Abstract
Purpose
The benefits of intraoperative dialysis during orthotopic liver transplantation remain controversial. In patients with anuric renal failure and portopulmonary hypertension, maintaining venous return during caval clamping and unclamping along with minimizing fluid overload is critical to avoiding right ventricular strain and failure.
Clinical features
We present the case of a 54-yr-old female who underwent orthotopic liver transplantation for alcohol-related liver disease with acute decompensation including severe hepatorenal syndrome (anuric requiring dialysis), probable hepatopulmonary syndrome, moderate pulmonary hypertension (right ventricular systolic pressure, 44 mm Hg), hepatic encephalopathy (grade 2), and esophageal varices. Prior to incision, pulmonary arterial pressures were 48/28 (mean, 35) mm Hg with a central venous pressure of 30 mm Hg, cardiac output of 7.4 L·min−1, and pulmonary vascular resistance of 98 dynes·sec·cm−5. In the context of right ventricular strain and volume overload observed on transthoracic echocardiography, we inserted an additional dialysis catheter into the right femoral vein. We initiated dialysis using the two catheters as a circuit (femoral line to the dialysis machine; blood was reinjected via the subclavian line) acting as a limited venovenous bypass, allowing right ventricular offloading and hemodialysis throughout the case. We removed 4.5 L via hemodialysis during the surgery, while avoiding acidosis, hyperkalemia, and sodium shifts. The patient tolerated reperfusion adequately despite pre-existing right ventricular dilation and dysfunction.
Conclusion
We report on the use two hemodialysis catheters in a patient undergoing orthotopic liver transplantation as a circuit for simultaneous anuric hepatorenal syndrome and moderate pulmonary hypertension with right ventricular dilation and dysfunction. We believe this technique was instrumental in the patient’s successful transplant.
Résumé
Objectif
Les avantages de la dialyse peropératoire pendant une transplantation hépatique orthotopique demeurent controversés. Chez la patientèle atteinte d’insuffisance rénale anurique et d’hypertension portopulmonaire, il est essentiel de maintenir le retour veineux pendant le clampage et le déclampage de la veine cave ainsi que de minimiser la surcharge hydrique, afin d’éviter la déformation et l’insuffisance ventriculaires droites.
Caractéristiques cliniques
Nous présentons le cas d’une femme de 54 ans qui a bénéficié d’une transplantation hépatique orthotopique pour une maladie hépatique liée à l’alcool avec une décompensation aiguë comprenant un syndrome hépatorénal sévère (anurie nécessitant une dialyse), un syndrome hépatopulmonaire probable, une hypertension pulmonaire modérée (pression systolique ventriculaire droite, 44 mm Hg), une encéphalopathie hépatique (grade 2) et des varices œsophagiennes. Avant l’incision, les pressions artérielles pulmonaires étaient de 48/28 (moyenne, 35) mm Hg avec une pression veineuse centrale de 30 mm Hg, un débit cardiaque de 7,4 L·min−1 et une résistance vasculaire pulmonaire de 98 dynes·sec·cm−5. Dans le contexte de la déformation ventriculaire et de la surcharge volémique droites observées à l’échocardiographie transthoracique, nous avons inséré un cathéter de dialyse supplémentaire dans la veine fémorale droite. Nous avons amorcé la dialyse en créant un circuit avec les deux cathéters (ligne fémorale en direction de l’appareil de dialyse; sang réinjecté via la ligne sous-clavière) agissant comme un pontage veino-veineux limité, permettant la décharge du ventricule droit et l’hémodialyse tout au long du cas. Nous avons retiré 4,5 L par hémodialyse pendant la chirurgie, tout en évitant l’acidose, l’hyperkaliémie et les changements en sodium plasmatique. La patiente a toléré la reperfusion de manière adéquate malgré la dilatation et le dysfonctionnement préexistants du ventricule droit.
Conclusion
Nous rapportons l’utilisation de deux cathéters d’hémodialyse pour créer un circuit chez une patiente bénéficiant d’une transplantation hépatique orthotopique pour le traitement d’un syndrome hépatorénal anurique simultané à une hypertension pulmonaire modérée avec dilatation et dysfonctionnement du ventricule droit. Nous pensons que cette technique a joué un rôle déterminant dans la réussite de la greffe chez la patiente.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The use of intraoperative hemodialysis (HD) during liver transplantation remains a topic of debate. Intraoperative HD is safe,1,2 but its effectiveness is contentious and it is not used routinely at all high-volume centres.3 The benefits of intraoperative HD are purported to include improved control of acid-base and electrolyte balance, improved fluid balance, temperature management, and improved hemodynamic stability particularly with respect to reperfusion and postreperfusion syndrome.4,5 Furthermore, a technique has been described wherein two dialysis catheters are placed: one above (subclavian or internal jugular vein) and one below (femoral vein) the diaphragm.4 This technique has been used to optimize dialysis efficiency by minimizing recirculation6 and is used in the management of poisoning cases. In liver transplantation, this approach can mimic a limited venovenous bypass with no requirement for systemic heparinization. We have used this technique once before at our centre in a patient with anuric hepatorenal syndrome, volume overload, and refractory hypotension despite high vasopressor doses.
In patients with portopulmonary hypertension and an element of right ventricular dysfunction, liver transplantation is a very high-risk procedure, with graft reperfusion being the most concerning phase.7,8 Dialysis may help reduce pulmonary hypertension and ventricular volume in patients with end-stage renal disease.9,10 Intraoperative HD may thus be used for this goal in portopulmonary hypertension.11,12 Using the technique described with two dialysis catheters, we hypothesized that we could optimize venous return during caval clamping, mitigate the changes to preload observed with caval clamping and unclamping, and help sustain hemodialysis efficiency and fluid removal in our patient with right ventricular dilation and dysfunction. We report on the successful use of limited venovenous bypass and intraoperative HD for liver transplantation in a high-risk patient with pulmonary hypertension and right ventricular dysfunction.
Case report
Preoperative
Written informed consent was obtained from the patient prior to publication of this report. A 54-yr-old White woman with chronic alcoholic liver disease and acute decompensation presented for liver transplantation. In the three months prior to the transplant, she was admitted to hospital for sepsis and decompensated liver failure with a MELD-Na score of 32. Transthoracic echocardiography (TTE) performed three months before the transplant showed normal biventricular function with right ventricular systolic pressure estimated at 44 mm Hg with no right heart catheterization. Two months prior to the transplant, she developed severe hepatorenal syndrome and was dialysis-dependent via a tunnelled right subclavian hemodialysis line. Immediately prior to the transplant, she had grade 2 hepatic encephalopathy, ascites requiring one paracentesis (5 L one week prior to the transplant) and gastric varices with no bleeding. Her last dialysis session finished four hours before surgery and was stopped prematurely for hemodynamic instability, which had been a recurring issue resulting in volume overload. She also had new hypoxia (possibly hepatopulmonary syndrome, but a bubble study was not done) superimposed with moderate right and small left pleural effusions requiring bi-level positive airway pressure in the intensive care unit (ICU) with 70% inspired oxygen (PaO2, 138 mm Hg; P/F ratio, 197 mm Hg). Her preoperative blood work included hemoglobin, 70 g·L−1; platelets, 128 × 109 L−1; international normalized ratio, 1.7; creatinine, 212 umol·L−1; sodium, 143 mmol·L−1; potassium, 4.0 mmol·L−1; total bilirubin, 103 umol·L−1; albumin, 39 g·L−1; glucose, 6.1 mmol·L−1; aspartate aminotransferase, 42 U·L−1; alanine aminotransferase, 14 U·L−1; alkaline phosphatase, 137 U·L−1; and lipase, 186 U·L−1. She arrived at the operating room on norepinephrine 0.1 µg·kg−1·min−1 and vasopressin 4 U·hr−1 (see Figs 1 and 2 for a timeline of hemodynamics and vasopressors).
Intraoperative hemodynamics during orthotopic liver transplant. (A) Systemic blood pressure (in mm Hg) recording systolic (circle), diastolic (triangle) and mean (square) arterial pressures; (B) pulmonary artery pressures (in mm Hg) recording systolic (circle), diastolic (triangle), and mean (square) pulmonary artery pressures; (C) central venous pressure (in mm Hg).
Noted event markers signify: 1 = intubation; 2 = decision to proceed with transplant; 3 = start hemodialysis and surgical incision (start preanhepatic phase); 4 = portal vein clamp (start anhepatic phase); 5 = reperfusion (start neohepatic phase); 6 = infrarenal aortic clamp (for aorto-hepatic artery bypass); 7 = release of infrarenal aortic clamp
Intraoperative vasopressor infusions during orthotopic liver transplant. Left y-axis: norepinephrine (circle) and epinephrine (square) infusion rates (µg·kg−1·min−1); right y-axis: vasopressin (triangle) infusion rate (U·hr−1).
Noted event markers signify: 1 = intubation; 2 = decision to proceed with transplant; 3 = start hemodialysis and surgical incision (start preanhepatic phase); 4 = portal vein clamp (start anhepatic phase); 5 = reperfusion (start neohepatic phase); 6 = infrarenal aortic clamp (for aorto-hepatic artery bypass); 7 = release of infrarenal aortic clamp
Intraoperative
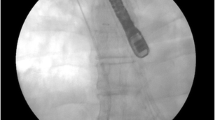
Following induction and intubation, central intravenous access in the right jugular vein was obtained with a 16-cm 7-Fr triple lumen catheter and a 9-Fr introducer sheath through which a pulmonary artery catheter was inserted and floated into the pulmonary artery. Pulmonary artery pressures initially were 48/28 mm Hg (mean, 35 mm Hg) with a central venous pressure (CVP) of 30 mm Hg. Pulmonary artery pressures were half systemic at this time (Fig. 1). We elected not to insert a transesophageal probe because of her known varices and the presence of blood in the mouth noted during intubation. We obtained a point-of-care TTE, which showed a moderately dilated right ventricle with depressed function. Cardiac output was 7.4 L·min−1 and pulmonary vascular resistance was 98 dynes·sec·cm−5, which supported high-flow pulmonary hypertension related to fluid overload.
It was unclear the extent to which our hemodynamic and TTE findings were related to portopulmonary hypertension vs volume overload. We elected to proceed with the transplant after inserting a second hemodialysis catheter into the right femoral vein. We then initiated HD: filter FX 60 (Fresenius Medical Care, Bad Homburg, Germany), blood flow 200 mL·min−1, and dialysate flow 300 mL·min−1 with no anticoagulation. The femoral catheter was the outflow to the dialysis machine and the subclavian catheter was the inflow from the dialysis machine. In this manner, we were able to offload the right ventricle via fluid removal, minimize recirculation, ensure adequate venous return during caval clamping, and minimize the sudden increase in preload with caval unclamping. We began with net fluid removal at 0.5 L·hr−1 with a potassium bath of 4 mmol·L−1. Serial arterial blood gases showed normal pH and potassium with otherwise benign biochemistry for a critically unwell patient (Table 1).
Starting HD and performing the laparotomy nearly simultaneously led to improvements in CVP and pulmonary pressure (Fig. 1), though high-dose vasopressors were still required (Fig. 2). Given the anticipated hemodynamic challenge of complete caval clamping, a cavo-cavostomy surgical approach was used, allowing for partial tangential caval clamping lasting 33 min. We continued hemodialysis at the same flows and fluid target during the anhepatic phase and the patient’s hemodynamics improved, potentially related to further reduction in right ventricular strain from fluid overload.
Immediately prior to reperfusion after 150 min of functional anhepatic time after liver devascularization, we paused the fluid removal and continued ultrafiltration with neutral fluid balance. Reperfusion was tolerated with volatile hemodynamic swings, but the patient was stabilized and fluid removal was restarted after 11 min. Poor flow was noted in the hepatic artery after arterial reperfusion. This required an infrarenal aortic conduit using a donor iliac artery, requiring infrarenal clamping of the aorta for 24 min, with significant improvement in arterial flow. This prolonged the surgical time between reperfusion and the end of the case (see Fig. 1). During this time, the liver became increasingly congested. The hourly fluid removal target was increased to 0.75 L·hr−1 for the remainder of the case. The patient continued to require three vasopressors for the remainder of the case and was transferred to the ICU after more than eight hours of surgical time. At the end of the case, the CVP was 11 mm Hg and the hepatic graft continued to be congested despite 4.5 L of fluid removal via HD (see Table 2 for fluid balance). To avoid any excess pressure on the liver, the abdomen was temporarily closed with a negative pressure dressing.
Postoperative
The patient was brought to the ICU intubated, ventilated, and sedated. The ICU team restarted sustained low-efficiency dialysis (SLED), which continued for 48 consecutive hours to remove 4 L. On postoperative day 2, she tolerated fluid removal with SLED with lower vasopressor doses and was able to return to the operating room for abdominal closure. The liver graft appeared well perfused with no congestion. She required continued ventilation until postoperative day 10 because of a combination of bilateral pleural effusions (each were drained with chest tubes) and high work of breathing. After being extubated, she still required a prolonged ICU stay in the context of continued vasopressor requirements, especially during sessions of SLED and eventually intermittent HD. She was transferred out of ICU after 33 days and eventually was discharged from hospital. Three months after her liver transplantation (five months after starting HD), she exhibited renal recovery and her dialysis line was removed.
Discussion
We present a case of a high-risk patient with pulmonary hypertension, probable hepatopulmonary syndrome, severe hepatorenal syndrome, and volume overload for orthotopic liver transplantation. We employed supra- and infradiaphragmatic dialysis catheters in a circuit (blood drawn from the femoral line to the dialysis machine and reinjected into the subclavian line) to minimize changes to preload observed with caval clamping and unclamping and to help sustain hemodialysis efficiency and fluid removal particularly during the anhepatic phase in our patient with right ventricular dilation and dysfunction. The use of dual dialysis catheters during liver transplantation has been described4 and we have previously used this technique in a liver transplant patient with marked hemodynamic instability. Here, we report its use for anuric hepatorenal syndrome with moderate pulmonary hypertension and right ventricular dysfunction.
Hepatorenal syndrome is one of the most common severe complications in decompensated cirrhosis and is the leading cause of death in advanced cirrhosis patients.13,14 Pretransplant hepatorenal syndrome is known to be associated with increased ICU length of stay and short-term mortality,15 though pretransplant HD does not independently predict postoperative mortality.16 Our patient exhibited anuric hepatorenal syndrome for the preceding two months and marked volume overload from suboptimal fluid removal due to hemodynamic instability since HD began. The patient’s hypervolemic status was tenuous as it was likely contributing to the measured pulmonary hypertension along with the new right ventricular dilation and dysfunction seen on intraoperative TTE. The extent of hypervolemia was apparent when pulmonary and central venous pressures decreased upon initiating HD with abdominal decompression with the laparotomy, and even further after application of a partial caval cross-clamp during the anhepatic phase. While a single HD line would likely have been acceptable to achieve our goal of intraoperative fluid removal, the second HD line in our case assisted in sustaining HD efficiency in the context of caval clamping and unclamping. Despite being nearly fluid neutral (+0.9 L, not accounting for insensible losses), she exhibited hepatic congestion and tissue edema such that her abdomen could not be closed until two days later.
Volume overload in patients undergoing liver transplantation can be detrimental and even life threatening. Our patient had high-flow pulmonary hypertension and associated right ventricular dysfunction, which we believe was primarily explained by volume overload. Acute right ventricular failure during the reperfusion and postreperfusion phases is an important concern for patients with pre-existing right ventricular dilation and/or dysfunction.17 To this end, right ventricular function is partially preload dependent. Excessive right ventricular preload, as would be expected during caval unclamping during a liver transplantation, can lead to acute dilation and dysfunction.18 By using a femoral dialysis catheter to bypass the partial caval clamp and reinject into the subclavian vein (instead of the convention of a single dialysis line), we were better able to maintain venous return during the anhepatic phase. We believe that this was also important in mitigating the sudden and substantial increase in preload that would have occurred with caval unclamping.
Despite our best efforts to maintain euvolemia with intraoperative HD, the patient remained volume overloaded with graft congestion and the abdomen could not be safely approximated. As the patient required a massive transfusion and had no urine output, the only method of fluid removal other than sequestration with hemoconcentration was HD. Despite high vasopressor and inotropic requirements, we were able to remove 4.5 L of fluid with HD. Her fluid balance at the end of the case was + 0.9 L (Table 2). Postoperative biochemistry and imaging indicated that the hepatic graft was functioning well. We are confident that without the use of intraoperative dialysis in this patient, graft dysfunction secondary to severe congestion and right ventricular failure could have potentially threatened the patient’s life and new liver in the perioperative period.
Conclusion
We present a case of a high-risk patient having successful orthotopic liver transplantation with the use of infra- and supradiaphragmatic dialysis catheters as a circuit from below to above the diaphragm. This system allowed for a limited venovenous bypass to offload the overloaded right ventricle, to remove fluid in a patient with anuric hepatorenal syndrome, and minimize electrolyte disturbances during the various stages of surgery. While the use of intraoperative HD is centre-dependent with a lack of evidence to guide its implementation, we believe it was instrumental in this case to allow for the patient to safely undergo liver transplantation. The use of limited systemic bypass via insertion of two dialysis catheters may be a useful strategy in volume-overloaded patients presenting for liver transplantation with pulmonary hypertension and right ventricular strain.
References
Kościelska M, Matuszkiewicz-Rowińska J, Zieniewicz K, et al. Intraoperative dialysis during liver transplantation. Transplant Proc 2020; 52: 2454–8. https://doi.org/10.1016/j.transproceed.2020.01.129
Karvellas CJ, Taylor S, Bigam D, et al. Intraoperative continuous renal replacement therapy during liver transplantation: a pilot randomized-controlled trial (INCEPTION). Can J Anesth 2019; 66: 1151–61. https://doi.org/10.1007/s12630-019-01454-0
Adelmann D, Olmos A, Liu LL, et al. Intraoperative management of liver transplant patients without the routine use of renal replacement therapy. Transplantation 2018; 102: e229–35. https://doi.org/10.1097/tp.0000000000002137
Bohorquez H, Koyner JL, Jones CR. Intraoperative renal replacement therapy in orthotopic liver transplantation. Adv Kidney Dis Health 2023; 30: 378–86. https://doi.org/10.1053/j.akdh.2023.03.003
Agopian VG, Dhillon A, Baber J, et al. Liver transplantation in recipients receiving renal replacement therapy: outcomes analysis and the role of intraoperative hemodialysis. Am J Transplant 2014; 14: 1638–47. https://doi.org/10.1111/ajt.12759
Twardowski ZJ, Van Stone JC, Jones ME, Klusmeyer ME, Haynie JD. Blood recirculation in intravenous catheters for hemodialysis. J Am Soc Nephrol 1993; 3: 1978–81. https://doi.org/10.1681/asn.v3121978
Krowka MJ, Plevak DJ, Findlay JY, Rosen CB, Wiesner RH, Krom RA. Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl 2000; 6: 443–50. https://doi.org/10.1053/jlts.2000.6356
Lai YK, Kwo PY. Portopulmonary hypertension. Clin Liver Dis 2023; 27: 71–84. https://doi.org/10.1016/j.cld.2022.08.002
Chan CT, Greene T, Chertow GM, et al. Effects of frequent hemodialysis on ventricular volumes and left ventricular remodeling. Clin J Am Soc Nephrol 2013; 8: 2106–16. https://doi.org/10.2215/cjn.03280313
Girsberger M, Chan CT. Retrospective single center cohort study: effect of intensive home hemodialysis on right ventricular systolic pressure and clinical outcomes. BMC Nephrol 2020; 21: 508. https://doi.org/10.1186/s12882-020-02159-z
Gupta R, Gan TJ. Peri-operative fluid management to enhance recovery. Anaesthesia 2016; 71: 40–5. https://doi.org/10.1111/anae.13309
Kandil S. Intraoperative anesthetic management of the liver transplant recipient with portopulmonary hypertension. Curr Opin Organ Transplant 2019; 24: 121–30. https://doi.org/10.1097/mot.0000000000000613
Bucsics T, Mandorfer M, Schwabl P, et al. Impact of acute kidney injury on prognosis of patients with liver cirrhosis and ascites: a retrospective cohort study. J Gastroenterol Hepatol 2015; 30: 1657–65. https://doi.org/10.1111/jgh.13002
Wang S, Zhou Z, Xu C, et al. Establishment and evaluation of an early prediction model of hepatorenal syndrome in patients with decompensated hepatitis B cirrhosis. BMC Gastroenterol 2023; 23: 1. https://doi.org/10.1186/s12876-022-02618-x
Horvatits T, Hübener P, Touma M, et al. Improvement of renal function prior to liver transplantation is not associated with better long-term renal outcome or survival. Ann Hepatol 2021; 26: 100559. https://doi.org/10.1016/j.aohep.2021.100559
Sharma P, Goodrich NP, Zhang M, Guidinger MK, Schaubel DE, Merion RM. Short-term pretransplant renal replacement therapy and renal nonrecovery after liver transplantation alone. Clin J Am Soc Nephrol 2013; 8: 1135–42. https://doi.org/10.2215/cjn.09600912
Bozbas SS, Bozbas H. Portopulmonary hypertension in liver transplant candidates. World J Gastroenterol 2016; 22: 2024–9. https://doi.org/10.3748/wjg.v22.i6.2024
Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc 2014; 11: 811–22. https://doi.org/10.1513/annalsats.201312-446fr
Author contributions
Ryan McGinn, Stuart A. McCluskey, Blayne A. Sayed, Toru Goto, Christopher T. Chan, and Patricia Murphy contributed to all aspects of this manuscript including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Acknowledgements
The authors would like to acknowledge the operating room nurses, dialysis nurses, and other staff in the operative room and intensive care unit involved who were instrumental in the successful pre-, intra-, and postoperative management of this complex case.
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McGinn, R., McCluskey, S.A., Sayed, B.A. et al. Intraoperative hemodialysis with supra- and infradiaphragmatic catheters for liver transplantation. Can J Anesth/J Can Anesth 71, 1165–1171 (2024). https://doi.org/10.1007/s12630-024-02777-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-024-02777-3