Abstract
Objectives
In this study, we examined the factors influencing the presence or absence of dental intervention in patients with pneumonia in an acute-care hospital, focusing on oral intake and its status.
Design
Observational study.
Setting
Teikyo University School of Medicine, Mizonokuchi Hospital.
Participants
Patients ≥65 years of age who were admitted to the Teikyo University School of Medicine, Mizonokuchi Hospital between January 1, 2018 and December 31, 2019 with pneumonia who were referred to the Department of Rehabilitation with suspected dysphagia were included in the study. Fifty patients who underwent dental intervention were compared with 50 controls who had received no dental interventions prior to the opening of the dental department.
Measurements
Time series matching was retrospectively performed using the Oral Health Assessment Tool (OHAT). From the medical records, age at admission, sex, pneumonia severity classification (age, dehydration, respiratory failure, orientation disturbance, and blood pressure [A-DROP] score), body mass index, Charlson’s Comorbidity Index, OHAT, functional oral intake scale (FOIS) score at admission and discharge, and the length of hospital stay were retrieved; FOIS level ≥4 was defined as established oral intake.
Results
The number of patients in the control group before matching was 179. Twelve patients with missing information and seven patients who died in the hospital were excluded from this study. Multivariable logistic regression analysis showed that dental intervention (odds ratio 3.0, p = 0.014) was associated with the establishment of oral intake at discharge. Multiple logistic regression analysis showed that dental intervention was a significant factor for FOIS at discharge (p = 0.002) and the length of hospital stay (p = 0.039).
Conclusion
Oral management with dental intervention was associated with establishing oral intake and reducing hospital stay in patients with pneumonia, regardless of pneumonia severity or comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The oral condition is related to swallowing function and oral intake. A study investigating factors affecting oral intake in acute-care hospital inpatients aged ≥40 years reported that level of consciousness, activities of daily living (ADL), and oral hygiene are associated with feeding status (1). There are multiple causes of dysphagia, including poor oral hygiene and organic and functional problems of the oral region (2). Furthermore, there is an association between the swallowing muscles and trunk muscles in the elderly (3). Since aspiration pneumonia leads to atrophy of the skeletal and swallowing muscles (4), hospitalization may worsen oral conditions and cause deterioration of oral and swallowing function.
In a study on hospital inpatients with cancer, appropriate preoperative oral management by dentists significantly reduced the risk of developing postoperative pneumonia and was also related to all-cause 30-day mortality (5). Additionally, oral management by dental hygienists affected the patients’ ADL, home discharge rates, and survival rates at a convalescent hospital (6). Thus, dental interventions (oral management) during hospitalization may not only improve oral hygiene but also its therapeutic effect. Further, to establish safe oral intake for inpatients, evaluation of the general condition and swallowing function, “oral management,” appropriate oral evaluation, and nutritional management are indispensable.
However, most studies to date have focused on the relationship between current oral conditions, swallowing function, and diet form. It remains unclear whether dental interventions during hospitalization influence oral intake in elderly patients with pneumonia. Furthermore, there is inadequate evidence regarding the need for dental intervention in dysphagia rehabilitation. Therefore, in this study, we investigated the factors influencing the presence or absence of dental intervention in patients with pneumonia in an acute-care hospital, focusing on its relationship with oral intake status.
Materials and Methods
Participants
This was a human observational study, and the manuscript conforms to the STROBE guidelines. The study protocol was approved by the Institutional Review Board of Teikyo University School of Medicine, Mizonokuchi Hospital (Approval ID: 20-006) and meets the guidelines of our responsible governmental agency. We explained the purpose of this study to the participants or their delegates and obtained their written informed consent before their participation. The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Patients aged ≥65 years who were admitted to Mizonokuchi Hospital with pneumonia between January 1, 2018 and December 31, 2019 who were referred to the Department of Rehabilitation for suspected dysphagia were included in this study. All patients provided informed consent prior to enrollment in this study. Patients who did not provide informed consent, those with missing information, and those who died while in the hospital were excluded from the study.
Data collection
Patients’ age, sex, pneumonia severity classification (age, dehydration, respiratory failure, orientation disturbance, and blood pressure [A-DROP] score), body mass index (BMI), Charlson’s Comorbidity Index (CCI) score, oral health assessment tool (OHAT) score, functional oral intake scale (FOIS) score at admission and discharge, Barthel Index score at admission, number of days to rehabilitation and dental intervention, number of dental interventions, and length of hospital stay after admission were obtained from medical records.
A-DROP
The A-DROP scoring system is an assessment tool that is used to assess the severity of community-acquired pneumonia (CAP) proposed by the Japanese Respiratory Society (7). Age (≥70 years for men and ≥75 years for women), dehydration (blood urea nitrogen ≥21 mg/ml or with dehydration), respiration (SpO2 ≤90%), orientation disturbance of consciousness, and systolic blood pressure (systolic blood pressure ≤90 mmHg) are assessed using a 6-point scale (minimum score 0 to maximum score 5). The A-DROP score is a modified version of the CURB-65 proposed by the British Thoracic Society. A study, which included 371 hospitalized patients with pneumonia validated the A-DROP score against the CURB-65 score for predicting pneumonia severity (8). The total score for all items was calculated.
FOIS
The FOIS score is a measure of patients’ oral intake (9). It is rated on a 7-point scale and ranges from level 1 (“nothing by mouth”) to level 7 (“total oral diet with no restrictions”). Established oral intake was defined as an FOIS level of 4 (“total oral diet of a single consistency”) or higher at discharge.
OHAT
Oral hygiene was assessed at the time of admission and was evaluated on a scale of 0=healthy, 1=oral changes, 2=unhealthy for eight items: lips, tongue, gums and tissues, saliva, natural teeth, dentures, oral cleanliness, and dental pain (10). The total score of all items was calculated.
Oral management status
The definition of oral management in this study is to perform oral hygiene and oral function management to prevent aspiration pneumonia and establish oral intake. The dentists performed an oral assessment and dental treatment. Treatment included prosthodontics, extractions, and procedures for oral mucosal disease, depending on the patient’s oral condition, general condition, and urgency. Furthermore, a diet form was suggested based on the patient’s oral condition. Oral care was performed by a skilled dental hygienist. The dentists had specialized knowledge about dysphagia and nutritional management, and the dental hygienist also had specialized knowledge about oral care to hospital inpatients. The frequency of dental interventions was adjusted from one to five times a week, depending on the patient’s OHAT score and condition. Oral care took approximately 15–20 minutes and included brushing and dental scaling by the bed or in a wheelchair.
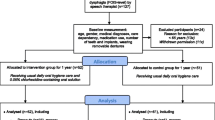
Data analysis
Fifty participants who received dental interventions for oral management after the opening of the Dental Department in April 2019 (dental intervention group) were retrospectively time-series matched 1:1 using the OHAT, with 50 participants who received no dental interventions before April 2019 as the control group. Among the eligible patients enrolled in the study, individuals in the control group who were admitted between April 1, 2018 and March 31, 2019 were arranged according to their order of admission. Similarly, patients who received dental intervention after April 2019 were also arranged according to their order of admission. We performed 1:1 pair matching of patients who received dental intervention and those in the control group with the same OHAT score, in chronological order from the oldest date of admission.
In this study, we considered the OHAT score as the largest confounding factor. Since high OHAT scores require intervention by dental professionals, the OHAT score is a very large confounding factor by indication. As this variable could not be adjusted for in the multivariate analysis, we decided to match cases based on the OHAT score. Furthermore, there were other potential confounding factors as well; however, matching all of these would have greatly decreased the sample size, which, in turn, would have resulted in a loss of statistical power. Moreover, we expected that the influence of the other confounding factors would be considerably reduced if OHAT was matched; thus, we decided to adjust for the remaining confounding factors in the multivariate analysis.
We first analyzed participant characteristics and outcomes at discharge. Age, sex ratio, A-DROP score, FOIS score at admission, FOIS score at discharge, OHAT, BMI, Barthel Index, CCI, number of days to rehabilitation intervention, oral intake independence, and length of hospital stay of patients in the dental intervention group were compared with those of controls using the Mann-Whitney U test.
We subsequently examined factors affecting established oral intake. Multivariable logistic regression analysis was performed with the presence or absence of established oral intake as the dependent variable to determine whether dental intervention was independently associated with oral intake. Additionally, multiple logistic regression analysis was performed using the FOIS score at discharge and the length of hospital stay as dependent variables to determine whether dental intervention was independently associated. We included propensity scores as explanatory variables in the multivariate analysis to reduce the number of variables included in the statistical models and to avoid overfitting (11). Propensity scores for dental intervention were calculated using logistic regression analysis, including baseline covariates, age, sex, A-DROP score, FOIS at admission, BMI, Barthel index at admission, and CCI as independent variables.
We also performed a post hoc power analysis to ascertain the statistical validity of our sample size. Data were analyzed with SPSS version 25.0 (IBM Inc., Tokyo, Japan). The level of significance for all analyses was set at p < 0.05.
Results
Post hoc power analysis of propensity score-matched pairs for the total oral intake at discharge (an alpha value equal to 0.05, Effect size w of 0.70, and total sample size of 100) demonstrated an observed power of 99.8%.
Participant characteristics and outcomes
The participants’ characteristics and outcomes before and after matching are shown in Table 1. The number of patients in the control group before matching was 179. Twelve patients with missing information and seven patients who died in the hospital were excluded from this study. None of the patients required tracheotomy or gastrostomy. The results showed that the significant items between the control and dental intervention groups before matching were A-DROP score at admission (2 and 3, respectively; p = 0.001), OHAT score at consultation (3 and 7, respectively; p < 0.001), BMI at admission (17.8 and 19.1, respectively; p = 0.01), CCI at admission (2 and 1.5, respectively; p = 0.001), and FOIS level at discharge (p = 0.009). Significant items between the control and dental intervention groups after matching were the FOIS level at discharge (2.0 and 3.3, respectively; p < 0.001), establishment of oral intake (12 and 27, respectively; p = 0.004), length of hospital stay (31 and 26, respectively; p = 0.034), and the CCI (2 and 1.5, respectively; p = 0.042). There was no significant difference in the number of days to rehabilitation between the control and dental intervention group before and after matching. The median (IQR) of number of days to dental intervention was 4 (3–8). The median (IQR) of number of times of dental intervention was 4 (1–7).
Factors affecting the establishment of oral intake
Multiple logistic regression analysis showed that dental intervention (odds ratio 3.0, p = 0.014) was a significant factor for establishing oral intake (Table 2).
Factors affecting the FOIS score at discharge and the length of hospital stay
Multiple regression analysis showed that dental intervention was a significant factor for determining the FOIS level at discharge (p = 0.002) (Table 3) and the duration of hospital stay (p = 0.039) (Table 4). Dental intervention was found to have an influence on both the FOIS score at discharge and the length of hospital stay.
Discussion
Our results revealed significant differences in the FOIS level, establishment of oral intake, and the length of hospital stay at discharge between the dental intervention group and the control group. It was also observed that dental intervention influenced the establishment of oral intake and the length of hospital stay. Dysphagia rehabilitation has proven to be effective in promoting oral intake in elderly patients with aspiration pneumonia (12). However, it remains unclear whether dental interventions affect oral intake. This study provides new evidence regarding the association between oral management and oral intake.
Effect of oral management on oral intake
Oral management includes not only oral hygiene management but also appropriate assessment of oral function and necessary treatment for each patient. Nurses provide daily oral care to patients who have difficulty in performing oral care on their own. However, they may not be able to provide adequate oral care due to time or technical problems. Thus, the involvement of dentistry will enable an early response to oral problems and improve the efficiency of oral management. Oral hygiene and remaining teeth condition in elderly hospitalized patients are also associated with nutritional status and comorbidities (13). Furthermore, poor oral health is related to sarcopenia, malnutrition, and low ADL (14). Therefore, it is desirable to perform oral management as part of managing swallowing function, nutritional status, and general condition.
As for the relationship between oral intake and length of hospital stay, a study of elderly patients with pneumonia reported that the early initiation of oral intake shortened the length of hospital stay (15). Additionally, patients with oral problems in convalescent hospitals had a longer hospital stay and higher in-hospital mortality rates than patients without oral problems (16). In order to initiate oral intake at an early stage, it is essential to maintain a good oral environment. In this study, the median time from hospitalization to dental intervention was 4 days, and oral management could be started relatively early. Elderly patients with aspiration pneumonia are prone to have poor oral hygiene, even if they are not eating orally. Furthermore, it has been reported in a study of patients in the acute phase that oral motor exercise in addition to usual oral care increased saliva flow compared to the usual oral care only group, as well as establishing oral intake at an early stage (17). Oral management immediately after the onset of pneumonia may have contributed not only to the prevention of pneumonia but also to functional approaches, such as prevention of disuse to establish oral intake.
Moreover, when oral intake cannot be established, successful rehabilitation would be difficult, and it would be required to consider alternative nutritional routes. In particular, for patients in acute care hospitals, the status of oral intake influences the subsequent treatment plan and prolongs the length of hospital stay. Therefore, it is considered that oral management from the early stage of hospitalization enables the early initiation of oral intake, and the establishment of oral intake shortens the length of hospital stay.
Effect of dental intervention with a team approach
Various effects of multidisciplinary interventions on inpatients have been reported previously. For example, in a study on patients with esophageal cancer, it has been reported that during the perioperative period, a multidisciplinary team approach consisting of a physician, dentist, dental hygienist, and therapist is effective for early ambulation, early initiation of oral intake, and in shortening the length of hospital stay (18). Similarly, in patients with acute stroke, multidisciplinary dysphagia rehabilitation, including intervention by dentists and dental hygienists, reduced the rates of pneumonia. Moreover, the frequency of oral management and swallowing function assessment by dentists was reportedly increased (19). In contrast, only a few studies have verified the outcome of each team member’s role for patients.
In this study, a speech-language therapist performed swallowing rehabilitation in both groups with and without dental intervention. One of the reasons for the significant increase in oral intake in the dental intervention group was that the dentist who performed the oral management had specialized knowledge in dysphagia rehabilitation and was able to provide advice on diet form based on the oral status and swallowing function. In dysphagia rehabilitation, it is also necessary to evaluate oral functions involving food transport and mastication. Therefore, an approach from the perspective of dentistry may be beneficial in some cases. In a team approach to establish oral intake, the involvement of dentistry and the provision of information on oral status to other professions can clarify problems related to swallowing and how to deal with them. It is highly significant for both patients and medical professionals to provide dental intervention during hospitalization.
Limitations
In this study, we only assessed the presence or absence of dental intervention on the outcomes. Since dental treatment by dentists and oral care by dental hygienist were sometimes performed simultaneously, the number of interventions by the dentist and dental hygienist, respectively, was not counted accurately. The procedures mainly consisted of oral care by a dental hygienist; however, necessary procedures, such as extractions and denture adjustments, were also performed. In addition, Oral care was performed by a single hygienist, and the procedures and intervention times were not prescribed; rather, they were adapted to each patient’s requirement. Therefore, there is a need to prescribe the frequency of intervention for the dentist and the dental hygienist and to determine which procedures are effective in establishing oral intake.
As for the FOIS, a diet form is assessed at level ≥4. It must also be considered whether chewing function is maintained. In acute-care hospitals, denture problems, such as ill-fitting dentures or not owning dentures, are a major factor for high OHAT scores at discharge. Additionally, the shortage of time makes it difficult to perform large-scale dental treatments, such as fabricating new dentures during hospitalization (20). In our study, due to the limited recovery of chewing function, it was considered that the FOIS level did not improve after dental intervention, which may have affected the FOIS at discharge. Future studies are required to investigate the relationship between functional recovery and oral intake through long-term oral management from admission to post-discharge. Apart from the patient’s condition, social factors might have also influenced the adjustment of hospital transfer and discharge, and further investigations are required to determine the length of hospital stay.
Conclusion
In acute-care hospitals, dental intervention for patients with pneumonia has been associated with the establishment of oral intake and reduced length of hospital stay. This study suggests the effectiveness and importance of early oral management. A multidisciplinary team approach is effective in dysphagia rehabilitation, and dental intervention and oral management may enhance the effectiveness of rehabilitation. However, it is important that the dental intervention is adaptable and is appropriate for the patients’ oral intake goals and their condition during hospitalization.
References
Furuya J, Suzuki H, Tamada Y, Onodera S, Nomura T, Hidaka R, Minakuchi S, Kondo H. Food intake and oral health status of inpatients with dysphagia in acute care settings. J Oral Rehabil 2020;47:736–742. doi: https://doi.org/10.1111/joor.12964
Rech RS, Baumgarten A, Colvara BC, Brochier CW, de Goulart B, Hugo FN, Hilgert JB. Association between oropharyngeal dysphagia, oral functionality, and oral sensorimotor alteration. Oral Dis 2018;24:664–672. doi: https://doi.org/10.1111/odi.12809
Yoshimi K, Nakagawa K, Hara K, Yamaguchi K, Nakane A, Kubota K, Furuya J, Tohara H. Relationship between tongue pressure and back muscle strength in healthy elderly individuals. Aging Clin Exp Res 2020;32:2549–2555. doi: https://doi.org/10.1007/s40520-020-01484-5
Komatsu R, Okazaki T, Ebihara S, Kobayashi M, Tsukita Y, Nihei M, Sugiura H, Niu K, Ebihara T, Ichinose M. Aspiration pneumonia induces muscle atrophy in the respiratory, skeletal, and swallowing systems. J Cachexia Sarcopenia Muscle 2018;9:643–653. doi: https://doi.org/10.1002/jcsm.12297
Ishimaru M, Matsui H, Ono S, Hagiwara Y, Morita K, Yasunaga H. Preoperative oral care and effect on postoperative complications after major cancer surgery. Br J Surg 2018;105:1688–1696. doi: https://doi.org/10.1002/bjs.10915
Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y, Yamaga M, Koga H. Hospital dental hygienist intervention improves activities of daily living, home discharge and mortality in post-acute rehabilitation. Geriatr Gerontol Int 2019;19:189–196.
Miyashita N, Matsushima T, Oka M, Japanese Respiratory Society. The JRS guidelines for the management of community-acquired pneumonia in adults: an update and new recommendations. Intern Med 2006;45:419–428. doi: https://doi.org/10.2169/internalmedicine.45.1691
Shindo Y, Sato S, Maruyama E, Ohashi T, Ogawa M, Imaizumi K. Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia. Respirology 2008;13:731–735. doi: https://doi.org/10.1111/j.1440-1843.2008.01329.x
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005;86:1516–1520. doi: https://doi.org/10.1016/j.apmr.2004.11.049
Chalmers JM, King PL, Spencer AJ, Wright FA, Carter KD. The oral health assessment tool-validity and reliability. Aust Dent J 2005;50:191–199. doi: https://doi.org/10.1111/j.1834-7819.2005.tb00360.x
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399–424. doi: https://doi.org/10.1080/00273171.2011.568786
Momosaki R, Yasunaga H, Matsui H, Horiguchi H, Fushimi K, Abo M. Effect of dysphagia rehabilitation on oral intake in elderly patients with aspiration pneumonia. Geriatr Gerontol Int 2015;15:694–699. doi: https://doi.org/10.1111/ggi.12333
Ni-Chroinin D, Montalto A, Jahromi S, Ingham N, Beveridge A, Foltyn P. Oral health status is associated with common medical comorbidities in older hospital inpatients. J Am Geriatr Soc 2016;64:1696–1700. doi: https://doi.org/10.1111/jgs.14247
Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor oral health as a determinant of malnutrition and sarcopenia. Nutrients 2019;11:2898. doi: https://doi.org/10.3390/nu11122898
Koyama T, Maeda K, Anzai H, Koganei Y, Shamoto H, Wakabayashi H. Early commencement of oral intake and physical function are associated with early hospital discharge with oral intake in hospitalized elderly individuals with pneumonia. J Am Geriatr Soc 2015;63:2183–2185. doi: https://doi.org/10.1111/jgs.13679
Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y, Shimazu S, Jeong S. Impaired oral health status on admission is associated with poor clinical outcomes in post-acute inpatients: A prospective cohort study. Clin Nutr 2019;38:2677–2683.
Wu CP, Xu YJ, Wang TG, Ku SC, Chan DC, Lee JJ, Wei YC, Hsiao TY, Chen CC. Effects of a swallowing and oral care intervention for patients following endotracheal extubation: a pre- and post-intervention study. Crit Care 2019;23:350. doi: https://doi.org/10.1186/s13054-019-2623-2
Akiyama Y, Iwaya T, Endo F, Shioi Y, Kumagai M, Takahara T, Otsuka K, Nitta H, Koeda K, Mizuno M et al. Effectiveness of intervention with a perioperative multidisciplinary support team for radical esophagectomy. Support Care Cancer 2017;25:3733–3739. doi: https://doi.org/10.1007/s00520-017-3801-x
Aoki S, Hosomi N, Hirayama J, Nakamori M, Yoshikawa M, Nezu T, Kubo S, Nagano Y, Nagao A, Yamane N et al. The multidisciplinaiy swallowing team approach decreases pneumonia onset in acute stroke patients. PLoS One 2016;11:e0154608. doi: https://doi.org/10.1371/journal.pone.0154608
Obana M, Furuya J, Matsubara C, Tohara H, Inaji M, Miki K, Numasawa Y, Minakuchi S, Maehara T. Effect of a collaborative transdisciplinary team approach on oral health status in acute stroke patients. J Oral Rehabil 2019;46:1170–1176. doi: https://doi.org/10.1111/joor.12855
Acknowledgments
The authors would like to thank Mikako Nakamura at the Teikyo University School of Medicine, Mizonokuchi Hospital, for coordinating the study.
Funding
Funding: This study was supported by Japanese Dental Science Federation (JDSF-DSP1-2021-116-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards: The experiments in this study comply with the current laws of the country in which they were performed.
Conflict of Interest Statement: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yoshimi, K., Nakagawa, K., Momosaki, R. et al. Effects of Oral Management on Elderly Patients with Pneumonia. J Nutr Health Aging 25, 979–984 (2021). https://doi.org/10.1007/s12603-021-1660-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1660-0