Abstract
Purpose of Review
The radiologist’s role is integral in the diagnosis and preoperative management of breast cancer patients. The pre-surgical localization of non-palpable breast masses has been achieved using wire-guided devices for decades. Despite being widely regarded as the gold standard for their proven effectiveness and cost-effectiveness, wire-guided localization (WGL) techniques have been associated with several drawbacks. These drawbacks include patient discomfort, the possibility of displacement prior to resection, and the requirement for placement on the same day as surgery. This review aims to outline non-wire localization (NWL) devices and techniques available as alternatives to WGL, including their benefits and limitations.
Recent Findings
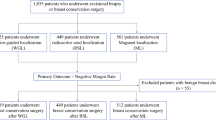
No significant differences have been found with surgical outcomes between WGL and NWL. Between 2013 and 2018, the use of WGL has decreased from 75 to 32%, and the use of radioactive seed localization has increased from 16 to 61%.
Summary
A multidisciplinary approach that considers the patient, provider, and healthcare institution and current research on surgical outcomes must be utilized to determine the optimal course of action for preoperative localization of non-palpable breast masses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With improvements in breast cancer screening education and technology over the past few decades, mammography has yielded a higher incidence of nonpalpable breast mass identification, warranting surgical removal because of the associated cancer risk [1, 2]. Wire-guided identification of nonpalpable breast masses has been the mainstay of preoperative localization since the 1970s, proving to be low cost and efficacious [3••]. To localize the finding on the day of surgery, a needle of varying gauges preloaded with a wire is inserted percutaneously under image guidance. Having the capability to reposition the wire after its positioning is an advantage of this established procedure. Aside from its documented benefits, WGL holds many limitations that have warranted further research into non-wire approaches. These limitations include patient distress and anxiety, the possibility of wire dislodgement prior to and after surgery, the risk of transection and kinking during surgery, and the requirement for wire implantation on the same day as surgery, which complicates scheduling across multiple departments [3••]. Additionally, WGL predetermines the surgical site, even if a more optimal location is discovered by the surgeon prior to the procedure.
Non-wire localization technologies and techniques have emerged as alternatives, and we seek to review the overall benefits and limitations of non-wire technology and the specifics of each. Non-wire localization (NWL) devices include radioactive seed localization (RSL), intraoperative ultrasound (IOUS), radar reflector localization (RRL), magnetic seed localization (MSL), and radiofrequency identification (RFID). The benefits for all non-wire devices overlay the aforementioned limitations of WGL.
There are general limitations to all NWL devices when compared to WGL that must be considered when planning a pre-surgical/surgical course of action for each patient. Unlike the relatively low cost of WGL, NWL comes with varying increased costs, both from a patient and institutional standpoint. Start-up, operating, and device costs must all be weighed. Another critical limitation of NWL is the inability to reposition the devices after deployment [3••]. Repositioning is feasible despite the potential for dislodgement with WGL, but this is not the case with NWL. There is also strict oversight and regulatory cautions in place for some of the NWL devices [3••]. Further research, usage, and training can potentially mitigate these challenges.
Radioactive Seed Localization (RSL)
Localizer Information
Radioactive seed localization (RSL) has been implemented since 2001 to identify nonpalpable breast lesions and localize axillary lymph nodes [3••]. Advancements in technology have led to breast cancers being detected earlier when masses are of smaller size which can make conservative removal of all cancerous tissue more difficult. RSLs allow radiologists to insert radioactive seeds into the center of abnormal tissue to aid surgeons in the conservative removal of the finding. The I-125 radioactive material is encased within a 4.5 × 0.8-mm titanium seed, approximately the size of a sesame seed. Radioactive material dosages range from 3.7–11.1 MBq [3••]. Before implantation, the seed is preloaded into a sterile 18-gauge needle with bone wax at the needle tip to ensure proper placement and limit seed migration [3••]. The needle is available in lengths from 5–15 cm. The seed is inserted into the lesion using mammographic, ultrasound, stereotactic, or tomosynthesis guidance but not MRI. Removal of the seeds is usually done within five days after placement, but radioactive seeds can be left for up to 60 days, depending on the institution and Nuclear Regulatory Commission (NRC) license agreement [3••]. The half-life of I-125 is 59.4 days, and it exhibits a gamma photon emission peak at 27 keV [3••]. Geiger-Muller (GM) survey meters are used preoperatively, intraoperatively, and post-operatively to check radioactive activity and seed presence [4]. In the instance where a patient will need a sentinel lymph node biopsy, seed placement must be done first as GM meters cannot differentiate between radioactive I-125 and the technetium-99 used for lymph node biopsy.
Benefits and Limitations
RSLs has several benefits when compared to WGL and other non-wire localization techniques. Unlike WGL, which must be inserted the day of procedure, RSL can be inserted for up to 60 days before removal which has led to better workflow efficiency regarding scheduling. RSL reduces the patient’s discomfort and anxiety that come with a protruding wire that has the potential to become displaced. This procedure allows for better radiology biopsy slot utilization, decreased time scheduling, and reduced radiology and surgery rescheduling leading to higher patient satisfaction [3••]. Several studies have shown that patients preferred RSL over WGL [3••, 5, 6]. Positive excision margins and re-excision for RSL range from 5–32%, similar to WGL [3••].
Compared to other non-wire techniques, RSL is the cheapest option, with costs ranging from $20 to $50 [3••]. Most hospitals already have intraoperative gamma probes, which are used for technetium-99 lymph node localization, further reducing initial start-up costs. In a study that assessed signal propagation and maximum detection distance in water and tissue environments, researchers found that RSL signal was detectable up to 60 mm, giving it the greatest depth detection compared to MSL and RRL [7]. Device migration for RSL is rare, ranging from 0.1–2%, and is most often related to post-biopsy hematoma or placement technique [3••].
The primary barrier to RSL implementation is adherence to NRC guidelines. In 2016, the United States NRC revised its guidelines, which now include authorized user training and experience requirements, the need to work under the supervision of an authorized user, appropriate use of radiation surveys and instrumentation, and understanding of the criteria of a medical event [3••]. Medical event criteria include using the wrong nucleotide, implantation of the wrong number of seeds, and implantation of a radioactive seed in the wrong patient [3••]. Radiologists, surgeons, and pathologists all must undergo proper handling technique training, and institutions must have emergency protocols in place in the case of seed breakage, leakage, or loss [3••]. While some studies have shown improved patient satisfaction, there has also been evidence of patient anxiety due to potential radiation exposure [8••].
Radar Reflector Localization (RRL)
Localizer Information
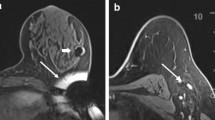
Radar reflector localization (RRL) is a type of zero-radiation breast mass localization technology that is preoperatively inserted via image guidance and located intraoperatively using electromagnetic wave signals [9•]. The reflector itself has two antennas on either side of it and is activated using infrared light impulses from the probe that then relay signals back to the handpiece. With the absence of radiation, RRL has been approved by the FDA for long-term implantation. It is currently approved for nonpalpable breast masses as deep as 6 cm and its double ended antenna system acts as an anchor for the device. The radar reflector is inserted into the lesion using mammographic, ultrasound, stereotactic, tomosynthesis, or MRI guidance.
SAVI SCOUT system is a specific type of RRL that is most widely used in this realm. A 2021 study demonstrated intraoperative localization and retrieval rates of 98.6% and 100% respectively with a 0% incidence of device migration [10]. Although, some studies have shown device migration in 4.5–7.0% of cases, most commonly from hematoma development [3••]. The positive margin rates associated with RRL have ranged from 0 to 16%. Therefore, it is important to approach the research studies with care and consider the study methodology and sample size of the studies. In one study, 7% of patients had positive margins, and 75% of those individuals' results were attributed to the underestimated tumor size during preoperative imaging [10].
Benefits and Limitations
One of the most significant benefits to the radio reflector technology is its real-time electromagnetic feedback, allowing the surgeon to make approach adjustments and decrease the removal of healthy tissue. In one study, 93.7% of radiologists and 98.6% of surgeons rated the SAVI SCOUT RRL system better than WGL with a corresponding patient satisfaction score of 9.7/10 [10]. Concerning to operating times, surgeons have reported no difference when compared to WGL. A distinct advantage of RRL when compared to other NWL devices is that little to no artifact is produced when imaged in a 1.5-3 T magnetic field [3••]. Radiologist, surgeon, and patient satisfaction rates have been reported as high but necessitate more studies for reproducibility.
The limitations of RRL systems revolve around its costs and intraoperative detection difficulties. The initial start-up costs for a healthcare institution are in the tens of thousands and the cost of each implantable device is $450 [3••]. The most significant amount of surgical probe interference was recorded for RRL when compared to RSL and MSL as well as significant deactivation of the reflector when contacting electrocautery or older halogen operating lights [7, 10]. Other reported sources of signal detection difficulties are associated with calcified fibroadenomas and hematomas [10, 11].
Magnetic Seed Localization (MSL)
Localizer Information
Magnetic seed localization (MSL) is a magnetic device used for the localization of nonpalpable breast masses and axillary lymph nodes. Magseed is a type of MSL that is the most well-studied in this domain. It was approved by the FDA in 2016 and is composed of surgical grade stainless steel and is about the size of a grain of rice (5 × 0.9 mm) [3••, 8••]. It is deployed through an 18-gauge needle and stabilized by a bone wax plug [3••]. The seed is inserted into the lesion using mammographic, ultrasound, stereotactic, or tomosynthesis guidance but not MRI [8••]. MSL also decouples seed placement and surgery, allowing for flexibility in surgery scheduling [3••, 8••]. Magnetic seeds have been approved for long term placement [12]. Intraoperatively, the surgeon uses a detector probe to locate the lesion using audio and numerical feedback [1]. Detector probes can sense up to a 4 cm depth of breast tissue, although compression and palpation by the surgeon have achieved greater distances [3••].
Benefits and Limitations
Compared to WGL and other NWL devices, the initial benefits are MSL's wire-free and radiation-free nature. Intraoperatively audible and numerical feedback has allowed surgeons to orient the target lesion better and decrease the amount of healthy tissue removed [3••]. Positive margins requiring re-excision ranged from 9–22%, with no statistically significant difference in re-excision rates when directly compared to WGL [3••]. Device migration has occurred in approximately 0–4.5% of cases [3••]. Approval of long-term use of Magseed is crucial for breast tumor or axillary lymph node localization after neoadjuvant therapy, which lasts 3–4 months [13]. Several studies have shown a technical placement success rate between 96–100% [14]. A study found that MSL devices could accurately be positioned by radiologists with a mean placement time of 4 min [14]. Radiologists and surgeons report seed placement and localization as being very easy [3••, 14]. Decreased patient anxiety with this method has been reported secondary to less discomfort and it being nonradioactive [3••]. Given the small size of the deployment needle when compared with other localization techniques and short procedure time, MSL is generally less invasive and well tolerated by patients [14].
Drawbacks to MSL include depth of marker implantation, cost, frequent probe recalibration, and magnetic resonance imaging (MRI) incompatibility. According to the manufacturer’s recommendation, depth of marker implantation is limited to 30 mm. Due to the probe's interference with paramagnetic surgical instruments and electrocautery, the probe must be frequently recalibrated leading to increased operation times [13]. To prevent interference, non-ferromagnetic surgical instruments can be used, but this could lead to added initial costs [3••, 14]. Compatibility with MRI is another important factor. Magseed is MRI-compatible but has a bloom artifact up to 4–6 cm rendering restaging imaging after neoadjuvant therapy inaccurate [13, 15]. MRI artifacts also limit the use of MSL for lesions that are only visible on MR [7]. The cost of the system is one of the main drawbacks, with the price of each probe and seed costing approximately $450, making it one of the most expensive devices on the market [3••, 13, 15]. Other considerations with MSL include nickel allergies and the presence of implantable devices such as a pacemaker. Manufacturer guidelines state that Magseed contains 10–15 times less nickel than normal medical stainless steel. Guidelines also state that the probe must not be placed within 15 mm of an operating pacemaker [16].
Sirius Pintuition
Localizer Information
Sirius Pintuition is a type of MSL that was CE marked in 2020 and approved by the FDA in 2021. The localizer measuring 5 × 1.6 mm is composed of biocompatible nickel-free titanium encasing, delivered in a preloaded and sterile 14G needle [9•, 17]. Pintuition is approved for long-term placement in the United States and up to 180 days in Europe in any soft tissue, allowing for use in both breast and axilla [9•, 17]. Intraoperatively, the surgeon uses a multi-sensor detector probe to locate the lesion using audio, numerical and directional feedback [9•]. The Pintuition probe is able to sense up to a 5 cm depth of breast tissue [9•, 17].
Benefits and Limitations
A few publications have shown a retrieval rate of the Pintuition localizer close to 100% [9•, 17, 18] as well as no migration [19]. Radiologists and surgeons report seed placement and localization as being very easy, more intuitive and less complex than WGL [18, 19]. Sirius Pintuition can be used with the traditional metallic surgical tools [9•, 19] unlike Magseeds. The Pintuition software provides spatial, directional guidance and the true distance in millimeters from the tip of the probe to the localizer and the calibration of the probe is only needed once per procedure.
Drawbacks to Pintuition include magnetic resonance imaging (MRI) artifact. Pintuition is labeled MRI-conditional up to 3 T but has a bloom artifact up to 5–6 cm rendering restaging imaging after neoadjuvant therapy inaccurate whenever the MRI modality is needed [9•]. Guidelines also state that the seed must not be placed within 5 cm of an operating pacemaker [17].
Radiofrequency Identification (RFID)
Localizer Information
Radiofrequency identification (RFID) was FDA approved in 2017 for localization of breast lesions using radio wave signals [3••]. The 11 × 2 mm RFID tag is composed of a ferrite rod wrapped in copper and a microprocessor enclosed in a glass casing within an anti-migratory polypropylene sheath [3••]. Tags are inserted via a 12-gauge needle applicator, which can be advanced to the center of the target lesion [3••]. The tag is inserted into the lesion using mammographic, ultrasound, stereotactic, or tomosynthesis guidance, but not MRI. The applicator comes in various lengths of 5, 6, or 10 cm. The RFID tag is used after percutaneous placement as well as during surgical excision for localization and has been found to have no interference from other equipment in the operating room [20]. A pencil-sized, single-use, sterile surgical reader is used intraoperatively to help the surgeon localize the tag and can detect the tag within a 40–60 mm distance [3••, 20]. The reader uses an audible sound which increases in volume as the device gets close to the tag. The reader also has a visual indicator that shows the tag’s distance from the detector. The visual display shows the tag’s unique identification number, which can be helpful if more than one tag is implanted into the same breast [3••].
Benefits and Limitations
RFID has relatively high satisfaction ratings among both patients and physicians. One study reported surgeon preference for RFID, citing the probe is lighter, easier to use, has more precise navigation, and more accurate estimation of distance to the tag [3••]. Positive excision rates range from 0–27%, similar to WGL and other non-wire techniques [3••]. Furthermore, the small caliber surgical probe (8-mm) can be used in small incisions without obscuring visualization of the target [3••]. While the insertion needle is larger gauge and could potentially lead to device displacement, data has shown negligible migration rates of 0–0.6% [3••].
Given the device’s larger size compared to other markers, placement difficulty has been reported, especially within dense breast tissue leading to placement of the tag at the edge of the lesion instead of the center [3••, 7]. McGugin et al., found that the unique identification number on tags placed closer than 1.8 cm were unable to be individually identified due to interference and wires were preferable to tags for short-distance bracketed procedures [3••]. RFID is the most expensive device, with each device costing $550, compared to WGL and other non-wire localization techniques [3••]. RFID has also been reported to cause artifact with MR imaging, posing similar challenges seen with MSL.
Intraoperative Ultrasound (IOUS)
Localizer Information
An alternative method to the pre-surgical localization of breast masses is the use of intraoperative ultrasound (IOUS). Multiple studies have documented it as an accurate and effective method for localization during the procedure [1]. A multi-frequency probe operating in the 7–18 MHz range is utilized by the radiologist or surgeon intraoperatively to locate the mass. Small probes are able to be used as well within the incision site for more accurate identification and clearer image. Compared to WGL and the forms of NWL described above, IOUS was shown to have significantly higher negative margin rates and decreased re-excision rates [20, 21].
Benefits and Limitations
The major benefit to IOUS is, of course, eliminating the need for a pre-operative localization procedure in the radiology department. IOUS further reduces the scheduling burden on the patient and allows a direct route to removal by the surgeon. In addition to the ability to visualize the mass in real time, allowing for approach adjustments, the surgeon is able to view the area post-procedure which can help ensure complete excision. Other benefits include its relatively low cost, lack of radiation used, non-invasive nature, and negative margin success as mentioned above.
One drawback to IOUS includes the presence of ultrasound machines in operating suites suitable for the procedure; some machines do not have the correct frequency or transducer type, so this is dependent on what is present in the institution. Finally, not all breast lesions can be visualized under ultrasound guidance. In this case ultrasound occult lesions, mammography, MRI, or other imaging techniques may be the only option for visualization. Furthermore, IOUS is classified as an intraoperative technique and is not adequately compared to the NWL devices used in the pre-operative setting discussed within this paper.
Conclusion
The present review delineated specific differentiations among NWL and the following broader topics that necessitate restatement. All NWL are of higher cost than WGL, RSL us the cheapest NWL option and RFID the most expensive. RSL has widely become adopted but is the only device containing radiation and thus comes with additional oversight and institutional requirements. IOUS presents with high negative margins and good surgical outcomes but necessitates a high degree of training for surgeons and eliminates performing the procedure in the radiology department.
The decrease in use of WGL for nonpalpable breast masses in the pre-operative setting with a correlated increase in use of certain NWL over the last decade indicates an interest in alternative methods to wire guidance. Our review of the current literature found no significant difference in surgical outcomes between WGL and NWL.
Multiple factors are at play for deciding the best pre-surgical course. The optimization of treatment plans necessitates the adoption of a multidisciplinary strategy that takes into account the unique circumstances of each team, which includes the patient, providers, and institution.
Data Availability
The data supporting the information presented in this paper are, as confirmed by the authors, contained within the paper.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bick U, Trimboli RM, Athanasiou A, Balleyguier C, Baltzer PA, Bernathova M, Borbely K, Brkljacic B, Carbonaro LA, Clause P, Cassano E, Colin C, Esen G, Evans A, Fellenberg EM, Fuchsjaeger MH, Gilbert FJ, Helbich TH, Heywang-Kobrunner SH, et al. Image-guided breast biopsy and localization: recommendations for information to women and referring physicians by the European Society of Breast Imaging. Insights Imaging. 2020;11(1):12. https://doi.org/10.1186/s13244-019-0803-x.
Wen H, Xu T, Huang Q, Zhang C, Zhang Q, Chen H. Nonpalpable breast masses. Medicine (Baltimore). 2020;99(50):e23556. https://doi.org/10.1097/MD.0000000000023556.
•• Davis KM, Raybon CP, Monga N, Waheed U, Michaels A, Henry C, Spalluto LB. Image-guided localization techniques for nonpalpable breast lesions: an opportunity for multidisciplinary patient-centered care. J Breast Imaging. 2021;3(5):e542-555. https://doi.org/10.1093/jbi/wbab061. This article provided ample information on individual localizer devices, outlining multiple alternatives to wire localization.
Ferreira HH, Souza CD, Rostelato ME. Radioactive seed localization for conservative surgery of nonpalpable breast cancer: recommendations for technology implantation program. Int J Surg Protoc. 2022;26(1):94–106. https://doi.org/10.29337/ijsp.182.
Gray RJ, Salud C, Nguyen K, Duaway E, Friedland J, Berman C, Peltz E, Whitehead G, Cox CE. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol. 2021;8(9):711–5. https://doi.org/10.1245/aso.2001.8.9.711.
Hughes JH, Mason MC, Gray RJ, McLaughlin SA, Degnim AC, Fulmer JT, Pockaj BA, Karstaedt PJ, Roarke MC. A multi-site validation trial of radioactive seed localization as an alternative to wire localization. Breast J. 2008;14(2):153–7. https://doi.org/10.1111/j.1524-4741.2007.00546.x.
Gabrielova L, Selingerova I, Zatecky J, Ondrej Z, Burkon P, Holanek M, Coufal O. Comparison of 3 different systems for non-wire localization of lesions in breast cancer surgery. Clin Breast Cancer. 2023;23(6):e323-330. https://doi.org/10.1016/j.clbc.2023.05.006.
•• Shirzai S, Hajismaeili H, Khosla M, Taj S, Sircar T, Vidya R. Comparison of wire and non-wire localization techniques in breast cancer surgery: a review of the literature with pooled analysis. Medicina. 2023;59:1297. https://doi.org/10.3390/medicina59071297. This 2023 article reviews the literature comparing wire to non-wire localization techniques in breast cancer surgery. This recent writing is of great importance with analyzing the effectiveness of both strategies from an up-to-date perspective.
• Banys-Paluchowski M, Kuhn T, Masannat Y, Rubio I, Boniface J, Ditsch N, Cakmak GK, Karakatasanis A, Dave R, Hahn M, Potter S, Kothar A, Gentilini OD, Gulluoglu BM, Lux MP, Smidt M, Weber WP, Sezen BA, Krawczyk N, Harvey J. Localization techniques for non-palpable breast lesions: current status, knowledge gaps, and rationale for the MELODY study (EUBREAST-4/iBRA-NET, NCT 05559411). Cancers (Basel). 2023;15(4):1173. https://doi.org/10.3390/cancers15041173.This 2023 article discusses updated results from the MELODY study; a multinational study in which breast cancer patients undergoing surgery utilizing image guidance are enrolled. The study examines multiple strategies/technologies and results are analyzed at the patient, surgeon, and radiologist perspective and preference.
Wazir U, Kasem I, Michell MJ, Suaris T, Evans D, Malhotra A, Mokbel K. Reflector-guided localization of non-palpable breast lesions: a prospective evaluation of the SAVI SCOUT System. Cancers (Basel). 2021;13(10):2409. https://doi.org/10.3390/cancers13102409.
Kappor MM, Patel MM, Scoggins ME. The wire and beyond: recent advances in breast imaging preoperative needle localization. RadioGraphic. 2019;39(7):1886–906. https://doi.org/10.1148/rg.2019190041.
Singh P, Scoggins ME, Sahin AA, Hwang RF, Kuerer HM, Caudle AS, Mittendorf EA, Thompson AM, Bedrosian I, Teshome M, DeSnyder SM, Meric-Bernstam F, Hunt KK. Effectiveness and safety of magseed-localization for excision of breast lesions: A prospective, phase IV trial. Annal Surg. 2020;1(2):e008. https://doi.org/10.1097/as9.0000000000000008.
Zatecky J, Kubala O, Jelinek P, Lurch M, Ihnat P, Peteja M, Brat R. Magnetic marker localization in breast cancer surgery. Arch Med Sci. 2020;19(1):122–7. https://doi.org/10.5114/aoms.2020.93673.
Depretto C, Pepa GD, Berardinis C, Suman L, Ferranti C, Marchesini M, Maugeri I, Martelli G, Gennaro M, Folli S, Pruneri G, Scaperrotta GP. Magnetic localization of breast lesions: a large-scale European evaluation in a national cancer institute. Clin Breast Cancer. 2023;23(8):e491-498. https://doi.org/10.1016/j.clbc.2023.08.004.
Zatecky J, Kubala O, Coufal O, Kepicova M, Faridova A, Raus K, Lurch M, Peteja M, Brat R. Magnetic seed (Magseed) localization in breast cancer surgery: a multicenter clinical trial. Breast Care (Basel). 2020;16(4):383–8. https://doi.org/10.1159/000510380.
EMEA: Sysmex Europe GmbH. Sentimag– Magseed [Infographic]. Retrieved March 1, 2024, from https://www.sysmex-europe.com/fileadmin/media/f100/Business_Lines/Oncology/SEG_Sentimag_Magseed_lymph_node_patient_information_BREAST_EN.pdf.
Sirius Medical website. Retrieved March 28, 2024, from https://ifu.sirius-medical.com/smed/GB/srp?keycode=SPS12.
Bessems M, et al. Safety and performance of Sirius Pintuition – a novel wire-free and non-radioactive localization system for breast cancer surgery. Eur J Surg Oncol. 2021;47(2):e1.
Stengs L, Van Veen S, Moormann G. A novel surgical marker navigation system to localise and remove non-palpable breast lesions: a Dutch centre experience. Breast Global J. 2023;1(2):49–56. https://doi.org/10.4103/bgj.bgj_2_23.
Davey MG, O’Donnell JP, Boland MR, Ryan EJ, Walsh SR, Kerin MJ, Lowery AJ. Optimal localization strategies for non-palpable breast cancers- A network meta-analysis of randomized controlled trials. Breast. 2022;62:103–13. https://doi.org/10.1016/j.breast.2022.02.004.
Athanansiou C, Mallidis E, Tuffaha H. Comparative effectiveness of different localization techniques for non-palpable breast cancer. A systematic review and network meta-analysis. Eur J Surg Oncol. 2022;48(1):53–9. https://doi.org/10.1016/j.ejso.2021.10.001.
Funding
Mr. Blackney and Ms. Telles declare that they have no conflict of interest. Dr. Moseley is a medical imaging consult for Merit Medical, Hologic, GE, and Siemens Medical.
Author information
Authors and Affiliations
Contributions
All authors (LB, LS, TWM) contributed to the conception and design of this review. All authors gave final approval of the version of the review to be published, and all authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blackney, L., Telles, L. & Moseley, T.W. Pre-surgical Breast Lesion Localization with Non-wire Devices: Information, Benefits, and Limitations. Curr Breast Cancer Rep 16, 377–382 (2024). https://doi.org/10.1007/s12609-024-00554-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-024-00554-1