Abstract
Purpose of Review
Oncoplastic surgery is a form of breast conservation surgery that involves volume displacement and replacement techniques to reconstruct the breast after a partial mastectomy. We aimed to report our clinical experiences with support from the literature as to the optimal application of oncoplastic surgery with regard to patient and disease selection and presentation, and discuss common technical considerations.
Recent Findings
Based on clinical experience and recent literature, oncoplastic surgery has several oncologic and reconstructive strengths including a decreased positive margin rate, high patient satisfaction, and additional benefit when applied to patients with both breast cancer and symptomatic macromastia.
Summary
Oncoplastic surgery constitutes an additional breast conservation option that is safe, well tolerated, and can provide autologous reconstruction after a large oncologic resection in a one-staged surgical effort that adds value for the appropriate breast cancer patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oncoplastic surgery is a form of breast conservation surgery [1, 2]. Its fundamental definition includes an oncologic resection with a partial mastectomy, ipsilateral reconstruction using volume displacement, or volume replacement techniques with possible contralateral symmetry surgery when appropriate [1, 3, 4]. In the realm of surgical options in breast surgery, its place lies in between the minimalistic approach of the standard lumpectomy and the maximalist approach of the mastectomy [5]. In providing the breast surgeon with another breast conservation option, the interest in oncoplastic surgery in the USA has been increasing [6], and there has been more than a doubling in the rate of oncoplastic surgeries performed over the last decade [7]. The goal of this paper is to provide an evidence-based response to address the following questions: (1) What patient population is appropriate for oncoplastic surgery? (2) What are the benefits of oncoplastic surgery? (3) What are the basic technical considerations, approaches, and associated common complications in oncoplastic surgery? (4) Does oncoplastic surgery provide value as a breast surgery option?
Methods
For each of the above questions, the authors provide an answer supported by peer-reviewed published evidence. Additionally, the answer can often come from clinical practice experience. If at any time there is a lack of evidence, this will be declared noting that the recommendation is based on anecdotal personal experience only. The clinical experience is based on a 3-year (2015–2018) single-institution oncoplastic surgery database using various forms of oncoplastic breast conservation techniques in 100 consecutive patients with breast cancer. Institutional review board approval was obtained in using this database.
Results
Oncoplastic Surgery Classification
Table 1 presents a commonly accepted approach for classifying oncoplastic procedures according to the amount of breast tissue that must be removed, rearranged, or replaced [1]. This classification system groups Level 1 volume displacement oncoplastic surgery into operations that correct for less than 20% breast volume defects and Level 2 volume displacement oncoplastic surgery into operations that correct for breast volume defects 20 to 50%. Lastly, for the more uncommon breast volume defects of greater than 50%, this classification system recommends the use of volume replacement techniques using local-regional flaps or implants.
What Patient Population Is Appropriate for Oncoplastic Surgery?
Given that oncoplastic surgery is a form of breast conservation, an eligible breast cancer patient cannot have contraindications to breast conservation and fundamentally needs to be open to the option of breast conservation. A history of prior breast radiation and other contraindications to adjuvant radiation are absolute contraindications for oncoplastic surgery. Likewise, inflammatory breast cancer is an absolute contraindication for oncoplastic surgery. Similarly, tumor volume burden relative to breast volume is another contraindication. By this, if a tumor involves the majority of the breast, a patient will likely be served better with a mastectomy and reconstruction when appropriate. Expanding on this reasoning, a breast cancer patient needs to have at least moderately sized breasts or at least Grade 2 ptosis to allow the surgeon to be able to use forms of tissue rearrangement common in oncoplastic surgery. It is extremely difficult to perform most types of oncoplastic surgery in women with small breasts and minimal nipple ptosis. Therefore, a breast cancer patient who wants and is eligible for breast conservation has moderate- to large-sized breasts (relative to tumor burden) or Grade 2 or 3 nipple ptosis should be provided the option for oncoplastic surgery. Possibly the greatest benefit from oncoplastic surgery is seen in those patients with both symptomatic macromastia and breast cancer. These patients have chronic back pain, neck pain, shoulder pain, bra strap indentation and grooving, and inframammary crease rashes in addition to their diagnosis of breast cancer. Performing a Level 2 volume displacement oncoplastic operation using reduction mammaplasty techniques to both remove large quantities of breast tissue result in lower positive margins and symptomatically happier patients [8••, 9•]. Lastly, those patients who have smaller breasts with minimal ptosis and relatively larger breast cancers who would prefer oncoplastic breast conservation options would be eligible for volume replacement options that include either local-regional flap options (such as the thoracodorsal artery perforator flap option) or implants [10,11,12].
What Are the Benefits of Oncoplastic Surgery?
There are several benefits of oncoplastic surgery when applied to the appropriate breast cancer patient. These benefits are best divided into oncologic and reconstructive outcomes.
Oncologic Benefits
One of the most important benefits that oncoplastic surgery provides is its ability to reduce positive margin rates compared to standard partial mastectomy. This makes common sense since the ability to remove larger areas of tissue (especially in Level 2 volume displacement designs using reduction mammaplasty techniques) allows for the entire removal of cancer relative to when removing smaller sections of breast tissue as seen in standard partial mastectomy. This logic has been shown to be true in the shaved margin literature where Chagpar et al. reduced their positive margin rate by half by removing more tissue with shaved margins [13]. Their positive margin rate, at best, after shaved margins was 19%. This was markedly less than their previous 38% positive margin rate in standard partial mastectomy operations. In general, standard partial mastectomy operations have a positive margin rate in the literature ranging between 20 and 40% [13]. While there is variation in oncoplastic positive margin rates in the literature, there is little doubt that there is a true reduction in positive margin rates compared to standard partial mastectomy [14]. Two large meta-analyses have shown that oncoplastic surgery has a positive margin rate between 10 and 12% [8, 15•]. Losken et al. noted that this lower positive margin rate held true in both Level 1 and Level 2 oncoplastic operations compared to standard partial mastectomy [15•]. In the author’s clinical experience, a similar lower positive margin rate of 6% was noted with oncoplastic surgery in the first 100 consecutive operations performed using Level 2 volume displacement oncoplastic surgery techniques (Table 2). During patient counseling, this was one of the most important decision-making factors that patients favor when choosing oncoplastic surgery. To them, it reduces the chances of a second operation for additional surgery whether that entails an additional shaved margin or a completion mastectomy. It allows them to continue on their cancer treatment journey and decreases the likelihood of a delay in adjuvant treatment in the setting of positive margins.
Reconstructive Benefits
In general, the reconstructive outcome in oncoplastic surgery involves autologous tissue most often from the ipsilateral remaining breast in a one stage reconstructive effort. In Level 2 volume displacement (involving reduction mammaplasty or mastopexy designs) or volume replacement operations, a symmetry contralateral breast operation is also performed. Oncoplastic reconstruction that is performed immediately after the large partial mastectomy resection have fewer post-operative complications than delayed efforts, and has the obvious benefit of requiring one surgery with immediate reconstruction rather than an obligatory two staged operation, at minimum, when choosing a delayed approach [16, 17]. From a reconstructive standpoint, a well-performed oncoplastic operation provides one of the most pleasing esthetic outcomes when using patient-reported outcome measures [9•, 18]. Oncoplastic reconstructive options are often utilized in subsequent operations when standard partial mastectomy efforts result in poor cosmesis which can happen as often as 28% of the time [19]. Patients feel that their oncoplastic reconstructive result provides at least the same or better results from a psychosocial perspective more than 50% of the time when compared to their pre-operative state, and these oncoplastic outcomes are reliably superior when compared to mastectomy operations with immediate reconstruction [9•]. Again, from the author’s clinical experience, these outcomes hold true and make sense since the oncoplastic reconstructions, especially using Level 2 volume displacement options, utilize esthetic mastopexy or reduction mammaplasty designs resulting in a less ptotic, cosmetically appealing breast form (Fig. 1). Aside from esthetic advantages, when applying oncoplastic techniques to a patient suffering from symptomatic macromastia, the advantages of the reconstructive effort increase exponentially. As noted earlier, symptomatic macromastia inherently is associated with back pain, neck pain, and shoulder pain among other chronic ailments, and when using a reduction mammaplasty (Level 2 volume displacement) design to remove the cancer and reconstruct the breast, a woman is likely freed of her macroscopic disease and of her macromastia symptoms. There is a large volume of literature touting the incredible value of reduction mammaplasty in macromastia patients [20, 21]. From clinical experience and common sense, the author has noted that patients suffering from both breast cancer and symptomatic macromastia receiving oncoplastic surgery are among the most satisfied breast cancer patients from a surgical outcome perspective (see Fig. 2).
Patient with large right upper outer quadrant breast cancer (pre-op: left photo) treated with a superomedial pedicle, inverted T skin incision oncoplastic surgery design (Level 2 volume displacement). Post-operatively at 6 months (right photo), successful oncologic resection and high patient satisfaction with the esthetic reconstructed breast form
Patient (pre-op: left photo) with large left upper outer quadrant breast cancer with symptomatic macromastia treated with an extended superomedial pedicle, inverted T skin incision oncoplastic surgery design (Level 2 volume displacement). Post-operatively 3 months after (right photo), pleased with successful oncologic resection and resolve of her symptomatic macromastia symptoms
What Are the Basic Technical Considerations, Approaches, and Associated Common Complications in Oncoplastic Surgery?
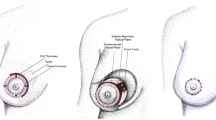
There are many approaches and techniques in oncoplastic surgery but one does not have to be a master of every technique to qualify as an able oncoplastic surgeon. Practically speaking, the approach depends on a three key factors: (1) How much tissue is being removed from the breast? (2) How large or ptotic is the breast (grades of breast ptosis are described in Table 3)? (3) Is the breast more glandular or fatty? The author tends to apply these questions to the oncoplastic classification scheme described by Clough et al. [1] (Table 1). Quite simply, if a breast that is moderately large at most and has Grade 1 or minimal Grade 2 ptosis is having less than 20% of the breast volume removed with a partial mastectomy, the Level 1 volume displacement oncoplastic operation is chosen. Typically, the author’s primary choice in this circumstance is a doughnut mastopexy design that can address any quadrant in the breast (Fig. 3). However, if the breast is predominantly fatty, then a Level 1 volume displacement oncoplastic design is not feasible as the approximating sutures will shred the fatty tissue. Additionally, if a doughnut mastopexy design is used in a Grade 3 ptotic or very large breast, then the cosmetic outcome will be suboptimal as this design does not adequately remove enough skin. If a breast is moderately to quite large and has Grade 2 or 3 ptosis and the volume of breast tissue to be removed is estimated to be 20 to 50% of the total breast volume, then a Level 2 volume displacement oncoplastic design is utilized. If the tumor is in the inferior pole, then a superomedial pedicle, inverted T (Wise) skin incision pattern is employed (Fig. 4). If the tumor is in the medial region of the breast, an inferior pedicle, inverted T (Wise) skin incision pattern is chosen (Fig. 5). Understanding when to use either the inferior or superomedial pedicle is essential as it allows the breast surgeon to address a cancer presentation in most regions of the breast. Additionally, given that the pedicles are typically de-epithelialized, the dermis left on the pedicle can be used to capture suture, thus allowing the pedicle to be transposed and fixed into the large partial mastectomy defects. This allows the use of Level 2 volume displacement oncoplastic techniques even in breasts that predominantly contain fatty tissue. The most common complication of the inverted T (Wise) skin incision pattern is wound healing where the inverted T junction dehisces [15•, 22]. Most of the time, this heals within 2 weeks with antibiotic ointment and dressing changes. Rarely, a skin graft has to be employed to cover this dehiscence. Lastly, if the more than 50% of the breast volume needs to be removed, then a volume replacement design is employed with either local-regional flaps or implants [11, 12]. With flaps, patients should be counseled about recipient and donor site complications that include scarring, seroma, and flap failure. With implants, the long-term risk of high-grade capsular contracture especially in the adjuvant setting of breast radiation is possible.
Does Oncoplastic Surgery Provide Value as a Breast Surgery Option?
With an ever cost-conscious health care system, any newer surgical technique or device should undergo rigorous value analysis. It is incumbent upon surgeons to be fair, yet skeptical, with their assessment regarding any new surgical paradigm that can add cost to the system as overall health care costs is a zero-sum game. Oncoplastic surgery does add direct cost to the system. There is additional surgical work being performed on the cancer side in addition to the contralateral breast for symmetry when appropriate. With this work comes costs and additional surgical risks for complications that can add further costs. In such, there is potential for the overuse of oncoplastic surgery in situations when a simple partial mastectomy alone would be appropriate. A small cancer in an older woman with smaller breasts and multiple co-morbidities can certainly be an example of when a partial mastectomy alone may be an optimal choice. Alternatively, a middle-aged woman in reasonable health with symptomatic macromastia and a moderately large tumor who is interested in breast conservation would be an excellent candidate for oncoplastic surgery using a Level 2 volume displacement (breast reduction type) design. Fortunately, there have been both clinical effectiveness studies using patient-related outcomes [9•, 23] and value analysis studies through the use of cost-utility analysis that have underscored the value of oncoplastic surgery when applied to the appropriate breast cancer patient [24••, 25, 26].
Conclusion
Oncoplastic surgery is an excellent breast conservation treatment option when applied to the appropriate breast cancer patient. When the appropriate technique is performed, patients tend to be satisfied from a post-operative psychosocial perspective, pleased with how they look and delighted at the lower positive margin rates afforded by this type of operation. It is becoming an accepted, standard option in the treatment options for breast cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010;17(5):1375–91.
Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol. 2005;6(3):145–57.
Hu J, Rainsbury RM, Segaran A, Predescu O, Roy PG. Objective assessment of clinical, oncological and cosmetic outcomes following volume replacement in patients undergoing oncoplastic breast-conserving surgery: protocol for a systematic review. BMJ Open. 2018;8(7):e020859.
Losken A, Hart AM, Chatterjee A. Updated evidence on the oncoplastic approach to breast conservation therapy. Plast Reconstr Surg. 2017;140(5S Advances in Breast Reconstruction):14S–22S.
Rainsbury RM. Surgery insight: oncoplastic breast-conserving reconstruction—indications, benefits, choices and outcomes. Nat Rev Clin Oncol. 2007;4(11):657–64.
Chatterjee A, Gass J, Burke MB, Kopkash K, El-Tamer MB, Holmes DR, et al. Results from the American Society of Breast Surgeons Oncoplastic Surgery Committee 2017 survey: current practice and future directions. Ann Surg Oncol. 2018;25:2790–4.
Jonczyk MM, Jean J, Graham R, Chatterjee A. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat. 2018;1–8.
•• Cruz MLDL, Blankenship MSA, MPH, MS, Chatterjee MA, Geha MR, et al. Outcomes after oncoplastic breast-conserving surgery in breast cancer patients: a systematic literature review. 0(0):1–12. This review confirmed the oncologic safety of oncoplastic surgery in patients with T1-T2 disease by revealing high rates of overall survival and disease-free survival with low local recurrence, distant recurrence, positive margin rate, re-excision rate, conversion to mastectomy rate and complication rates.
• Kelsall JE, McCulley SJ, Brock L, Akerlund MTE, Macmillan RD. Comparing oncoplastic breast conserving surgery with mastectomy and immediate breast reconstruction: case-matched patient reported outcomes. J Plast Reconstr Aesthet Surg. This paper compared outcomes between women undergoing oncoplastic breast conserving surgery and those undergoing mastectomy and immediate reconstruction with regards to body image scale scores of psychosocial function and patient reported outcome measures for breast appearance and return to function. Better psychosocial and self-rated satisfaction with breast appearance was achieved for oncoplastic breast conserving surgery.
Chatterjee A. Long term effects of modern breast cancer surgery. Gland Surg. 2017.
Barnea Y, Friedman O, Arad E, Barsuk D, Menes T, Zaretski A, et al. An oncoplastic breast augmentation technique for immediate partial breast reconstruction following breast conservation. Plast Reconstr Surg. 2017;139(2):348e–57e.
Almasad JK, Salah B. Breast reconstruction by local flaps after conserving surgery for breast cancer: an added asset to oncoplastic techniques. Breast J. 2008;14(4):340–4.
Chagpar AB, Killelea BK, Tsangaris TN, Butler M, Stavris K, Li F, et al. A randomized, controlled trial of cavity shave margins in breast cancer. N Engl J Med. 2015;373(6):503–10.
Weber WP, Soysal SD, El-Tamer M, Sacchini V, Knauer M, Tausch C, et al. First international consensus conference on standardization of oncoplastic breast conserving surgery. Breast Cancer Res Treat. 2017;165(1):139–49.
• Losken A, Dugal CS, Styblo TM, Carlson GW. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg. 2014;72(2):145–9. This paper compared literature outcomes between BCT alone and BCT with the oncoplastic approach and found lower positive margin rate, reexcision rate, and local recurrence rate in the oncoplastic group. Satisfaction with the aesthetic outcome was also significantly higher in the oncoplastic group.
Patel KM, Hannan CM, Gatti ME, Nahabedian MY. A head-to-head comparison of quality of life and aesthetic outcomes following immediate, staged-immediate, and delayed oncoplastic reduction mammaplasty [outcomes article]. Plast Reconstr Surg. 2011;127(6):2167–75.
Roughton MC, Shenaq D, Jaskowiak N, Park JE, Song DH. Optimizing delivery of breast conservation therapy: a multidisciplinary approach to oncoplastic surgery. Ann Plast Surg. 2012;69(3):250–5.
Rezai M, Knispel S, Kellersmann S, Lax H, Kimmig R, Kern P. Systematization of oncoplastic surgery: selection of surgical techniques and patient-reported outcome in a cohort of 1,035 patients. Ann Surg Oncol. 2015;22(11):3730–7.
Wang HT, Barone CM, Steigelman MB, Kahlenberg M, Rousseau D, Berger J, et al. Aesthetic outcomes in breast conservation therapy. Aesthet Surg J. 2008;28(2):165–70.
Taylor AJ, Tate D, Brandberg Y, Blomqvist L. Cost-effectiveness of reduction mammaplasty. Int J Technol Assess Health Care. 2004;20(3):269–73.
Tykkä E, Räsänen P, Tukiainen E, Asko-Seljavaara S, Heikkilä A, Sintonen H, et al. Cost-utility of breast reduction surgery-a prospective study. J Plast Reconstr Aesthet Surg. 2010;63(1):87–92.
De La Cruz L, Blankenship SA, Chatterjee A, Geha R, Nocera N, Czerniecki BJ, et al. Outcomes after oncoplastic breast-conserving surgery in breast cancer patients: a systematic literature review. Ann Surg Oncol. 2016;23(10):3247–58.
Chand ND, Browne V, Paramanathan N, Peiris LJ, Laws SA, Rainsbury RM. Patient-reported outcomes are better after oncoplastic breast conservation than after mastectomy and autologous reconstruction. Plast Reconstr Surg Glob Open. 2017;5(7):e1419.
•• Asban A, Homsy C, Chen L, Fisher C, Losken A, Chatterjee A. A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with single stage implant reconstruction in the treatment of breast cancer. Breast. 2018;41:159–64. This paper investigated the cost-utility of large volume displacement oncoplastic surgery versus mastectomy with single stage implant reconstruction and found large volume displacement oncoplastic surgery to be cost-effective compared to mastectomy with single staged implant reconstruction.
Chatterjee A, Offodile AC II, Asban A, Minasian RA, Losken A, Graham R, et al. A cost-utility analysis comparing oncoplastic breast surgery to standard lumpectomy in large breasted women. Adv Breast Cancer Res. 2018;07(02):14.
Chatterjee A, Asban A, Chen L, Fisher C. Abstract 56. A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with free flap reconstruction in the treatment of breast cancer. Plast Reconstr Surg Glob Open. 2017;5(2 Suppl).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Abhishek Chatterjee, Mengdi Yao, Yurie Sekigami, Yuanxin Liang, and Salvatore Nardello declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Local-Regional Evaluation and Therapy
Rights and permissions
About this article
Cite this article
Chatterjee, A., Yao, M., Sekigami, Y. et al. Practical Perspectives Regarding Patient Selection and Technical Considerations in Oncoplastic Surgery. Curr Breast Cancer Rep 11, 35–42 (2019). https://doi.org/10.1007/s12609-019-0305-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-019-0305-3