Abstract
Purpose of Review
The majority of Central and Eastern European (CEE) countries report inferior breast cancer survival rates compared with Western European countries. We review limitations in access to screening programs, surgery, radiotherapy, pathology, palliative care, and antineoplastic medicines as potential explanations for these disparities.
Recent Findings
Most CEE countries do not have the quality and quantity of radiotherapy needed to adequately service the population. Surgical services are widely accessible, but sentinel node biopsy is not universally available. There are important limitations for CEE patients in accessing high-quality pathology. Many patients living with advanced cancer are in dire need of palliation services. Important inequalities exist in availability and patient costs, especially for newer, more expensive drugs, across Europe, while drug shortages affect several “essential,” old, and inexpensive drugs.
Summary
Improvements in radiotherapy, surgery, and pathology and access to medicines are needed, together with the provision of trained health care professionals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Central and Eastern European (CEE) countries represent the group of countries comprising Albania, Bulgaria, Croatia, the Czech Republic, former Yugoslavian countries, Hungary, Moldova, Poland, Romania, the Slovak Republic, and the three Baltic states: Estonia, Latvia, and Lithuania (Fig. 1).
Map of regions in Europe (available at http://mapofunitedstates.us/world-map-and-regions/world-map-and-regions-western-europe-region-map-noeyesneed-926-x-767-pixels/)
Due to their similar economic background in the post-communist system, these countries are usually analyzed together as they share common characteristics.
Disparities in cancer outcomes can be evaluated using key metrics such as cancer survival, which also reflects the effectiveness of health care systems. According to EUROCARE-5, cancer survival has improved across Europe, starting in 2000, due to access to enhanced diagnosis and treatment. However, important differences in breast cancer outcomes are still evident comparing CEE with the rest of the European Union (EU) [1]. With the exception of the Czech Republic, which has a 5-year survival rate of 78.0% (CI 77.3–78.7), the rest of CEE countries have a 5-year survival rate of 10–15% lower than the European mean (81.8%, 95% CI 81.6–82.0) [1].
According to the World Bank, the Czech Republic, Estonia, Hungary, Latvia, Lithuania, Poland, Slovenia, and Slovak Republic are high income countries (HIC). The rest of the countries in CCE region (Albania, Bulgaria, Serbia, Romania) are low- and middle-income countries (LMICs).
In the majority of CEE countries, increases in incidence for breast cancer were among the highest observed in the EU as a whole, while mortality decreased only modestly [2]. The causes of these disparities are undoubtedly multifactorial, including general population health and lifestyle, late stage at diagnosis, health system and cancer care infrastructure, lack of access to specific equipment such as radiotherapy and to trained oncology specialists, and last but not least, patient access and availability to cancer medication.
Other contributing factors include the absence of national cancer plans, late or incomplete implementation of screening programs, decentralization of cancer care, and poor access to standard care [3]. Certain issues are explained by the historical and geopolitical situation of the former “Eastern/Soviet Bloc” that led to geopolitical isolation for 5 decades, until the early 1990s when the Soviet-influenced governance fell apart in most CEE countries. Ten CEE countries are currently integrated into the 28-state EU economic and political systems (EU-28), including the EU health care system [3]. This has led to improvement and access for private health care in the context of social health insurance systems funded through employment-related premiums [3].
In 2015, the EU-28 mean on health spending per capita was 2781€/per person; the lowest rates were observed in Romania (816€), Latvia (1030€), Bulgaria (1108€), or Serbia (1049€) [4]. The majority of health spending across Eastern Europe is publicly financed on average costs and direct out-of-pocket payments account for approximately 15%, but direct out-of-pocket costs can represent a much greater share in some countries: Bulgaria (46%), Hungary (28%), Latvia (39%), Serbia (37%), or even half of it in Albania [4]. Furthermore, there is a substantial disparity when comparing health care costs for cancer per person versus health expenditure per capita in EU, the costs for cancer per person remain low in CEE countries, and the European mean percentage is represented only by 3%, ranging from 1.44% in Bulgaria, 2.57% in Romania, 3% in Czech Republic, and 3.63% in Slovenia.
Nevertheless, significantly limited health care resources that are present in certain environments pose unique challenges for the clinicians working in this area. Certain aspects of breast cancer management are unavailable, e.g., immunohistochemistry, which hence prohibits the use of standard guidelines. In this context, data presented in OECD Health Statistics 2016 have shown that since 2009, several countries including Hungary and Montenegro reduced the percentage of Gross Domestic Product (GDP) allocated to health care [4]. Unfortunately, in line with the EU directives, health care and its management represents a national responsibility. Guidelines and indicators are recommended, but are not mandatory, and the final decisions, approval, and implementation are at the discretion of each country’s national administration.
Because of lack of resources, clinicians are thus forced sometimes to make decisions against their best medical knowledge. For example, if targeted therapies such as trastuzumab are not available, oncologists are forced to provide suboptimal treatment. Confined by a limited budget, the clinician is obliged to become a manager of scarce resources. Nowadays, with the current trend of meaningful advances that come at a high cost, even traditionally “wealthy” systems struggle to cover the cost of cancer care, which is becoming unaffordable even in high-income countries using the current models of care delivery and financing [5].
Systems Data Regarding Comprehensive Breast Cancer Care
A substantial difficulty in assessing access to quality breast surgery and loco-regional and systematic care in the CEE is the paucity of prospectively collected health system and long-term cancer outcome data. In many CEE countries, registry data are often very limited, health information systems and reporting are weak, and long-term follow-up of patients in clinical and research context is suboptimal [6].
European cancer indicators are in the process of being developed. Professional societies like the European Society of Breast Cancer Specialists (EUSOMA) play an important role in developing quality indicators in breast cancer [7] and these recommendations are being followed on a voluntary basis in CEE. The quality indicators are also used by breast centers in order to qualify for a standardized audit and quality control in order to become certified as quality breast units. In 2006, the European Parliament adopted a resolution supported by EUSOMA and Europa Donna meant to ensure a nationwide provision of specialist breast units by 2016, since treatment in a specialist breast unit has been proven to raise chances of survival and to improve quality of life (European Parliament resolution on breast cancer in the enlarged European Union (RE/636089EN.doc) B6-0528/2006). As a consequence, the European Commission Initiative on Breast Cancer (ECIBC) is currently developing a European Quality Assurance Scheme for Breast Cancer Services, to establish common quality and safety requirements for breast cancer services throughout the EU that will constitute the basis for a voluntary accreditation scheme for breast units in the EU.
Access to Breast Cancer Screening
Cancer screening remains a major public health problem in Eastern Europe as late stage at presentations is still prevalent. Population-based screening programs, if organized properly, can be highly effective in reducing mortality and incidence for breast cancer [8]. Important differences regarding population participation can be observed across countries in CEE, irresponsive of charge for the screening program (Table 1).
In December 2003, the Council of the European Union proposed several recommendations for screening in EU countries, including the CEE region [8]. Out of the 28 member states, 25 were planning, piloting, or rolling out (ongoing or completed) population-based screening programs. Three member states (Bulgaria, Greece, and Slovakia) had only non-population-based programs. Romania had only a small-scale pilot or demonstration project ongoing so that the majority of the potential target population was subject to non-population-based activity. Bulgaria had implemented a pilot project to provide breast, cervical, and colorectal cancer screening using a population-based approach. The pilot project was completed in 2014 and at present the country has only a non-population-based screening program [8].
In contempt of the EU recommendations, participation rate for breast cancer screening for women aged 50–69 remains low, with a rate of 43.1% in Croatia, 66.3% in Estonia, 82% in Romania with the mention that screening is performed only at a small scale pilot in the North-West region of the country, or 82.5% in Slovenia (Table 1).
This is mainly due to lack of awareness of screening and utilization of clinical breast examination or breast awareness as an educational tool for the population. Low participation rates result in a high overdiagnosis rate, which translates into higher overall costs for the health care systems in CEE [8].
Future community efforts should emphasize the importance and integration of new preventive strategies into existing health care systems and programs, as an important percent of women in Eastern Europe still do not benefit from population-based screening programs (Table 1).
Access to Surgery in Eastern Europe
Many LMICs, including countries from CEE, have centralized cancer centers that provide all cancer surgical procedures. In contrast, there might be major shortages or no availability of even basic surgery in distant rural areas [6].
Patients with cancer, and specifically cancers that need surgical treatment such as breast cancer, face two principal types of costs: (1) direct costs associated with accessing treatment, including both the costs of surgery and the non-medical costs associated with accessing treatment; and (2) indirect costs as a result of lost productivity secondary to the illness itself and time and labor losses associated with seeking treatment [6]. Cancer exerts substantial economic effects not only at the household level but also at national, regional, and global levels, affecting economic, productivity, and growth in countries at all stages of development [12].
Sentinel lymph node biopsy is not universally available in many CEE countries though published data on coverage is lacking. A surgeon working in the second largest county in Croatia reported that out of 300 breast cancer-related surgeries performed in a year, no sentinel lymph node dissections were performed; in contrast, the procedure is available in another hospital performing 200 cases per year [13]. Few studies to assess this procedure have been reported from Hungary [14, 15] or Czech Republic [16].
Mastectomy rates in Eastern Europe are still above the breast conservative surgery rates. Efforts are being performed to present data on surgical practices and guidelines from CEE countries, but a number of studies are relatively small and underpowered [15, 17].
Finally, research on cancer surgery is not widely available in many CEE countries. The Lancet Oncology Commission on Global Cancer Surgery reported that only 1% of patients are enrolled in surgical clinical trials in the CEE region [6].
Access to Radiotherapy in Eastern Europe
Radiotherapy plays a critical and inseparable component of comprehensive cancer treatment and care and is an essential tool for effective treatment. Variable patterns of cancer presentation and limited information on the current proportion of patients receiving radiotherapy complicate needs assessment [18].
During the past 20 years, several investigators [19,17,21] have developed evidence-based [22] estimates of desirable radiotherapy use in clinical practice. Most CEE countries do not have the quality and quantity of radiotherapy needed for an adequate service to the population, with under capacity rates ranging from 20 to 70% (Fig. 2) [23].
Radiotherapy procedures are usually provided as in-patient procedures rather than out-patient, reflecting the Soviet-inspired culture of hospital-centered care [3]. Radiotherapy facilities need highly specialized staff, raising important challenges in training, recruitment, and retention of a suitable health workforce, in view of the high cost and time commitment of training assumed by the country versus the increasing mobility of the health workforce (e.g., skilled physicians, nurses, technicians, physicists) who could be attracted abroad [19]. In the last decade, a continuous migration towards Western countries of this highly specialized staff is a reality that hinders the provision of quality radiotherapy services in many CEE countries. Due to this lack of access to radiotherapy, health care professionals are sometimes reluctant to refer patients for the treatment when appropriate [19].
Maintaining effective routine radiotherapy operations is essential for continuous access, through costly maintenance contracts. Lack of funding for maintenance leads to periods of services not being provided, or in some cases, cessation of services as repairs might not be affordable [24].
Access to Pathology
Breast cancer care is crucially dependent on complete and accurate pathology to allow the multidisciplinary team to arrive to optimal treatment recommendations. However, staffing, training, and equipment limitations are obstacles in most LMICs including CEE countries [25]. Diagnostic pathology and immunohistochemistry are usually available in academic cancer centers from main cities in Eastern Europe, but in smaller centers these resources are frequently unavailable. Delays in pathology review are also common, and costs can be prohibitive [26]. Quality-assurance measures ensure optimum testing and confirm accuracy [25]. Even in high-resource settings, discordance rates between low-volume and high-volume laboratories can exceed 20% [27].
Testing for molecular makers which add value to standard clinical and pathological parameters has significantly impacted clinical practice in many cancer types. This is, in part, due to the considerable complexity of the cancer disease at the clinical, morphological, and molecular levels, and the development of targeted therapies.
There is a paucity of published data on molecular testing in CEE countries [28]. Molecular testing for targeted therapies such as anti-Her2 therapies for breast cancer (e.g., trastuzumab, lapatinib, pertuzumab, and TDM-1) or olaparib for BRCA-positive patients with ovarian and breast cancer, as well as other molecular alterations in lung or colorectal cancer has patchy availability in most of the CEE countries [28].
Significant barriers exist to proving high-quality molecular pathology to women with breast cancer in CEE countries: (1) there is no specific reimbursement for costly “pathology” testing including immunohistochemistry, as hospitals are reimbursed via DRG (disease related groups) system; (2) the regulatory authorities expect that if special testing is required to prescribe a medication, the cost of testing is to be supported by the pharmaceutical company; (3) most of the molecular testing (e.g., Her2, EGFR, ALK, BRAF, BRCA) is pharma-sponsored through a voucher system; (4) very few pathology labs have external quality assurance systems as the “payer,” mainly represented by pharmaceutical companies, does not usually require this. Some pathology labs lack quality assurance even for “traditional” techniques. The few laboratories that are offering “newer” techniques such as PCR or next-generation sequencing (NGS) are lacking patient volume and need to implement quality assurance programs, and (5) if a certain drug is not reimbursed, there are no mechanisms to finance the tests. Despite the potential conflict of interests, pharma funding at this moment represents the only solution for clinicians to provide access to molecular targeted therapies for their patients.
BRCA1/2 mutation testing is in the early phase of development in CEE countries. Although several reports are currently available on BRCA1/2 mutations in populations from different geographic areas in CEE [29, 30], the samples sizes are small, as there is a wide variability in access to genetic testing. These studies usually are the result of impressive efforts made by clinicians in this area to increase access for BRCA1/2 testing for their patients, by gathering financial support, mostly via national or international grants [29, 30]. Reimbursement of BRCA1/2 is not yet provided by national health systems in many countries; as PARP inhibitors are entering the therapeutic scene in breast cancer, testing is currently supported by pharmaceutical companies.
The yet-to-be-fulfilled promise of personalized medicine and the availability of multigene panel testing, often aggressively marketed towards the unsuspecting patient (who has to cover the cost), brings potential benefit but also challenges in the management of breast cancer patients. The complexities of multigene data management clearly require decision support tools. However, these tests are often ordered by the patient, and the results interpreted by medical oncologists with variable understanding of the field. The challenge ahead is how to incorporate these results into clinical practice, and how to provide patients with the best possible evidence-based care in limited-resource settings.
In conclusion, there are important limitations for CEE patients in accessing high-quality pathology, and testing for molecular alterations is not offered to all eligible patients. Multigene panel testing has become available in CEE countries, but costs must be covered by the patients, while experts needed for interpreting the results are lacking.
Access to Palliative and Supportive Care
There is a slow change of paradigm across CEE countries regarding the concept of palliative care, moving away from the old concept of terminal care towards integration of supportive and palliative care throughout the continuum of cancer care. However, limited resources, centralization of services, lack of patient-oriented information, limited registries, or absence or inadequate national cancer control plans leads to a situation in which many patients live with advanced cancer and are in dire need of palliation services.
According to a global survey in palliative care, only 14% of people who need palliative care receive it. The use of drugs for pain relief per capita in high-resource settings is about 1000 times that in low-resource settings, showing substantial deficits in access to basic and essential medicines [31].
In Romania, the role of palliative care has increased after recognition in 2003 of Hospice Casa Sperantei, the first Romanian hospice, as Beacon of Excellence in Eastern and Central Europe [31] following a study of 475 service providers in 28 countries in the region. Nowadays, Romania is recognized as a successful model in the process of legal adjustment and implementation of regulations concerning access to strong pain medication for cancer and non-cancer patients, and the model has been copied in the new Moldavian regulation [32]. However, important steps and investments are needed to generalize the successful examples to bring relief to all patients in need for palliation.
Access to Research
Research in Eastern Europe is influenced by political, economic, and scientific realities in CEE. Political instability combined with the global economic crisis brought a negative economic trend across CEE countries in the last decades, leading to a sustained migration of trained researchers towards Western Europe. Research is underrepresented in CEE, as local academic research is mainly covered by grants, or projects funded by programs of the Medical Science Academy, mainly in the field of experimental basic science, but clinical research (clinical trials phase II or III) is increasing mainly due to pharmaceutical companies interest in performing studies in this region. Due to access issues to newer medicines, Eastern Europe has a high recruitment potential and increasing experienced investigators.
Breast cancer clinical research, usually sponsored by industry, has been particularly successful [6]. According to the data on clinicaltrials.gov , several CEE countries have more than 100 clinical trials ongoing in breast cancer (Hungary, Greece) with the rest averaging between 50 and 100 ongoing studies (Romania, Czech Republic, Bulgaria). European countries that are not part of the EU have less access to clinical trials. This data has to be also interpreted in the context of demographic population, as smaller countries like Slovenia, Croatia, or Slovakia still conduct around 40 clinical trials in the field of breast cancer.
One important barrier for conducting clinical trials is the time between final protocol approval and inclusion of the first patient into randomized clinical trials. A study performed by Central European Cooperative Oncology Group showed that the average time interval from the moment of final protocol approval and the inclusion of the first patient was 18 months, and that most of the time was spent for regulatory procedures, i.e., approval from ethical review boards (9 months) or by relevant authorities (10 months). The “paper to patient” process required on average almost 19 months for 6 multicenter trials conducted by CECOG and the regulatory procedures used more than 50% of the duration of the whole process [10], as the European median is 52 days, range 0–151 days [33]. Optimization is urgently needed and a clear optimization is imperative in order to provide novel therapies available to patients more quickly [10].
There are several benefits for improving research and clinical trials access in Eastern Europe including: (1) improving information exchange from HIC to LMIC, (2) increase the sample size and population diversity of a clinical trial, (3) better understanding of evidence based medicine and cancer control plans, (4) improvement of infrastructure and medical expertise of the health system, and (5) increasing patients access to medicines through participation in clinical trials that otherwise would be inaccessible due to financial barriers [34].
Access to Antineoplastic Medicines
Advances in clinical research through the conduct of randomized clinical trials have added new therapeutic options for breast cancer patients leading to improved outcomes. However, innovation comes at a high cost, which currently exerts important pressure on health budgets. For most CEE countries, cancer health expenditure per person is significantly below the EU average (Table 1). Although EU members benefit from a unified mechanism of granting marketing authorization for medicines through the European Medicines Agency (EMA), reimbursement remains a national issue. Therefore, after EMA approval, each of the 28 EU countries has their own system of deciding reimbursement. Especially in CEE, where national health authorities struggle to provide best coverage within the limits of allocated funds, this leads to uneven access to medicines and important delays for patients in accessing newer, more expensive medications. One study showed delays of up to 10 years in certain CEE countries between EMA approval of trastuzumab and its reimbursement [35].
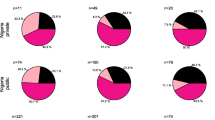
To map the issues related to medicine access across Europe and the world, the European Society of Medical Oncology (ESMO) conducted a series of surveys. The ESMO European Consortium Study [36, 37] subsequently reported on approval, reimbursement, and actual availability of cancer medicines used to treat the 13 most frequent solid tumors in European countries and the world. The information is a time-constrained “snapshot” of the situation in 2014 and is subject to change overtime, although the main conclusions still remain applicable in CEE countries. The ESMO survey data concludes that important inequalities exist in availability and patient costs, especially for newer, more expensive drugs, across Europe. According to the survey, with very few exceptions, most of the agents used in adjuvant management of early-stage breast cancer were subsidized and widely available in CEE. In 2015, the WHO Model List of Essential Medicines (EML) was updated to include an important number of antineoplastic medicines, among which is trastuzumab for early and metastatic breast cancer. Adjuvant trastuzumab was not subsidized in four CEE countries (Armenia, Georgia, Kyrgyzstan, and Uzbekistan) and is only available at full cost to patients in these countries. Reimbursement pre-approval was commonly requested for trastuzumab and other expensive agents, but this process rarely caused delays in therapy of > 4 weeks [36]. However, in the metastatic setting, other Her2-targeted agents, including pertuzumab, TDM-1, and lapatinib, were not reimbursed and only available at full cost for the patient in most CEE countries. Other newer medicines such as fulvestrant or everolimus were infrequently available for patients outside of Western Europe [36].
One of the most important yet unexpected conclusion of the ESMO survey showed that drug shortages affect several “essential,” old, and inexpensive drugs such as tamoxifen, 5-FU, or cisplatin (all on the WHO EML) [38]. In CEE, medicine shortages affect WHO EML medicines, with relevant therapeutic implications for many patients with breast cancer; it is unacceptable for patients to lack access to tamoxifen for several months in a row—which happened in a few countries in 2016.
One way of addressing the shortage problem in Eastern Europe of so-called financial toxicity for patients and health care systems could be the use and understanding of value-based cancer care. The term “value-based care” implies that the bold position must be taken to place an arbitrary limit of a “price on life” [39] to ensure patients continue to be able to receive life-saving cancer medications with greatest value [40, 39]. As described below, both ASCO and ESMO have developed frameworks—ASCO value-based framework and EMSO magnitude of clinical benefit scale (MCBS)—but they have yet to be adopted by CEE countries. An analysis of the Economist Intelligence Unit reported on causes of cancer medicine shortages across Europe and devised policy recommendations that can be applied at the national or regional level to prevent and manage shortages [41]. The issue of lack of access to newer, more expensive medicines highlights the struggle of many policy makers to accommodate progress within the limits of the allocated budget.
Guidelines
Resource-stratified guidelines can be an important tool to improve breast cancer care in resource-limited settings. Unfortunately, disparities remain regarding level of dissemination, implementation, and acceptance into routine practice in CEE. At this moment, it is unknown how LMICs will integrate the resource-stratified guidelines into clinical practice as there is lack of compliance in following guidelines. Barriers include lack of consensus about optimal management for common clinical cases, lack of applicability of recommendations, lack of outcome expectancy, inability to overcome the inertia of previous practice, patient behaviors or preferences, and logistical and financial barriers [42, 43].
From 2002 to 2013, the Breast Health Global Initiative (BHGI) developed a resource-stratified framework for breast cancer control across all resource settings and in 2005 presented the four-tier resource-stratification framework (basic, limited, enhanced, maximal) [42]. In 2017, the BHGI, in collaboration with the UICC and the NCI Center for Global Health, published 14 Knowledge Summaries for Comprehensive Breast Cancer Control, which summarizes content from the guidelines, to facilitate decision-making by policymakers, health care administrators, and advocates. NCCN has created their own resource-stratified framework for breast and other cancers [43, 44].
How to Improve Access When Resources Are Limited
Recent years have seen many medicines approved based on different endpoints with variable incremental benefit for the patient. The ESMO Magnitude of Clinical Benefit Scale (ESMO-MCBS) was designed to scale the benefit of new anticancer drug approved by EMA through a published, transparent process performed by a dedicated ESMO committee [45, 46]. Drugs which obtain the highest scores (A&B or 5&4) are included in the ESMO guidelines and highlighted as the highest priority for rapid reimbursement by national bodies across Europe. Other scales have also recently been proposed by various bodies (ASCO Value Framework, NCCN evidence blocks, Drug Abbacus, etc.). Despite using different approaches, there is a fair degree of agreement across the scales in highlighting that there is a weak concordance between the clinical benefit provided by a certain intervention and its price. A recent study found no correlation between the price of 37 anticancer drugs approved by FDA from 2000 to 2015 and the amount of clinical benefit provided, as evaluated by the ASCO Value Framework and the ESMO Magnitude of Benefit Scale [47].
Payment for cancer medicines is a budget decision for the health care system. Decisions must be made on objective and verifiable criteria where expenditures are compared to relevant alternative uses within and outside cancer care. Value-based payment requires development of sophisticated systems where payment is based on outcome in clinical practice. Unfortunately, financial management in CEE is impaired, and there is a very poor link between spending and outcome. Judicious spending is urgently needed in resource-limited settings such as CEE countries. It is clear that some CEE countries need more money allocated for (breast) cancer care, and this should be done using prioritization mechanisms such as the ESMO Magnitude of Clinical Benefit and stratified guidelines such as the BHGI guidelines [48] or the NCCN-stratified guidelines.
When deciding reimbursement of different medicines, policy makers often make decisions about supporting drugs in health systems based on erroneous or poorly understood data. Effect sizes and statistical significance are misused. It should be made clear that statistical significance does not equal clinical benefit, as underlined by the American Statistical Association: p values do not measure the size of an effect or the importance of a result. By itself, a p value does not provide evidence regarding a model or hypothesis; therefore, scientific conclusions and policy decisions should not be based only on p < 0.05 [49]. Moreover, there is substantial under-reporting of toxicity: studies have shown that 58% of potentially fatal adverse events are not in the initial FDA drug label, and 39% are not reported in any published randomized trial [31]. Toxicity is likely to be higher when new drugs are prescribed to general population as compared to the highly selected individuals included in clinical trials [49]. While FDA and EMA register drugs on the basis of p < 0.05, pharmaceutical companies will continue to perform large trials to detect small differences, sometimes with limited benefit for the patient.
Conclusions and Way Forward
There are important limitations across CEE in the availability and access to the multiple services required for the qualitative management of breast cancer patients, which lead to worse clinical outcomes in the region. There are many areas that need improvement. The overarching issue of chronic underfinancing by national health authorities of cancer expenditure is difficult to tackle; raising awareness among decision makers of the consequences of not investing in cancer care with the involvement of the civil society is critical to position cancer on the national agenda. Population education is dearly needed to decrease late presentation and uptake of the screening programs, where available. Awareness of both surgeons and patients on the benefits of minimizing surgery through breast conservation and sentinel node biopsy, together with investments for the needed equipment are keys to improve long-term quality of life of breast cancer patients. Increase of radiotherapy capacity is urgently needed in several CEE countries; the burden of the initial big financial investment is the main barrier. Access to essential, inexpensive medicines should be a health priority; adoption of preventive strategies to inform and take action to prevent medicine shortages is key to ensure continuity of quality care. Reimbursement of newer, more expensive medicines should be prioritized on the basis of the magnitude of benefit provided by the intervention. The current situation, where new therapies providing marginal benefit in highly selected patients are approved at high price, is neither desirable nor sustainable. Consideration of “clinical benefit” and “value” that includes quality and consistency of evidence for effectiveness, toxicity, and cost is welcome. Pressure should be put on registration agencies (FDA, EMA) to use a criterion of value for approval, rather than statistical significance of an outcome measure. We, as oncologists, should stop saying it is not our problem and act using these evidences to improve the outcome of our patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, Trama A, Visser O, Brenner H, et al. Cancer survival in Europe 1999–2007 by country and age: EUROCARE-5 2014;15(1):23–34. Doi: 10.1016/S1470-2045(13)70546-1.
Hery C, Ferlay J, Boniol M, Autier P. Quantification of changes in breast cancer incidence and mortality since 1990 in 35 countries with Caucasian-majority populations. Ann Oncol. 2008 Jun;19(6):1187–94. https://doi.org/10.1093/annonc/mdn025.
Esiashvili N. Radiation oncology in the developing economies of central and Eastern Europe. Semin Radiat Oncol. 2017;27(2):150–7. https://doi.org/10.1016/j.semradonc.2017.01.001.
https://www.oecd.org/els/health-systems/Health-at-a-Glance-Europe-2016-CHARTSET.pdf
Meropol NJ, Schrag D, Smith TJ, Mulvey TM, Langdon RM Jr, Blum D, et al. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27:3868–74. https://doi.org/10.1200/JCO.2009.23.1183.
Sullivan R, Alatise OI, Anderson BO, Audisio R, Autier P, Aggarwal A, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16(11):1193–224. https://doi.org/10.1016/S1470-2045(15)00223-5.
Biganzoli, et al. Quality indicators in breast cancer care: An update from the EUSOMA working group. Eur J Cancer. 2017;86:59–81.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R, et al. Economic burden of cancer across the European Union: a population-based cost analysis. RLancet Oncol. 2013 Nov;14(12):1165–74. https://doi.org/10.1016/S1470-2045(13)70442-X.
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–403. https://doi.org/10.1016/j.ejca.2012.12.027.; EUCAN national estimates (eco.iarc.fr/eucan).
European commission. Cancer screening in the European Union report on the implementation of the council recommendation on cancer screening. Reprint May 2017.
Ades F, Senterre C, Zardavas D, de Azambuja E, Popescu R, Parent F, et al. An exploratory analysis of the factors leading to delays in cancer drug reimbursement in the European Union: the trastuzumab case. Eur J Cancer. 2014 Dec;50(18):3089–97. https://doi.org/10.1016/j.ejca.2014.09.011.
Chaker L, Falla A, van der Lee SJ, et al. The global impact of non-communicable diseases on macro-economic productivity: a systematic review. Eur J Epidemiol. 2015;30:357–95. https://doi.org/10.1007/s10654-015-0026-5.
Josip Banovich. Breast specialized surgeon from KBC split, Krizine, Croatia. Personal communication.
Dare AJ, Anderson BO, Sullivan R, Pramesh CS, Yip CH, Ilbawi A, et al. Surgical services for cancer care. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, editors. Cancer volume, disease control priorities in developing countries. 3rd ed. Washington, DC: World Bank; 2015. http://dcp-3.org/chapter/1536/surgical-services-cancer-care.
Atun R, Jaffray DA, Barton MB, Bray F, Baumann M, Vikram B, et al. Expanding global access to radiotherapy. Lancet Oncol. 2015 Sep;16(10):1153–86. https://doi.org/10.1016/S1470-2045(15)00222-3.
Delaney G, Jacob S, Featherstone C, Barton M. The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104:1129–37.
Borras JM, Barton M, Grau C, Corral J, Verhoeven R, Lemmens V, et al. The impact of cancer incidence and stage on optimal utilization of radiotherapy: methodology of a population based analysis by the ESTRO-HERO project. Radiother Oncol. 2015;116:45–50. https://doi.org/10.1016/j.radonc.2015.04.021. published online May 19
Borras JM, Lievens Y, Dunscombe P, Coffey M, Malicki J, Corral J, et al. The optimal utilization proportion of external beam radiotherapy in European countries:an ESTRO-HERO analysis. Radiother Oncol. 2015;116:38–44. https://doi.org/10.1016/j.radonc.2015.04.018. published online May 14
Rosenblatt E, Izewska J, Anacak Y, Pynda Y, Scalliet P, Boniol M, et al. Radiotherapy capacity in European countries: an analysis of the Directory of Radiotherapy Centres (DIRAC) database. Lancet Oncol. 2013;14:e79–86. https://doi.org/10.1016/S1470-2045(12)70556-9.
Samiei M. Challenges of making radiotherapy accessible in developing countries. http://globalhealthdynamics.co.uk/cc2013/wp-content/uploads/2013/04/83-96-Samiei-varian-tpage-incld-Tpage_2012.pdf.
Anderson BO, Yip CH, Smith RA, Shyyan R, Sener SF, Eniu A, et al. Guideline implementation for breast healthcare in low- and middle-income countries: diagnosis resource allocation. Cancer. 2008;113(suppl):2257–68. https://doi.org/10.1002/cncr.23844.
Shyyan R, Masood S, Badwe RA, Errico KM, Liberman L, Ozmen V, et al. Breast cancer in limited-resource countries: diagnosis and pathology. Breast J. 2006;12(suppl 1):S27–37.
Soofi Y, Khoury T. Inter-institutional pathology consultation: the importance of breast pathology subspecialization in a setting of tertiary cancer center. Breast J. 2015;21:337–44. https://doi.org/10.1111/tbj.12420.
Negru S, Papadopoulou E, Apessos A, Stanculeanu DL, Ciuleanu E, Volovat C, et al. KRAS, NRAS and BRAF mutations in Greek and Romanian patients with colorectal cancer: a cohort study. BMJ Open. 2014;4:e004652. https://doi.org/10.1136/bmjopen-2013-004652.
Eniu A, Pop L, Stoian A, Dronca E, Matei R, Ligtenberg M, et al. Understanding BRCA1 and BRCA2 mutated breast cancer cases in Romania: first report on founder mutations in Romanians. Ann Oncol. 2017;Volume 28(suppl_5):mdx362.047. https://doi.org/10.1093/annonc/mdx362.047.
Connor SR, Bermedo MCS, editors. Global atlas of palliative care at the end of life. Geneva: World Health Organization; 2014. http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
Mosoiu D, Eniu A. Barriers towards establishing palliative care in Eastern Europe and prospects for improvement in the future: Romania as an example. In: Silberman M, editors. Palliative Care: Perspectives, Practices and Impact on Quality of Life, Nova Science Publishers, 2017, ISBN: 978-1-53612-084-4).
T. Brodowicz, I. Steiner, S. Beslija, T. E. Ciuleanu, M. Inbar, M. Krzakowski, Z. Kahan, V. et al, Time inclusion between final protocol approval and inclusion of the first patient into randomized clinical trials performed by the Central European Cooperative Oncology Group (CECOG): a 10 years experience, Journal of Clinical Oncology200927:15S, 6546–654621.1 Ramya Ramaswami, Eduardo Paulino, Adriana Barrichello, Angelica Nogueira-Rodrigues, Alexandra Bukowski, Jessica St. Louis, Paul E. Goss, Disparities in Breast, Lung, and Cervical Cancer Trials Worldwide, Journal of Global Oncology, no. 4 (May 2018) 1–11.https://doi.org/10.1200/JGO.17.00226.
Metzger-Filho O, de Azambuja E, Bradbury I, Saini KS, Bines J, Simon SD, et al. Analysis of regional timelines to set up a global phase III clinical trial in breast cancer: the adjuvant lapatinib and/or trastuzumab treatment optimization experience. Oncologist. 2013 Feb;18(2):134–40. https://doi.org/10.1634/theoncologist.2012-0342.
Ramaswami R, Paulino E, Barrichello A, Nogueira-Rodrigues A, Bukowski A, Louis JSt., Goss PE, Disparities in breast, lung, and cervical cancer trials worldwide. J Glob Oncol. 4:1–11. https://doi.org/10.1200/JGO.17.00226.
Cherny N, Sullivan R, Torode J, Saar M, Eniu A. ESMO European consortium study on the availability, out-of-pocket costs and accessibility of antineoplastic medicines in Europe. Ann Oncol. 2016 Aug;27(8):1423–43. https://doi.org/10.1093/annonc/mdw213.
Cherny NI, Sullivan R, Torode J, Saar M, Eniu A. ESMO international consortium study on the availability, out-of-pocket costs and accessibility of anti-neoplastic medicines in countries outside of Europe. Ann Oncol. 2017;28:2633–47. https://doi.org/10.1093/annonc/mdx521.
http://www.who.int/medicines/publications/essentialmedicines/en/
Cancer medicines shortages in Europe, Policy recommendations to prevent and manage shortages. Economist Intelligence Unit (EIU) Healthcare study. available at http://www.eiu.com/graphics/marketing/pdf/ESMO-Cancer-medicines-shortages.pdf (accessed 27 Apr 2018).
Cherny NI, Sullivan R, Dafni U, Kerst JM, Sobrero A, Zielinski C, et al. ESMO-magnitude of clinical benefit scale. Ann Oncol. 2015;26(8):1547–73. https://doi.org/10.1093/annonc/mdv249.
Anderson BO, Duggan C. Resource-stratified guidelines for cancer management: correction and commentary. J Glob Oncol. 2017;3:84–8.
World Health Organization: The seventieth world health assembly. Cancer prevention and control in the context of an integrated approach, in The seventieth world health assembly (ed): A70/a/CONF./9. Geneva, 2017.
Carlson RW, Scavone J, Koh W-J, et al: NCCN framework for resource stratification: a framework for providing and improving global quality oncology care. J Natl Compr Cancer Netw:in press, 2016.
Cherny NI, Dafni U, Bogaerts J, Latino NJ, Pentheroudakis G, Douillard JY, et al. ESMO-magnitude of clinical benefit scale version 1.1. Ann Oncol. 2017 Oct 1;28(10):2340–66. https://doi.org/10.1093/annonc/mdx310.
Vivot A, Jacot J, Zeitoun J-D, Ravaud P, Crequit P, Porcher R. Clinical benefit, price and approval characteristics of FDA-approved new drugs for treating advanced solid cancer, 2000–2015. Ann Oncol. https://doi.org/10.1093/annonc/mdx053.
Eniu A, Carlson RW, El Saghir NS, Bines J, Bese NS, Vorobiof D, et al. Breast health global initiative treatment panel. Guideline implementation for breast healthcare in low- and middle-income countries: treatment resource allocation. Cancer. 2008;113(8 Suppl):2269–81. https://doi.org/10.1002/cncr.23843.
Seruga B, Sterling L, Wang L, Tannock IF. Reporting of serious adverse drug reactions of targeted anticancer agents in pivotal phase III clinical trials. J Clin Oncol. 2011;29(2):174–85. https://doi.org/10.1200/JCO.2010.31.9624.
Wasserstein RL, Lazar NA. The ASA's statement on p-values: context, process, and purpose. Am Stat. 2016;70(2):129–33. https://doi.org/10.1080/00031305.2016.1154108.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Global Breast Cancer
Rights and permissions
About this article
Cite this article
Eniu, A., Antone, N. Access to Affordable Breast Cancer Care in Eastern Europe. Curr Breast Cancer Rep 10, 170–178 (2018). https://doi.org/10.1007/s12609-018-0285-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-018-0285-8