Abstract
Purpose of Review
When patients are diagnosed with breast cancer, they are often interested to know as much about their disease as possible. At the same time, treating physicians want to determine prognosis and management. This article reviews imaging and pathology findings for the various invasive ductal carcinoma (IDC).
Recent Findings
This review describes the spectrum of imaging and pathologic findings of IDC, including subtypes, to guide determining radiological-pathological concordance and next steps of management.
Summary
While there are some imaging features highly suspicious for IDC, there is significant overlap with benign entities. This review focuses on the important differences between IDC subtypes and benign entities and when this affects management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Invasive ductal carcinoma (IDC) is the most common type of breast cancer and accounts for approximately 80% of breast cancer diagnoses [1,2,3]. Then invasive lobular carcinoma (ILC) accounts for about 1 of 10 invasive breast cancers. The subtypes of invasive carcinoma are rare with each subtype making up fewer than 5% of the invasive breast cancers. This paper details the imaging and pathology findings for the various invasive mammary carcinoma special subtypes.
Although the pathologic and radiological aspects of special subtypes of IDC have been well-described in the literature, they are reported mostly as case report or case studies. These special cases are important to understand because sometimes they are difficult to diagnose by imaging alone and on core needle biopsy, requiring waiting until excision for final diagnosis. Diagnosis provides information for prognosis and treatment plan. The earlier classification was based on the histological morphology. Current molecular tests have demonstrated that breast cancers clusters into distinct biologic subsets according to their gene expression patterns. The molecular classification predicts the prognosis more accurately and helps to manage the individual patients according to the individual tumor gene profile.
We performed a literature review that was supplemented by an internal review of our pathology database at UTMB. Review of representative cases for subtypes of invasive mammary carcinoma at the University of Texas Medical Branch (UTMB) from 2017 to 2020 revealed invasive ductal carcinoma (IDC), no special type (NST), tubular carcinoma, mucinous carcinoma, micropapillary carcinoma, medullary carcinoma, neuroendocrine carcinoma, apocrine carcinoma, cribriform carcinoma, adenoid cystic carcinoma, and metaplastic carcinoma including squamous cell carcinoma, osteoid differentiation, chondroid differentiation, and spindle cell carcinoma. The purpose of this study is to review the mammographic, sonographic, and MRI findings of specific types of invasive mammary carcinoma and to correlate the radiologic features with clinical and histopathologic findings.
Invasive Breast Cancer, No Special Type (NST)
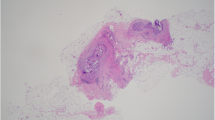
IDC no special type (NST), previously known as IDC not otherwise specified (NOS), is the most common type of IDC accounting for about 40–75% of all invasive breast cancers [4]. It is a diagnosis of exclusion, which means that for the diagnosis to be made, all the other specific types must be ruled out [5]. IDC NST typically presents as a hyperdense mass with irregular shape and spiculated margins on mammogram [6]. In our data set for patients with IDC NST, most had the typical presentation other than one with architectural distortion and another with diffuse skin thickening on mammogram. IDC NST typically presents as a hypoechoic irregular mass with angular margins on ultrasound [6]. This was the ultrasound presentation for all our patients except for the patient with subtle architectural distortion and the patient with diffuse skin thickening on mammogram. Ultrasound for the latter two patients demonstrated no sonographic abnormality within the breast. The typical MRI features of IDC NST are an irregular mass with irregular margins and iso to hypointense to parenchyma on T2-weighted images with rapid wash in and rapid wash out kinetics [6]. All our patients with IDC NST demonstrated the typical MRI features. On pathology, IDC NST usually presents with a wide scope of morphological variation and clinical behaviors, such as tumor size, grade, relative proportion of tumor cell and stroma, and types of margins [4]. Heterogenous growth patterns, including diffuse sheets, nests, cords, or singly distributed cells with variable amount of ductal differentiation is seen with IDC NST. The ductal differentiation amount ranges from more than 70% of tumor tissue to complete absence [4]. Tumor cells are pleomorphic and usually have prominent nucleoli and numerous mitoses. Sixty percent of cases demonstrate areas of necrosis and calcification [4]. Sometimes foci of squamous metaplasia, apocrine metaplasia, or clear cell changes are present. The amount of stroma is variable, ranging from none to abundant (Fig. 1).
Tubular Carcinoma
Tubular carcinoma of the breast is a slow-growing cancer that metastasizes infrequently and accounts for approximately 1 to 2% of invasive breast cancers [7,8,9,10]. The rates of these entities are generally very wide because there is a race/ethnicity-based gap in the incidence and distribution of breast cancer subtypes [11]. Tubular carcinoma typically presents as a small spiculated mass on mammogram and an irregular mass with posterior acoustic shadowing on ultrasound [12•]. Two of our cases presented as small irregular masses with spiculated margins, while the other two cases presented as 0.9 cm of grouped amorphous calcifications and 3 cm of scattered amorphous calcifications. Most tubular carcinomas can be identified on sonography as hypoechoic masses with ill-defined margins and posterior acoustic shadowing [13]. On breast MRI, tubular carcinomas can be described as hyperintense breast carcinomas with or without dark internal septation like appearance on T2-weighted images [14]. Low ADC values from DW imaging can be used to differentiate tubular carcinoma from hyperintense benign breast lesions [14]. Histologically, the characteristic feature of tubular carcinoma is the predominance of tubules with angulated shapes, arranged haphazardly in a desmoplastic stroma. The tubules are composed of a single layer of epithelial cells without surrounding myoepithelial cells. Pure tubular carcinoma (greater than 90% characteristic morphology of tubular carcinoma) has limited metastatic potential and excellent prognosis. Management for tubular carcinoma is usually complete excision with hormonal therapy. Chemotherapy and radiation therapy do not improve disease-free survival or overall survival and therefore are rarely administered (Fig. 2).
Mucinous Carcinoma
Mucinous carcinoma accounts for 1 to 7% of all breast carcinomas [15]. A mass on mammography and a hypoechoic lesion with heterogeneous internal echo on sonography is the most common appearance of mucinous breast carcinoma [16•]. For the 46 cases of mucinous carcinoma reported by Liu et al., a palpable mass was present in 40 cases (87.0%) [16•]. Mammogram demonstrated well-defined margins for thirty-one (61.3%) cases of pure mucinous type and two (33.3%) of mixed mucinous carcinoma [16•]. On ultrasound, 76.5% lesions of pure type and 71.4% lesions of mixed type demonstrated a heterogeneous internal echo [16•]. The typical MRI findings of pure mucinous carcinoma include a circumscribed mass with extremely high-signal intensity on T2-weighted imaging and benign-appearing kinetics with gradual and persistent enhancement [17]. Higher-grade or mixed mucinous lesions might have more suspicious imaging features. Mucinous carcinomas show variable signal intensity on fat-saturated T1-weighted MR images, depending on the differences in protein composition of the tumor, and are homogeneously or heterogeneously hyperintense on fat-saturated T2-weighted images, which correlates with the large mucinous component at histologic examination. After contrast agent administration, most mucinous carcinomas gradually and progressively enhance, often with a rim of heterogeneous enhancement. At UTMB, we identified two cases of mucinous carcinoma over the specified time period. Both of our cases demonstrated an irregular mass on mammogram and heterogenous echogenicity on ultrasound, consistent with the literature. Histologically, mucinous carcinoma demonstrates small clusters of tumor cells floating in acellular mucin. The carcinoma can be pure mucinous or mixed mucinous depending on the percentage of the mucinous component. Pure mucinous carcinomas (mucin component > 90%) are associated with a better prognosis. Mixed mucinous carcinoma (> 10% nonmucinous areas) has prognosis dependent on nonmucinous component (Fig. 3) [18].
Micropapillary Carcinoma
Micropapillary carcinoma is an aggressive subtype and accounts for 2 to 8% of all breast carcinoma. It has a high early recurrence rate and decreased survival that typically occur during the sixth decade of life [19, 25, 26]. Lymphatic invasion and axillary lymph node metastases are very common [19,20,21,22,23, 24••]. The most common finding on mammogram is an irregular spiculated mass [27•]. The most common finding on ultrasound is an irregular hypoechoic mass with spiculated margins and posterior acoustic shadowing [27•]. The most common finding on MRI is an irregular mass with washout kinetics [27•]. At UTMB, we identified two cases of micropapillary carcinoma over the specified time period. Both of our patients presented for diagnostic workup of a palpable abnormality. The imaging for both our patients demonstrated an irregular mass, consistent with the description in prior literature. For the mass that was over 3 cm, there was also a morphologically abnormal lymph node. The mass under 1 cm did not demonstrate axillary lymphadenopathy. Histologically, invasive micropapillary carcinoma show distinctive architecture, characterized by tufts of tumor cells arranged in morule like clusters devoid of fibrovascular cores and surrounded by empty clear spaces. They display an inside-out arrangement, with the luminal aspect of the cell present on the outer surface of the cluster (Fig. 4).
Medullary Carcinoma
Medullary carcinoma accounts for less than 5% of all invasive breast cancers [28]. Among breast cancers arising in BRCA-1 carriers, about 13% are medullary carcinoma. Mammogram demonstrates a mass with rounded, oval, or lobulated shape with a well-defined tumor border [29••]. Ultrasound similarly shows a well-circumscribed hypoechoic mass [29••]. MRI features include a round, oval, or lobular mass with a smooth margin with either homogenous or heterogeneous internal enhancement with delayed peripheral enhancement [30,31,32]. These MRI features are not specific for medullary carcinoma and can be found in other histologic types of breast cancers as well as in benign lesions [30, 31]. At UTMB, we identified one case of medullary carcinoma over the specified time period. Our case of medullary carcinoma did not present with well-defined smooth margin on mammogram and on ultrasound presented as a complex solid and cystic mass rather than a hypoechoic mass. The WHO recommends using the term carcinomas with medullary features rather than medullary carcinoma or atypical medullary carcinoma. The histological features include syncytial growth pattern, pushing borders, prominent lymphoplasmacytic infiltrate, and majority of the cases are triple negative for ER/PR/Her2. Strictly defined medullary carcinoma is reported to have a better prognosis than stage-matched triple-negative breast cancer. However, medullary carcinoma can be a controversial entity in that adherence to the criteria for diagnosis has been variable across studies and institutions, which can be misleading given it is an otherwise high-grade triple-negative breast carcinoma. Many expert breast pathologists prefer to avoid this terminology in reporting practices for these reasons (Fig. 5).
Carcinoma with Neuroendocrine Features
Primary neuroendocrine carcinoma of the breast accounts has been reported to range from less than 1–5% of invasive breast cancers, according to the different series and the different diagnostic criteria [33]. Park et al.’s review of 87 patients with neuroendocrine carcinoma of the breast showed palpable mass (55.8%) as a common clinical manifestation [34••]. Mammogram showed a high-density, round or oval, or lobular mass with nonspiculated margins [34••]. Ultrasound showed an irregular (65.4%), hypoechoic (78.4%) mass, with indistinct margins (43.5%), and no or enhanced posterior acoustic features (77.9%). MRI showed an irregular mass (83.3%), irregular margins (63.6%), and washout kinetics (85.7%) [34••]. At UTMB, we identified one case of carcinoma with neuroendocrine features over the specified time period. Our patient had clinical and imaging presentation similar to the description in the literature. The diagnostic imaging workup for the patient’s palpable mass revealed an irregular mass with spiculated margins on mammogram and angular margins on ultrasound.
According to 2012 WHO Classification of Tumor of the Breast, carcinomas with neuroendocrine features are subclassified into 3 groups: well-differentiated neuroendocrine tumor (WD-NET), poorly differentiated neuroendocrine carcinoma (PD-NEC), or small cell carcinoma, and invasive breast carcinoma with neuroendocrine differentiation (IBC-NED), which is a breast carcinoma of special or no special type that demonstrates neuroendocrine differentiation by immunohistochemistry [35]. Well-differentiated NETs of the breast consist of solid nests and trabeculae of tumor cells. The tumor cells can be spindled, plasmacytoid, or polygonal and are separated by thin fibrovascular septa. The chromatin ranges from evenly distributed with inconspicuous nucleoli to hyperchromatic or vesicular with prominent nucleoli. The diagnosis of NET requires expression of neuroendocrine markers. The most sensitive and specific immunohistochemical markers are synaptophysin and chromogranin A (Fig. 6).
Apocrine Carcinoma
Invasive apocrine carcinoma (IAC) of the breast is a rare subtype of breast cancer and accounts for less than 1 to 4% of breast carcinomas [36]. It is difficult to differentiate IAC from other subtypes of invasive mammary carcinoma by radiologic appearance alone as the findings are non-specific [37, 38]. Most mammographic findings of IAC demonstrate microcalcification [38]. A case of IAC demonstrating an oval circumscribed hyperdense mass with microcalcification on mammogram was reported by Onoue et al. [39]. A case of IAC showing an irregular shaped IAC with microcalcification was reported by Gokalp et al. [37]. Out of the five case reports by Seo et al., one case demonstrated an irregular, partly indistinct hyperdense mass, while another presented as an asymmetry [40]. IAC shows variable sonographic appearances including irregular shapes, non-circumscribed solid mass with heterogeneous internal echo pattern according to several previous case reports [37, 40]. All five cases reported by Seo et al. showed irregular solid masses with heterogeneous internal echo patterns and noncircumscribed margins [40]. On breast MRI, it typically presents as an enhancing mass with fast enhancement and delayed washout pattern [39]. There was variability in the imaging findings for our four cases of apocrine carcinoma. There were two cases detected on screening mammogram as subcentimeter irregular masses, one detected on screening mammogram as architectural distortion and the other detected on diagnostic mammogram as a large palpable oval mass. Grossly, apocrine carcinoma is indistinguishable from conventional invasive ductal carcinoma. Histologically, invasive apocrine carcinoma is characterized by apocrine morphology with abundant eosinophilic and granular cytoplasm, distinct cell borders, and centrally or eccentrically located nuclei with prominent nucleoli. Apocrine carcinoma has a characteristic hormonal receptor profile that is negative for estrogen receptor-alpha (ER) and progesterone receptor (PR) and is positive for androgen receptor (AR). Her-2/neu overexpression and amplification are present in approximately 30% of tumors. Apocrine carcinoma has similar or slightly better prognosis as invasive ductal carcinoma (Fig. 7).
Cribriform Carcinoma
Invasive cribriform carcinoma (ICC) of the breast is a rare subtype and accounts for 1 to 3% of invasive breast carcinoma with lower frequency of axillary nodal metastases and thus a favorable prognosis [41•]. The imaging features are nonspecific with mammogram showing irregular shape (72.8%), spiculated margins (63.7%), and a high density (81.8%) mass. Ultrasound demonstrates irregular shape (77.8%), spiculated margins (29.6%), hypoechogenicity (81.5%), and no posterior acoustic features (85.2%). MRI demonstrates an irregular shaped mass (62.0%) and irregular (42.9%) margins. Our case of cribriform carcinoma did show an irregular mass on imaging. Despite only being subcentimeter in size, axillary lymphadenopathy was also found in this patient. ICC is generally divided into three forms by histological features. Pure (> 90% cribriform pattern), classical (< 90% and > 50% cribriform pattern, mixed with < 50% tubular carcinoma), and mixed form (< 90% and > 50% cribriform pattern, mixed with 10–49% non-tubular carcinoma). Histologically, tumor cells in ICC are arranged as cribriform islands. Most IDD show excellent prognosis. Pure ICC (> 90% cribriform pattern) has better prognosis than mixed ICC (Fig. 8).
Metaplastic Carcinoma
Metaplastic breast carcinomas represent 0.25–1% of invasive breast cancers [42]. It is a heterogenous group of tumors composed of adenocarcinoma with metaplastic elements. These can include squamous cell, spindle cell (sarcomatoid), osteoid, chondroid, or lipomatous components [43••], and the predominant pattern of differentiation defines its additional subtypes, described in more detail below. In addition, metaplastic carcinoma can contain varying amounts of invasive carcinoma of no special type (NST) or be comprised entirely of the metaplastic component. The mammographic, sonographic, and MRI imaging characteristics of metaplastic breast carcinomas can be similar to invasive ductal carcinoma as well as benign lesion, thus preventing complete differentiation of such tumors on imaging [44].
On breast MRI, metaplastic breast carcinomas present as a round or oval-shaped mass, often with gentle lobulations, and frequently with circumscribed margins, and generally isointense or hypointense, similar to other histologic types of invasive breast carcinoma [45, 46]. High-signal intensity on T2-weighted images due to necrotic component and cystic degeneration is a frequent finding. High signal on T2-weighted images is also observed in mucinous carcinoma, invasive ductal carcinoma with infarction or necrosis, encapsulated papillary carcinoma, and invasive papillary carcinoma, in addition to metaplastic breast carcinoma [47, 48]. The reported enhancement characteristics of these lesions include heterogeneous, rim-like, or containing nonenhancing internal components. The frequently reported kinetic pattern is early enhancement and a delayed washout corresponding to the enhancing peripheral portion and nonenhancing internal components [45, 46].
Majority of metaplastic carcinomas are triple (ER, PR, Her2) negative. Therefore, extensive immunostaining panels of cytokeratin (AE1/AE3, Cam5.2, CK5/6, 34βE12) need to be performed to demonstrate the evidence of origin as epithelial malignancy. Metastases may preferentially be via blood vessels. Lymph node metastases are less frequent.
Squamous Cell Carcinoma
Metaplastic squamous cell carcinoma (SCC) represents less than 0.1% of invasive breast cancer cases [42]. The clinical presentation and imaging findings for our patients are consistent with the description in the literature. The common clinical presentation is a rapidly growing, relatively large breast mass without nodal involvement [43••, 49••]. The mass is typically very dense with calcifications infrequently on mammogram [30, 49••]. Squamous cell carcinoma is round or lobular with well-circumscribed or microlobulated margins on ultrasound [30]. Heterogeneous echogenicity with cystic components from necrosis and cystic degeneration may be seen within the mass [30, 49••]. Histologically, metaplastic squamous cell carcinoma is composed of tumor cells with squamous differentiation. Other components can be observed such as spindle cells, osteocytes, and chondrocytes. For diagnosis of primary SCC of the breast, the following three criteria must be fulfilled: absence of an associated primary SCC in a second site, the absence of skin involvement, and the SCC that predominates by more than 90% (Fig. 9) [50].
Osteoid Differentiation
The prevalence of breast cancer with osseous/cartilaginous metaplasia is very rare that estimated to occur in only 0.003–0.12% of invasive breast cancer cases [51]. Metaplastic carcinoma with osteoid differentiation is expected to present as a calcified breast mass on imaging. The differential diagnosis for a calcified breast mass includes primary osteosarcoma and osteoid [52]. Osteosarcoma typically presents as a densely calcified ivorylike mass at mammography [53]. Primary osteosarcoma, as well as other sarcomas, of the breast is extremely rare. Malignant neoplasms of the breast with osseous differentiation are considered components of metaplastic carcinoma or heterologous components of malignant phyllodes tumors until proven otherwise [54]. Our patient presented with a palpable mass with oval shape and indistinct margins with subtle associated amorphous and punctate calcifications. Histologically, metaplastic carcinoma with mesenchymal differentiation may demonstrate admixture of osseous and cartilaginous differentiation. Identification of the presence of a carcinomatous (epithelial) component is important in navigating the differential diagnosis (Fig. 10).
Chondroid Differentiation
Metaplastic carcinoma with chondroid differentiation (MCCD), again very rare, estimated to occur in only 0.003–0.12% of invasive breast cancer cases has nonspecific findings on mammography, sonography, and MRI [51]. It may present as an indistinct high-density mass with amorphous or coarse calcifications on mammography and a relatively circumscribed complex echoic mass with posterior enhancement on sonography [55]. MRI may show a relatively circumscribed mass with a nonenhancing T2 intermediate-to-high-signal-intensity internal component on MRI [51]. Our two patients presented with equal to high-density irregular masses, one larger at presentation with coarse calcifications and the other smaller with amorphous calcifications. Histologically, breast carcinoma with mesenchymal differentiation may demonstrate combinations of mesenchymal elements. Metaplastic chondroid carcinoma usually comprised a malignant lesion with neoplastic epithelial cells admixed with areas of chondroid differentiation (Fig. 11).
Spindle Cell Carcinoma
Spindle cell carcinoma (sometimes referred to as sarcomatoid carcinoma) is a subgroup of metaplastic carcinoma [56]. Spindle cell carcinoma typically presents as a palpable breast mass at a mean age of 61 years, more commonly among African American and Hispanic women [57]. Mammogram typically shows a round or lobulated mass, with up to 25% containing pleomorphic or linear calcifications and overlying skin thickening in 13% of cases [58••]. Common features include speculations and architectural distortion of the surrounding tissue [59]. Ultrasound typically shows a heterogeneous round mass with indistinct margins, internal vascularity, and posterior acoustic shadowing, with or without cystic areas [60]. It is uncommon to have calcifications and axillary lymph node involvement [61]. MRI of metaplastic carcinoma demonstrates irregular spiculated mass with decreased T1 signal intensity, increased T2 signal intensity, and variable enhancement [59, 61]. Our case of spindle cell carcinoma matched the clinical presentation and imaging findings reported in the literature, presenting as a large palpable irregular mass. Histologically, spindle cell carcinoma is characterized by atypical spindle cells which can have multiple architectural patterns, typically arranged in wavy, interlacing, or fascicular pattern. The differential diagnoses include primary or metastatic sarcoma (rare), phyllodes tumor, nodular fasciitis, metastatic melanoma, scar, fibromatosis, myofibroblastoma, pseudoangiomatous stromal hyperplasia (PASH), etc. The presence of carcinomatous component and immunostaining are helpful in making the diagnosis (Fig. 12).
Adenoid Cystic Carcinoma
Less than 0.1% of invasive breast cancers are adenoid cystic carcinoma (AdCC) [62]. This type of cancer is most common in salivary glands but can also present rarely as a primary tumor in the breast since the breast is also an exocrine gland. This rare subtype does not typically metastasize to axillary lymph nodes and thus has a good overall prognosis [63•]. A smooth or irregular mass or asymmetric density is the typical mammographic appearance [63•]. A heterogeneous or hypoechoic, irregular mass is the typical sonographic appearance [64]. The MRI appearance described by two case reports is a benign-appearing, circumscribed mass without washout kinetics [63•]. The mammogram and ultrasound for our patient with AdCC demonstrated an irregular mass as described in previous literature. Histologically, AdCC usually consists of well-circumscribed tumor nodules with an infiltrative pattern at the peripheral border. Histologically, the tumor demonstrates many growth patterns, including tubular, cribriform, trabecular solid, and basaloid. There are dual population of cells (ductal epithelial cells and myoepithelial cells/basaloid cells) and two types of lumens. Luminal-type cells form solid nests or small tubules with true luminal spaces that appear empty. Myoepithelial-type cells surround basement membrane-like material which are described as pseudolumina. Immunostains are positive for ductal components, myoepithelial components, and CD117 (c-kit). MYB overexpression is sensitive but nonspecific marker for AdCC. Grading of breast adenoid cystic carcinoma is similar to the salivary gland counterpart (Grade I: no solid elements; Grade II: < 30% solid elements; Grade III: > 30% solid elements). Some studies showed that the presence but not the percentage of solid growth is an independent predictor for adverse outcome (Fig. 13).
Conclusion
Invasive breast cancer could be divided into many subtypes. Invasive breast carcinoma of no special type (NST) is a diagnosis of exclusion, which means that for the diagnosis to be made, all the other specific types must be ruled out.
Some of these special types may have a better prognosis than the conventional invasive ductal carcinoma, such as tubular carcinoma, mucinous carcinoma, and adenoid cystic carcinoma. Medullary carcinoma may have a better prognosis than stage-matched triple negative breast ductal cancer; however, it is a problematic and often controversial diagnosis. Other subtypes may have the same or worse prognoses than invasive ductal carcinoma, NST, such as metaplastic carcinoma (including spindle cell carcinoma and squamous cell carcinoma), and micropapillary carcinoma.
Review of the cases demonstrated imaging findings that match descriptions in prior literature for the most part. However, interesting imaging findings include two tubular carcinoma cases that presented as calcifications, variable presentation for our four apocrine carcinoma cases, a complex solid and cystic mass for our medullary carcinoma case, metastatic lymphadenopathy in our cribriform carcinoma case, and wide variability in our eight cases of invasive carcinoma of no special type.
The imaging and pathology findings of these rare subtypes have some recurring features. Nevertheless, imaging findings do overlap among the subtypes, so radiologic-pathologic correlation is required to make the accurate diagnosis which helps to predict prognosis and personalized treatment plan.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Dillon DA, Guidi AJ, Schnitt SJ. Ch. 25: Pathology of invasive breast cancer. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the Breast. 5th ed. Philadelphia: Lippincott-Williams & Wilkins; 2014.
Henry NL, Shah PD, Haider I, Freer PE, Jagsi R, Sabel MS. Chapter 88: Cancer of the breast. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, editors. Abeloff’s Clinical Oncology. 6th ed. Philadelphia: Elsevier; 2020.
Jagsi R, King TA, Lehman C, Morrow M, Harris JR, Burstein HJ. Chapter 79: Malignant tumors of the breast. In: DeVita VT, Lawrence TS, Lawrence TS, Rosenberg SA, editors. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2019.
Makki J. Diversity of breast carcinoma: histological subtypes and clinical relevance. Clin Med Insights Pathol. 2015;8:23–31. https://doi.org/10.4137/CPath.S31563 Published 2015 Dec 21.
Sinn HP, Kreipe H. A brief overview of the WHO Classification of Breast Tumors, 4th Edition, Focusing on Issues and Updates from the 3rd Edition. Breast Care (Basel, Switzerland). 2013;8(2):149–54. https://doi.org/10.1159/000350774.
Niknejad MT, Skandhan AKP, et al. Invasive ductal carcinoma. https://radiopaedia.org/articles/invasive-ductal-carcinoma?lang=us. Accessed 28 June 2021
Mitnick JS, Gianutsos R, Pollack AH, et al. Tubular carcinoma of the breast: sensitivity of diagnostic techniques and correlation with histopathology. AJR. 1999;172:319–23.
Sheppard DG, Whitman GJ, Fornage BD, et al. Tubular carcinoma of the breast: mammographic and sonographic features. AJR. 2000;174:253–7.
Leibman AJ, Lewis M, Kruse B. Tubular carcinoma of the breast: mammographic appearance. AJR. 1993;160:263–5.
Limaiem F, Mlika M. Tubular breast carcinoma. [Updated 2020 Oct 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542223/.
Kong X, Liu Z, Cheng R, et al. Variation in breast cancer subtype incidence and distribution by race/ethnicity in the United States from 2010 to 2015. JAMA Netw Open. 2020;3(10): e2020303. https://doi.org/10.1001/jamanetworkopen.2020.20303.
Günhan-Bilgen Işil, Oktay Ayşenur. Tubular carcinoma of the breast: mammographic, sonographic, clinical and pathologic findings. Eur J Radiol. 2007;61(1):158–62. This study retrospectively reviewed 32 invasive tubular carcinoma cases. Invasive tubular carcinoma is seen as a small spiculated mass on mammography, and as an irregular mass with posterior acoustic shadowing.
Sheppard DG, Whitman GJ, Fornage BD, Stelling CB, Huynh PT, Sahin AA. Tubular carcinoma of the breast. Am J Roentgenol. 2000;174(1):253–7.
Yilmaz R, Bayramoğlu Z, Emirikçi S, Önder S, Salmaslıoğlu A, Dursun M, Acunaş G, Özmen V. MR Imaging features of tubular carcinoma: preliminary experience in twelve masses. Eur J Breast Health. 2018;14(1):39–45. https://doi.org/10.5152/ejbh.2017.3543.PMID:29322118;PMCID:PMC5758062.
Toikkanen S, Kujari H. Pure and mixed mucinous carcinomas of the breast: a clinicopathologic analysis of 61 cases with long-term follow-up. Hum Pathol. 1989;20:758–64.
Liu Haiquan, Tan Hongna, Cheng Yufan, et al. Imaging findings in mucinous breast carcinoma and correlating factors. Eur J Radiol. 2011;80(3):706–12. This study investigated the radiologically features of pure mucinous type and mixed mucinous carcinoma of breast. Radiologically, mucinous carcinoma demonstrates as a mass on mammography and a hypoechoic lesion with heterogeneous internal echo on sonography. There was no correlation found between sonographic findings and histological types.
Bitencourt AGV, Graziano L, Osório CABT, Guatelli CS, Souza JA, Mendonça MHS, Marques EF. MRI features of mucinous cancer of the breast: correlation with pathologic findings and other imaging methods. Am J Roentgenol. 2016;206(2):238–46.
Li CI. Risk of mortality by histologic type of breast cancer in the United States. Horm Cancer. 2010;1:156–65.
Luna-Moré S, Gonzalez B, Acedo C, Rodrigo I, Luna C. Invasive micropapillary carcinoma of the breast: a new special type of invasive mammary carcinoma. Pathol Res Pract. 1994;190:668–74.
Middleton LP, Tressera F, Sobel ME, et al. Infiltrating micropapillary carcinoma of the breast. Mod Pathol. 1999;12:499–504.
Nassar H, Wallis T, Andea A, Dey J, Adsay V, Visscher D. Clinicopathologic analysis of invasive micropapillary differentiation in breast carcinoma. Mod Pathol. 2001;14:836–41.
Siriaunkgul S, Tavassoli FA. Invasive micropapillary carcinoma of the breast. Mod Pathol. 1993;6:660–2.
Walsh MM, Bleiweiss IJ. Invasive micropapillary carcinoma of the breast: eighty cases of an under-recognized entity. Hum Pathol. 2001;32:583–9.
Kim MJ, Gong G, Joo HJ, Ahn SH, Ro JY. Immunohistochemical and clinicopathologic characteristics of invasive ductal carcinoma of breast with micropapillary carcinoma component. Arch Pathol Lab Med. 2005;129:1277–82. This study reviewed 38 invasive micropapillary carcinoma cases compared with 217 cases of invasive carcinoma without micropapillary component. The results of this study showed that invasive micropapillary carcinoma are associated with larger tumor size, more frequent lymphovascular invasion and nodal metastases, and higher stage.
Kuroda H, Sakamoto G, Ohnisi K, Itoyama S. Clinical and pathologic features of invasive micropapillary carcinoma. Breast Cancer. 2004;11:169–74.
Tresserra F, Grases PJ, Fábregas R, Férnandez-Cid A, Dexeus S. Invasive micropapillary carcinoma: distinct features of a poorly recognized variant of breast carcinoma. Eur J Gynaecol Oncol. 1999;20:205–8.
Jones KN, Guimaraes LS, Reynolds CA, et al. Invasive micropapillary carcinoma of the breast: imaging features with clinical and pathologic correlation. Am J Roentgenol. 2013;200:689–95. https://doi.org/10.2214/AJR.12.8512. This study reviewed 41 cases with invasive micropapillary carcinoma feature. The most common radiological findings are irregular mass on mammography, and irregular hypoechoic mass with spiculated margins and posterior acoustic shadowing on sonography. MRI reveals irregular mass with washout kinetics, or diffuse heterogeneous non-mass like enhancement.
Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363(20):1938–48.
Meyer JE, Amin E, Lindfors KK, Lipman JC, Stomper PC, Genest D. Medullary carcinoma of the breast: mammographic and US appearance. Radiology. 1989;170(1 Pt 1):79–82. The radiological features were reviewed in a total of 24 medullary carcinoma of breast cases. On mammography, tumors appear as round or oval, noncalcified massed. Sonography demonstrates well-defined masses with an inhomogeneous, hypoechoic texture.
Yoo JL, Woo OH, Kim YK, Cho KR, Yong HS, Seo BK, Kim A, Kang EY. Can MR imaging contribute in characterizing well-circumscribed breast carcinomas? Radiographics. 2010;30(6):1689–702.
Tominaga J, Hama H, Kimura N, Takahashi S. MR imaging of medullary carcinoma of the breast. Eur J Radiol. 2009;70(3):525–9.
Jeong SJ, Lim HS, Lee JS, Park MH, Yoon JH, Park JG, Kang HK. Medullary carcinoma of the breast: MRI findings. AJR Am J Roentgenol. 2012;198(5):W482–7.
Inno A, Bogina G, Turazza M, et al. Neuroendocrine carcinoma of the breast: current evidence and future perspectives. Oncologist. 2016;21(1):28–32. https://doi.org/10.1634/theoncologist.2015-0309.
Park Y M, Yun W, Wei W, Yang W T. Primary neuroendocrine carcinoma of the breast: clinical, imaging, and histologic features. Am J Roentgenol. 2014;203:W221–30. https://doi.org/10.2214/AJR.13.10749. The radiological findings were retrospectively reviewed in 84 cases with primary neuroendocrine breast carcinoma (NEC). In comparison to those non-specific type invasive mammary carcinoma, breast NEC more frequently demonstrates as high density, round or oval, or lobular mass with non-spiculated margins on mammography, and an irregular hypoechoic mass with indistinct margins, no or enhanced posterior acoustic features on sonograms. MRI reveals an irregular mass with irregular margins and washout kinetics.
Bussolati G, Badve S. Carcinomas with neuroendocrine features. In: Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van der Vijver MJ, editors. WHO classification of tumours of the breast. Lyon, France: IARC Press; 2012:62–63. World Health Organization Classification of Tumours; vol 4.
Kim Ji Min, Kim Shin Young, MeeHye Oh, et al. A rare case of invasive apocrine carcinoma of the breast with unusual radiologic findings. Iran J Radiol. 2016;13(3):e35298.
Gokalp G, Topal U, Haholu A, Kizilkaya E. Apocrine carcinoma of the breast: mammography and ultrasound findings. European Journal of Radiology Extra. 2006;60(2):55–9.
Gilles R, Lesnik A, Guinebretiere JM, Tardivon A, Masselot J, Contesso G, et al. Apocrine carcinoma: clinical and mammographic features. Radiology. 1994;190(2):495–7. https://doi.org/10.1148/radiology.190.2.8284405.
Woo O, Kim A, Cho K, Seo B, Kang E. Apocrine carcinoma of the breast: clinical presentations, multimodality imaging findings and pathologic correlation. Cancer Res. 2009;69(2 Supplement):4029. https://doi.org/10.1158/0008-5472.SABCS-4029.
Seo KJ, An YY, Whang IY, Chang ED, Kang BJ, Kim SH, et al. Sonography of invasive apocrine carcinoma of the breast in five cases. Korean J Radiol. 2015;16(5):1006–11. https://doi.org/10.3348/kjr.2015.16.5.1006.
Lee YJ, Choi BB, Suh KS. Invasive cribriform carcinoma of the breast: mammographic, sonographic, MRI, and 18 F-FDG PET-CT features. Acta Radiol. 2015;56(6):644–51. https://doi.org/10.1177/0284185114538425. This study reviewed 28 cases of invasive cribriform carcinoma. The most common radiological findings are irregular shape mass, spiculated margin, some with pleomorphic calcifications. These features are highly suggestive of malignancy, but are not distinguishable from invasive breast carcinoma of no special type.
Grenier J, Soria JC, Mathieu MC, et al. Differential immunohistochemical and biological profile of squamous cell carcinoma of the breast. Anticancer Res. 2007;27(1B):547–55.
PezziCM P-P, ColeK FrankoJ, KlimbergVS BlandK. Characteristics and treatment of metaplastic breast cancer: analysis of 892 cases from the National Cancer Data Base. Ann Surg Oncol. 2007;14(1):166–73. This review examined a total of 892 patients with metaplastic carcinoma reported to the National Cancer Database from 2001 to 2003. The data demonstrated that metaplastic breast carcinoma is a rare tumor with larger size, less nodal involvement, higher tumor grade, and negative hormone receptors.
Kim Hyun Jeong, Kim Shin Young, Huh Sun. Multimodality imaging findings of metaplastic breast carcinomas. Ultrasound Q. 2018;34(2):88–93. https://doi.org/10.1097/RUQ.0000000000000340.
Chang YW, Lee MH, Kwon KH, et al. Magnetic resonance imaging of metaplastic carcinoma of the breast: sonographic and pathologic correlation. Acta Radiol. 2004;45:18–22.
Choi BB, Shu KS. Metaplastic carcinoma of the breast: multimodality imaging and histopathologic assessment. Acta Radiol. 2012;53:5–11.
Velasco M, Santamaría G, Ganau S, et al. MRI of metaplastic carcinoma of the breast. AJR Am J Roentgenol. 2005;184:1274–8.
Ryckman EM, Murphy TJ, Meschter SC, et al. AIRP best cases in radiologic-pathologic correlation: metaplastic squamous cell carcinoma of the breast. Radiographics. 2013;33:2019–24.
Günhan-Bilgen I, Memiş A, Ustün EE, Zekioglu O, Ozdemir N. Metaplastic carcinoma of the breast: clinical, mammographic, and sonographic findings with histopathologic correlation. AJR Am J Roentgenol. 2002;178(6):1421–5. This retrospective study investigated mammographic and sonographic findings of breast metaplastic carcinoma and correlated the radiologic features with histopathologic findings. Clinically, metaplastic breast cancer manifests as rapid growing palpable mass. Complex echogenicity with solid and cystic components may be seen on sonography and is related to necrosis and cystic degeneration seen histologically.
Behranwala KA, Nasiri N, Abdullah N, Trott PA, Gui GP. Squamous cell carcinoma of the breast: clinico-pathologic implications and outcome. Eur J Surg Oncol. 2003;29:386–9.
Esbah O, Turkoz FP, Turker I, Durnali A, Ekinci AS, Bal O, et al. Metaplastic breast carcinoma: case series and review of the literature. Asian Pac J Cancer Prev. 2012;13:4645–9.
Dekkers Ilona A, Cleven Arjen, Lamb Hildo J, Kroon Herman M. AIRP best cases in radiologic-pathologic correlation: primary osteosarcoma of the breast. RadioGraphics. 2019;39(3):626–9. https://doi.org/10.1148/rg.2019180181.
Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma—clinical, imaging, pathologic, and differential considerations. Skeletal Radiol. 1993;22(7):485–500.
Hicks DG, Lester SC. In Diagnostic Pathology: Breast (Second Edition), 2016.
Hee Jung Shin, Hak Hee Kim, Sun Mi Kim, et al. Imaging features of metaplastic carcinoma with chondroid differentiation of the breast. Am J Roentgenol. 2007;188:691–696. https://doi.org/10.2214/AJR.05.0831.
Wargotz ES, Deos PH, Norris HJ. Metaplastic carcinomas of the breast. Part II. Spindle cell carcinoma. Hum Pathol. 1989;20:732–40.
Taliaferro AS, Fein-Zachary V, Venkataraman S, et al. Imaging features of spindle cell breast lesions. Am J Roentgenol. 2017;209:454–64. https://doi.org/10.2214/AJR.16.17610.
Yang WT, Hennessy B, Broglio K, et al. Imaging differences in metaplastic and invasive ductal carcinomas of the breast. AJR. 2007;189:1288–93. This study compared the imaging features of metaplastic carcinoma with those of invasive breast carcinoma of no special type. They found that metaplastic carcinoma shows round or oval shape with circumscribed margins, while the invasive breast carcinoma of no special type demonstrates irregular shape, spiculated margins, segmentally distributed calcifications, and posterior acoustic shadowing.
Leddy R, Irshad A, Rumboldt T, Cluver A, Campbell A, Ackerman S. Review of metaplastic carcinoma of the breast: imaging findings and pathologic features. J Clin Imaging Sci. 2012;2:21.
Günhan-Bilgen I, Memiş A, Üstün EE, Zekioglu O, Özdemir N. Metaplastic carcinoma of the breast: clinical, mammographic, and sonographic findings with histopathologic correlation. AJR. 2002;178:1421–5.
Velasco M, Santamaría G, Ganau S, et al. MRI of metaplastic carcinoma of the breast. AJR. 2005;184:1274–8.
Rosen PP. Adenoid cystic carcinoma of the breast: a morphologically heterogeneous neoplasm. Pathol Annu 1989;24:237–254
Glazebrook KN, Reynolds C, Smith RL, et al. Adenoid cystic carcinoma of the breast. Am J Roentgenol. 2010;194:1391–6. https://doi.org/10.2214/AJR.09.3545. This paper retrospectively reviewed 11 cases of adenoid cystic carcinoma. Tumors show asymmetric densities or irregular masses on the mammography, and appear as irregular, heterogeneous, or hypoechoic masses with minimal vascularity on sonography. Tumor enhancement by MRI better delineated some cases which show subtle findings on sonography. MRI shows irregular or spiculated mass or suspicious enhancement kinetics.
Santamaría G, Velasco M, Zanón G, et al. Adenoid cystic carcinoma of the breast: mammographic appearance and pathologic correlation. AJR. 1998;171:1679–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Best Practice Approaches Breast Radiology-Pathology Correlation and Management
Rights and permissions
About this article
Cite this article
Nguyen, Q.D., He, J. Invasive Ductal Carcinoma NST and Special Subtypes: Radiology-Pathology Correlation. Curr Breast Cancer Rep 13, 347–364 (2021). https://doi.org/10.1007/s12609-021-00436-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-021-00436-w