected in 8 patients (9.75%). These included achalasia cardia (6) and distal esophageal spasm (2). After exclusion of these patients, ineffective esophageal motility was noted in 24 (32.4%) and normal motility in 50 (67.6%).
Twenty-four-hour pH testing (Table 1)
A total of 74 patients underwent 24-h pH testing (24 IEM; 50 normal peristalsis). Significant acid reflux with good symptom correlation was noted in 56 patients, suggesting the diagnosis of GERD. Eighteen patients did not have significant acid reflux (Johnson-DeMeester score < 14.7). Of them, twelve were diagnosed as hypersensitive esophagus and six as functional heartburn.
To summarize, 8.5% of patients with refractory GERD had GERD mimics like eosinophilic esophagitis, supragastric belching and rumination syndrome. Of the 82 patients analyzed, 56 (68.3%) had definite diagnosis of GERD and 31.7% (26) had non-GERD conditions, namely motility disorders, functional heartburn and hypersensitive esophagus.
Discussion
The present study highlights that 31.7% of patients with typical GERD symptoms, refractory to treatment with PPI, have non-GERD conditions. Detailed evaluation including history and endoscopic biopsies is likely to identify potential GERD mimics like eosinophilic esophagitis, rumination and supragastric belching.
The presence of alternative diagnosis in patients with GERD has been studied earlier. Herregods et al. [20] reported that among 106 patients presenting with persistent typical reflux symptoms, only 69 patients received a final diagnosis of GERD. Thus, it is of utmost importance to differentiate between GERD and other likely diagnoses in order to provide appropriate and cost-effective treatment. A hospital-based study from northern India reported that the prevalence of eosinophilic esophagitis in patients with GERD was 3.2%. The authors noted that eosinophilic esophagitis should be considered as a possibility in patients with history of allergy, no-response to PPI and absolute eosinophil count of ≥ 250/cu mm [17]. Supragastric belching is more frequent in patients with typical reflux symptoms than in healthy subjects [21]. It is caused by either sucking of air into the esophagus by decreasing the intrathoracic pressure or pushing air into the esophagus by contracting the pharyngeal muscles during glottis closure. It tends to stop when the patient keeps their mouth open and this simple test helps in diagnosing this phenomenon in office practice. Rumination syndrome is characterized by the effortless and often repetitive regurgitation of recently ingested food into the mouth. It is caused by contraction of the abdominal muscles and subsequent increase in intragastric pressure that pushes the stomach contents upward. These patients commonly present with symptoms of recurrent vomiting and regurgitation. A detailed clinical history helps in diagnosis. Diaphragmatic breathing and baclofen may be useful in the management of these disorders along with behavioral treatments [22,23,24].
Patients with achalasia or other esophageal motility disorders may present with symptoms similar to GERD and are often misdiagnosed. A recent study highlighted that one-third of achalasia patients complain of heartburn [25]. Regurgitation and chest pain are also common presenting features of achalasia in Indian setting and may lead to confusion with GERD [26]. Moreover, upper GI endoscopy may be reported as normal or low-grade esophagitis in many patients [26]. Another study showed that 15.5% of total patients with refractory GERD symptoms had esophageal motility disorders [10]. In the present study, we did HREM study for all patients prior to 24-h pH testing and identified 8 cases with major motility disorders. Even the diagnosis of ineffective motility has shown to reduce repeat upper GI contrast studies, endoscopy, and psychological therapy in children with refractory GERD [27].
Functional heartburn and reflux hypersensitivity are common disorders reported in patients with refractory GERD symptoms [16, 28]. Functional heartburn affects women more than men and is primarily treated with neuromodulators. Psychological intervention and complementary and alternative medicines play important roles in the management of these patients [28]. Reflux hypersensitivity (previously called hypersensitive esophagus) has been recently introduced by Rome IV as a new functional esophageal disorder and affects primarily young to middle-aged women [16]. It frequently overlaps with other functional GI disorders. Esophageal neuromodulators, such as tricyclic anti-depressants and selective serotonin reuptake inhibitors, play an important role in its management [29].
The present study has limitations such as retrospective design and small sample size. Provocative testing like multiple rapid swallows was not done in all patients and hence, not included in analysis. Impedance pH testing was not done due to non-availability of equipment. Certain factors that can lead to refractory symptoms include improper dosage or timing of medications, lifestyle issues and poor drug compliance. These could not be addressed in the present study. Moreover, presence of associated psychiatric disorders and use of medications like calcium channel blockers, nitrates and anti-inflammatory drugs were not noted.
Despite these shortcomings, the present study highlights that it is important to differentiate refractory GERD symptoms from other diseases not related to reflux; HREM and 24-h pH testing are important tests for this. Further prospective studies with larger sample size are required from India to develop guidelines to help in proper management of such patients.
References
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–80.
Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–40.
Bhatia SJ, Reddy DN, Ghoshal UC, et al. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2011;30:118–27.
Chowdhury SD, George G, Ramakrishna K, et al. Prevalence and factors associated with gastroesophageal reflux disease in southern India: a community-based study. Indian J Gastroenterol. 2019;38:77–82.
Wang HY, Leena KB, Plymoth A, et al. Prevalence of gastro-esophageal reflux disease and its risk factors in a community-based population in southern India. BMC Gastroenterol. 2016;16:36.
Bhatia S, Gupta D, Vennalaganti P. Epidemiology of gastroesophageal reflux in Asia. The rise of acid reflux in Asia. J Neurogastroenterol Motil. 2017;17:14–27.
Bhatia SJ, Makharia GK, Abraham P, et al. Indian consensus on gastroesophageal reflux disease in adults: a position statement of the Indian Society of Gastroenterology. Indian J Gastroenterol. 2019;38:411–40.
Kahrilas PJ, Boeckxstaens G, Smout AJ. Management of the patient with incomplete response to PPI therapy. Best Pract Res Clin Gastroenterol. 2013;27:401–14.
International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74.
Wang F, Li P, Ji GZ, et al. An analysis of 342 patients with refractory gastroesophageal reflux disease symptoms using questionnaires, high-resolution manometry, and impedance-pH monitoring. Medicine (Baltimore). 2017;96:e5906.
Sloan S, Rademaker AW, Kahrilas PJ. Determinants of gastroesophageal junction incompetence: hiatal hernia, lower esophageal sphincter, or both? Ann Intern Med. 1992;117:977–82.
Martinucci I, Bortoli ND, Giacchino M, et al. Esophageal motility abnormalities in gastroesophageal reflux disease. World J Gastrointest Pharmacol Ther. 2014;5:86–96.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Savarino E, Zentilin P, Savarino V. NERD: an umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol. 2013;10:371–80.
Savarino E, Pohl D, Zentilin P, et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut. 2009;58:1185–91.
Aziz Q, Fass R, Gyawali CP, et al. Esophageal disorders. Gastroenterology. 2016;150:1368–79.
Baruah B, Kumar T, Das P, et al. Prevalence of eosinophilic esophagitis in patients with gastroesophageal reflux symptoms: a cross-sectional study from a tertiary care hospital in North India. Indian J Gastroenterol. 2017;36:353–60.
Chial HJ, Camilleri M, Williams DE, Litzinger K, Perrault J. Rumination syndrome in children and adolescents: diagnosis, treatment and prognosis. Pediatrics. 2003;111:158–62.
Koukias N, Woodland P, Yazaki E, Sifrim D. Supragastric belching: prevalence and association with gastroesophageal reflux disease and esophageal hypomotility. J Neurogastroenterol Motil. 2015;21:398–403.
Herregods TV, Troelstra M, Weijenborg PW, Bredenoord AJ, Smout AJ. Patients with refractory reflux symptoms often do not have GERD. Neurogastroenterol Motil. 2015;27:1267–73.
Hemmink GJ, Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Supragastric belching in patients with reflux symptoms. Am J Gastroenterol. 2009;104:1992–7.
Ong AM, Chua LT, Khor CJ, Asokkumar R, S/O Namasivayam V, Wang YT. Diaphragmatic breathing reduces belching and proton pump inhibitor refractory gastroesophageal reflux symptoms. Clin Gastreoenterol Hepatol. 2018;16:407–16.
Chitkara DK, Van Tilburg M, Whitehead WE, Talley NJ. Teaching diaphragmatic breathing for rumination syndrome. Am J Gastroenterol. 2006;101:2449–52.
Blondeau K, Boecxstaens V, Rommel N, et al. Baclofen improves symptoms and reduces postprandial flow events in patients with rumination and supragastric belching. Clin Gastroenterol Hepatol. 2012;10:379–84.
Andolfi C, Bonavina L, Kavitt RT, Konda VJ, Asti E, Patti MG. Importance of esophageal manometry and pH monitoring in the evaluation of patients with refractory gastroesophageal reflux disease: a multicenter study. J Laparoendosc Adv Surg Tech A. 2016;26:548–50.
Jain M. Achalasia cardia: a diagnosis often delayed! Indian J Gastroenterol. 2019;38:183–4.
Hsing TY, Tsai IJ, Tsu CT, Wu JF. Role of esophageal manometry in children with refractory gastroesophageal reflux symptoms. Pediatr Int. 2019;61:807–1.
Yamasaki T, O’Neil J, Fass R. Update on functional heartburn. Gastroenterol Hepatol (NY). 2017;13:725–34.
Yamasaki T, Fass R. Reflux hypersensitivity: a new functional esophageal disorder. J Neurogastroenterol Motil. 2017;23:495–503.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MJ and VA declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
The study was approved by the Institutional Ethics Board.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jain, M., Agrawal, V. Role of esophageal manometry and 24-h pH testing in patients with refractory reflux symptoms. Indian J Gastroenterol 39, 165–170 (2020). https://doi.org/10.1007/s12664-020-01032-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-020-01032-z