Abstract
Introduction
Among the pathological entities that affect the maxillofacial region, Keratocystic odontogenic tumour has been subject to a lot of debates, controversies and speculations because of its diverse nature and high recurrence rates.
Materials and methods
The authors conducted a search in English literature using the following keywords; “Odontogenic keratocyst” and “Keratocystic odontogenic tumour”. The aim of the paper was to review all aspects of the entity, including etiology, pathogenesis, clinical and radiological manifestations, growth potential, recurrence and treatment modalities.
Conclusion
The controversial nature of the pathology not withstanding, there is in general a broad consensus on treating the entity conservatively with emphasis on a long term review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First described by Phillipsen [1] in 1956, this pathological entity has evoked much controversies and debates in terms of the treatment options and the recurrence rates in world literature. Having been classified as a cyst of odontogenic origin for over five decades, the pathogenesis, histological character and progress of the entity finally led to the metamorphosis from a cyst to an odontogenic tumour in 2005. The enigma of KCOT is centred on the lack of recognition about the true biologic nature of this condition. KCOT involves approximately 11 % of all cysts in the maxillofacial region [2] and is located most commonly in the mandibular ramus and angle region [3, 4].
Materials and Method
The author conducted a search in English literature using the following keywords; “Odontogenic keratocyst” and “Keratocystic odontogenic tumour”. Since the aim of the paper was to review all aspects of the entity, no inclusion criteria was specified. All aspects related to etiology, pathogenesis, clinical and radiological manifestations, growth potential, recurrence and treatment modalities were included in the review of literature.
Etiology
The etiology of KCOT is probably related to the development of the dental lamina and in particular remnants of it after this organ has served its purpose. These epithelial islands derived from the dental lamina are mainly found in the gingiva and periodontal ligament. This explains the clinical entity of lateral periodontal or lateral follicular presentation of these tumours. One of the enigmas dogging this entity is explaining why they develop from such epithelial remnants or why they develop selectively from one such epithelial island, while being dormant in the other areas. The clinical implication of this lies in the fact that if one removes such a lesion some of these epithelial residues may be left behind which may later give rise to a new one [5].
The common presence of KCOT posterior to the 3rd molar region is difficult to explain if dental lamina is believed to be the etiological derivative due to the unlikely possibility of remnants or offshoots of this dental lamina being located in the mucosa posterior to the last molar [6]. It is therefore probable that offshoots of the basal layer of the epithelium of the oral mucosa may also be involved in the etiology of KCOTs [7, 8].
One important consideration is the presence of these islands in at least 50 % of the cases in the overlying attached mucosa. This has great implications in management where it becomes mandatory to excise that part of the mucosa, in conjunction with enucleation. Failure to do so will leave behind the potential source for recurrence of the lesion [9].
Pathogenesis
One of the characteristic features of the growth of this pathology is the tendency to grow along the cancellous channels with very little cortical expansion. Various theories of expansion of KCOT have been proposed to explain this. These include intraluminal hyperosmolality, active epithelial proliferation [10], collagenolytic activity of the cyst wall [11] and synthesis of interleukin 1 and 6 by keratinocytes. This will induce the secretion of keratocyte growth factor from interactive fibroblasts along with tumour necrosis factor leading to increased levels of prostaglandins and increased expression of parathyroid related protein. It has also been seen that the release of inflammatory cytokines such as IL-1 from the epithelial cells tend to activate the resorption of bone around the lesions by stimulating osteoclastogenesis and activation [12, 13].
Autophagy, a lysosome-dependent catabolic process has an important role in the regulation of tumour growth through degradation of cellular proteins and organelles. This provides amino acids, nucleotides, and lipids for the production of ATP and macromolecular synthesis. Autophagy, activated during tumour development, and having a significant role in antiapoptosis and proliferation of tumour cells is a significant finding in KCOTs [14].
Change in Nomenclature
It took over five decades for the reestablishment of this entity as a tumour, though, way back in 1967, Toller [10] had suggested terming it as a benign neoplasm based on its clinical behaviour. In 1984, Ahlfors et al. [11] showed the basal layer of the lesion budding into connective tissues. A significant part of the biological behaviour of KCOTs in infiltration beyond its epithelial periphery is characterised by the marked claudin-3 loss of expression in its basal layer when compared with other cysts, suggesting that this may indicate alteration of basal cell polarity and impaired barrier function of the lining epithelium, contributing to its biological behavior [15].
The genetic picture in KCOT has also influenced this decision to reclassify it. PTCH (Patched), a tumour suppressor gene involved in both NBCCS and sporadic KCOTs occur on chromosome 9 q22.3–q31 [13]. Usually PTCH forms a receptor complex with the oncogene SMO for the SHH (Sonic hedgehog) ligand. SHH binding to PTCH releases the inhibition of growth signal transduction seen in PTCH binding to SMO. Thus the proliferating–stimulating effects of SMO are then predominant as seen in these conditions. The neoplastic capability and high recurrence have been attributed to a higher frequency of occurrence of proliferating nuclear antigen Ki67, p53 and bcl-2 positivity [12].
All the evidence finally forced WHO to reclassify the lesion in 2005 based on several factors like locally destructive and highly recurrent nature & the presence of mitotic figures in the suprabasal layers.
WHO defined it as “A benign unicystic or multicystic, intraosseous tumour of odontogenic origin with a characteristic lining of parakeratinised stratified squamous epithelium and potential for aggressive infiltrative behaviour” [16].
Clinical Features
The unique clinical characteristics of this entity are the local destruction and tendency for multiplicity especially when associated with syndromes like the naevoid basal cell carcinoma syndrome or Gorlin Gotz syndrome. While there is no doubt about the epithelial origin of the pathology, the triggering factors are still a matter of conjecture. An interesting finding was shown by Alva et al. [17] when a retrospective study of 183 cases showed 17.1 % of the cases showing koilocytosis, a feature seen in human papilloma virus (HPV) infections thus displaying the wide morphological variations of the condition.
The tumour has a predilection for the mandibular 3rd molar region and usually manifest as multilocular radiolucencies with scalloped well defined margins. Aspiration biopsies reveal keratin flakes with protein levels <4 g/100 ml [9].
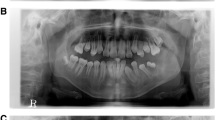
Radiographic Picture
Classically the KCOT has been shown to have a definite radiolucent entity with well defined borders extending along the cancellous bone. It can either be a unilocular or multilocular entity. A study by Buckley et al. [18] have shown that the presence of a multilocular radiolucency is associated with a 12-fold increase in probability of the lesion being a KCOT.
Treatment Options
The treatment modalities have evoked the greatest debates and controversies because of the recurrence potential of the tumour. Management of KCOT should focus on selecting the best modality that carries the lowest possible risk of recurrence and minimum morbidity. Management options in KCOT can broadly be divided into conservative treatment and radical management. Conservative treatment aims at preserving the bony architecture as much as possible while removing the pathology as in marsupialisation or decompression. More aggressive forms of management are enucleation with/without curettage along with adjunctive uses of chemical/cryo cauterisation or resection.
Conservative Management
Marsupialisation
Marsupialisation was first described by Partsch [19] in 1882 for the treatment of cystic lesions. This technique is based on the externalization of the cyst, through the creation of a surgical window in the buccal mucosa and in the cystic wall. Their borders are then sutured to create an open cavity that communicates with the oral cavity. This procedure relieves pressure from the cystic fluid, allowing reduction of the cystic space and facilitates bone apposition under the cystic walls.
This method preserves the bone structure and associated teeth especially in young patients. These techniques are less traumatic for the patient, reduce hospital stay and avoid the need for reconstruction.
Melugin [20] has described marsupialisation as a technique-sensitive, tissue-sparing treatment modality for the management of large lesions in proximity to one or more nonerupted teeth or other vital structures. Marsupialization allows for gradual decompression of the cyst cavity, which often draws the cyst walls away from teeth and other vital structures and replaces cyst with bone.
One of the main deterrents to marsupialisation in managing KCOTs has been the incomplete removal of the epithelium. However, studies have shown that a significant feature of marsupialization is the epithelial changes that occur in the remaining cystic lining. The cystic wall showed thickening [21] with inhibition of IL-1a [22], epithelial dedifferentiation and loss of cytokeratin 10 production [23] including change of the keratotic character from parakeratin to orthokeratin. August et al. [24] reported the differentiation of the epithelium once treatment is carried out. Through histochemical analyses based on Cytokeratin-10 tests, August et al. accomplished the pre-operatory identification of the lesion in 14 KCOTs. After surgery, the same analysis was carried out again in the cystic epithelium and it was seen that 64 % of the patients did not present Cytokeratin-10 in the epithelium analyzed, showing differentiation of this tissue thus reducing the rate of recurrence. In 2003, August et al. [23] further examined the nature of the cyst lining before and after decompression with cytokeratin stains and reported positive cytokeratin-10 staining in the predecompression biopsy and negative cytokeratin-10 stains in the postdecompression specimen. In 3, 6, 9 and 12-month samples, a return to more normal oral epithelium with 9 months of decompression treatment was evident. This evidence has proved to be a decisive factor in propagating the more conservative method of removal without the danger of diseased tissue remaining.
Another possible way of removing all pathological tissue without endangering vital structures or weakening the bone is a two stage procedure where marsupialisation is followed by removal of the rest of the lesion at a later stage after the thinned out bone has increased in dimension, thus avoiding injury to structures or the probability of pathological fracture.
The resultant smaller cyst is therefore easier to completely excise subsequently. In a study Kubota et al. [25] have indicated that the larger lesions shrink faster than smaller lesions in patients with KCOT. While this 2 stage procedure ensures complete removal without endangering the surrounding areas, the second stage allows for new bone formation thus ensuring a complete comprehensive removal of the lining, which was not possible in a single stage marsupialization procedure. In analysing 14 identifiable studies involving 938 patients, marsupialisation was found to have lesser recurrence than enucleation according to Wushou et al. [26].
Recurrence
One of the biggest disadvantages of conservative management is the inadequate removal of the pathological epithelium. Studies have shown increased recurrence of the lesion with decompression and curettage up to 14 % in a 2 years follow-up [27].
Schmidt [28] explaining the role for enucleation and cryosurgery in the management of the tumour has shown that the rates of recurrence vary enormously, from a maximum of 62 % to a minimum of 0 %. The majority of recurrent cases occur within the first 5 years after treatment [29, 30]. For this reason, most surgeons advocate complete removal with wide margins or curettement of the surrounding tissues. The enucleation alone is associated with the highest recurrence rates because of the thin lining becoming fragmented during removal. To reduce the chances of recurrence, various adjunctive therapies have been advocated, including peripheral ostectomy or the use of Carnoy’s solution, cryotherapy or electrocautery.
The three most common reasons for recurrence are parts of the lining being left behind, presence of microcysts in the connective tissue of the cyst wall left behind after enucleation and development of a new lesion from an epithelial island or microcyst left behind in the mucosa [5].
In their study, Kinard et al. [31] analysed the overall 5 year disease free rate and found younger patients had an increased risk for recurrent disease compared to older patients. Enucleation with or without adjuvant therapy was associated with a statistically significant decreased risk for recurrent disease compared with decompression with or without secondary cystectomy. Another interesting finding was that multilocular lesions were 33.6 times more likely to recur than unilocular lesions. In a review of 51 patients treated over a period of 15 years, Chirapathomsakul and co workers [32] found most of the recurrences occurring in the symphysis-body region. According to them one of the probable reasons for this could be the tendency of surgeons to treat this region conservatively due to the presence of teeth. They suggest extractions if there is any doubt about leaving pathologic tissue behind.
Another interesting finding by Stoelinga was the absence of microcysts in the surrounding bone when block resections were carried out on five recurrent KCOTs. The author therefore is a vociferous opponent of any radical treatment like resections [33].
A systematic review of data from 1999 to 2010 was analysed by Johnson et al. [34] to provide a current consensus on management and recurrence rates. They arrived at a conclusion that:
-
1.
Simple enucleation of the KCOT is not endorsed because of the high recurrence rate.
-
2.
A small KCOT where the margins can be accessed may be enucleated with adjunctive measures, such as Carnoy’s solution.
-
3.
A large, expanding KCOT is best treated with a 2-stage approach. Marsupialization first, followed by enucleation and adjunctive measures to decrease the surgical injury to the patient.
-
4.
Marginal or segmental resection offers the lowest recurrence rate. It is not advocated as a primary treatment modality for most tumors because of its morbidity and the benign nature of the disease.
Carnoy’s Solution
One of the most popular adjunctive aids in KCOT management is the Carnoy’s solution. It was first used for reducing the recurrence rate and tanning of the epithelial lining of cysts by Cutler and Zollinger [35]. It consists of 60 % ethanol, 30 % chloroform and 10 % glacial acetic acid with 0.1 Gm ferric chloride. The FDA has imposed a ban on pharmacies compounding therapeutic agents containing chloroform, currently listed as a carcinogenic agent. In its initial use in KCOT management, Voorsmit and co workers [36] established its excellent penetrative properties with rapid local fixation in addition to being a good haemostatic.
The presence of vital structures like nerves and vessels in the vicinity however predisposes these structures to the harmful effects of this fixative. The effect of medicaments like BIPP, Whitehead’s varnish, Carnoy’s solution and surgicel on the nerve were studied by Loescher and Robinson [37]. They showed persistent damaging effects of Carnoy’s solution on the sensory nerves.
Therefore the time of exposure of the nerve to the solution is critical. The severity of the neurological damage depends on the tissue penetration according to the diffusion rate. It was shown in the study by Bernard Frerich and co workers [38] on IAN nerves of rabbits that above 5 min of exposure led to an almost complete abolition of motor and sensory nerve function. It was seen that after exposures of up to 3 min the agent is bound primarily to the epineurium and perineurium. For this period, the perineurium appears to act as a tight diffusion barrier, paramount for the maintenance of a functionally intact endoneurial environment. This perineurial barrier resists chemical damage until the exposure time reaches a critical point ranging somewhere between 3 and 5 min, when a sudden breakdown takes place and Carnoy’s solution floods the endoneurial space. Another study has reported minimal sensory damage when the exposure did not exceed 3 min [39].
In contrast, the effect on the vessel is less critical and even after 5 min of exposure; the damage seemed to be reversible [40].
One factor that is yet to be studied is the effect of a ‘‘modified’’ version of the solution without chloroform, on the penetrative capability and effect of the solution [41].
Cryosurgery
An alternative to chemical cauterization is the use of cryosurgery after removal of the lesion. A temperature of −20 °C is required to devitalize tissues and only liquid nitrogen can deliver this on a consistent basis. Cryosurgery causes cell death by direct damage from intracellular and extracellular ice crystal formation plus osmotic and electrolyte disturbances.
Salmassy and Pogrel [42] used a triple freeze/thaw technique with a 1-min freeze followed by a slow thaw for each cycle. The advantages of liquid nitrogen over other methods of devitalizing tissue beyond the visible lesion of the margin are (1) The bone matrix left behind acts as a scaffold for new bone formation (2) Ability to place a bone graft immediately to accelerate healing and minimize the risk of a pathologic fracture. Another advantage of this method is the reversible effects on the neural tissue. It has been shown that after exposure, there is return of sensation. Freezing devitalizes the neuron itself but the axon sheath is resistant to freezing and remains intact. Functionally, the injury is analogous to neuropraxia and the intact axon sheath allows growth of a new neuron [28].
Len Tolstunov and Trevor Treasure [43] have used a double freeze thaw cycle with good results. Pogrel [44] has elucidated the advantages of liquid nitrogen in the management of KCOT by stating that the technique causes less bleeding and scarring, proven reversibility of IAN function, as well as protection of teeth vitality and sinus membrane integrity from freezing. The disadvantages are a potential lack of precision, with the risk of collateral hard and soft tissue injury, pathological fracture through the thin inferior border of the mandible exposed to the freezing agent and possible difficulty in securing a liquid nitrogen supply.
One of the problems after removal of the lining is the inability to clinically ensure complete removal of the pathology. Iwai et al. [45] have recommended the use of 1 % methylene blue on the bone and peripheral ostectomy till all the dyed bone is removed. This dye has a tendency to penetrate into epithelial cells that have an abnormal increase in nucleic acid.
Radical Management
Radical treatment of the pathology has been advocated since it early days based on the aggressive nature and recurrent potential.
Ahlfors et al. [11], in describing it as a tumour recommended it to be regarded as a benign cystic neoplasm rather than a developmental or other type of jaw cyst. According to them in order to reduce the high recurrence rate, surgery should include marginal resection, including a rim of uninvolved bone, similar to the treatment suggested in cases of unicystic ameloblastoma.
Resection of the segment has undoubtedly shown 0 % recurrence as compared to a series of conservative measures used [46, 47]. However the morbidity associated with these resections have been a deterrent in adopting this treatment modality in a benign tumour, notwithstanding its recurrent potential.
In the AAOMS symposium on odontogenic keratocysts in 2002, MacIntosh [48] argued that this entity should be approached initially with the same aggressiveness as the ameloblastoma and basal cell carcinoma.
In a more sober approach to the pathology, Tolstunov and Treasure [43] have suggested that aggressive resection should be limited to recurrent KCOTs (three or more times) or those that have undergone ameloblastic or malignant degeneration.
Reserving radical resection to those KCOTs with parakeratinised epithelium and associated with Basal cell nevus syndrome was advocated by Kolokythas et al. [49].
New Avenues in Management
With advances in genetic and molecular research with special reference to PTCH1 mutations and involvement of the Hedgehog signaling pathway a more lucid understanding of the pathogenesis has been realised. It is probable that future treatment strategies will use molecular approaches that may eventually reduce or eliminate the need for aggressive surgical intervention [50].
Management Protocol
While there has been no doubt about the efficacy of radical resection being the procedure with the least incidence of recurrence, the incidence of this pathology in a younger age group should address the crippling nature of the surgery and the morbidity associated with the reconstructive procedures.
There is enough evidence to support the need for more conservative options like marsupialisation or a 2 stage procedure since there is ample evidence of alteration of the remaining epithelium and the safer removal after the decompression leads to new bone formation under the epithelium.
In summation management can be recommended as:
-
1.
Resection being confined to large lesions affecting most of the bony architecture leaving no room for preservation of the native tissue. It therefore becomes the last alternative in large lesions involving most of the bone with perforation.
-
2.
Most cases can be taken up for enucleation along with chemical cauterisation with Carnoy’s solution.
-
3.
Marsupialisation is indicated when the underlying bone is thinned out. This can be augmented with a secondary enucleation with chemical cauterisation procedure after adequate bone has formed.
-
4.
All cases to be reviewed for a minimum period of 5 years due to the evidence of most recurrences occurring in this post op phase.
Conclusion
With the histological character, pathogenesis and recurrence influencing factors being clearer now, management of KCOTs today should focus on the following principles:
-
1.
Proper diagnosis.
-
2.
Conservative treatment as far as possible.
-
3.
Use of adjuvants like Carnoy’s solution maintaining the critical exposure time near vital structures.
-
4.
Use of cryosurgery where available.
-
5.
Long term follow up for at least 5 years.
-
6.
Repeat surgery if required.
References
Phillipsen H (1956) On keratocysts in the jaws. Tandleagebladet 60:963
Maurette PE, Jorje J, de Moraes M (2006) Conservative treatment of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg 64(3):379–383
Brown RM (1970) The odontogenic keratocyst: clinical aspects. Br Dent J 128(5):228–231
Brannon RB (1976) The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part 1. Clinical features. Oral Surg Oral Med Oral Pathol 42(1):54–72
Stoelinga PJW (2005) The treatment of odontogenic keratocysts by excision of the overlying, attached mucosa, enucleation, and treatment of the bony defect with Carnoy solution. J Oral Maxillofac Surg 63:1662–1666
Stoelinga PJW, Peters JH (1973) A note on the origin of keratocysts of the jaws. Int J Oral Surg 2:37
Stoelinga PJW (1976) Studies on the dental lamina as related to its role in the aetiology of cysts and tumours. J Oral Pathol 5:65
Kramer IRH, Pindborg JJ, Shear M (1992) Histological typing of odontogenic tumours. Springer, Berlin
Stoelinga PJW (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 30:14
Toller P (1967) Origin and growth of cysts of the jaws. Ann R Coll Surg Engl 40(5):306–336
Ahlfors E, Larsson A, Sjogren S (1984) The odontogenic keratocyst: a benign cystic tumour? J Oral Maxillofac Surg 42(1):10
Barnes L, Eveson JW, Reichart P, Sidransky D (eds) (2005) Pathology and genetics of head and neck tumours. WHO classification of tumour series. IARC Press, Lyon
Cohen MM Jr (1999) Nevoid basal cell carcinoma syndrome: molecular biology and new hypotheses. Int J Oral Maxillofac Surg 28:216–223
Lia R-F, Chena G, Zhaoa Y, Zhaoa Y-F, Liua B (2014) Increased expression of autophagy-related proteins in keratocystic odontogenic tumours: its possible association with growth potential. Br J Oral Maxillofac Surg 52:551–556
Siar CH, Abbas SA (2013) Claudin expression and tight junction protein localization in the lining epithelium of the keratocystic odontogenic tumors, dentigerous cysts and radicular cysts. Oral Surg Oral Med Oral Pathol Oral Radiol 115:652–659
Piatelli A, Fioroni M, Rubini C (1998) Differentiation of odontogenic keratocysts from other cysts by the expression of bcl-2 immunoreactivity. Oral Oncol 34:404
Gonzalez-Alva P et al (2008) Keratocystic odontogenic tumour: a retrospective study of 183 cases. J Oral Sci 50(2):205–212
Buckley PC, Seldin EB, Dodson TB, August M (2012) Multilocularity as a radiographic marker of the keratocystic odontogenic tumor. J Oral Maxillofac Surg 70:320–324
Partsch C (1892) Uber Kiefercysten. Dtsch Mschr Zahnheilkd 10:271
Melugin MB (2002) The role of marsupialization, local enucleation, and enucleation with peripheral ostectomy in the management of odontogenic keratocyst symposium: the odontogenic keratocyst revisited. J Oral Maxillofac Surg 60(8 Suppl):14–16
Marker P, Brondum N, Clausen PP et al (1996) Treatment of large odontogenic keratocyst by decompression and later cystectomy: a long term follow-up and histologic study of 23 cases. Oral Surg Oral Med Oral Path Oral Radiol Endod 82:122
Ninomiya T, Kubota Y, Koji T et al (2002) Marsupialization inhibits interleukin 1a expression and epithelial cell proliferation in odontogenic keratocysts. J Oral Pathol Med 31:526
August M, Faquin WC, Troulis M et al (2003) Dedifferentiation of odontogenic keratocyst epithelium after cyst decompression. J Oral Maxillofac Surg 61:678
August M, Faquin WC, Troulis M et al (2000) Differentiation of odontogenic keratocysts from nonkeratinizing cysts by use of fine-needle aspiration biopsy and cytokeratin-10 staining. J Oral Maxillofac Surg 58:935; discussion 940
Kubota Y, Imajo I, Itonaga R, Takenoshita Y (2013) Effects of the patient’s age and the size of the primary lesion on the speed of shrinkage after marsupialisation of keratocystic odontogenic tumours, dentigerous cysts, and radicular cysts. Br J Oral Maxillofac Surg 51:358–362
Wushou A, Zhao YJ, Shao ZM (2014) Marsupialization is the optimal treatment approach for keratocystic odontogenic tumour. J Cranio-Maxillofac Surg 42(7):1540–1544
Maurette PE, Jorge J, de Moraes M (2006) Conservative treatment protocol of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg 64:379–383
Schmidt BL, Pogrel MA (2004) Neurosensory changes after liquid nitrogen cryotherapy. J Oral Maxillofac Surg 62:1183–1187
Shear M (2002) The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 2. Proliferation and genetic studies. Oral Oncol 38:323
Shear M (2002) The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 3. Immunocytochemistry of cytokeratin and other epithelial cell markers. Oral Oncol 38:407
Kinard BE, Chuang SK, August M, Dodson TB (2013) Most patients with asymptomatic, disease-free third molars elect extraction over retention as their preferred treatment. J Oral Maxillofac Surg 71:1353–1358
Chirapathomsakul D, Sastravaha P, Jansisyanont P (2006) A review of odontogenic keratocysts and the behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:5–9
Stoelinga PJW, Bronkhorst FB (1988) The incidence, multiple presentation and recurrence of aggressive cysts of jaws. J Craniomaxillofac Surg 16:184
Johnson NR, Batstone MD, Savage NW (2013) Management and recurrence of keratocystic odontogenic tumor: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 116:e271–e276
Cutler EC, Zollinger R (1933) Sclerosing solution in the treatment of cysts and fistulae. Am J Surg 19:441
Voorsmit RACA, Stoelinga PJW, van Hadst UJGM (1981) The management of keratocysts. J Maxfac Surg 9:228–236
Loescher AR, Robinson PP (1998) The effect of surgical medicaments on peripheral nerve function. BJOMS 36:327–332
Frerich B, Cornelius CP, Wiethijlter H (1994) Critical time of exposure of the rabbit inferior alveolar nerve to Carnoy’s solution. J Oral Maxillofac Surg 52:599–606
Júnior OR, Borba AM, Ferreira Alves CA, Júnior JG (2007) Carnoy’s solution over the inferior alveolar nerve as a complementary treatment for keratocystic odontogenic tumors. Rev Clín Pesq Odontol 3(3):199–202
Saulacic N, Stajcic Z, Stajcic LS, Piattelli A, Iizuka T, Lombardi T (2009) Effects of Carnoy’s solution on blood vessels of the axillary fossa of rats. Int J Oral Maxillofac Surg 38:876–879
Ecker J, Koslovsky DA (2014) Current role of carnoy’s solution in treating keratocystic odontogenic tumors. J Oral Maxillofac Surg 72(9 Suppl):e161–e162
Salmassy DA, Pogrel MA (1995) Liquid nitrogen cryosurgery and immediate bone grafting in the management of aggressive primary jaw lesions. J Oral Maxillofac Surg 53:784
Tolstunov L, Treasure T (2008) Surgical treatment algorithm for odontogenic keratocyst: combined treatment of odontogenic keratocyst and mandibular defect with marsupialization, enucleation, iliac crest bone graft, and dental implants. J Oral Maxillofac Surg 66:1025–1036
Pogrel MA (1993) The use of liquid nitrogen cryotherapy in the management of locally aggressive bone lesions. J Oral Maxillofac Surg 51:269
Iwai T, Hirota M, Maegawa J, Tohnai I (2011) Use of methylene blue for precise peripheral ostectomy of keratocystic odontogenic tumour. Br J Oral Maxillofac Surg 49:e84–e85
Zhao YF, Wei JX, Wang SP (2002) Treatment of odontogenic keratocysts: a follow-up of 255 Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:151
Kaczmarzyk T, Mojsa I, Stypulkowska J (2012) A systematic review of the recurrence rate for keratocystic odontogenic tumour in relation to treatment modalities. Int J Oral Maxillofac Surg 41:756–767
MacIntosh RB (2002) The role of osseous resection in the management of odontogenic keratocysts symposium: the odontogenic keratocyst revisited. J Oral Maxillofac Surg 60(8):14–16
Kolokythas A, Fernandes RP, Pazoki A, Ord RA (2007) Odontogenic keratocyst: to decompress or not to decompress? A comparative study of decompression and enucleation versus resection/peripheral ostectomy. J Oral Maxillofac Surg 65:640–644
Shiva Bharani KSN, Shubha Lakshmi S, Rajay Kamath AD, Hammannavar R (2013) Case report. Keratocystic odontogenic tumor: treatment review and future diagnostic trends. J Oral Maxillofac Surg Med Pathol 25(1):85–92
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menon, S. Keratocystic Odontogenic Tumours: Etiology, Pathogenesis and Treatment Revisited. J. Maxillofac. Oral Surg. 14, 541–547 (2015). https://doi.org/10.1007/s12663-014-0734-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-014-0734-5