Abstract
Purpose of Review
Standard DCIS management consists of surgery with consideration of adjuvant radiation and endocrine therapy. However, widespread recognition of the overdiagnosis and overtreatment burden in DCIS has led to a reevaluation of this standard. The purpose of this review is to summarize the foundational clinical trials in DCIS and to discuss ongoing efforts in treatment de-escalation.
Recent Findings
Standard of care DCIS management is based on large high-quality randomized clinical trials. The results of those trials have been durable over more than a decade of follow-up. However, we now better appreciate that DCIS is a heterogeneous disease with variable risk of progression. Clinicopathologic and molecular tools are helping better define which patients with DCIS would benefit from de-escalation. Modern clinical trials have proven the safety of shorter and lower dose radiation regimens in low-risk patients, and results from active monitoring trials are highly anticipated. In addition, decision support tools, shared decision-making, and molecular testing promise to help guide patients through an increasingly complex decision-making process.
Summary
Current treatment of DCIS has moved towards successful de-escalation of treatment for those patients with low risk of progression. Further incorporation of molecular tools will allow for personalized treatment based on individual risk and preferences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ductal carcinoma in situ (DCIS) was previously understood to be a precursor to invasive cancer and thus has been treated with surgery with or without adjuvant radiation. This approach has been very successful, and as a result, long-term breast cancer mortality following treatment for DCIS is very low, only 1.5−3% [1, 2]. But with improved understanding of disease pathogenesis, we now understand that this approach comes at the expense of overtreatment for some patients. It is likely that we detect and treat lesions that would not cause harm during a patient’s lifetime. This contributes to rising healthcare costs, medical waste, and patient physical, financial, and psychological morbidity.
In concert with a refocusing of the healthcare system at large on value, it is only within the past 5−10 years that the concepts of overdiagnosis and overtreatment have gained traction in academic literature [3, 4]. Numerous studies support the now widely held principle that DCIS is a significant contributor to the overdiagnosis burden in breast cancer. Studies of clinically detected lesions treated with biopsy alone report invasive cancer rates of 39−53% with long-term follow-up [5,6,7,8,9]. If the ultimate goal of de-escalation is to treat only those lesions which have the potential to cause harm during a patient’s lifetime, these data suggest that 47−61% of clinically detected DCIS is overdiagnosed. A study by Ryser et al., which used the Breast Cancer Surveillance Consortium to predict the natural course of screen-detected breast cancers, estimated an overdiagnosis rate of 15.4% [10]. Though estimates of overdiagnosis vary according to the methods used, these data have called into question the traditional understanding of breast cancer pathogenesis as progressing from DCIS to invasive cancer. Indeed, it is now better understood to be a non-obligate precursor. DCIS was rare prior to widespread breast cancer screening, but now represents 20−30% of screen-detected breast cancers [11]. Despite a notable rise in DCIS incidence, there has been no reduction in the diagnosis of late-stage breast cancer, suggesting that not all DCIS would have progressed [12]. Taken together these data suggest that a significant proportion of DCIS lesions are overdiagnosed.
Further, uniform application of standard therapies for DCIS results in overtreatment in many patients. Multiple studies have demonstrated that clinicopathologic criteria can stratify recurrence risk; it is generally accepted that patients with low-risk DCIS derive less absolute benefit from standard therapies than patients with high-risk DCIS [1, 13,14,15,16,17,18,19,20,21]. However, no consensus definition of low risk has yet emerged. Evidence in support of overdiagnosis and overtreatment in DCIS has reached critical mass and has been used to support broad-based de-escalation efforts. This review will summarize early clinical trials and will explore the state of the science in de-escalation across treatment modalities in DCIS care.
Early Randomized Trials of Adjuvant Therapy for DCIS
Adjuvant Radiation Therapy
The management of DCIS with adjuvant radiotherapy (RT) has been driven by high quality clinical trials. Four randomized clinical trials initiated in the 1980s and 1990s and two subsequent meta-analyses have evaluated the use of RT in patients with DCIS [1, 13, 18,19,20, 22, 23] These trials, which include NSABP B-17, EORTC 10853, SweDCIS, and UK/ANZ, enrolled nearly 4000 patients and form the basis of support for the benefit of adjuvant RT in reducing the risk of local recurrence following lumpectomy for DCIS [24]. They included all-risk DCIS and employed whole breast radiation (WBI), generally without a boost to the tumor bed. As summarized in the EBCTCG meta-analyses, adjuvant RT reproducibly reduces the risk of in situ and invasive ipsilateral breast tumor recurrence (IBTR) by 50% or more [20, 23]. While adjuvant RT has not been shown to reduce breast cancer mortality following lumpectomy for DCIS, it does reduce the risk of invasive IBTR, which has been shown to be associated with an increased risk of death [1].
Adjuvant Systemic Therapy
Three randomized trials have evaluated the use of tamoxifen in DCIS. IBIS-I, which published long-term follow-up data in 2015, reported that tamoxifen therapy reduced the risk of all new breast cancers by 29%, but had no effect on breast cancer-specific survival [21]. Similarly, NSABP B-24 reported that tamoxifen reduced the risk of invasive IBTR and contralateral breast cancer by 32% without an effect on mortality [1]. A subgroup analysis of patients enrolled in NSABP B-24 confirmed that endocrine therapy only benefitted patients with ER-positive DCIS [25]. The NSABP B-35 and ATAC trials supported the superiority of anastrozole to tamoxifen in postmenopausal women, primarily in those < 60 years of age [26, 27]. IBIS-II confirmed the non-inferiority of anastrozole in postmenopausal women, but failed to establish its superiority, likely due to a low event rate and shorter follow-up [28].
For patients with HER2-positive DCIS, the NSABP B-43 trial explored the use of adjuvant trastuzumab in conjunction with RT. The study enrolled over 2000 patients but did not meet its pre-specified event threshold. The trial reported a non-significant 19% reduction in IBTR events between the RT with trastuzumab and RT alone groups (p = 0.26) [29].
Importantly, adherence to endocrine therapy is variable. Studies conducted in different settings among various patient populations report adherence rates of 30−72% [30,31,32]. One potential option to improve adherence is dose reduction; DeCensi and colleagues conducted a multi-center trial of tamoxifen 5 mg daily for 3 years in women with high risk histologies, including DCIS, and found that dose-reduced tamoxifen decreased the risk of all events (HR of 0.48, 95% CI, 0.26 to 0.92; P = 0.02) and contralateral events (HR 0.25, 95% CI, 0.07 to 0.88; P = 0.02) [33]. Nevertheless, since side effects can be significant, while absolute benefit is small, the threshold to discontinue endocrine therapy in women with DCIS should be low.
De-escalation of Treatment Modalities
Radiation Therapy
Although adjuvant radiotherapy consistently reduces the risk of IBTR following lumpectomy for DCIS [20, 23], the absolute benefit of radiotherapy depends on baseline recurrence risk. For some women, the recurrence risk following lumpectomy alone may be low enough where observation is acceptable. An ipsilateral recurrence risk of < 10% at 10 years is generally considered an acceptable threshold at which to omit RT, though individual patients may assess risk differently. Three studies have prospectively defined low-risk DCIS using similar clinicopathologic criteria and have reported LR rates of 14.4−15.6% at 10−15 years without RT (Table 1) [13, 34, 35]. RTOG 9804 defined low-risk DCIS as those lesions that were grade 1 or 2, ≤.5 cm, and were excised with margins ≥3 mm. Even in this low-risk group, where the median size of DCIS was only 0.5 cm, RT reduced the risk of LR by 64% (7.1% with RT vs 15.1% without RT) at 15 years [13]. The prospective cohort ECOG-ACRIN E5194 and DFCI studies similarly reported rates of LR of about 1% per year without plateau [34, 35]. As evidenced by these studies, clinicopathologic criteria have been unable to identify a population of patients who have a recurrence risk of < 10% without adjuvant RT. Investigation into the ability of refined clinicopathologic criteria and molecular testing to prospectively identify patients with lower rates of recurrence following lumpectomy alone for DCIS is ongoing (Table 2).
For those who receive RT, there is now an array of options for appropriately selected patients that can dramatically reduce treatment time and toxicity. Randomized data support the use of hypofractionated WBI with or without a tumor bed boost [36, 37] or accelerated partial breast radiation (APBI) [38]. Several recently published results have contributed to these recommendations.
Hypofractionation reduces the duration of RT treatment from 6−7 weeks to 3 weeks or less while still treating the entire breast [39]. Recently published randomized data now support the safety of hypofractionation in DCIS patients. The DBCG-HYPO trial randomized 246 (13.3% of the overall cohort) patients with DCIS to receive the standard 50 Gy in 25 fractions or 40 Gy in 15 fractions and did not find a difference in LR based on fractionation [36]. More recently, the BIG 3-07/TROG 07.01 randomized study showed no difference in recurrence rates between the standard and hypofractionation arms for patients with DCIS [40]. The ongoing NOVEMBER trial is enrolling patients with all-risk DCIS lesions to be treated with 9 fractions over the course of 2 weeks (Table 2; NCT03345420).
APBI has the potential to reduce treatment duration even further, but risks leaving potentially untreated disease elsewhere in the breast and is therefore only recommended for patients with low-risk DCIS. Summarized in Tables 1 and 2, modes of APBI delivery are numerous, but the body of evidence supporting APBI use in DCIS is limited by the small number of patients included in trials. A Cochrane review of partial breast irradiation for early breast cancer published in 2021 reported slightly reduced local recurrence-free survival with the use of PBI/APBI compared to WBI (HR 1.21 [95% CI 1.03−1.42]) with similar overall survival and cause-specific survival [41]. However, only 6.3% of included patients had DCIS [41]. Nevertheless, the most recent ASTRO APBI consensus statement, published in 2017, expands the acceptability conditions to include DCIS patients meeting RTOG 9804 inclusion criteria based on the low recurrence rate in the observational arm of this trial (Table 1) [42].
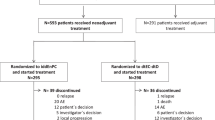
The largest and most mature clinical trial of APBI in DCIS is NSABP B-39/RTOG 0413, which randomized 4216 patients, 24% of whom had DCIS, to WBI or APBI (Table 1) [38]. At 10 years of follow-up, there was no increased risk of IBTR in the DCIS patients who received APBI (HR 1.01 [CI.61−1.68], P = 0.48) [38]. The RAPID trial randomized patients to receive either twice daily external beam APBI or WBI with or without a boost. There was no difference in IBTR between study groups (Table 1; HR 1.27 [90% CI 0.84−1.91]), but there was increased late toxicity and adverse cosmesis in the APBI arm [43]. Boutrus et al. reported improved cosmetic outcomes with once daily versus twice daily fractions and similar recurrence rates, although median follow-up was only 74 months and only 8.8% of the patients had DCIS [44]. Twice daily regimens have since gone out of favor. There are several ongoing trials investigating the use of APBI for DCIS patients (Table 2). Optimal de-escalation of RT will reduce total treatment duration without sacrificing recurrence risk or cosmesis (Fig. 1).
Treatment guidelines for DCIS. Ongoing active surveillance trials may add observation as an option for primary treatment of DCIS (dashed lines). In addition, ongoing biomarker research may add molecular testing as part of the workup for some or all DCIS patients to determine benefit from adjuvant radiation
Surgery
De-escalation efforts in the surgical management of DCIS center around the safety of active monitoring (AM) for patients with low-risk disease. AM is currently not recommended outside of a clinical trial, as prospective data are lacking. However, multiple studies have predicted the safety of AM using both real-world and simulated datasets [45, 46]. In their analysis of the Surveillance, Epidemiology, and End Results (SEER) database, Byng et al. reported a 3% risk of ipsilateral invasive breast cancer at 10 years in a cohort of women with low-risk DCIS who did not receive local treatment [14, 47]. This is well within age-specific norms for women without a previous diagnosis of DCIS or invasive breast cancer [14, 47].
To fill the evidence gap, four phase III, international, randomized clinical trials have been initiated to determine the safety and effectiveness of AM: COMET (USA; NCT02926911), LORD (Europe; NCT02492607), LORIS (UK), and LORETTA (Japan) [48,49,50,51]. The LORD trial converted to a patient preference trial in 2020. The ability of these trials to accurately identify cases of DCIS at low risk of invasive progression will be critical to their success. As discussed previously, clinicopathologic criteria have been unable to sufficiently risk stratify patients considering adjuvant RT. Even so, all four of these trials use clinicopathologic criteria to define trial eligibility. Understandably, several studies have called this strategy into question. The upstage rate to invasive disease at surgery among patients eligible for active monitoring trials has been reported in various studies: 6−21.7% for COMET, 7−24% for LORIS, and 5−10% for LORD [52,53,54]. While a valid concern, eliminating any risk of upgrade is impossible, and a prospective study is the best setting in which to test the long-term safety of AM and its ability to appropriately identify and manage disease progression. Indeed, the cancer-specific survival of patients on AM in the prostate cancer literature is over 95% despite a known risk of progression, suggesting the potential for real world feasibility of AM in DCIS [55].
A key component of AM will also be its acceptability to patients. It is well understood that patients with DCIS dramatically overestimate their risk of invasive cancer, which contributes to psychological morbidity and could limit incorporation of AM into practice in the future [56,57,58,59]. And so, patient reported outcomes from ongoing trials will provide much needed insight into AM acceptability and associated psychosocial morbidity.
In the meantime, prostate cancer serves as a valid model for the tolerability of AM in cancer patients. Low-risk prostate cancer has a prolonged natural history and excellent survival, like DCIS. Furthermore, patients with prostate cancer cite many of the same factors as important in their treatment decision making as those reported by DCIS and breast cancer patients [57, 58, 60,61,62]. Evidence from prospective AM prostate cancer cohorts suggests that patients have generally favorable levels of anxiety and depression and that few patients opt for active treatment unless clinically indicated [63,64,65]. While an imperfect surrogate, these findings suggest that some DCIS patients may tolerate AM without undue psychosocial effects. The percentage of patients opting for AM of prostate cancer has increased dramatically since it was first recommended, lending credence to this conclusion [66]. Evaluation of patient-reported outcomes will be critical to understanding the role of surgical de-escalation for low-risk DCIS.
Prognostic and Predictive Tools
The holy grail of prognostic and predictive tools in DCIS care is a method to predict the risk of invasive recurrence or progression and the benefit from local and adjuvant therapies. Multiple tools have been developed that use clinicopathologic characteristics to predict the local recurrence risk following surgical excision. The Van Nuys prognostic index (VNPI), originally published in 1995 and updated since, is one such example [67]. Silverstein et al. identified a population of patients with VNPI scores of 4−6 who did not have improved recurrence-free survival with adjuvant radiation [67]. However, subsequent studies have contradicted these findings [16, 68]. The Memorial Sloan Kettering Cancer Center (MSKCC) nomogram uses 10 variables to predict 5- and 10-year probability of IBTR [69]. Attempts at external validation of the nomogram have had variable results [15, 70, 71]. Yi et al. reported that the nomogram overestimated the observed risk of recurrence, especially among patients with the highest estimated risk [70]. These findings are supported by others [71]. Thus far, clinicopathologic variables have not been able to reliably predict local recurrence (LR).
In keeping with the rise in genomic testing in oncology more broadly, several molecular tests have been developed to identify low-risk subsets of DCIS patients. The Oncotype DX DCIS Score is a 12-gene assay that is predictive of LR risk following breast conserving surgery [72]. The assay has two major limitations. The first is that it does not predict adjuvant RT benefit [72]. The second is that clinicopathologic criteria remained significant predictors of LR independent of DCIS score, limiting the interpretability of the test. In a subsequent analysis, the authors explored the effects of these other variables on 10-year LR rates [73]. They provided further detail on LR risk within subgroups of tumor size, age, and DCIS score [73]. Multiple subgroups had a LR risk of less than 8% at 10 years, suggesting that these patients might reasonably consider omission of RT [73]. These additional clinical variables have now been incorporated into DCIS Score reporting, now called the Refined DCIS Score (RDS).
Two studies are investigating the use of the RDS in clinical practice. The ELISA study is prospective cohort study investigating outcomes following surgery alone in women with low-risk DCIS according to RDS and clinicopathologic criteria (NCT04797299). The DUCHESS study is evaluating the effect of RDS on treatment decisions and published initial results in 2021 (NCT02766881) [74]. They reported that the assay led to a change in treatment recommendation in 35.2% of cases and decreased the percentage of cases in which RT was recommended from 79% to 50%. Use of the assay was also associated with improved patient satisfaction and reduced decisional conflict [74].
Oncotype Dx, a 21-gene assay, itself widely used in early-stage luminal A invasive breast cancer, has also recently been shown by Rakovitch et al. to predict breast cancer-related mortality benefit from RT in 1362 patients in the Ontario DCIS cohort [24, 75]. Though retrospective in nature, this study was the first to report a population of DCIS patients who had improved cause-specific mortality with the addition of RT [75]. This study highlights the need for thoughtful consideration of valid endpoints in DCIS trials, which are almost always recurrence and not survival, but further studies are needed to clarify the role of Oncotype Dx in DCIS care.
The DCISionRT assay is the only molecular test in DCIS that has been shown to identify a subgroup of patients that do not benefit from RT [76]. Bremer and colleagues retrospectively analyzed archived tissue samples from 721 patients with DCIS treated with breast conserving surgery [76]. The authors incorporated molecular and clinicopathologic characteristics into a biological signature, called DCISionRT, that is expressed as a Decision Score (DS) on a scale of increasing LR risk from 0 to 10. Patients with a score or 3 or less had a 10-year invasive breast cancer (IBC) risk of 4% [76]. Among patients with DS≤3, adjuvant radiation also did not appear to significantly reduce the risk of IBC (HR 0.6 [95% CI 0.2−2.3]; P = 0.49) [76]. In comparison, patients with DS > 3 had a 70% reduction in IBC risk with adjuvant RT (HR 0.3 [95% CI 0.1−0.6]; P = 0.003). However, the confidence interval in the low-risk group was wide, and there were only 33 IBC events [76]. The PREDICT registry trial will prospectively evaluate the impact of DCISionRT on treatment decisions and monitor outcomes (NCT03448926).
Cost Effectiveness of Predictive Tools
The proliferation of expensive molecular testing has appropriately raised questions as to how these tests should be applied in clinical practice to promote high value care. Highlighting this, a comparison of the MSKCC Nomogram, which is available for free online, and RDS, reported that LR risk estimates were concordant in 92% of the 59 patients in the study [71]. Further analysis suggested that benefit from RDS may be restricted to patients at highest risk of recurrence according to clinicopathologic criteria. Kim et al. determined that DCISionRT testing is cost-effective compared to the current practice of using clinicopathologic characteristics to make RT treatment decisions, especially among patients with clinically high-risk DCIS [77]. Raldow and colleagues used a similar method to evaluate DCISionRT, but they did not incorporate clinicopathologic characteristics into their modeling and used higher cost estimates than other studies. Universal DCISionRT testing with RT for patients with elevated genomic risk became cost effective when the cost of testing was less than $4588 [78]. Overall, DCISionRT is likely to be cost-effective for use in clinical practice in some situations. As the cost of molecular testing comes down, barriers to more routine use will become less significant.
Only one study has evaluated the cost effectiveness of the Oncotype DCIS Score. The results, which showed that the DCIS Score is not cost effective, likely reflect the inability of this assay to predict benefit from RT [79]. Results varied significantly with only minor changes in treatment utility, emphasizing the importance of patient risk tolerance in DCIS treatment decision-making [79]. Taken together, the cost-effectiveness of molecular testing is dictated largely by the predictive power of the test, the clinical risk of the lesion, patient risk tolerance, and cost. As molecular tests improve and costs decrease, their clinical applications will likely expand. It is also important to note the value that patients place on personalized medicine, which will likely continue to drive the development and use of molecular assays [74].
Decision Aids and Shared Decision-Making
Decision aids are patient-facing tools designed to communicate diagnostic and prognostic information and help clarify patient values [80]. Shared decision-making (SDM) is the process of partnering with patients in health decisions. Together, the clinician and patient discuss reasonable options and patient preferences and collaborate to reach a decision [81]. The relative equivalence of standard treatment options and ongoing de-escalation efforts mean that DCIS treatment decision-making is highly sensitive to patient preferences and therefore well suited to SDM [82, 83]. An ongoing shift away from paternalistic practice creates even more space for values-based decision-making.
While this represents a positive step in healthcare delivery, we should also recognize that patients and clinicians are being asked to navigate an increasingly complex treatment landscape, and the factors that affect treatment decisions are widely varied and fluid [58, 84,85,86,87]. Time pressure in clinical encounters makes it challenging to effectively communicate diagnostic and prognostic information, discuss relevant treatment options and values and preferences, and come to a shared decision all within the time allotted. Recently, the information gathering and decision-making process has expanded outside of the clinical encounter in the form of decision aids [80, 88,89,90]. The quality of decision aids is variable, but some have been shown to increase knowledge, improve risk perception, and reduce decisional conflict [91, 92]. However, utilization of decision aids in routine practice is low [93,94,95]. Increased attention should be given to developing and sustainably implementing high quality decision aids, as this may facilitate quality decision making and improve patient-reported outcomes where treatments are preference sensitive.
The shift from a more paternalistic practice of medicine to one that actively engages patients in their own care is almost certainly here to stay. Therefore, SDM is now a foundational skill in clinical practice. However, as with decision aids, incorporation into clinical practice varies. While physicians generally support SDM in theory, this does not reflect actual behavior, where use of SDM is much lower [96, 97]. Clinician-cited barriers to SDM include challenges communicating treatment equipoise, the perceived difficulties of engaging patients with less formal education, a feeling that some patients might prefer a more paternalistic approach, and the constraints of time [81, 96]. Patients often describe physician communication as a barrier [97]. Thus, there is a need for innovative approaches to support and incentivize providers to authentically partner with their patients in the treatment planning process. In the end, de-escalation should be centered on patients: how best to prepare and safely guide them through DCIS treatment in a way that is most aligned with their values and preferences, and which promotes high value care delivery.
Conclusion
De-escalation aims to right-size therapies using high quality evidence to better balance the risks of a disease with the risks and benefits of its treatment. De-escalation is therefore hinged on accurate risk stratification, which determines eligibility for an increasingly complex array of treatment pathways. In the case of DCIS, clinicopathologic criteria have thus far been unable to stratify patients to the degree required to make treatment decisions, and so focus has shifted onto molecular assays, following a similar trend to that seen in invasive breast cancer. It is likely that molecular assays will become important tools in surgical and adjuvant decision making in DCIS. Risk assessments are then contextualized within a patient’s own values and goals, with the help of the provider, to come up with a treatment plan. The complexity of this process requires a creative and multifaceted approach to preparing patients and providers for informed shared decision making that will extend beyond the bounds of the clinical encounter, to right-size treatment to both disease risk and patient preference.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wapnir IL, Dignam JJ, Fisher B, Mamounas EP, Anderson SJ, Julian TB, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–88. https://doi.org/10.1093/jnci/djr027.
van Maaren MC, Lagendijk M, Tilanus-Linthorst MMA, de Munck L, Pijnappel RM, Schmidt MK, et al. Breast cancer-related deaths according to grade in ductal carcinoma in situ: a Dutch population-based study on patients diagnosed between 1999 and 2012. Eur J Cancer. 2018;101:134–42. https://doi.org/10.1016/j.ejca.2018.07.003.
Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. 2016;12(11):646–53. https://doi.org/10.1038/nrendo.2016.110.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13. https://doi.org/10.1093/jnci/djq099.
Rosen PP, Braun DW Jr, Kinne DE. The clinical significance of pre-invasive breast carcinoma. Cancer. 1980;46(4 Suppl):919–25 10.1002/1097-0142(19800815)46:4+<919::aid-cncr2820461311>3.0.co;2-z.
Betsill WL Jr, Rosen PP, Lieberman PH, Robbins GF. Intraductal carcinoma. Long-term follow-up after treatment by biopsy alone. JAMA. 1978;239(18):1863–7. https://doi.org/10.1001/jama.239.18.1863.
Collins LC, Tamimi RM, Baer HJ, Connolly JL, Colditz GA, Schnitt SJ. Outcome of patients with ductal carcinoma in situ untreated after diagnostic biopsy: results from the Nurses’ Health Study. Cancer. 2005;103(9):1778–84. https://doi.org/10.1002/cncr.20979.
Sanders ME, Schuyler PA, Dupont WD, Page DL. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103(12):2481–4. https://doi.org/10.1002/cncr.21069.
Sanders ME, Schuyler PA, Simpson JF, Page DL, Dupont WD. Continued observation of the natural history of low-grade ductal carcinoma in situ reaffirms proclivity for local recurrence even after more than 30 years of follow-up. Mod Pathol. 2015;28(5):662–9. https://doi.org/10.1038/modpathol.2014.141.
Ryser MD, Lange J, Inoue LYT, O'Meara ES, Gard C, Miglioretti DL, et al. Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. Ann Intern Med. 2022;175(4):471–8. https://doi.org/10.7326/M21-3577.
Ward EM, DeSantis CE, Lin CC, Kramer JL, Jemal A, Kohler B, et al. Cancer statistics: breast cancer in situ. CA Cancer J Clin. 2015;65(6):481–95. https://doi.org/10.3322/caac.21321.
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005. https://doi.org/10.1056/NEJMoa1206809.
McCormick B, Winter KA, Woodward W, Kuerer HM, Sneige N, Rakovitch E, et al. Randomized phase III trial evaluating radiation following surgical excision for good-risk ductal carcinoma in situ: long-term report from NRG oncology/RTOG 9804. J Clin Oncol. 2021;39(32):3574–82. https://doi.org/10.1200/JCO.21.01083.
Byng D, Retel VP, Schaapveld M, Wesseling J, van Harten WH, Pc GC. Treating (low-risk) DCIS patients: what can we learn from real-world cancer registry evidence? Breast Cancer Res Treat. 2021;187(1):187–96. https://doi.org/10.1007/s10549-020-06042-1.
Collins LC, Achacoso N, Haque R, Nekhlyudov L, Quesenberry CP Jr, Schnitt SJ, et al. Risk prediction for local breast cancer recurrence among women with DCIS treated in a community practice: a nested, case-control study. Ann Surg Oncol. 2015;22(Suppl 3):S502–8. https://doi.org/10.1245/s10434-015-4641-x.
Di Saverio S, Catena F, Santini D, Ansaloni L, Fogacci T, Mignani S, et al. 259 Patients with DCIS of the breast applying USC/Van Nuys prognostic index: a retrospective review with long term follow up. Breast Cancer Res Treat. 2008;109(3):405–16. https://doi.org/10.1007/s10549-007-9668-7.
Lei RY, Carter DL, Antell AG, Nowels MA, Tole SP, Bennett JP, et al. A comparison of predicted ipsilateral tumor recurrence risks in patients with ductal carcinoma in situ of the breast after breast-conserving surgery by breast radiation oncologists, the Van Nuys Prognostic Index, the Memorial Sloan Kettering Cancer Center DCIS Nomogram, and the 12-Gene DCIS Score Assay. Adv Radiat Oncol. 2021;6(2):100607. https://doi.org/10.1016/j.adro.2020.10.020.
Group EBCC, Group ER, Bijker N, Meijnen P, Peterse JL, Bogaerts J, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma-in-situ: ten-year results of European Organisation for Research and Treatment of Cancer randomized phase III trial 10853--a study by the EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. J Clin Oncol. 2006;24(21):3381–7. https://doi.org/10.1200/JCO.2006.06.1366.
Emdin SO, Granstrand B, Ringberg A, Sandelin K, Arnesson LG, Nordgren H, et al. SweDCIS: Radiotherapy after sector resection for ductal carcinoma in situ of the breast. Results of a randomised trial in a population offered mammography screening. Acta Oncol. 2006;45(5):536–43. https://doi.org/10.1080/02841860600681569.
Early Breast Cancer Trialists’ Collaborative, Correa C, McGale P, Taylor C, Wang Y, Clarke M, Davies C, Peto R, Bijker N, Solin L, Darby S. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J Natl Cancer Inst Monogr. 2010;2010(41):162–77. https://doi.org/10.1093/jncimonographs/lgq039.
Cuzick J, Sestak I, Cawthorn S, Hamed H, Holli K, Howell A, et al. Tamoxifen for prevention of breast cancer: extended long-term follow-up of the IBIS-I breast cancer prevention trial. Lancet Oncol. 2015;16(1):67–75. https://doi.org/10.1016/S1470-2045(14)71171-4.
Cuzick J, Sestak I, Pinder SE, Ellis IO, Forsyth S, Bundred NJ, et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. The Lancet Oncology. 2011;12(1):21–9. https://doi.org/10.1016/s1470-2045(10)70266-7.
Goodwin A, Parker S, Ghersi D, Wilcken N. Post-operative radiotherapy for ductal carcinoma in situ of the breast. Cochrane Database Syst Rev. 2013;11:CD000563. https://doi.org/10.1002/14651858.CD000563.pub7.
Network NCC: Breast Cancer (Version 2.2022- December 20, 2021). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf (2021). .
Allred DC, Anderson SJ, Paik S, Wickerham DL, Nagtegaal ID, Swain SM, et al. Adjuvant tamoxifen reduces subsequent breast cancer in women with estrogen receptor-positive ductal carcinoma in situ: a study based on NSABP protocol B-24. J Clin Oncol. 2012;30(12):1268–73. https://doi.org/10.1200/JCO.2010.34.0141.
Cuzick J, Sestak I, Baum M, Buzdar A, Howell A, Dowsett M, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol. 2010;11(12):1135–41. https://doi.org/10.1016/S1470-2045(10)70257-6.
Margolese RG, Cecchini RS, Julian TB, Ganz PA, Costantino JP, Vallow LA, et al. Anastrozole versus tamoxifen in postmenopausal women with ductal carcinoma in situ undergoing lumpectomy plus radiotherapy (NSABP B-35): a randomised, double-blind, phase 3 clinical trial. Lancet. 2016;387(10021):849–56. https://doi.org/10.1016/S0140-6736(15)01168-X.
Forbes JF, Sestak I, Howell A, Bonanni B, Bundred N, Levy C, et al. Anastrozole versus tamoxifen for the prevention of locoregional and contralateral breast cancer in postmenopausal women with locally excised ductal carcinoma in situ (IBIS-II DCIS): a double-blind, randomised controlled trial. Lancet. 2016;387(10021):866–73. https://doi.org/10.1016/S0140-6736(15)01129-0.
Cobleigh MA, Anderson SJ, Siziopikou KP, Arthur DW, Rabinovitch R, Julian TB, et al. Comparison of radiation with or without concurrent trastuzumab for HER2-positive ductal carcinoma in situ resected by lumpectomy: a phase III clinical trial. J Clin Oncol. 2021;39(21):2367–74. https://doi.org/10.1200/JCO.20.02824.
Karavites LC, Kane AK, Zaveri S, Xu Y, Helenowski I, Hansen N, et al. Tamoxifen acceptance and adherence among patients with ductal carcinoma in situ (DCIS) treated in a multidisciplinary setting. Cancer Prev Res (Phila). 2017;10(7):389–97. https://doi.org/10.1158/1940-6207.CAPR-17-0029.
Llarena NC, Estevez SL, Tucker SL, Jeruss JS. Impact of fertility concerns on tamoxifen initiation and persistence. J Natl Cancer Inst. 2015;107(10). https://doi.org/10.1093/jnci/djv202.
Zhao H, Hei N, Wu Y, Chan W, Lei X, Cameron C, et al. Initiation of and adherence to tamoxifen and aromatase inhibitor therapy among elderly women with ductal carcinoma in situ. Cancer. 2017;123(6):940–7. https://doi.org/10.1002/cncr.30425.
DeCensi A, Puntoni M, Guerrieri-Gonzaga A, Caviglia S, Avino F, Cortesi L, et al. Randomized placebo controlled trial of low-dose tamoxifen to prevent local and contralateral recurrence in breast intraepithelial neoplasia. J Clin Oncol. 2019;37(19):1629–37. https://doi.org/10.1200/JCO.18.01779.
Wong JS, Chen YH, Gadd MA, Gelman R, Lester SC, Schnitt SJ, et al. Eight-year update of a prospective study of wide excision alone for small low- or intermediate-grade ductal carcinoma in situ (DCIS). Breast Cancer Res Treat. 2014;143(2):343–50. https://doi.org/10.1007/s10549-013-2813-6.
Solin LJ, Gray R, Hughes LL, Wood WC, Lowen MA, Badve SS, et al. Surgical excision without radiation for ductal carcinoma in situ of the breast: 12-year results from the ECOG-ACRIN E5194 study. J Clin Oncol. 2015;33(33):3938–44. https://doi.org/10.1200/JCO.2015.60.8588.
Offersen BV, Alsner J, Nielsen HM, Jakobsen EH, Nielsen MH, Krause M, et al. Hypofractionated versus standard fractionated radiotherapy in patients with early breast cancer or ductal carcinoma in situ in a randomized phase III trial: the DBCG HYPO trial. J Clin Oncol. 2020;38(31):3615–25. https://doi.org/10.1200/JCO.20.01363.
King MT, Link EK, Whelan TJ, Olivotto IA, Kunkler I, Westenberg AH, et al. Quality of life after breast-conserving therapy and adjuvant radiotherapy for non-low-risk ductal carcinoma in situ (BIG 3-07/TROG 07.01): 2-year results of randomized, controlled, phase 3 trial. Lancet Oncol. 2020;21:685–98. https://doi.org/10.1016/S1470-2045(20)30085-1.
Vicini FA, Cecchini RS, White JR, Arthur DW, Julian TB, Rabinovitch RA, et al. Long-term primary results of accelerated partial breast irradiation after breast-conserving surgery for early-stage breast cancer: a randomised, phase 3, equivalence trial. The Lancet. 2019;394(10215):2155–64. https://doi.org/10.1016/s0140-6736(19)32514-0 Though this trial failed to meet its prespecified endpoint for equivalence, a subgroup analysis of DCIS patients showed no increased risk of ipsilateral breast tumor recurrence.
Smith BD, Bellon JR, Blitzblau R, Freedman G, Haffty B, Hahn C, et al. Radiation therapy for the whole breast: executive summary of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Pract Radiat Oncol. 2018;8(3):145–52. https://doi.org/10.1016/j.prro.2018.01.012.
Chua BH, Link EK, Kunkler IH, Whelan TJ, Westenberg AH, Gruber G, et al. Radiation doses and fractionation schedules in non-low-risk ductal carcinoma in situ in the breast (BIG 3-07/TROG 07.01): a randomised, factorial, multicentre, open-label, phase 3 study. Lancet. 2022;400(10350):431–40. https://doi.org/10.1016/S0140-6736(22)01246-6.
Hickey BE, Lehman M. Partial breast irradiation versus whole breast radiotherapy for early breast cancer. Cochrane Database Syst Rev. 2021;8:CD007077. https://doi.org/10.1002/14651858.CD007077.pub4.
Correa C, Harris EE, Leonardi MC, Smith BD, Taghian AG, Thompson AM, et al. Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol. 2017;7(2):73–9. https://doi.org/10.1016/j.prro.2016.09.007.
Whelan TJ, Julian JA, Berrang TS, Kim D-H, Germain I, Nichol AM, et al. External beam accelerated partial breast irradiation versus whole breast irradiation after breast conserving surgery in women with ductal carcinoma in situ and node-negative breast cancer (RAPID): a randomised controlled trial. The Lancet. 2019;394(10215):2165–72. https://doi.org/10.1016/s0140-6736(19)32515-2.
Boutrus RR, El Sherif S, Abdelazim Y, Bayomy M, Gaber AS, Farahat A, et al. Once daily versus twice daily external beam accelerated partial breast irradiation: a randomized prospective study. Int J Radiat Oncol Biol Phys. 2021;109(5):1296–300. https://doi.org/10.1016/j.ijrobp.2020.11.044.
Ryser MD, Worni M, Turner EL, Marks JR, Durrett R, Hwang ES. Outcomes of active surveillance for ductal carcinoma in situ: a computational risk analysis. J Natl Cancer Inst. 2016;108(5). https://doi.org/10.1093/jnci/djv372.
Ryser MD, Weaver DL, Zhao F, Worni M, Grimm LJ, Gulati R, et al. Cancer outcomes in DCIS patients without locoregional treatment. J Natl Cancer Inst. 2019;111(9):952–60. https://doi.org/10.1093/jnci/djy220.
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438–51. https://doi.org/10.3322/caac.21583.
Kanbayashi C, Thompson AM, Hwang E-SS, Partridge AH, Rea DW, Wesseling J, et al. The international collaboration of active surveillance trials for low-risk DCIS (LORIS, LORD, COMET, LORETTA). Journal of Clinical Oncology. 2019;37(15_suppl):TPS603-TPS. https://doi.org/10.1200/JCO.2019.37.15_suppl.TPS603.
Hwang ES, Hyslop T, Lynch T, Frank E, Pinto D, Basila D, et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9(3):e026797. https://doi.org/10.1136/bmjopen-2018-026797.
Francis A, Thomas J, Fallowfield L, Wallis M, Bartlett JM, Brookes C, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer. 2015;51(16):2296–303. https://doi.org/10.1016/j.ejca.2015.07.017.
Elshof LE, Tryfonidis K, Slaets L, van Leeuwen-Stok AE, Skinner VP, Dif N, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ - The LORD study. Eur J Cancer. 2015;51(12):1497–510. https://doi.org/10.1016/j.ejca.2015.05.008.
Grimm LJ, Ryser MD, Partridge AH, Thompson AM, Thomas JS, Wesseling J, et al. Surgical upstaging rates for vacuum assisted biopsy proven DCIS: implications for active surveillance trials. Ann Surg Oncol. 2017;24(12):3534–40. https://doi.org/10.1245/s10434-017-6018-9.
Oseni TO, Smith BL, Lehman CD, Vijapura CA, Pinnamaneni N, Bahl M. Do eligibility criteria for ductal carcinoma in situ (DCIS) active surveillance trials identify patients at low risk for upgrade to invasive carcinoma? Ann Surg Oncol. 2020;27(11):4459–65. https://doi.org/10.1245/s10434-020-08576-6.
Patel GV, Van Sant EP, Taback B, Ha R. Patient selection for ductal carcinoma in situ observation trials: are the lesions truly low risk. AJR Am J Roentgenol. 2018;211(3):712–3. https://doi.org/10.2214/AJR.17.19244.
Network NCC: Prostate Cancer (Version 2.2022). https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf .
Partridge A, Adloff K, Blood E, Dees EC, Kaelin C, Golshan M, et al. Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. J Natl Cancer Inst. 2008;100(4):243–51. https://doi.org/10.1093/jnci/djn010.
Kim C, Liang L, Wright FC, Hong NJL, Groot G, Helyer L, et al. Interventions are needed to support patient-provider decision-making for DCIS: a scoping review. Breast Cancer Res Treat. 2018;168(3):579–92. https://doi.org/10.1007/s10549-017-4613-x.
Rutherford C, Mercieca-Bebber R, Butow P, Wu JL, King MT. Treatment decision-making in ductal carcinoma in situ: a mixed methods systematic review of women's experiences and information needs. Patient Educ Couns. 2017;100(9):1654–66. https://doi.org/10.1016/j.pec.2017.04.009.
De Morgan S, Redman S, D'Este C, Rogers K. Knowledge, satisfaction with information, decisional conflict and psychological morbidity amongst women diagnosed with ductal carcinoma in situ (DCIS). Patient Educ Couns. 2011;84(1):62–8. https://doi.org/10.1016/j.pec.2010.07.002.
Anandadas CN, Clarke NW, Davidson SE, O'Reilly PH, Logue JP, Gilmore L, et al. Early prostate cancer--which treatment do men prefer and why. BJU Int. 2011;107(11):1762–8. https://doi.org/10.1111/j.1464-410X.2010.09833.x.
Davison BJ, Breckon E. Factors influencing treatment decision making and information preferences of prostate cancer patients on active surveillance. Patient Educ Couns. 2012;87(3):369–74. https://doi.org/10.1016/j.pec.2011.11.009.
Xu J, Dailey RK, Eggly S, Neale AV, Schwartz KL. Men’s perspectives on selecting their prostate cancer treatment. J Natl Med Assoc. 2011;103(6):468–78. https://doi.org/10.1016/s0027-9684(15)30359-x.
Venderbos LD, van den Bergh RC, Roobol MJ, Schroder FH, Essink-Bot ML, Bangma CH, et al. A longitudinal study on the impact of active surveillance for prostate cancer on anxiety and distress levels. Psychooncology. 2015;24(3):348–54. https://doi.org/10.1002/pon.3657.
van den Bergh RC, Essink-Bot ML, Roobol MJ, Wolters T, Schroder FH, Bangma CH, et al. Anxiety and distress during active surveillance for early prostate cancer. Cancer. 2009;115(17):3868–78. https://doi.org/10.1002/cncr.24446.
Bellardita L, Valdagni R, van den Bergh R, Randsdorp H, Repetto C, Venderbos LD, et al. How does active surveillance for prostate cancer affect quality of life? A systematic review. Eur Urol. 2015;67(4):637–45. https://doi.org/10.1016/j.eururo.2014.10.028.
Cooperberg MR, Carroll PR. Trends in management for patients with localized prostate cancer, 1990-2013. JAMA. 2015;314(1):80–2. https://doi.org/10.1001/jama.2015.6036.
Silverstein MJ. The University of Southern California/Van Nuys prognostic index for ductal carcinoma in situ of the breast. The American Journal of Surgery. 2003;186(4):337–43. https://doi.org/10.1016/s0002-9610(03)00265-4.
Kunkiel M, Niwinska A. Assessment of the usefulness of prognostic Van Nuys Prognostic Index in the treatment in ductal carcinoma in situ in 15-year observation. Sci Rep. 2021;11(1):22645. https://doi.org/10.1038/s41598-021-02126-0.
Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, et al. Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol. 2010;28(23):3762–9. https://doi.org/10.1200/JCO.2009.26.8847.
Yi M, Meric-Bernstam F, Kuerer HM, Mittendorf EA, Bedrosian I, Lucci A, et al. Evaluation of a breast cancer nomogram for predicting risk of ipsilateral breast tumor recurrences in patients with ductal carcinoma in situ after local excision. J Clin Oncol. 2012;30(6):600–7. https://doi.org/10.1200/JCO.2011.36.4976.
Van Zee KJ, Zabor EC, Di Donato R, Harmon B, Fox J, Morrow M, et al. Comparison of local recurrence risk estimates after breast-conserving surgery for DCIS: DCIS nomogram versus refined oncotype DX breast DCIS score. Ann Surg Oncol. 2019;26(10):3282–8. https://doi.org/10.1245/s10434-019-07537-y.
Rakovitch E, Nofech-Mozes S, Hanna W, Baehner FL, Saskin R, Butler SM, et al. A population-based validation study of the DCIS Score predicting recurrence risk in individuals treated by breast-conserving surgery alone. Breast Cancer Res Treat. 2015;152(2):389–98. https://doi.org/10.1007/s10549-015-3464-6.
Rakovitch E, Gray R, Baehner FL, Sutradhar R, Crager M, Gu S, et al. Refined estimates of local recurrence risks by DCIS score adjusting for clinicopathological features: a combined analysis of ECOG-ACRIN E5194 and Ontario DCIS cohort studies. Breast Cancer Res Treat. 2018;169(2):359–69. https://doi.org/10.1007/s10549-018-4693-2.
Rakovitch E, Parpia S, Koch A, Grimard L, Soliman H, Stevens C, et al. DUCHESS: an evaluation of the ductal carcinoma in situ score for decisions on radiotherapy in patients with low/intermediate-risk DCIS. Breast Cancer Res Treat. 2021;188(1):133–9. https://doi.org/10.1007/s10549-021-06187-7.
Rakovitch E, Sutradhar R, Nofech-Mozes S, Gu S, Fong C, Hanna W, et al. 21-gene assay and breast cancer mortality in ductal carcinoma in situ. J Natl Cancer Inst. 2021;113(5):572–9. https://doi.org/10.1093/jnci/djaa179.
Bremer T, Whitworth PW, Patel R, Savala J, Barry T, Lyle S, et al. A biological signature for breast ductal carcinoma in situ to predict radiotherapy benefit and assess recurrence risk. Clin Cancer Res. 2018;24(23):5895–901. https://doi.org/10.1158/1078-0432.CCR-18-0842 Results show that the Decision Score identifies patients who have a low risk of invasive recurrence. Additionally, this is also the only predictive test of its kind that has been able to identify low-risk DCIS patients who do not seem to benefit from radiotherapy.
Kim H, Vargo JA, Smith KJ, Beriwal S. Cost-effectiveness analysis of biological signature DCISionRT use for DCIS treatment. Clin Breast Cancer. 2021;21(3):e271–e8. https://doi.org/10.1016/j.clbc.2020.10.007.
Raldow AC, Sher D, Chen AB, Punglia RS. Cost effectiveness of DCISionRT for guiding treatment of ductal carcinoma in situ. JNCI Cancer Spectr. 2020;4(2):pkaa004. https://doi.org/10.1093/jncics/pkaa004.
Raldow AC, Sher D, Chen AB, Recht A, Punglia RS. Cost effectiveness of the oncotype DX DCIS score for guiding treatment of patients with ductal carcinoma in situ. J Clin Oncol. 2016;34(33):3963–8. https://doi.org/10.1200/JCO.2016.67.8532.
Schmitz R, Wilthagen EA, van Duijnhoven F, van Oirsouw M, Verschuur E, Lynch T, et al. Prediction models and decision aids for women with ductal carcinoma in situ: a systematic literature review. Cancers (Basel). 2022;14(13). https://doi.org/10.3390/cancers14133259.
Zeuner R, Frosch DL, Kuzemchak MD, Politi MC. Physicians' perceptions of shared decision-making behaviours: a qualitative study demonstrating the continued chasm between aspirations and clinical practice. Health Expect. 2015;18(6):2465–76. https://doi.org/10.1111/hex.12216.
Lee CN, Chang Y, Adimorah N, Belkora JK, Moy B, Partridge AH, et al. Decision making about surgery for early-stage breast cancer. J Am Coll Surg. 2012;214(1):1–10. https://doi.org/10.1016/j.jamcollsurg.2011.09.017.
Greenup RA, Rushing C, Fish L, Campbell BM, Tolnitch L, Hyslop T, et al. Financial costs and burden related to decisions for breast cancer surgery. J Oncol Pract. 2019;15(8):e666–e76. https://doi.org/10.1200/JOP.18.00796.
Lawhon VM, England RE, Wallace AS, Williams CP, Williams BR, Niranjan SJ, et al. It’s important to me: a qualitative analysis on shared decision-making and patient preferences in older adults with early-stage breast cancer. Psychooncology. 2021;30(2):167–75. https://doi.org/10.1002/pon.5545.
Angarita FA, Elmi M, Zhang Y, Look Hong NJ. Patient-reported factors influencing the treatment decision-making process of older women with non-metastatic breast cancer: a systematic review of qualitative evidence. Breast Cancer Res Treat. 2018;171(3):545–64. https://doi.org/10.1007/s10549-018-4865-0.
Hamelinck VC, Bastiaannet E, Pieterse AH, Jannink I, van de Velde CJ, Liefers GJ, et al. Patients' preferences for surgical and adjuvant systemic treatment in early breast cancer: a systematic review. Cancer Treat Rev. 2014;40(8):1005–18. https://doi.org/10.1016/j.ctrv.2014.06.007.
Chapman BM, Yang JC, Gonzalez JM, Havrilesky L, Reed SD, Hwang ES. Patient preferences for outcomes following DCIS management strategies: a discrete choice experiment. JCO Oncol Pract. 2021;17(11):e1639–e48. https://doi.org/10.1200/OP.20.00614.
Fridman I, Chan L, Thomas J, Fish LJ, Falkovic M, Brioux J, et al. A web-based personalized decision support tool for patients diagnosed with ductal carcinoma in situ: development, content evaluation, and usability testing. Breast Cancer Res Treat. 2022;192(3):517–27. https://doi.org/10.1007/s10549-022-06512-8.
Juraskova I, Butow P, Bonner C, Bell ML, Smith AB, Seccombe M, et al. Improving decision making about clinical trial participation - a randomised controlled trial of a decision aid for women considering participation in the IBIS-II breast cancer prevention trial. Br J Cancer. 2014;111(1):1-7. https://doi.org/10.1038/bjc.2014.144.
Ozanne EM, Schneider KH, Soeteman D, Stout N, Schrag D, Fordis M, et al. OnlineDeCISion.org: a web-based decision aid for DCIS treatment. Breast Cancer Res Treat. 2015;154(1):181–90. https://doi.org/10.1007/s10549-015-3605-y.
Stacey D, Bennett CL, Barry MJ, Col NF, Eden KB, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;10:CD001431. https://doi.org/10.1002/14651858.CD001431.pub3.
Vromans R, Tenfelde K, Pauws S, van Eenbergen M, Mares-Engelberts I, Velikova G, et al. Assessing the quality and communicative aspects of patient decision aids for early-stage breast cancer treatment: a systematic review. Breast Cancer Res Treat. 2019;178(1):1–15. https://doi.org/10.1007/s10549-019-05351-4.
Wang EH, Gross CP, Tilburt JC, Yu JB, Nguyen PL, Smaldone MC, et al. Shared decision making and use of decision AIDS for localized prostate cancer : perceptions from radiation oncologists and urologists. JAMA Intern Med. 2015;175(5):792–9. https://doi.org/10.1001/jamainternmed.2015.63.
Elwyn G, Rix A, Holt T, Jones D. Why do clinicians not refer patients to online decision support tools? Interviews with front line clinics in the NHS. BMJ Open. 2012;2(6). https://doi.org/10.1136/bmjopen-2012-001530.
O’Brien MA, Charles C, Lovrics P, Wright FC, Whelan T, Simunovic M, et al. Enablers and barriers to using patient decision aids in early stage breast cancer consultations: a qualitative study of surgeons’ views. Implement Sci. 2014;9:174. https://doi.org/10.1186/s13012-014-0174-0.
Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: a systematic review. Patient Educ Couns. 2015;98(9):1046–57. https://doi.org/10.1016/j.pec.2015.05.004.
Covvey JR, Kamal KM, Gorse EE, Mehta Z, Dhumal T, Heidari E, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer. 2019;27(5):1613–37. https://doi.org/10.1007/s00520-019-04675-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors ALN, SW, and SM declare no conflicts of interest. ESH has research support from R01 CA185138-01; U2C CA-17-035 Pre-Cancer Atlas (PCA) Research Centers; DOD BC132057; BCRF 19-074; PRECISION CRUK Grand Challenge (E.S.H.).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nash, A.L., Wang, S., McDuff, S. et al. De-escalation in DCIS Care. Curr Breast Cancer Rep 15, 58–68 (2023). https://doi.org/10.1007/s12609-023-00475-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-023-00475-5