Abstract
Purpose
Initially introduced as a safer alternative to smoking, electronic cigarettes (e-cigarettes) and vaping have since been associated with lung injury. Nevertheless, there is limited perioperative data on their potential contribution to the harmful effects of mechanical ventilation on the lungs. We hypothesized that, in adults undergoing noncardiothoracic surgeries, preoperative vaping/e-cigarette use is associated with hypoxemia during the first postoperative hour, and with an increased incidence of intraoperative and postoperative pulmonary complications.
Methods
We conducted a retrospective cohort study in which we included patients reporting as vapers/e-cigarette users within one year before surgery as the exposure group, and nonvapers as the control group. The primary outcome was the time-weighted average (TWA) SpO2/FIO2 ratio in the postanesthesia care unit during the first postoperative hour. The secondary outcome was a composite of intraoperative and postoperative pulmonary complications until discharge. We used entropy balancing to adjust for confounding, and fit weighted linear regression and logistic regression models to estimate treatment effects.
Results
A total of 110,940 patients met the inclusion criteria, and 1,941 of these were vapers/e-cigarette users. The average treatment effect on the treated for TWA SpO2/FIO2 ratio (N = 109,217) was estimated to be a mean difference of 4 (95% confidence interval [CI], 1 to 8; P = 0.007). This is equivalent to a 4% change in SpO2 at a 30% FIO2 (or at a fixed FIO2). The difference was statistically significant. The average treatment effect on the treated for experiencing intraoperative and postoperative pulmonary complications (N = 110,940) was an odds ratio of 1.04 (95% CI, 0.71 to 1.54; P = 0.84).
Conclusion
Vaping/e-cigarette use was neither associated with clinically significant hypoxemia during the first hour in the postanesthesia care unit nor with an increase in pulmonary complications. Nevertheless, our findings cannot definitively exclude the deleterious effects of vaping and e-cigarette use on the lungs, and anesthesiologists should consider potential perioperative complications.
Résumé
Objectif
Initialement introduites comme une alternative plus sécuritaire au tabagisme, les cigarettes électroniques et le vapotage ont depuis été associés à des lésions pulmonaires. Néanmoins, il existe peu de données périopératoires concernant leur contribution potentielle aux effets nocifs de la ventilation mécanique sur les poumons. Nous avons émis l’hypothèse que, chez les adultes bénéficiant de chirurgies non cardiothoraciques, l’utilisation préopératoire de vapotage/de cigarette électronique était associée à une hypoxémie au cours de la première heure postopératoire et à une incidence accrue de complications pulmonaires peropératoires et postopératoires.
Méthode
Nous avons mené une étude de cohorte rétrospective dans laquelle nous avons inclus les patient·es déclarant avoir vapoté ou utilisé des cigarettes électroniques dans l’année précédant la chirurgie comme groupe d’exposition, et les personnes ne vapotant pas comme groupe témoin. Le critère d’évaluation principal était le rapport de SpO2/FIO2 moyen pondéré dans le temps en salle de réveil pendant la première heure postopératoire. Le critère d’évaluation secondaire était un mélange de complications pulmonaires peropératoires et postopératoires jusqu’au congé de l’hôpital. Nous avons utilisé l’équilibrage d’entropie pour ajuster les facteurs de confusion et ajusté les modèles de régression linéaire pondérée et de régression logistique pour estimer les effets du traitement.
Résultats
Au total, 110 940 patient·es répondaient aux critères d’inclusion, dont 1941 étaient des vapoteurs ou vapoteuses/utilisaient des cigarettes électroniques. L’effet moyen du traitement sur le rapport de SpO2/FIO2 moyen pondéré dans le temps des personnes traitées (N = 109 217) a été estimé à une différence moyenne de 4 (intervalle de confiance [IC] à 95 %, 1 à 8; P = 0,007). Cela équivaut à une variation de 4 % de la SpO2 à 30% FIO2 (ou à une FIO2 fixe). La différence était statistiquement significative. L’effet moyen du traitement sur les personnes traitées pour des complications pulmonaires peropératoires et postopératoires (N = 110 940) était un rapport de cotes de 1,04 (IC 95 %, 0,71 à 1,54; P = 0,84).
Conclusion
L’utilisation du vapotage et de la cigarette électronique n’était associée ni à une hypoxémie cliniquement significative au cours de la première heure en salle de réveil, ni à une augmentation des complications pulmonaires. Néanmoins, nos résultats ne peuvent exclure de manière définitive les effets délétères du vapotage et de l’utilisation de la cigarette électronique sur les poumons, et les anesthésiologistes devraient tenir compte des complications périopératoires potentielles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Electronic cigarettes (e-cigarettes) and vaping were developed to be a new substitute for smoking and were advertised as a safer option than conventional cigarettes despite the paucity of safety data. Electronic cigarettes entered the USA market around 2007 and have become the most common tobacco product used by American youths since 2014.1 According to a 2018 Centers for Disease Control report, 3.2% of USA adults (around 8.1 million) were current e-cigarette users.2
Fewer toxic chemicals have been detected in the aerosol from e-cigarettes compared with conventional cigarette smoking.3 Nevertheless, these new devices are not entirely harmless, and emerging pulmonary complications increase concerns about their safety. The most known harmful substance is vitamin E acetate, which is present in tetrahydrocannabinol (THC)-containing products, and has been associated with the development of e-cigarette or vaping product use associated lung injury (EVALI).4 Many other chemicals, flavours, and metals are also used in these devices and can lead to pulmonary toxicities.5,6,7
Hypoxemia and pulmonary complications are among the most common preventable postoperative complications independent of smoking and vaping.8,9 Postoperative hypoxemia is common and prolonged in patients recovering from major noncardiac surgery, with around 20% having at least 10 min·hr−1 of SpO2 < 90%.10 Postoperative hypoxemia can be caused by atelectasis, ventilator-induced lung injury, ventilation/perfusion mismatch, hypoventilation, and pulmonary edema.9,11,12 Hypoxemia is associated with prolonged hospitalization, intensive care unit admissions, mortality, and increased cost of care.
Available evidence suggests that vaping/e-cigarette use should be of concern to anesthesiologists, with a possible higher risk of postoperative hypoxemia and pulmonary complications. There are apparently no data on perioperative outcomes for patients who vape or use e-cigarettes. Therefore, we sought to undertake an evaluation of perioperative outcomes for vapers. Our primary hypothesis was that preoperative vaping/e-cigarette use, in adults undergoing noncardiothoracic surgery, is associated with increased hypoxemia (defined by the peripheral oxygen saturation divided by the fraction of inspired oxygen [SpO2/FIO2 ratio], a surrogate measure of oxygenation) during the first postoperative hour. Our secondary hypothesis was that vaping is associated with a higher risk of intraoperative and postoperative pulmonary complications compared with nonvaping.
Methods
The current analysis was a retrospective, single-centre, cohort study using data from the Cleveland Clinic Perioperative Health Documentation System (Cleveland, OH, USA) and was conducted after approval by the Institutional Review Board of the Cleveland Clinic Foundation on 7 April 2021, with waived individual consent.
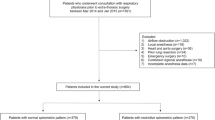
We included data from all adults undergoing noncardiothoracic surgeries lasting more than 1 hr under general anesthesia with mechanical ventilation at the Cleveland Clinic Main Campus between January 2015 and April 2021. We excluded data from patients who had missing postanesthesia care unit (PACU) SpO2 and FIO2 data, as well as patients who had another surgery during the same hospitalization or received mechanical ventilation during the 48 hr before surgery. Patients who were intubated within 24 hr after surgery were excluded from the primary analysis.
The exposure of interest was vaping/e-cigarette use within one year before surgery. It was identified from providers’ notes on social history in the electronic health record and by searching for the International Classification of Diseases (ICD)-10 code (F17.29) for vaping nicotine. We also planned to record the specific type of vaping and e-cigarettes, what substance was used (e.g., nicotine, THC, etc.), the frequency of use, and dual smoking/vaping status when these data were available. Control group patients were identified as patients who did not use e-cigarettes in the year before surgery. No restrictions were placed on the absence of vaping screening as it was unavailable for most patients. Conventional cigarette smokers were part of both the treatment and control groups, but we adjusted for smoking status as a confounder in our analysis.
Our primary outcome was time-weighted average (TWA) SpO2/FIO2 ratio in the PACU during the first postoperative hour. Peripheral oxygen saturation data were collected from the electronic record. Fraction of inspired oxygen was estimated from the type of device and the oxygen flow based on the conversion table (Electronic Supplementary Material [ESM] eTable 1), assuming that FIO2 was unchanged between recordings. The SpO2/FIO2 ratio has been used as a reliable continuous and noninvasive surrogate for the partial pressure of arterial oxygen to FIO2 (PaO2/FIO2) ratio in adults with acute lung injury and acute respiratory distress syndrome (ARDS),13,14 and accepted as a replacement for the PaO2/FIO2 ratio in the respiratory part of the Sequential Organ Failure Assessment score.15 A 10% difference in the SpO2/FIO2 ratio between the two groups, corresponding to a 10% change in SpO2 at a fixed FIO2, was considered significant, a threshold based on previous studies that showed a 10% decrease in PaO2/FIO2 from baseline was clinically meaningful for lung injury.16,17
Our secondary outcome was a collapsed composite of intraoperative and postoperative pulmonary complications that occurred at any time between the beginning of the surgery and 72 hr postoperatively or discharge, whichever came first. This outcome was defined as the presence of at least one of the following complications as identified by their ICD-9/ICD-10 codes, including but not limited to: pulmonary infection and pneumonia, respiratory failure, bronchospasm, atelectasis, pulmonary oedema, pneumothorax, ARDS, pulmonary embolism, and all vaping-related disorders (ESM eTable 2).
Statistical analysis
For our primary hypothesis, we estimated the average treatment effect on the treated (ATT) for the TWA SpO2/FIO2 ratio. The ATT represents the effect of being exposed to vaping in our current vaping population and thus, correspondingly, how much harm could be prevented if patients were prevented from vaping. We used entropy balancing to adjust for confounding. This is similar to inverse probability of treatment weighting using logistic regression models, but offers certain advantages.18 Inverse probability of treatment weighting using logistic regression models is often an iterative process in which the propensity score model is tweaked and modified until satisfactory balance is achieved on confounders. Entropy balancing, on the other hand, uses optimization techniques to directly find weights that balance covariates between the two groups, thus obviating the need to perform an ad hoc search for the correct model specification.19
To calculate the ATT, we first estimated the weights using entropy balancing. All patients in the vaping group received a weight of 1, while patients in the nonvaping group received the estimated weight wi. Intuitively, the idea is to give more weight to nonvapers who are similar to vapers on confounder distribution, and less weight to those who are dissimilar. The distribution of weights was examined, and extreme weights were removed by trimming to the first and 99th percentile. Then, we evaluated the balance on the specified covariates using the absolute standardized difference (ASD), with an ASD > 0.10 indicating imbalance. Weighted outcome regression models were then fit to estimate ATT.
In the primary analysis, ATT mean difference was estimated using a weighted linear regression model with the TWA SpO2/FIO2 ratio as the outcome and vaping/e-cigarette use as the primary covariate of interest. Robust standard errors were calculated using the sandwich estimator. We adjusted for smoking status, comorbidities, and demographic factors (Table 1).
For the secondary analysis, we used a similar procedure. We fitted a weighted logistic regression model to estimate the ATT odds ratio with a composite of intraoperative and postoperative pulmonary complications as the outcome and vaping/e-cigarette use status as the primary covariate of interest. Robust standard errors were calculated using the sandwich estimator.
We conducted two sensitivity analyses: the first one was conducted using the minimum SpO2/FIO2 as the outcome instead of TWA SpO2/FIO2. In the second one, we defined certain confounders to be treated as mediators. This is because a limitation of our analysis is that the patients were measured at only one time point. Thus, it is possible that some of the listed confounders are in fact mediators (e.g., a patient could have developed chronic obstructive pulmonary disease [COPD] after they started vaping). Lung cancer, COPD, and asthma were identified as potential mediators (Figure). These mediators were not used when calculating the new weights, allowing us to estimate the total effect of vaping.
All analyses were conducted at a significance level of 0.05. R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analyses.
Sample size justification
Planned
Based on a preliminary query, about 300 out of 10,000 surgery patients at the Cleveland Clinic used vaping/e-cigarettes per year. Assuming a TWA PACU SpO2/FIO2 ratio mean of 300 and a residual standard deviation of 80 after adjusting for other confounders and without considering any interaction, we planned to have more than 80% power to detect a difference of 10 or larger, assuming a minimal final sample size of 600 vapers and 19,400 nonvapers.
Actual
The final primary analysis population had 1,907 vapers out of a total of 109,217 patients. Weighting procedures, such as entropy balancing or inverse probability of treatment weighting, generally increase the variance of statistical estimates, which should be taken into account when estimating the power. The effective sample size (ESS) is a metric that quantifies this loss of precision and represents the number of unweighted observations that the weighted observations would be equivalent to. After weighting, the ESS was 1,907 vapers and 40,608 nonvapers. Keeping other parameters the same as before, we had more than 80% power to detect a mean difference of 10 or larger for TWA SpO2/FIO2 ratio as planned.
Results
We identified a total of 110,940 patients (1,941 vapers) who met the specified inclusion and exclusion criteria for the study. Of these, 109,217 (1,907 vapers) patients were included in the primary analysis after excluding patients with missing outcomes data, and those who were intubated in the 24 hr following surgery. There were no meaningful differences in the rates at which vapers were excluded for postoperative intubation (0.9%) compared with nonvapers (0.8%). All patients were included in the secondary analysis. For the primary analysis, we achieved satisfactory balance (ASD < 0.1) on all variables using entropy balancing (Table 1, Figure).
In the PACU, oxygen was delivered with a nasal cannula in 85% of the patients, with simple face masks in 14% of the patients, and with other devices in less than 1% of the patients (ESM eTable 3). This distribution was similar between both groups.
The unadjusted median [interquartile range] TWA SpO2/FIO2 ratio (N = 109,217) was 350 [302–396] in the vaping group and 348 [297–379] in the nonvaping group. The ATT mean difference [vapers − nonvapers] for the TWA SpO2/FIO2 ratio was estimated to be 4 (95% confidence interval [CI], 1 to 8; P = 0.007). This is equivalent to a 4% change in SpO2 at a 30% FIO2 (or at a fixed FIO2). The estimated treatment effect was statistically significant (Table 2). The interaction between vaping and smoking status was not statistically significant (P = 0.22). Similar results were observed when repeating the analysis with a more fine-grained categorization of smoking status, i.e., current smoker, former smoker, and never smoker (ESM eTable 4).
The intraoperative and postoperative pulmonary complications (N = 110,940) incidence was 1.4% (n = 27) in the vaping group and 1.3% (n = 1,447) in the nonvaping group. The ATT odds ratio (vapers/nonvapers) for experiencing pulmonary complications was estimated to be 1.04 (95% CI, 0.71 to 1.54; P = 0.84). The estimated treatment effect was not statistically significant (Table 2).
Our first sensitivity analysis showed that, when we used the minimum SpO2/FIO2 ratio as the outcome, the ATT mean difference was estimated to be 2 (95% CI, −2 to 5; P = 0.35). The average minimum SpO2/FIO2 ratio was estimated to be 309 (95% CI, 303 to 315) in the vaping group and 307 (95% CI, 301 to 303) in the nonvaping group.
In the second analysis, we excluded predefined mediators, i.e., asthma, COPD, and lung cancer. The ATT mean difference for the TWA SPO2/FIO2 ratio was estimated to be 4 (95% CI, 1 to 7; P = 0.01). The mean TWA SpO2/FIO2 ratio was estimated to be 348 (95% CI, 344 to 352) in the vaping group and 344 (95% CI, 342 to 346) in the nonvaping group.
Discussion
Our primary outcome was hypoxemia (SpO2/FIO2 ratio), a reliable surrogate for the PaO2/FIO2 ratio.13,14 We used this outcome to power the detection of vaping/e-cigarette use effect on the lungs even without having a definite documented diagnosis of a pulmonary complication. Although there is no other available perioperative data regarding vaping/e-cigarette use and hypoxemia that we can refer to or establish a comparison with, it is worth reporting that, in the nonoperative setting, hypoxia was the main presenting vital abnormality in vapers/e-cigarette users that were subsequently diagnosed with EVALI.20 Based on these data, we expected to observe more severe hypoxemia in vapers/e-cigarette users than in nonusers. The results of our analysis ultimately did not support this hypothesis.
Vaping/e-cigarette use was also not associated with a statistically significant increase in intraoperative and postoperative pulmonary complications. As with hypoxemia, there are no perioperative data on the effects of vaping on postoperative pulmonary complications. Nevertheless, a previous study in the nonoperative setting compared the lung function of 30 healthy individuals who had vaped in the last six months to 30 control individuals who had not. In the vaping group, they observed a significant reduction in lung function secondary to peripheral obstructive airway disease.21
Multiple factors could explain the lack of evidence for an association between vaping and pulmonary complications observed in our study. One important reason might be that our population was at lower risk of developing pulmonary complications. Only 28% had intra-abdominal surgeries, where complications are common. Another reason might be that we did not account for duration or intensity of vaping. It is reasonable to hypothesize that higher levels of exposure to vaping would result in greater lung damage. It has been shown that prolonged exposure to toxic substances and more severe lung damage is needed to detect postoperative pulmonary complications in middle age.22,23,24 Nevertheless, these details were not available for our analysis.
Our results should be interpreted cautiously considering the many limitations of our study. One limitation is that we used SpO2 as a continuous and noninvasive surrogate, instead of arterial blood samples, to assess postoperative lung function in the PACU. Nevertheless, the SpO2/FIO2 ratio is a validated measure of oxygenation that allows continuous and early detection of impaired oxygenation and lung injury, and it is a predictor of early development of ARDS and hospital mortality.13,25,26 Another limitation is that we assessed oxygenation only within the first hour of admission to the PACU. Therefore, delayed effects of vaping on oxygenation would be overlooked. A third important limitation is the risk of exposure underdocumentation since it is a new entity in preoperative screening. This would explain the low prevalence of vaping in our patient population compared with estimates from other studies. In general, providers are not used to completing and documenting vaping and e-cigarette use, or they may erroneously document it as smoking, which could be confused with cigarette smoking. Nevertheless, the Cleveland Clinic has already added a specific screening tool for vaping to its electronic medical record system, and we also used a free-text search to enhance the detection of exposure. A related limitation is that the specific type of substance used does not need to be documented in the screening tool. It is important to differentiate between nicotine, cannabidiol, THC, butane hash oils (dabs), and many other illicit products that can cause a different range of complications.27 Unfortunately, we did not have sufficient data to disaggregate the effects of different substances. Moreover, the extent to which patients abstained from vaping before surgery, which would impact the harmful effect on lungs, was also not documented. Finally, it is worth mentioning that most of the patients in the exposure group were either current or former smokers, and although the interaction between vaping and smoking status was not significant, we had only limited power to assess differential effects of vaping in nonsmokers compared with smokers.
In summary, our analysis of patients undergoing noncardiothoracic surgery did not show evidence of a clinically meaningful association between vaping/e-cigarette use, and either hypoxemia during the first hour in PACU or an increased risk of postoperative pulmonary complications. Nevertheless, our findings cannot definitively exclude the deleterious effects of vaping and e-cigarette use on the lungs, and anesthesiologists should consider potential perioperative complications.
References
Centers for Disease Control and Prevention. Surgeon General’s advisory on e-cigarette use among youth; 2018. Available from URL: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/surgeon-general-advisory/index.html (accessed April 2024).
Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults—United States, 2018. MMWR Morb Mortal Wkly Rep 2019; 68: 1013–9. https://doi.org/10.15585/mmwr.mm6845a2
National Academies of Sciences E, Medicine, Health, et al. In: Eaton DL, Kwan LY, Stratton K, eds. Public Health Consequences of E-Cigarettes. National Academies Press; 2018.
Blount BC, Karwowski MP, Morel-Espinosa M, et al. Evaluation of bronchoalveolar lavage fluid from patients in an outbreak of e-cigarette, or vaping, product use-associated lung injury—10 states, August–October 2019. MMWR Morb Mortal Wkly Rep 2019; 68: 1040–1. https://doi.org/10.15585/mmwr.mm6845e2
Iskandar AR, Zanetti F, Marescotti D, et al. Application of a multi-layer systems toxicology framework for in vitro assessment of the biological effects of Classic Tobacco e-liquid and its corresponding aerosol using an e-cigarette device with MESH™ technology. Arch Toxicol 2019; 93: 3229–47. https://doi.org/10.1007/s00204-019-02565-9
Williams M, Li J, Talbot P. Effects of model, method of collection, and topography on chemical elements and metals in the aerosol of tank-style electronic cigarettes. Sci Rep 2019; 9: 13969. https://doi.org/10.1038/s41598-019-50441-4
Antonini JM, Taylor MD, Zimmer AT, Roberts JR. Pulmonary responses to welding fumes: role of metal constituents. J Toxicol Environ Health A 2004; 67: 233–49. https://doi.org/10.1080/15287390490266909
The LAS VEGAS Investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS—an observational study in 29 countries. Eur J Anaesthesiol 2017; 34: 492–507. https://doi.org/10.1097/eja.0000000000000646
Canet J, Sabaté S, Mazo V, et al. Development and validation of a score to predict postoperative respiratory failure in a multicentre European cohort: a prospective, observational study. Eur J Anaesthesiol 2015; 32: 458–70. https://doi.org/10.1097/eja.0000000000000223
Sun Z, Sessler DI, Dalton JE, et al. Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Anesth Analg 2015; 121: 709–15. https://doi.org/10.1213/ane.0000000000000836
Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G. Re-expansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth 1993; 71: 788–95. https://doi.org/10.1093/bja/71.6.788
Suzuki S. Oxygen administration for postoperative surgical patients: a narrative review. J Intensive Care 2020; 8: 79. https://doi.org/10.1186/s40560-020-00498-5
Rice TW, Wheeler AP, Bernard GR, et al. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 2007; 132: 410–7. https://doi.org/10.1378/chest.07-0617
Festic E, Bansal V, Kor DJ, Gajic O. SpO2/FiO2 ratio on hospital admission is an indicator of early acute respiratory distress syndrome development among patients at risk. J Intensive Care Med 2015; 30: 209–16. https://doi.org/10.1177/0885066613516411
Pandharipande PP, Shintani AK, Hagerman HE, et al. Derivation and validation of SpO2/FiO2 ratio to impute for PaO2/FiO2 ratio in the respiratory component of the sequential organ failure assessment score. Crit Care Med 2009; 37: 1317–21. https://doi.org/10.1097/ccm.0b013e31819cefa9
Douville NJ, Jewell ES, Duggal N, et al. Association of intraoperative ventilator management with postoperative oxygenation, pulmonary complications, and mortality. Anesth Analg 2020; 130: 165–75. https://doi.org/10.1213/ane.0000000000004191
Hovaguimian F, Lysakowski C, Elia N, Tramèr MR. Effect of intraoperative high inspired oxygen fraction on surgical site infection, postoperative nausea and vomiting, and pulmonary function: systematic review and meta-analysis of randomized controlled trials. Anesthesiology 2013; 119: 303–16. https://doi.org/10.1097/aln.0b013e31829aaff4
Hainmueller J, Xu Y. Ebalance: a Stata package for entropy balancing. J Stat Softw 2013; 54. https://doi.org/10.2139/ssrn.1943090
Harvey RA, Hayden JD, Kamble PS, Bouchard JR, Huang JC. A comparison of entropy balance and probability weighting methods to generalize observational cohorts to a population: a simulation and empirical example. Pharmacoepidemiol Drug Saf 2017; 26: 368–77. https://doi.org/10.1002/pds.4121
Pajak A, Bascoy S, Li JC, Benninghoff M, Deitchman A. E-cigarette or vaping product use associated lung injury among three young adults: a retrospective case series from Delaware. Cureus 2020; 12: e11031. https://doi.org/10.7759/cureus.11031
Meo SA, Ansary MA, Barayan FR, et al. Electronic cigarettes: impact on lung function and fractional exhaled nitric oxide among healthy adults. Am J Mens Health 2019; 13: 1557988318806073. https://doi.org/10.1177/1557988318806073
Marini S, Buonanno G, Stabile L, Ficco G. Short-term effects of electronic and tobacco cigarettes on exhaled nitric oxide. Toxicol Appl Pharmacol 2014; 278: 9–15. https://doi.org/10.1016/j.taap.2014.04.004
Flouris AD, Chorti MS, Poulianiti KP, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol 2013; 25: 91–101. https://doi.org/10.3109/08958378.2012.758197
Blagev DP, Harris D, Dunn AC, Guidry DW, Grissom CK, Lanspa MJ. Clinical presentation, treatment, and short-term outcomes of lung injury associated with e-cigarettes or vaping: a prospective observational cohort study. Lancet 2019; 394: 2073–83. https://doi.org/10.1016/s0140-6736(19)32679-0
Sleiman M, Logue JM, Montesinos VN, et al. Emissions from electronic cigarettes: key parameters affecting the release of harmful chemicals. Environ Sci Technol 2016; 50: 9644–51. https://doi.org/10.1021/acs.est.6b01741
Centers for Disease Control and Prevention. Outbreak of severe pulmonary disease associated with using e-cigarette, or vaping, products; 2020. Available from URL: https://archive.cdc.gov/www_cdc_gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html (accessed May 2024).
Breitbarth AK, Morgan J, Jones AL. E-cigarettes—an unintended illicit drug delivery system. Drug Alcohol Depend 2018; 192: 98–111. https://doi.org/10.1016/j.drugalcdep.2018.07.031
Author contributions
Remie Saab, Eva Rivas, Esra Kutlu Yalcin, Lloyd Chen, Mateo Montalvo, Federico Almonacid-Cardenas, Kurt Ruetzler, and Alparslan Turan contributed to the conception and design of the study. Remie Saab, Eva Rivas, Esra Kutlu Yalcin, Lloyd Chen, Mateo Montalvo, Federico Almonacid-Cardenas, Karan Shah, and Alparslan Turan contributed to the acquisition of data. Karan Shah, Remie Saab, Eva Rivas, and Alparslan Turan contributed to the analysis of data. Karan Shah, Remie Saab, Eva Rivas, and Alparslan Turan contributed to the interpretation of data.
Disclosures
None of the authors has a conflict of interest.
Funding statement
No external funding and no competing interests declared. This study was supported by internal funding from the Department of Outcomes Research, Cleveland Clinic, Cleveland, OH, USA.
Prior conference presentations
Poster presentation at the 2022 American Society of Anesthesiologists Annual Meeting (18–22 October, Philadelphia, PA, USA).
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Saab, R., Rivas, E., Yalcin, E.K. et al. The association of vaping and electronic cigarette use with postoperative hypoxemia and respiratory complications: a retrospective cohort analysis. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02801-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02801-6