Abstract
Background
The McIvor blade, a tongue retractor with a thin curved blade, is used to improve the operating field during a tonsillectomy. We compared the success rate and incidence of complications between digital insertion and McIvor blade-guided insertion of the laryngeal mask airway (LMA™) ProSeal™ when performed by anesthesia residents in children.
Methods
A total of 134 anesthetized non-paralyzed pediatric patients were included in the study. Patients were allocated randomly to one of two groups, i.e., Digital group (LMA ProSeal insertion using the digital insertion technique) or McIvor group (LMA ProSeal insertion using the Mclvor blade-guided technique). All patients were managed by anesthesia residents who were unskilled in using each technique. We assessed success rates of insertion at the first attempt, insertion time for an effective airway, and postoperative blood staining.
Results
The success rate of insertion at the first attempt was higher in the McIvor group than in the Digital group (97% vs 78%, respectively; P = 0.003), and insertion time with a successful first attempt was shorter in the McIvor group than in the Digital group (20.5 [4.5] sec vs 22.8 [6.7] sec, respectively; P = 0.021). The overall insertion time for an effective airway was also shorter in the McIvor group than in the Digital group (20.9 [5.7] sec vs 26.0 [9.8] sec, respectively; P < 0.001). Blood staining was more frequent in the Digital group than in the McIvor group (23% vs 6%, respectively; P = 0.035).
Conclusion
When inserting the LMA ProSeal in children, anesthesia residents were more successful using the McIvor blade-guided insertion technique than using the digital insertion technique. (ClinicalTrials.gov number, NCT01191619).
Résumé
Contexte
La lame de McIvor, un abaisse-langue muni d’une lame mince et courbe, est utilisée pour améliorer le champ opératoire pendant une amygdalectomie. Nous avons comparé le taux de réussite et l’incidence de complications entre une insertion digitale et une insertion avec lame de McIvor du masque laryngé LMA™ ProSeal™, réalisée chez des enfants par des résidents en anesthésie.
Méthode
Au total, 134 patients pédiatriques non curarisés anesthésiés ont été recrutés pour l’étude. Les patients ont été aléatoirement répartis en deux groupes, soit le groupe digital (insertion du LMA ProSeal à l’aide d’une technique d’insertion digitale) ou le groupe McIvor (insertion du LMA ProSeal à l’aide d’une technique guidée par une lame de McIvor). Tous les patients ont été pris en charge par des résidents en anesthésie qui ne possédaient pas d’expérience avec l’une ou l’autre technique. Nous avons évalué les taux de réussite de l’insertion à la première tentative, le temps d’insertion jusqu’à obtention de voies aériennes perméables, et les taches de sang après l’opération.
Résultats
Le taux de réussite de l’insertion à la première tentative était plus élevé dans le groupe McIvor que dans le groupe digital (97 % vs 78 %, respectivement; P = 0,003), et le temps d’insertion lors d’une première tentative réussie était plus court dans le groupe McIvor que dans le groupe digital (20,5 [4,5] sec vs 22,8 [6,7] sec, respectivement; P = 0,021). Le temps global d’insertion jusqu’à obtention de voies aériennes perméables était également plus court dans le groupe McIvor que dans le groupe digital (20,9 [5,7] sec vs 26,0 [9,8] sec, respectivement; P < 0,001). Les taches de sang étaient plus fréquentes dans le groupe digital que dans le groupe McIvor (23 % vs 6 %, respectivement; P = 0,035).
Conclusion
Lors de l’insertion d’un masque laryngé LMA ProSeal chez des enfants, les résidents en anesthésie ont eu plus de succès en utilisant une technique d’insertion guidée par lame de McIvor qu’avec une technique d’insertion digitale. (Numéro de ClinicalTrials.gov, NCT01191619).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The ProSeal laryngeal mask airway (LMA ProSealTM) (The Laryngeal Mask Company Ltd., Victoria, Seychelles) is an advanced form of the LMA with a softer and larger cuff to improve sealing and a drain tube to permit venting of the stomach.1-4 However, when a larger cuff is used, it is more difficult to save space for inserting the LMA ProSeal in the patient’s mouth, and the larger cuff is more likely to fold over.5,6 In particular, LMA ProSeal insertion in pediatric patients may be impeded by a relatively large tongue, a floppy epiglottis, and the frequent presence of tonsillar hypertrophy.
The McIvor blade (GerMedUSA Inc., NY, USA) is a tongue retractor with a thin curved blade and a flat handle (Fig. 1). It is used to secure the operating field by pressing on the tongue during a tonsillectomy. We hypothesized that retracting the tongue with the McIvor blade would provide more space in the patient’s mouth to insert the LMA ProSeal This technique could improve the success rate of LMA ProSeal insertion as well as reduce the frequency of injuries to the pharyngeal wall in children. Thus, we compared the success rate and incidence of complications between the digital technique and the McIvor blade-guided insertion technique when performed by anesthesia residents in pediatric patients.
Methods
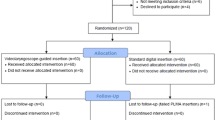
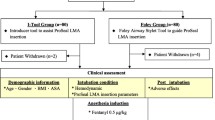
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital, Seongnam, Korea. Written informed parental consent was obtained during the preoperative visit. A total of 136 patients (American Society of Anesthesiologists physical status I-II, aged three to nine years) scheduled for minor surgery under general anesthesia were enrolled.
Patients were excluded if they had a known or predicted difficult airway, loose teeth, recent sore throat, mouth opening <2.5 cm, or if they were at risk of aspiration. An investigator with no clinical involvement in our study allocated the patients randomly to one of the two groups using block randomization (block size 6). A second investigator, also with no clinical involvement in the present study, assigned the groups, i.e., Digital group (LMA ProSeal insertion using the digital insertion technique) or McIvor group (LMA ProSeal insertion using the Mclvor blade-guided technique - size #3 from Mclvor mouth gag sets) by opening an opaque sealed envelope.
In the operating room, thiopental 5 mg·kg−1 was administered intravenously and a standard anesthesia protocol was followed. Routine monitoring was applied, including the electrocardiogram, pulse oximetry, gas analyzer, noninvasive blood pressure monitor, tidal volume monitor, and airway pressure monitor. Manual mask ventilation was performed using 2-8 vol% sevoflurane in 50% oxygen and 50% nitrous oxide and was continued for at least 30 sec until conditions were suitable for LMA ProSeal insertion (apnea and lack of response to jaw thrust). The LMA ProSeal sizes 2, 2.5, or 3 were used in children weighing 10-20 kg, 20-30 kg, or >30 kg, respectively. All patients were managed by anesthesia residents who were unskilled with the digital insertion technique (i.e., <15 LMA ProSeal or LMA uses). After a ten-minute explanation for each insertion technique (digital and McIvor blade) according to the instruction manual (LMA™ airway instruction manual, The Laryngeal Mask Company Ltd, 2005), junior residents in the anesthesiology department (postgraduate year 1) performed LMA ProSeal insertion with each technique under the supervision of the attending physicians. Each resident performed an equal number of insertions with each technique (less than five insertions for each technique).
The digital insertion technique (Digital group) was performed according to the manufacturer’s instructions. The posterior aspect of the deflated mask was coated with a water-based lubricant. The LMA ProSeal cuff was fully deflated, held like a pen, and inserted while pressing along the palatopharyngeal curve using the index finger. The LMA ProSeal was advanced into the hypopharynx until definite resistance was felt. The McIvor blade-guided technique (McIvor group) involved the following steps. The LMA ProSeal was lubricated on the posterior aspect of the deflated mask with a water-based lubricant. With the patient’s head extended, the McIvor blade was fully inserted under the patient’s tongue. The tongue was lifted gently with the McIvor blade and the LMA ProSeal was introduced into a space between the McIvor blade and the maxillary incisors while an operator was holding the bite block of the LMA ProSeal (Fig. 2). The LMA ProSeal was advanced into the hypopharynx until definite resistance was felt, and then the McIvor blade was removed. All techniques were performed in the sniffing position using a midline or slight lateral approach with the cuff fully deflated.
McIvor blade-guided insertion of the ProSeal laryngeal mask airway (LMA ProSeal). With the patient’s head extended, the McIvor blade is fully inserted beneath the patient’s tongue - (a) and (b). The LMA ProSeal is introduced into a space between the McIvor blade and maxillary incisors while an operator holds the bite block of the LMA ProSeal - (c) and (d). Informed consent for the photographs was obtained from the patient’s parent
For both techniques, once the LMA ProSeal was inserted into the hypopharynx, the cuff was inflated with air until effective ventilation was established or until the maximum recommended inflation volume was reached. An effective airway was judged by a square-wave capnograph trace and no audible leak with peak airway pressure at ≤ 12 cmH2O during manual ventilation. Oropharyngeal leaks were detected by listening over the patient’s mouth. The following airway maneuvers were allowed: chin lift, jaw thrust, head extension, or flexion of the neck. Fixation was according to the manufacturer’s instructions. The number of insertion attempts was also recorded. If the placement failed after two attempts, the insertion was recorded as a failure and the attending anesthesiologist performed the LMA ProSeal insertion or tracheal intubation. Insertion time was defined as the time from picking up the McIvor blade (McIvor group) or the LMA ProSeal (Digital group) to confirming successful placement after inflation of the cuff (the appearance of the end-tidal CO2 trace on the monitor screen). Times for all individual attempts were added to calculate the insertion time, and data from patients with failed LMA ProSeal insertion after two attempts were excluded from calculation. The ease of insertion was assessed by the success rate at the first attempt. All episodes of hypoxia (SpO2 < 90%), airway reflex activation (coughing, gagging, and/or laryngospasm), or vomiting during LMA ProSeal insertion were documented. Data were recorded on standardized data sheets by observers who were unblinded to the insertion technique. At the end of surgery, the LMA ProSeal was removed when protective upper airway reflexes returned. Anesthesiologists or nurses blinded to the method of insertion recorded the presence or absence of blood on the laryngeal masks.
Statistical analysis
The primary aim of the present study was to compare the success rate of first attempts at insertion. Secondary outcomes included insertion time and postoperative complications.
Sample size calculation was performed using Power Analysis and Sample Size (PASS) software (2005, NCSS, USA). The computation was based on a published study in which inexperienced personnel achieved an 83% success rate for first attempt LMA ProSeal insertion in adults using the digital technique2 and on accepting that an incremental improvement in success rate was 16% in absolute terms. Sixty-one patients were required in each group for a significance level of 95% with a power of 80%. Therefore, 68 patients per group were enrolled to compensate for possible dropouts. The SPSS software version 12.0 (SPSS Inc, Chicago, IL, USA) was used for statistical analysis; the Student’s t test was used to analyze insertion times, and Chi square analysis was used to compare the number of insertion attempts (success rates), the presence of blood on the LMA ProSeal, and the occurrence of complications. A P value of<0.05 was considered statistically significant.
Results
One hundred and forty patients were assessed for eligibility from July to December 2010; the parents of four patients declined to participate, and 136 patients were subsequently enrolled in this study. Tracheal intubation was performed for two patients due to excessive oral secretions, and 134 patients completed the study. Demographic data are summarized in Table 1. The two groups were comparable in terms of age, weight, height, sex, and size of LMA ProSeal. Fourteen anesthesia residents (postgraduate year 1) performed the LMA ProSeal insertions.
Comparison data for the digital insertion and McIvor blade-guided techniques are presented in Table 2. The success rate of insertion at the first attempt was higher with the McIvor-guided technique than with the digital insertion technique (97% vs 78%, respectively; P = 0.003). Insertion time at the first attempt and the overall insertion time for an effective airway were shorter in the McIvor group than in the Digital group (Table 2). Blood staining was more frequent in the Digital group than in the McIvor group (P = 0.035). During LMA ProSeal insertion, no significant differences in hemodynamic responses were observed between the techniques, and there were no episodes of hypoxia, airway reflex activation, or vomiting.
Discussion
When anesthesia residents performed LMA ProSeal insertion in pediatric patients using the McIvor blade-guided technique, they achieved greater success at the first attempt and there was a lower incidence of postoperative blood staining than when they performed the LMA ProSeal insertion using the digital technique.
The main cause of difficult and failed insertions with the digital technique is impaction of the LMA ProSeal at the back of the mouth and glottic inlet.7,8 In particular, the differences in airway anatomy and the frequent presence of tonsillar hypertrophy can complicate LMA ProSeal insertion in pediatric patients. The manufacturer recommends inserting the LMA ProSeal with digital manipulation or with an introducer; however, insertion with these techniques is sometimes difficult even for experienced personnel. An 83% success rate has been reported for LMA ProSeal insertion by inexperienced personnel on their first attempt.2
Several techniques have been introduced to improve the insertion success rate; the use of fibroscopy,9 an Eschmann® Tracheal Tube Introducer (i.e., gum-elastic bougie),4,10 and a suction catheter.11 However, these techniques do not leave enough oral space for LMA ProSeal insertion; leaving a larger space between the tongue and retropharynx and not requiring the introduction of an index finger would make insertion in children easier.
A major advantage of the McIvor blade-guided technique is provision of sufficient oral space by displacing the tongue; it guides the distal cuff of the LMA ProSeal directly into the hypopharynx without oropharyngeal impaction, and it prevents the cuff from folding over, which can reduce mucosal injury. In addition, there is no need for the operator to place the index finger into the patient’s oral space to provide more room for insertion. A potential disadvantage of the McIvor blade-guided technique is the difficulty of use in patients with a limited mouth opening as it would reduce rather than increase the oral space for LMA ProSeal insertion.
In previous studies of LMA ProSeal insertion in children, experienced personnel have achieved success rates ranging from 84-94% on their first attempt.4,12,13 In the present study, inexperienced personnel achieved a 78% success rate on their first attempt using the digital technique. Considering inexperienced personnel achieved an 83% first-attempt success rate at LMA ProSeal insertion in adults using the same technique,2 our results show that LMA ProSeal insertion in children is also challenging for inexperienced personnel. In contrast to adults, the main cause of cardiac arrest in children is progressive respiratory failure. When respiratory failure occurs, adequate intervention to prevent further deterioration would improve outcomes.14 In the present study, the Digital group’s slightly longer insertion times at first attempt and overall attempt might be considered as clinically insignificant.4 However, this result should not be ignored because the overall attempt time did not account for the failure cases (9% in the digital technique). Accordingly, we suggest that unskilled personnel use the McIvor blade-guided technique to facilitate successful airway management in children.
The use of a laryngoscope for LMA ProSeal insertion has been suggested as an alternative technique when the digital insertion technique has failed.15,16 However, it remains unclear whether laryngoscope-guided insertion can improve the success rate of LMA ProSeal insertion.17 The blade of the laryngoscope is much thicker than the McIvor blade. In addition, the laryngoscopic blade allows only the right half of the oral space for insertion due to displacement of the tongue to the left side of the blade. Thus, it might be less effective than the McIvor blade in preserving oral space.
This study has several limitations. First, our operators were unblinded, and they may have been biased toward a given technique of LMA ProSeal insertion. However, the operators were unaware of both the purpose of this study and the outcome variables. Furthermore, they were instructed not to deviate from the study protocol. These two factors should have offset any potential bias arising from the lack of operator and observer blinding. Second, data (except for the presence of blood staining) were collected by unblinded observers, a possible factor of bias, although the study was performed following a detailed protocol, and observers’ biases should have had little effect on the results. Third, all insertions were performed by junior anesthesia residents (postgraduate year 1) who were unskilled in the digital technique (<15 LMA ProSeal or LMA uses). On the other hand, none of the anesthesia residents had experience with the McIvor blade-guided technique. Nevertheless, they achieved a higher success rate of insertion at the first attempt (as the primary outcome) using the McIvor blade-guided technique. In our view, this result supports the superiority of the McIvor blade-guided technique over the digital technique when performed by unskilled personnel in children. However, the efficacy of experienced personnel performing the McIvor blade-guided insertion technique is unclear, and further evaluations are required. Fourth, we did not evaluate the position of the LMA ProSeal directly using a fibreoptic bronchoscope; correct placement was confirmed by clinical assessment.
In conclusion, when anesthesia residents performed LMA ProSeal insertion in children using the McIvor blade-guided insertion technique, the success rate at first attempt and the reduction of oropharyngeal mucosal injury proved superior to the digital insertion technique for airway management.
References
Brain AI, Verghese C, Strube PJ. The LMA ‘ProSeal’—a laryngeal mask with an oesophageal vent. Br J Anaesth 2000; 84: 650-4.
Coulson A, Brimacombe J, Keller C, et al. A comparison of the ProSeal and classic laryngeal mask airways for airway management by inexperienced personnel after manikin-only training. Anaesth Intensive Care 2003; 31: 286-9.
Hohlrieder M, Brimacombe J, von Goedecke A, Keller C. Guided insertion of the ProSeal laryngeal mask airway is superior to conventional tracheal intubation by first-month anesthesia residents after brief manikin-only training. Anesth Analg 2006; 103: 458-62.
Lopez-Gil M, Brimacombe J, Barragan L, Keller C. Bougie-guided insertion of the ProSeal laryngeal mask airway has higher first attempt success rate than the digital technique in children. Br J Anaesth 2006; 96: 238-41.
Cook TM, Silsby J, Simpson TP. Airway rescue in acute upper airway obstruction using a ProSeal laryngeal mask airway and an Aintree catheter: a review of the ProSeal laryngeal mask airway in the management of the difficult airway. Anaesthesia 2005; 60: 1129-36.
Hwang JW, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Comparison of two insertion techniques of ProSeal laryngeal mask airway: standard versus 90-degree rotation. Anesthesiology 2009; 110: 905-7.
Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology 2000; 93: 104-9.
Evans NR, Gardner SV, James MF, et al. The proseal laryngeal mask: results of a descriptive trial with experience of 300 cases. Br J Anaesth 2002; 88: 534-9.
Brimacombe J, Keller C. Awake fibreoptic-guided insertion of the ProSeal laryngeal mask airway. Anaesthesia 2002; 57: 719.
Brimacombe J, Keller C. Gum elastic bougie-guided insertion of the ProSeal Laryngeal Mask Airway. Anaesth Intensive Care 2004; 32: 681-4.
Garcia-Aguado R, Vinoles J, Brimacombe J, Vivo M, Lopez-Estudillo R, Ayala G. Suction catheter guided insertion of the ProSeal laryngeal mask airway is superior to the digital technique. Can J Anesth 2006; 53: 398-403.
Lopez-Gil M, Brimacombe J. The ProSeal laryngeal mask airway in children. Pediatr Anesth 2005; 15: 229-34.
Wheeler M. ProSeal laryngeal mask airway in 120 pediatric surgical patients: a prospective evaluation of characteristics and performance. Pediatr Anesth 2006; 16: 297-301.
Young KD, Seidel JS. Pediatric cardiopulmonary resuscitation: a collective review. Ann Emerg Med 1999; 33: 195-205.
Goudsouzian NG, Denman W, Cleveland R, Shorten G. Radiologic localization of the laryngeal mask airway in children. Anesthesiology 1992; 77: 1085-9.
Elwood T, Cox RG. Laryngeal mask insertion with a laryngoscope in paediatric patients. Can J Anaesth 1996; 43: 435-7.
Koay CK, Yoong CS, Kok P. A randomized trial comparing two laryngeal mask airway insertion techniques. Anaesth Intensive Care 2001; 29: 613-5.
Declaration of interest
The authors report no conflict of interest. We have no financial or other relationship that might lead to a conflict of interest regarding this work. We alone are responsible for the content and writing of this paper.
This study was not supported by any funding sources.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hwang, J., Han, S., Hwang, J. et al. The McIvor blade improves insertion of the LMA ProSeal™ in children. Can J Anesth/J Can Anesth 58, 796–801 (2011). https://doi.org/10.1007/s12630-011-9540-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9540-4