Abstract
Objectives
Sarcopenia refers to age-related loss of skeletal muscle mass. SARC-F is a screening tool for sarcopenia with high specificity and relatively good overall diagnostic accuracy but with low sensitivity. This study evaluated the diagnostic utility of SARC-F and its three modified versions (SARC-CalF, SARC-F+AC, and SARC-CalF+AC) for screening sarcopenia in community-dwelling older adults.
Design
Diagnostic accuracy study.
Settings and Participants
We screened sarcopenia of older adults (age ≥ 60 years) in three communities in 2020. The participants’ information and anthropometric measurements were collected, respectively.
Methods
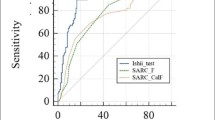
The updated consensuses of AWGS2019 and the EWGSOP2 were applied as the reference standards. we performed sensitivity/specificity analyses and estimated the areas under the receiver operating characteristic curves (AUCs) of the four scales.
Results
The prevalence of sarcopenia was 26.4% and 12.5% based on the AWGS2019 and EWGSOP2 criteria, respectively. The sensitivities/specificities of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 12.26%/95.59%, 47.17%/91.53%, 82.08%/68.47%, and 75.47%/83.73%, respectively, using the AWGS2019 criteria. Further, the corresponding AUCs of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 0.650 (95% confidence interval [CI]: 0.601–0.697), 0.811 (95% CI: 0.769–0.848), 0.801 (95% CI: 0.759–0.839), and 0.848 (95% CI: 0.809–0.881), respectively. Using the EWGSOP2 criteria, the sensitivities/specificities of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 20.00%/95.44%, 56.00%/86.61%, 70.00%/81.20%, and 80.00%/74.93%, respectively. The AUCs of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 0.706 (95% CI: 0.659–0.750), 0.799 (95% CI: 0.756–0.837), 0.815 (95% CI: 0.774–0.852), and 0.834 (95% CI: 0.794–0.869), respectively.
Conclusions
The modified versions of SARC-F+AC and SARC-CalF+AC, which have superior sensitivity, can be used to screen sarcopenia in community-dwelling older adults. SARC-CalF+AC had the highest overall diagnostic accuracy for screening sarcopenia among community-dwelling older adults.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is a progressive and generalized skeletal muscle disorder that involves accelerated loss of muscle mass and function (1, 2). It is a formally recognized muscle disease with a diagnosis code in the international classification of disease, tenth revision, and there was clinical modification in 2016 (3). Sarcopenia is associated with increased adverse outcomes, including functional decline, falls, fractures, hospitalization, and mortality (4, 5). Moreover, it increases the disease burden. Janssen et al. reported that the estimated direct healthcare cost attributable to sarcopenia in the United States in 2000 was $18.5 billion (6). Therefore, there is a need to promptly identify and prevent sarcopenia.
Malmstrom et al. developed SARC-F as the first tool for convenient sarcopenia diagnosis (7). I t contains five domains: strength, assistance walking, rising from a chair, climbing stairs, and falling. Additionally, SARC-F has predictive utility for clinically significant outcomes (8, 9). However, a major limitation of SARC-F is its low sensitivity. According to Kera et al., the sensitivity of SARC-F was only 8.0% and 5.3% using the (European Working Group on Sarcopenia in Older People, (EWGSOP) and Asian Working Group for Sarcopenia (AWGS) criteria, respectively, in community-dwelling older Japanese adults (10). Using the EWGSOP criteria, Bahat et al. and Kotlarczyk et al. reported that the sensitivity of SARC-F was 25.0% (community-dwelling older Turkish adults) (11) and 18.2% (long-term care communities in Pennsylvania) (12), respectively. This low sensitivity could yield a high risk of missed diagnosis of sarcopenia. Barbosa-Silva et al. attributed this low sensitivity to the omission of low muscle mass in the questionnaire. Moreover, they suggested that adding calf circumference to SARC-F (SARC-CalF) could significantly improve its sensitivity from 33.3% to 66.7% in Brazil (13). The EWGSOP2 and AWGS2019 consensus both recommend calf circumference as an anthropometric value correlated with sarcopenia (14, 15). According to the EWGSOP criteria, Krzymińska-Siemaszko et al. reported an increased sensitivity of SARC-CalF (30.0% to 60.0%) in Poland (16). In a Chinese study conducted by Yang et al., the sensitivity of SARC-CalF using the EWGSOP and AWGS criteria increased from 20.0% to 48.9% and from 29.5% to 60.7%, respectively, in community-dwelling older adults (17). Despite the improved sensitivity of SARC-CalF, it still cannot sufficiently detect sarcopenia in community-dwelling older adults. Das et al. reported that arm circumference could be a useful indicator of nutritional status and muscle mass (18). Moreover, arm circumference, which is a single indicator, is associated with sarcopenia in older adults (19, 20). We aimed to assess whether adding arm circumference to SARC-F and SARC-CalF could improve their sensitivity for screening sarcopenia in community-dwelling older adults.
Methods
Study Design and patient selection
This was a diagnostic accuracy study. With assistance from community workers, we held public lectures on sarcopenia in Danxia, Lianxi, and Yutang Community in Luzhou City, China. We recruited older adults (age ≥ 60 years) involved in the presentations between January and August 2020. The exclusion criteria were as follows: implanted pacemaker; inability to walk; clinically visible edema; severe heart failure; severe renal failure; and inability to communicate with interviewers. The participants provided written informed consent before the study. Trained medical students collected the participants’ information and anthropometric measurements through face-to-face interviews. The collected information included age; sex; education; smoking; alcohol drinking; SARC-F; and a history of chronic diseases such as hypertension, coronary heart disease, diabetes, chronic obstructive pulmonary disease, stroke, and hyperlipidemia. The study protocol was approved by the Research Ethics Committee of the Affiliated Hospital of Southwest Medical University (approval no.: KY2019176).
Data collection
Muscle mass was assessed using a bioimpedance analysis (BIA) device (InBody 770, Biospace, Seoul, Korea) to estimate the appendicular skeletal muscle mass (ASM). Skeletal muscle mass was calculated as follows: skeletal muscle mass index (kg/m2) = ASM/height2. Handgrip strength was assessed using a handheld Jamar dynamometer. The participants were asked to stand naturally, grip the device with their dominant hand, and squeeze as hard as possible. The best results obtained during three trials were retained. Usual gait speed was determined with the participants walking 6 m at their usual speed. Walking time was measured twice using a stopwatch and converted to m/s, with the average value being included in the analysis (14). The calf circumference was measured as the widest calf circumference with the participant standing. The arm circumference was measured at the midpoint between the olecranon process and the acromion with the arm extended (21). Body height and weight were measured using a height and weight scale. Body mass index (BMI) (kg/m2) was calculated as follows: body weight/height2.
Assessment of Sarcopenia by Using Different Criteria
We used the AWGS2019 and EWGSOP2 criteria as the reference standards for sarcopenia: Table 1 presents the detailed criteria used in this study.
SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were used to detect sarcopenia. The SARC-F scores ranged from 0 to 10, with each item being assigned 2 points; moreover, a score ≥ 4 was predictive of sarcopenia (7). According to the AWGS2019 criteria, the recommended cut-off points for calf circumference for men and women are < 34 cm and < 33 cm, respectively (13). The calf and arm circumference items are scored as 0 and 10 points if the value is above and below the cut-off points, respectively (16, 17). A total SARC-CalF score ≥ 11 is indicative of a positive screening for sarcopenia. The other cut-off points were obtained using the area under the curve (AUC) and Youden methods (22).
Statistical Analyses
Demographics and clinical characteristics were summarized using descriptive statistics. Categorical and continuous variables were compared using the chi-square test and Student’s t-test, respectively. We calculated the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio of the four aforementioned tools for identifying sarcopenia. We generated receiver operating characteristic (ROC) curves to compare the diagnostic performance of the screening tools, with the AUC indicating the screening accuracy. Comparisons between ROC curves were performed using the DeLong method. The sensitivities and specificities of the screening tools for individuals with and without sarcopenia were compared using McNemar’s test. The cut-off points were obtained using the AUC and Youden methods. Statistical analyses were performed using SPSS v20.0 (SPSS Statistics; IBM, Armonk, NY) and MedCalc Statistical Software v19.0.4 (MedCalc Software bvba, Ostend, Belgium). Statistical significance was set at P < 0.05.
Results
Characteristics of the participants
We recruited 439 volunteers; among them, we excluded 38 for the following reasons: age < 60 years (n = 2), missing BIA tests (n = 33), and physical disability preventing completion of the 6-m usual walking speed test (n = 3). The remaining 401 community-dwelling older adults were included in the analysis. The mean age of the participants was 70.51 ± 6.18 years, with half of them being females.
Table 2 shows the characteristics of the participants and subgroups with or without sarcopenia according to the AWGS2019 and EWGSOP2 criteria. The prevalence of sarcopenia was 26.4% and 12.5% based on the AWGS2019 and EWGSOP2 criteria, respectively. Approximately 63.3% of the participants had chronic diseases. The most common chronic diseases were hypertension (67.7%) and diabetes (24.0%). Participants with sarcopenia were significantly older than those without sarcopenia (P < 0.001). Moreover, patients with sarcopenia had significantly lower BMI, calf circumference, arm circumference, gait speed, handgrip strength, ASM, and skeletal mass index than patients without sarcopenia (P < 0.001) (Table 2).
The cut-off points of arm circumference
According to the AWGS2019 criteria, the AUCs of the arm circumference in men and women were 0.792 (95% confidence interval [CI]: 0.729–0.846) and 0.813 (95% CI: 0.752–0.864). The optimal cut-off points of arm circumference for screening sarcopenia were ≤ 29.5 cm and ≤ 28.4 cm in men and women, respectively. The sensitivity/specificity of arm circumference in men and women were 81.1%/67.8%, and 81.1%/69.1%, respectively (Fig. 1).
The cut-off points of SARC-F+AC and SARC-CalF+AC
According to the AWGS2019 criteria, the AUCs of SARC-F+AC and SARC-CalF+AC were 0.801 (95% CI: 0.759–0.839) and 0.848 (95% CI: 0.809–0.881), respectively. According to the EWGSOP2 criteria, the AUCs of SARC-F+AC and SARC-CalF+AC were 0.815 (95% CI: 0.774–0.852) and 0.834 (95% CI: 0.794–0.869), respectively. The optimal cut-off points of SARC-F+AC and SARC-CalF+AC for screening sarcopenia were (7 and 12) and (11 and 12) according to the AWGS2019 and EWGSOP2 criteria, respectively (Fig. 2).
Comparison of SARC-F and its Modified Versions for Screening Sarcopenia
According to the AWGS2019 criteria, the AUCs of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 0.650 (95% CI: 0.601–0.697), 0.811 (95% CI: 0.769–0.848), 0.801 (95% CI: 0.759:0.839), and 0.848 (95% CI: 0.809–0.881), respectively. The sensitivities of SARC-F, SARC-CalF, SARC-F+AC, and SARC-CalF+AC were 12.26% (95% CI: 6.7%–20.1%), 47.17% (95% CI 37.4%–57.1%), 82.08% (95% CI: 73.4%–88.8%), and 75.47% (95% CI: 66.2%–83.3%), respectively. The specificities of SARC-F, SARC-CalF, SARC-F +AC and SARC-CalF+AC were 95.59% (95% CI: 92.6%–97.6%), 91.53% (95% CI: 87.7%–94.4%), 68.47% (95% CI: 62.8%–73.7%), and 83.73% (95% CI 79.0%–87.8%), respectively (Figure 3, Table 3).
The sensitivity of SARC-F+AC was significantly higher than that of SARC-CalF and SARC-CalF+AC (P < 0.001). Moreover, the AUC of SARC-CalF+AC was significantly higher than that of SARC-F+AC and SARC-CalF (P < 0.001). Based on both criteria, the sensitivity of SARC-CalF+AC was significantly higher than that of the other tools (Tables 3 and 4).
Discussion
In China, the sarcopenia prevalence has been gradually increasing with the aging population. Early identification and prevention of sarcopenia are of significant public health importance. SARC-F is a sarcopenia screening tool with low sensitivity, which restricts its use given the increased risk of a missed diagnosis (23, 24). Therefore, there is a need to improve the sensitivity of SARC-F.
In our study, the sensitivity of SARC-F was 12.26% and 20.0% using the AWGS2019 and EWGSOP2 criteria, respectively. In Hong Kong, the sensitivities of SARC-F for screening sarcopenia among community-dwelling elderly people (≤ 65 years) were 4.8% and 9.4% in men and women, respectively, while the corresponding specificities were 98.8% and 94.2% (25). In Japan, the sensitivities of SARC-F for screening diabetes were 14.6% and 33.3% in men and women, respectively, while the corresponding specificities were 85.8% and 72.4% (26). Our findings are consistent with previous reports of the low sensitivity of SARC-F. In our study, the sensitivity of SARC-CalF, which adds calf circumference to SARC-F, increased from 12.26% to 47.17% using the AWGS2019 criteria and from 20.0% to 56.0% using the EWGSOP2 criteria. Using the EWGSOP criteria, the sensitivity of SARC-CalF was increased from 37.5% to 62.5%, from 28.6% to 46.4%, and from 33.3% to 66.7% in our study, Poland (16), and China (17), respectively. In Japan, the sensitivity of SARC-CalF increased from 13.3% to 66.7% using the AWGS criteria (27). Taken together, these findings suggest that the sensitivity of SARC-CalF for sarcopenia screening, which did not exceed 80%, may not be insufficient for identifying cases among community-dwelling older adults.
The arm circumference is an appropriate measurement for identifying children with severe acute malnutrition for admission into outpatient therapeutic programs (28). James et al. reported that arm circumference could identify chronic energy deficiency and predict BMI (29). Furthermore, arm circumference measurements are independently associated with sarcopenia (18–20). Additionally, it is less susceptible to distortion by edema in the lower extremities (30). Accordingly, in the case of lower leg edema, arm circumference should be used rather than calf circumference. Therefore, we added arm circumference to SARC-F and SARC-CalF and analyzed their screening utility for sarcopenia in community-dwelling older adults. Using both the AWGS2019 and EWGSOP2 criteria, there was significantly improved sensitivity of SARC-F+AC and SARC-CalF+AC, with the specificity remaining > 70%. Furthermore, the cut-off points of arm circumference were ≤ 29.5 cm and ≤ 28.4 cm in men and women, respectively. In a Japanese study, the optimal cut-off values of arm circumference were 25.0 cm and 22.7 cm for men and women, respectively (30). SARC-F and its modified versions have several advantages, including being simple, inexpensive, safe, and appropriate for the routine assessments of institutionalized older adults. We found that adding arm circumference to SARC-F and SARC-CalF can significantly improve the sensitivity of the original scale. Accordingly, SARC-F+AC and SARC-CalF+AC can be used to screen for sarcopenia in community-dwelling older adults. Specifically, SARC-F+AC can be used as the first step in community screening for sarcopenia, with SARC-CalF+AC being subsequently applied for more accurate identification. This could significantly contribute to the early prevention of sarcopenia occurrence and development as well as health promotion.
This study has several strengths. First, our findings demonstrated that SARC-F+AC and SARC-CalF+AC can be used to screen for sarcopenia in community-dwelling older adults. This is the first study to demonstrate the diagnostic utility of arm circumference combined with SARC-F for screening sarcopenia. Additionally, we identified the optimal cut-off points of arm circumference for screening sarcopenia in a Chinese population, which has rarely been investigated. Furthermore, we used the latest updated consensus for diagnosing sarcopenia. However, further studies are required to validate these findings in different populations.
Conclusion
Our findings demonstrated that the modified versions of SARC-F have better diagnostic performance than the original questionnaire. Applying SARC-F+AC or SARC-F+AC may facilitate sarcopenia screening in community-dwelling older adults and improve the identification of sarcopenia.
References
Woo J. Sarcopenia. Clin Geriatr Med 2017;33:305–314. https://doi.org/10.1016/j.cger.2017.02.003.
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019;393:2636–2646. https://doi.org/10.1016/S0140-6736(19)31138-9.
Anker SD, Morley JE, von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle 2016;7:512–514. https://doi.org/10.1002/jcsm.12147.
Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord 2017;16:21. https://doi.org/10.1186/s40200-017-0302-x.
Yalcin A, Aras S, Atmis V, Cengiz OK, Cinar E, Atli T, Varli M. Sarcopenia and mortality in older people living in a nursing home in Turkey. Geriatr Gerontol Int 2017;17:1118–1124. https://doi.org/10.1111/ggi.12840.
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc 2004;52:80–85. https://doi.org/10.1111/j.1532-5415.2004.52014.x.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc 2013;14:531–532. https://doi.org/10.1016/j.jamda.2013.05.018.
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 2016;7:28–36. https://doi.org/10.1002/jcsm.12048.
Fu X, Tian Z, Thapa S, Sun H, Wen S, Xiong H, Yu S. Comparing SARC-F with SARC-CalF for screening sarcopenia in advanced cancer patients. Clin Nutr 2020;39:3337–3345. https://doi.org/10.1016/j.clnu.2020.02.020.
Kera T, Kawai H, Hirano H, Kojima M, Watanabe Y, Motokawa K, et al. SARC-F: A validation study with community-dwelling older Japanese adults. Geriatr Gerontol Int 2019;19:1172–1178. https://doi.org/10.1111/ggi.13768.
Bahat G, Oren MM, Yilmaz O, Kılıç C, Aydin K, Karan MA. Comparing SARC-F with SARC-CalF to screen sarcopenia in community living older adults. J Nutr Health Aging 2018;22:1034–1038. https://doi.org/10.1007/s12603-018-1072-y.
Kotlarczyk MP, Perera S, Nace DA, Resnick NM, Greenspan SL. Identifying sarcopenia in female long-term care residents: A comparison of current guidelines. J Am Geriatr Soc 2018;66:316–320. https://doi.org/10.1111/jgs.15213.
Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC, Grupo de Estudos em Composição Corporal e Nutrição. Enhancing SARC-F: improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc 2016;17:1136–1141. https://doi.org/10.1016/j.jamda.2016.08.004.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21:300–307. https://doi.org/10.1016/j.jamda.2019.12.012.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31. https://doi.org/10.1093/ageing/afy169.
Krzymińska-Siemaszko R, Deskur-Śmielecka E, Kaluźniak-Szymanowska A, Lewandowicz M, Wieczorowska-Tobis K. Comparison of diagnostic performance of SARC-F and its two modified versions (SARC-CalF and SARC-F+EBM) in community-dwelling older adults from Poland. Clin Interv Aging 2020;15:583–594. https://doi.org/10.2147/CIA.S250508.
Yang M, Hu X, Xie L, et al. Screening sarcopenia in community-dwelling older adults: SARC-F vs SARC-F combined with calf circumference (SARC-CalF). J Am Med Dir Assoc 2018;19:277.e1–277.e8. https://doi.org/10.1016/j.jamda.2017.12.016.
Das A, Saimala G, Reddy N, Mishra P, Giri R, Kumar A, et al. Mid-upper arm circumference as a substitute of the body mass index for assessment of nutritional status among adult and adolescent females: learning from an impoverished Indian state. Public Health 2020;179:68–75. https://doi.org/10.1016/j.puhe.2019.09.010.
Esteves CL, Ohara DG, Matos AP, Ferreira VTK, Iosimuta NCR, Pegorari MS. Anthropometric indicators as a discriminator of sarcopenia in community-dwelling older adults of the Amazon region: a cross-sectional study. BMC Geriatr 2020;20:518. https://doi.org/10.1186/s12877-020-01923-y.
Tsai HJ, Chang FK. Associations between body mass index, mid-arm circumference, calf circumference, and functional ability over time in an elderly Taiwanese population. PLOS ONE 2017;12:e0175062. https://doi.org/10.1371/journal.pone.0175062.
Akın S, Mucuk S, Öztürk A, Mazıcıoğlu M, Göçer Ş, Arguvanlı S, Şafak ED. Muscle function-dependent sarcopenia and cut-off values of possible predictors in community-dwelling Turkish elderly: calf circumference, midarm muscle circumference and walking speed. Eur J Clin Nutr 2015;69:1087–1090. https://doi.org/10.1038/ejcn.2015.42.
Martínez-Camblor P, Pardo-Fernández JC. The Youden index in the generalized receiver operating characteristic curve context. Int J Biostat 2019;15. https://doi.org/10.1515/ijb-2018-0060.
Urzi F, Šimunič B, Buzan E. Basis for sarcopenia screening with the SARC-CalF in nursing homes. J Am Med Dir Assoc 2017;18:991.e5–991.e10. https://doi.org/10.1016/j.jamda.2017.07.011.
Kurita N, Wakita T, Kamitani T, Wada O, Mizuno K. SARC-F validation and SARC-F+EBM derivation in musculoskeletal disease: the SPSS-OK study. J Nutr Health Aging 2019;23:732–738. https://doi.org/10.1007/s12603-019-1222-x.
Woo J, Leung J, Morley JE. Validating the SARC-F: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc 2014;15:630–634. https://doi.org/10.1016/j.jamda.2014.04.021.
Ida S, Murata K, Nakadachi D, Ishihara Y, Imataka K, Uchida A, et al. Development of a Japanese version of the SARC-F for diabetic patients: an examination of reliability and validity. Aging Clin Exp Res 2017;29:935–942. https://doi.org/10.1007/s40520-016-0668-5.
Ito A, Ishizaka M, Kobayashi K, Sawaya Y, Hara T, Nagasaka Y, Yakabi A, Watanabe M, Kubo A. Changes in the screening efficacy of lower calf circumference, SARC-F score, and SARC-CalF score following update from AWGS 2014–2019 sarcopenia diagnostic criteria in community-dwelling older adults. J Phys Ther Sci 2021;33:241–245. https://doi.org/10.1589/jpts.33.241.
Abitew DB, Yalew AW, Bezabih AM, Bazzano AN. Comparison of mid-upper-arm circumference and weight-for-height Z-score in identifying severe acute malnutrition among children aged 6–59 months in south Gondar Zone, Ethiopia. J Nutr Metab 2021;2021:8830494. https://doi.org/10.1155/2021/8830494.
Madden AM, Smith S. Body composition and morphological assessment of nutritional status in adults: a review of anthropometric variables. J Hum Nutr Diet 2016;29:7–25. https://doi.org/10.1111/jhn.12278.
Endo K, Sato T, Kakisaka K, Takikawa Y. Calf and arm circumference as simple markers for screening sarcopenia in patients with chronic liver disease. Hepatol Res 2021;51:176–189. https://doi.org/10.1111/hepr.13589.
Acknowledgments
This work was supported by the Danone Dietary Nutrition Research and Education Fund [grant number DIC2019-10]. We would like to thank the participants and community workers for their support.
Author information
Authors and Affiliations
Contributions
Author contributions: JH contributed to the design of the study and critically revised the manuscript for important intellectual content and approved the final version of the manuscript. ZJL and LTT contributed to the interpretation of the data and drafted the manuscript. ZJL, LTT, CXY, JW, and WM performed the study. And all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest: None of the authors has a confict of interest to declare.
Ethical standards: The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. All subjects have given written informed consent. The study protocol was approved by the Research Ethics Committee of the Affiliated Hospital of Southwest Medical University (approval no.: KY2019176).
Rights and permissions
About this article
Cite this article
Zhou, J., Li, T., Chen, X. et al. Comparison of the Diagnostic Value of SARC-F and Its Three Modified Versions for Screening Sarcopenia in Chinese Community-Dwelling Older Adults. J Nutr Health Aging 26, 77–83 (2022). https://doi.org/10.1007/s12603-021-1718-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1718-z