Abstract
Purpose
The transformative impact of Artificial intelligence (AI) on clinical trials is explored. To identify the potential benefits of AI in enhancing both the efficiency and effectiveness of clinical research, while also examining the challenges associated with its implementation.
Methods
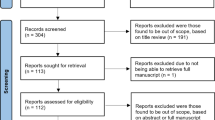
Through an analysis of research literature, case studies, and relevant regulatory frameworks, which highlights the potential of AI in clinical research. This includes improvements in patient recruitment, streamlined data analysis, and optimized clinical trial design. Case studies are presented to showcase the effectiveness of AI in achieving better trial outcomes.
Results
Challenges that come with implementing AI such as issues regarding accountability and transparency due to increased reliance on AI-driven insights. Additionally, regulatory uncertainties around approving and overseeing AI-powered clinical trials, and ethical considerations concerning data privacy and potential biases within AI algorithms, are identified. Despite these challenges, the research emphasizes AI's potential to transform drug development by making clinical trials more efficient and insightful.
Conclusion
The paper concludes by suggesting future research directions that explore the ethical, legal, and regulatory implications of AI in clinical trials, while further investigating its potential benefits for medical advancements.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Initially defined in 1955, artificial intelligence (AI) is the source of technological advancement in creating intelligent computer programs. Artificial intelligence (AI) aims to replicate human decision-making processes by the mechanization of human intelligence processes such as logical reasoning based on self-learning and self-correction [1]. Artificial intelligence has significantly expanded healthcare in drug development and clinical design by exhibiting human-level intelligence in performing complex tasks [2]. The change is driven by AI's ability to study and analyze vast datasets, identify different patterns, and make data-driven predictions, all of which are invaluable in the complex world of clinical research. Currently, AI is being increasingly utilized in clinical trials for maintaining electronic health records and identifying eligible participants for clinical trials more efficiently [3]. Further study protocols made using AI for designing the trials can increase the success rate of clinical trials significantly [4]. A clear difference between the traditional method of conducting clinical trials and the use of AI for clinical trials is visualized in Fig. 1. Data analysis and interpretation can be more streamlined and evident for AI-based drug development and understanding the trends in a patient-centric approach [5]. The use of AI in clinical trials is subject to regulatory oversight to ensure patient safety and data integrity; many regulatory bodies have issued guidelines for it. FDA is working on a flexible risk-based regulatory framework for AI/ML in drug development [6]. The Indian Council of Medical Research (ICMR) has issued "Ethical Guidelines for Application of Artificial Intelligence in Biomedical Research and Healthcare, 2023" to offer ethics steerage for stakeholders on the use of AI in healthcare [7]. FDA also released an "Artificial Intelligence/Machine Learning (AI/ML)-Based Software as Medical Devices (SaMD) Action Plan" that outlines five actions FDA intends to address challenges posed by adaptive AI and machine learning Technologies in Medical Devices the solution of. Regulators around the world are taking steps to tighten guidelines and promote innovation that protects patient welfare [8].
1.1 The possibilities of AI in transforming the drug development process
AI assists drug discovery by designing new d rugs that target specific proteins and predicting drug interactions within the body, which allows researchers to identify promising candidates and avoid failure early on [9]. By monitoring patient reactions to therapy, selecting and enrolling those who could profit from new medicine, and designing trials more effectively, AI can revolutionize the industry. This innovation can decrease cost and time spent on identifying therapeutic targets and introducing new medications. As pharmaceuticals inevitably interact with the human body, AI has the capability to enhance their efficacy [10]. AI can be used to identify, design, and predict how drugs are likely to interact with the human body [11]. This can speed up the development and release of novel medications by researchers. A firm called Benevolent AI uses artificial intelligence (AI) to evaluate enormous biological data sets to find novel targeted medications and forecast their efficacy and safety. Verily is a company that is using AI to develop new tools for clinical trials [12]. For example, Verily is developing a wearable device that can monitor patients' responses to treatment in real-time real time. Many regulation bodies are regulating AI and how AI is used in clinical trials a comparison of different nations is shown in Table 1.
2 Evolving role of AI in clinical trials
AI can help recruit patients for trials by analyzing the patients' data and identifying the eligible patients or volunteers faster and more accurately, reducing the burden on the sponsors [4]. The design of the trials would be more patient-centric by studying the historical data to have relevant endpoints in the population [8]. The vast datasets, ensuring data quality, real-time anomaly detection, and identifying potential adverse events early AI will reduce errors and patient safety by optimizing patient dosage and treatment plans. Patient engagements using AI tools like chatbots will enhance the patient experience and provide a more comprehensive understanding of treatment impact in real-world settings [13]. Artificial intelligence can oversee informed consent procedures, protocol adherence, ethical compliance, and trial conduct integrity. It can also help with regulatory submissions by automating document creation and guaranteeing rules are followed, which speeds up the approval process [14].
2.1 The impact of AI in drug development
AI-powered algorithms that can analyze massive databases, making the identification of possible medications more precise and efficient [15]. Also, by reducing drug failures and costs, researchers can measure the safety and efficacy of drugs due to AI’s predictive knowledge, freeing up time to focus on optimal medicine AI enables personalized medicine to optimize treatment regimens based on clinical and genetic information [12]. Furthermore, AI streamlines affected person recruitment, records evaluation, and clinical trial design, main to swifter and more price-effective studies, as shown in Fig. 2. Artificial Intelligence drastically lowers costs by way of reducing the time and resources needed for remedy research [15]. AI also improves drug safety by lowering patient risks via early detection of possible toxicity and adverse effects. AI's capacity to assess patient data from real-world settings enhances the findings of clinical trials by offering a thorough grasp of how well drugs work in a range of patient groups [16, 17].
3 AI in clinical trial design, conduct, and analysis
Deep Learning and machine learning are AI techniques used in the pharma industry where machine learning analyses data to build models for decision-making. It comes in two categories, Supervised learning for predication and unsupervised learning for extracting patterns from unlabelled data. Deep learning uses complex models to process large amounts of data [18]. Another field used in drug research is natural language processing (NLP), used for interpreting textual or natural language data. Optical character recognition (OCR) aims to electronically convert images of handwritten human text/printed or typed text into machine-encoded text using pattern recognition and computational vision [9, 19].
AI has transformed drug delivery across all stages, from target identification to clinical trials, making the traditionally expensive and failing process more efficient [20]. AI can assist in choosing parent compounds that might have a better chance of success throughout the development phase and which may increase the effectiveness of the search for showing the association between indications and biomarkers [21]. AI has the significant potential for making plans, designing, and carrying out clinical studies. To increase recruitment by matching affected person functions to choice criteria, massive and numerous datasets, including digital medical facts (EMRs), published clinical literature, and scientific trial databases, may be connected collectively using ML, DL, NLP, and OCR [22]. AI can improve patient selection for clinical trials by analyzing vast amounts of medical records (EMRs). This reduces variability and allows researchers to identify patients with a higher chance of responding to treatment (predictive enrichment). Machine learning helps in this process, by using algorithms to identify patients likely to develop Alzheimer’s (AD). This approach was tested with a tool simulating drugs, the disease, and its course for early AD, even undergoing regulatory evaluation [23].
AI systems have the potential to automatically analyse digital eligibility databases for clinical trials and EMRs and then match those results with clinical trials that are recruiting participants through social media, trial announcements, or registries. Patients can contact investigator sites to have their eligibility assessed and become more aware of clinical studies that interest them sooner. There has been a 58.4% increase in enrolment for lung cancer thanks to AI-based clinical trial matching [20]. A wearable device is not connected to any other nonwearable device. However, it fully functions when connected to the user/patient body either directly or indirectly through clothing, which can perform measurements or data processing tasks. Wearable technology and machine learning models have been used to monitor trial participants for Parkinson's disease, automatically identify cognitive and emotional states, and evaluate sleep quality in neurology trials [24].
AI in drug development faces data hurdles, including digitizing and accessing medical records (EMR). Standardizing data formats across wearables and EMRs is a challenge. Mining large, scattered datasets (genes, trials, articles) is complex. Privacy regulations limit data access, adding to legal hurdles. Data privacy regulations limit access to specific patient data. Similar legal hurdles about data security and impact clinical trial matching [1, 25]. The Food and Drug Administration (FDA) [23] considers software with an AI or ML component a medical device. For technical certification, clinical, quality systems, sophisticated machine learning research, safety and efficacy assurance, transparency, and real-world performance management, the FDA wants AI developers with any new technology that claims artificial intelligence (AI) compliance with these standards in order to enhance the efficiency of clinical design and execution, additive testing intended should be as addition or replacement should be certified [26].
4 AI technologies in clinical research
AI helps to find the right patient for research studies, analyse data, and plan studies better. This improves the research faster and helps find better results, which makes it more efficient and outcomes more precise [27]. One such use is in Patient Recruitment using AI, which is a critical phase in clinical trials and AI has brought innovation in this area and has shown to be a game changer for solving the problem of patient recruitment [5]. Natural Language Processing (NLP) and Text Mining NLP and text mining technology extract precious insights from scientific literature, electronic health statistics (EHRs), and scientific reports. They permit researchers to get entry to a wealth of unstructured statistics, facilitating literature opinions, unfavourable event tracking, and the identification of relevant patient cohorts. NLP-powered tools like IBM Watson aid in fact extraction and interpretation [28].
5 Real-world examples of successful AI-driven clinical trials
AI is advancing clinical trials by identifying ideal patients, optimizing designs, and predicting treatment responses, leading to faster development and improved patient outcomes.
5.1 Use of AI in oncology clinical trials
Data-driven algorithms combined with real-world patient data have potentially improved many areas of clinical trials [29]. Clinical trials for cancer have been transformed in recent years by AI technology, making research more productive and successful trials [30]. AI-based early detection and diagnostic systems have been used for the analysis of CT scans, X-ray, and other medical imaging data. For example, research by Hamamoto et al. indicates that using AI in radiography to identify cancer has led to faster and more accurate results in clinical trials [31, 32]. Individualised Care Artificial intelligence is used to analyse patient data and create plans. These plans take into account the patient's current health status, past treatment outcomes, and genetic profiles. Studies have demonstrated how AI might enhance anti-cancer medication design, leading to more individualised treatment [20]. Artificial intelligence has improved the accessibility of clinical trial patient monitoring and recruitment. Analysing relevant databases and electronic health information can help find potential candidates. Real-time patient data provided by AI-powered technologies also guarantees a greater adherence to trial protocols. The ability of AI models to predict patient reactions to diverse treatments is essential for improving clinical trial designs. By selecting the most promising therapies, these predictive powers increase the possibility that clinical trials will be successful [20]. AI applications in cancer clinical trials create ethical issues and must adhere to regulatory requirements. To guarantee that AI algorithms are open, objective, and respectful of patient privacy, safeguards are required [30].
5.2 Use of AI in Glaucoma trials
Automated systems such as Artificial Intelligence (AI) could be used to identify diseases in a large population. However, several issues may arise throughout the AI pipeline, including inappropriate bias, health disparities, and decreased equity. AI applications in ophthalmology have primarily focused on conditions affecting the posterior portion of the eye [33, 34]. AI has demonstrated the potential to help diagnose illness and predict its progression, such as identifying changes in photoreceptors in choroideremia and retinitis pigmentosa, as well as Retinal Nerve Fiber Layer (RNFL) loss in multiple sclerosis. Optical Coherence Tomography (OCT) AI systems have also employed technology to connect structural and functional changes in glaucoma, with the retinal ganglion cell axonal complex optimised approach showing good predictive value in predicting Visual Field (VF) thresholds using OCT images [35]. To help treat glaucoma, AI must be able to determine the possibility of glaucoma and track the disease's progression. An objective, verified, and standardised definition of glaucoma is needed to act as a ground truth for cases used to train the system. The automated detection of intermediate glaucoma, when patients start to exhibit VF anomalies or functional changes and are more likely to develop visual impairment over their lifespan, should be the primary focus of AI research [36, 37].
Parameters for diagnosis include the Optic Nerve Head (ONH) cup-to-disc ratio, Retinal Nerve Fiber Layer (RNFL) thickness, and Ganglion Cell-Inner Plexiform Layer (GCIPL) thickness. Fundus photography and quantitative OCT image processing are significant choices for AI-assisted glaucoma diagnosis, as they help identify retinal abnormalities and test for eye illness. Patient's eyes can be imaged in community settings and primary care offices using portable fundus cameras. Extensive, diverse training and validation sets that have been clinically validated against outcome or other prognostic standards are required [33]. Support from numerous centers worldwide is required, and cost savings must be shown for AI to become a popular tool for managing glaucoma. By identifying glaucoma early on, patients can avoid more involved and expensive operations, lowering expenses both personally and globally [37].
6 Regulatory challenges in AI-driven clinical trials
Regulatory concerns around AI in clinical trials have proven to be challenging for all the global regulators, which need to be identified and understand the issues causing it. A few of the regulatory challenges are discussed further:
7 Lack of regulatory guidance
Artificial Intelligence in medical trials lacks complete regulatory development due to several elements. Firstly, the rapid evolution of AI technologies makes it hard for regulators to maintain pace with new packages and algorithms. Additionally, the range of AI technologies utilised in medical trials, including system studying and natural language processing, necessitates unique pointers for each, in addition to complicating the regulatory panorama [5]. AI in trials faces data privacy, security, and ethical concerns (bias, transparency). International harmonization is crucial due to transnational research. Limited data on AI safety and efficacy hinders comprehensive guidelines. Regulators are working on frameworks to address these challenges [8].
8 Data availability and standards
For artificial intelligence (AI) to be applied ethically and successfully in clinical trials and healthcare, it is imperative that data-related issues and ethical challenges be addressed. Legislators, data scientists, and medical experts must collaborate across fields to solve ethical issues within the use of AI, including biases among the patients, justice, and benefits [38]. The integrity of clinical trial data should be preserved by regulators by establishing criteria for data security and quality of the data. This comprises procedures for data purification to get rid of mistakes and inconsistencies [39, 40]. Additionally, data sharing and interoperability standards are essential, enabling effortless communication between various healthcare systems and AI tools [41]. These process protects patient data and encourage ethical considerations of AI applications in healthcare, which will eventually improve patient results [16].
9 Ethical considerations
The rapid advancement of AI in healthcare demands ethical guidelines to ensure its responsible use. These guidelines act as a framework to maximize the benefits of AI while minimizing potential risks. They typically focus on core principles like patient autonomy, safety, inclusivity, risk minimization, reliability, and accountability [27]. For instance, the Indian Council of Medical Research (ICMR) placed a strong focus on fairness, validity, and reliability in its ethical guidelines for artificial intelligence (AI) in healthcare. These suggestions address all of the important aspects of AI, such as the requirement for informed consent, data security, and preventing bias in algorithms [42]. Ensuring AI technology conforms with ethical and legal criteria is the aim, since it promotes safety, trust, and equitable healthcare results. As AI's role in healthcare and research grows, adherence to such ethical guidelines is becoming more and more crucial to safeguard patients and the integrity of medical procedures [40].
10 Evaluation criteria
Medical device management poses a distinct problem, encompassing machine learning and artificial intelligence (AI). AI-based medical devices must comply with dynamic and changing rules that call for specialist evaluation criteria, in contrast to traditional medical devices that are subject to a regulatory framework centered on safety and efficacy [43]. While specific laws are lacking, best practices are emerging to govern AI in healthcare. Organizations worldwide recognize the need for ethical, inclusive, transparent, and efficient AI development and assessment criteria [44]. Given the dynamic nature of AI technology and its potential to impact patient safety and healthcare results, it is imperative to broaden the scope of the requirements in order to guarantee its responsible application in the medical field [13]. These ongoing efforts aim to balance innovation and patient safety in the rapidly advancing field of AI in medical devices.
11 Regulatory initiatives
11.1 FDA's flexible framework
The FDA is aggressively developing a flexible, chance-based regulatory framework to leverage artificial intelligence and machine learning (AI/ML) capabilities inside the pharmaceutical industry. This framework is intended to promote the safe and reliable integration of AI-powered equipment during the phases of drug development and scientific trials [43]. The FDA's strategy acknowledges that the use of AI and ML technologies can significantly speed up the discovery of new drugs and enhance the efficacy and stability of existing ones. The hazards of applying AI/ML in healthcare are taken into account in the FDA policy. It aims to offer suitable oversight based on possible advantages and hazards, allowing for the acceleration of low-risk technology while upholding thorough evaluations for high-risk applications [45]. To determine if AI-powered tools are as safe and effective as conventional medications, the FDA is dedicated to making sure that these tools are extensively studied. Establishing norms and regulations for creating and utilising AI/ML in healthcare is part of this [46]. The framework's goals are to lower obstacles, streamline the regulatory procedure for AI/ML applications, and improve industry uptake. In general, the FDA's accommodating stance on AI/ML in medicine shows a progressive mindset that maximizes the technology's potential while protecting patient safety and treatment options [47].
11.2 European medicines agency (EMA)
The EMA is focused investigating the use of artificial intelligence (AI) in clinical trials. In July 2023, the EMA released a reflection paper outlining current thinking on using AI to develop safe and effective medicines. This paper reflects EMA's recognition of AI's potential for medicine and the tests that are effective [48]. EMA's interest in AI extends to clinical trial design, where AI can transform key steps in study preparation and execution, ultimately increasing trial success rates and reducing costs [49]. Regulatory guidance on AI in medicine and its application in medicine is being developed, focusing on areas such as data generation. In summary, the EMA has been involved in the research and planning of using AI in clinical trials in recognition of its transformative potential in pharmaceutical and clinical research [50, 13].
11.3 The national medical product administration (NMPA)
Regarding the application of artificial intelligence (AI) in clinical trials, China has been actively adopting rules and standards. One of the key elements of Chinese regulation is the requirement for careful planning and design of research projects. In order to obtain reliable and valid trial results, careful consideration is given to choosing an appropriate sample size, establishing control groups, and using the right procedures [51]. Recruitment and patient retention are also covered by Chinese policies. It is advised to use strategies including expanding the reach of recruitment websites, integrating patient advocacy groups, and making use of electronic health data. China places a high value on observing moral standards and obtaining informed agreement before enforcing regulations. Protecting patient privacy and maintaining data integrity are crucial. Increasing openness and simplifying procedures for regulation are two more important aspects to take into account [52]. China has implemented regulations and procedures that govern the use of AI in clinical studies [53].
11.4 The central drugs standard control organization (CDSCO)
The potential of AI to revolutionize clinical trials has been welcomed by the Indian Council of Medical Research (ICMR). There are various advantages of employing AI in clinical trials in India. AI can, among other things, make it simpler to identify patients for clinical trials by looking through patient data and electronic health records [54]. This increases recruitment efficacy by enabling researchers to identify candidates more quickly. In addition, massive datasets may be analysed by AI-driven algorithms to identify potential safety concerns and unfavourable occurrences, ensuring study participant safety. AI can also enhance trial techniques, leading to less costly and time-consuming research. The promise of AI in clinical trials has prompted the ICMR and CDSCO to take the lead [55]. With a range of stakeholders, they have developed frameworks and rules to regulate the use of AI in clinical studies. The need of data protection, transparency, and ethical considerations while utilising AI in medical research is emphasised by these proposals. Furthermore, the ICMR and CDSCO have launched pilot programmed to assess the practicality and effectiveness of AI in clinical trials. Although there is a lot of promise for using AI in clinical trials in India, there are a few challenges that need to be solved. Interoperability, standardisation, and the availability and quality of data are major challenges [7]. It is also important to carefully consider the ethical and legal implications of using AI in clinical research. The use of AI in clinical trials by the ICMR and CDSCO demonstrates India's dedication to use cutting-edge technology to enhance medical research [56]. Through the use of AI, they want to accelerate the creation of novel therapies, lower expenses, and increase patient safety—all of which will help the worldwide endeavour to improve healthcare outcomes [57]. This progressive approach underscores India's position as a burgeoning hub for clinical research and innovation in the pharmaceutical sector [58].
12 Specific regulatory considerations for the use of AI in clinical trials
Guidelines for Good Clinical Practice (GCP) are essential for integrating AI and machine learning in clinical studies. The conduct of these studies will be ethically sound and prioritise patient safety and data integrity if GCP guidelines are followed [59]. Regarding AI uses in clinical trials, regulatory scrutiny by organisations like the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) has increased. These organisations assess the application of AI and machine learning in several trial-related areas, including patient selection, dosage, and product design. The FDA's proposed risk-based regulatory framework intends to evaluate the degree of risk connected to AI uses in medication development. With the help of this framework, it is possible to adjust the regulatory requirements following the perceived risk [60]. Transparency and comprehensibility are crucial components when using AI models in clinical trials. Regulatory bodies emphasise the requirement for sponsors to provide evidence of the decision-making processes used by AI algorithms to protect the integrity and openness of the trial. Clinical studies must include thorough and accurate documentation of AI-related activities. The use of AI in trial design, data analysis, and decision-making must be fully documented by sponsors [61].
13 The future of AI in clinical trials
A significant role for generative AI is being played in patient eligibility and recruiting. AI systems can analyse enormous volumes of data to identify the best applicants, cutting down on hiring-related expenses and delays. Another useful use is predictive analytics, where AI analyses past test data to forecast results and assist researchers in making defensible choices [40]. Real-time analytics using AI-powered sensors and wearables enable continuous data collection, ensure faster discovery of problems, and improve data quality. Moreover, AI-driven drug discovery accelerates the development of new therapies by identifying and optimizing potential drugs [13]. Finally, AI facilitates adaptive test design, adjusting test parameters based on emerging data to increase performance. Some emerging trends in AI applications for clinical trials, are summarized in Table 2.
13.1 Recruitment optimization
AI is increasingly being used to identify suitable candidates for clinical trials, reducing recruitment time and costs. It has shown remarkable results in clinical trials. Researchers are increasingly turning to AI to improve recruitment, especially by finding the right people for these trials [62]. AI uses patient profiles, medical records, and social media data to screen potential participants better and compare them to the most appropriate clinical trials; if this approach is for professionals, the hiring process will be faster and reduce associated time and costs [63]. The use of AI technology in clinical trial recruitment improves enrollment rates, ultimately resulting in more successful trial outcomes. Scientific journals have recognized the power of AI in this area, underscoring its potential to transform recruitment in clinical trials [40].
13.2 Predictive analytics
Artificial Intelligence (AI)-pushed predictive models are instrumental in forecasting various crucial elements of clinical trials, including trial outcomes, affected person responses, and protection profiles. By leveraging massive datasets and complex algorithms, AI can provide valuable insights into how a scientific trial will spread. One of the most significant blessings of AI-driven predictive analytics is the early identification of capacity problems [22]. Researchers can hit upon anomalies or deviations from expected consequences, enabling quicker choice-making and the adjustment of study parameters. This enhances the overall efficiency of medical trials and is essential to affected persons' safety. Early identification of adverse occasions or safety issues permits fast intervention, ensuring the well-being of participants. Scientific journals have significantly documented the positive effect of AI-pushed predictive analytics on clinical trials, recognizing its capability to streamline studies strategies, lessen fees, and improve the overall success charge of studies [5, 63].
13.3 Real-world data analysis
Traditionally, drug efficacy has been monitored through randomised clinical trials, limited by the ability to capture real-world scenarios and patient experiences. The use of AI empowers researchers and healthcare providers to explore more real-world data with electronic health records and wearable data [64]. AI tools can identify patterns, relationships, and trends in this data, find effective drugs for patient populations, identify potential side effects, and diagnose unexpected benefits or risks. This in-depth understanding of drug action by health professionals can inform more informed decisions by regulators and pharmaceutical companies [65, 66]. AI tools can also help identify subgroups of patients who may respond differently to a drug, enabling personalized treatments. However, challenges such as data privacy and security, addressing biases in data, and maintaining transparency and interpretability are critical to fully harnessing the potential of AI in this field [62].
13.4 Natural language processing (NLP)
Algorithms are transforming healthcare by analyzing medical records. They automate tasks like coding and data entry, freeing doctors for patient care. NLP a special type of algorithm, extracts valuable information from clinical data, even unstructured records. This allows for improved diagnosis, treatment plans, and identification of adverse drug reactions. As NLP advances, even better patient care and medical research breakthroughs are expected [64].
14 The ethical and regulatory implications of using AI in clinical trials
The increasing use of artificial intelligence (AI) in clinical trials brings ethical and regulatory challenges. Ethically, concerns are centered around data availability, standards, and privacy. Integrating AI requires ensuring data privacy and obtaining informed consent, especially when patients may not fully understand the implications of AI data usage. Additionally, addressing bias in AI algorithms is essential to prevent unequal treatment and outcomes [67]. On the regulatory front, specialized approaches to regulating AI in healthcare are necessary due to their complexity and potential impact on patient safety and data protection. Balancing the foreseen benefits of AI in clinical trials with these ethical and regulatory considerations is crucial to harness its full potential responsibly [6].
14.1 AI liability in clinical trials
In clinical trials the investigators might face failure scenarios related to incorrect diagnosis due to programming errors or biased training data sets available. AI developers can be stand accountable for hardware malfunction or any design flaws leading to patient harm. The sponsors and data providers can be liable for data breaches, failure in monitoring the patient confidentiality. However, clearer guidelines and robust safeguards are essential to minimize risks and protect all data used for conducting the trials [68, 69].
14.2 Current legislation and potential remedies on liability
Liability for AI use in clinical trials is governed by a mix of international and national regulations, frameworks like the European Union’s general Data Protection Regulation (GDPR) address data protection and privacy, crucial for handling patient data in AI based clinical trials. The European Union proposed AI Act which aims to set comprehensive rules for AI usage, including in healthcare. The U.S. Food and Drug Administration (FDA) provides guidance on AI in Medical devices, focusing on safety and efficacy. The UK MHRA has its own AI strategy, emphasizing ethical considerations and regulatory compliances. Potential remedies for liability include stringent validation processes, regular audits, and adherence to best practices for AI development and deployment [44, 48]. Establishing clear accountability, enhancing transparency, and ensuring robust data protection are essential to mitigate risks and safeguard all stakeholders in clinical trials. Global harmonization efforts are underway to develop international standards and guidelines for AI in healthcare, such as World Health Organization (WHO) and the Organization for Economic Cooperation and Development (OECD). Moreover, it is essential to stay updated on the rapidly changing legal landscape to effectively manage AI-related risks in clinical trials. Consulting with legal experts specializing in AI and healthcare law is crucial for navigating the complexities of this area [7, 15, 68].
15 Conclusion
AI can design more effective studies, analyze vast amounts of data, improve upon data analysis, patient recruitment, and trial design. AI algorithms can analyze large datasets and identify trends that might indicate treatment effectiveness or side effects. Nevertheless, ethical and regulatory considerations must be addressed. Regulatory agencies must develop frameworks to encourage transparency, patient safety, and data integrity. Artificial intelligence applications include image analysis, natural language processing, and personalised treatments. As artificial intelligence (AI) continues to influence medicine, it is critical to strike a balance between innovation and patient safety while maintaining transparency and responsibility. By implementing solid laws and encouraging ethical AI use, we can unlock the full potential of AI in clinical studies, paving the way for a more efficient, effective, and patient-centered future of drug discovery.
References
Bhatt A. Artificial intelligence in managing clinical trial design and conduct: Man and machine still on the learning curve? Perspect Clin Res. 2021;12:1–3.
Ramesh AN, Kambhampati C, Monson JRT, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004;86:334–8.
Cramer G. Forward Thinking for the Integration of AI into Clinical Trials [Internet]. ACRP. 2023 [cited 2023 Sep 26]. Available from: https://www.acrpnet.org/2023/06/forward-thinking-for-the-integration-of-ai-into-clinical-trials/
A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities - ScienceDirect [Internet]. [cited 2023 Sep 26]. Available from: https://www.sciencedirect.com/science/article/pii/S2444569X2300029X
Pharmaceuticals | Free Full-Text | The role of AI in drug discovery: challenges, opportunities, and strategies [Internet]. [cited 2023 Sep 26]. Available from: https://www.mdpi.com/1424-8247/16/6/891
Research C for DE and. Artificial Intelligence and Machine Learning (AI/ML) for Drug Development [Internet]. FDA. FDA; 2023 [cited 2023 Oct 2]. Available from: https://www.fda.gov/science-research/science-and-research-special-topics/artificial-intelligence-and-machine-learning-aiml-drug-development
Ethical_Guidelines_AI_Healthcare_2023.pdf [Internet]. [cited 2023 Oct 2]. Available from: https://main.icmr.nic.in/sites/default/files/upload_documents/Ethical_Guidelines_AI_Healthcare_2023.pdf
Artificial Intelligence Applied to clinical trials: opportunities and challenges | SpringerLink [Internet]. [cited 2023 Oct 1]. Available from: https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s12553-023-00738-2
Zhong F, Xing J, Li X, Liu X, Fu Z, Xiong Z, et al. Artificial intelligence in drug design. Sci China Life Sci. 2018;61:1191–204.
Estimation of clinical trial success rates and related parameters | Biostatistics | Oxford Academic [Internet]. [cited 2023 Oct 18]. Available from: https://academic.oup.com/biostatistics/article/20/2/273/4817524
Calaprice-Whitty D, Galil K, Salloum W, Zariv A, Jimenez B. Improving clinical trial participant prescreening with Artificial Intelligence (AI): A comparison of the results of AI-assisted vs standard methods in 3 oncology trials. Ther Innov Regul Sci. 2020;54:69–74.
Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Artificial Intelligence in Healthcare. 2020;1(1):25–60. https://doi.org/10.1016/B978-0-12-818438-7.00002-2.
Harrer S, Shah P, Antony B, Hu J. Artificial intelligence for clinical trial design. Trends Pharmacol Sci. 2019;40:577–91.
Vuksanaj K. AI in Clinical Trials Reality versus Hype [Internet]. GEN - Genetic Engineering and Biotechnology News. 2023 [cited 2023 Oct 1]. Available from: https://www.genengnews.com/topics/artificial-intelligence/ai-in-clinical-trials-reality-versus-hype/
BDCC | Free Full-Text | Artificial intelligence in pharmaceutical and healthcare research [Internet]. [cited 2023 Oct 1]. Available from: https://www.mdpi.com/2504-2289/7/1/10
The Evolution Of Clinical Trials: The Promise Of AI And The Role Of Big Tech [Internet]. [cited 2023 Oct 1]. Available from: https://www.cbinsights.com/research/clinical-trials-ai-tech-disruption/
Jeyaraman M, Balaji S, Jeyaraman N, Yadav S. Unraveling the ethical enigma: artificial intelligence in healthcare. Cureus. 2023;15(8). https://doi.org/10.7759/cureus.43262.
Kolluri S, Lin J, Liu R, Zhang Y, Zhang W. Machine learning and artificial intelligence in pharmaceutical research and development: a review. AAPS J. 2022;24:19.
Chan HCS, Shan H, Dahoun T, Vogel H, Yuan S. Advancing drug discovery via artificial intelligence. Trends Pharmacol Sci. 2019;40:592–604.
Wang L, Song Y, Wang H, Zhang X, Wang M, He J, et al. Advances of artificial intelligence in anti-cancer drug design: a review of the past decade. Pharmaceuticals. 2023;16:253.
Burki T. A new paradigm for drug development. Lancet Digit Health. 2020;2:e226–7.
Sarkar C, Das B, Rawat VS, Wahlang JB, Nongpiur A, Tiewsoh I, et al. Artificial intelligence and machine learning technology driven modern drug discovery and development. Int J Mol Sci. 2023;24:2026.
Niazi SK. The coming of age of AI/ML in drug discovery, development, clinical testing, and manufacturing: the FDA perspectives. Drug Des Devel Ther. 2023;17:2691–725.
Vora LK, Gholap AD, Jetha K, Thakur RRS, Solanki HK, Chavda VP. Artificial intelligence in pharmaceutical technology and drug delivery design. Pharmaceutics. 2023;15:1916.
Pharmaceuticals | Free Full-Text | Advances of Artificial Intelligence in Anti-Cancer Drug Design: A Review of the Past Decade [Internet]. [cited 2023 Oct 19]. Available from: https://www.mdpi.com/1424-8247/16/2/253
Selvaraj C, Chandra I, Singh SK. Artificial intelligence and machine learning approaches for drug design: challenges and opportunities for the pharmaceutical industries. Mol Divers. 2022;26:1893–913.
Frontiers | Scoping review of the current landscape of AI-based applications in clinical trials [Internet]. [cited 2023 Oct 2]. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.949377/full
Scopus preview - Scopus - Document details - Deep learning [Internet]. [cited 2023 Oct 18]. Available from: https://www.scopus.com/record/display.uri?eid=2-s2.0-84930630277&origin=inward&txGid=4af35adae0520473f8fee302d0db19d8
Liu R, Rizzo S, Whipple S, Pal N, Pineda AL, Lu M, et al. Evaluating eligibility criteria of oncology trials using real-world data and AI. Nature. 2021;592:629–33.
Dong J, Geng Y, Lu D, Li B, Tian L, Lin D, et al. Clinical trials for artificial intelligence in cancer diagnosis: a cross-sectional study of registered trials in ClinicalTrials.gov. Front Oncol. 2020;10:1629.
Application of Artificial Intelligence Technology in Oncology: Towards the Establishment of Precision Medicine - PMC [Internet]. [cited 2023 Oct 19]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7760590/
Region Örebro County. Artificial Intelligence Supporting CAncer Patients Across Europe - the ASCAPE Project [Internet]. clinicaltrials.gov; 2022 Oct. Report No.: NCT04879563. Available from: https://clinicaltrials.gov/study/NCT04879563
Yousefi S. Clinical applications of artificial intelligence in glaucoma. J Ophthalmic Vis Res. 2023;18:97–112.
Application of artificial intelligence in ophthalmology - PMC [Internet]. [cited 2023 Oct 21]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6133903/
The application of artificial intelligence in glaucoma diagnosis and prediction - PMC [Internet]. [cited 2023 Oct 21]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10192631/
Artificial Intelligence Algorithms to Diagnose Glaucoma and Detect Glaucoma Progression: Translation to Clinical Practice - PubMed [Internet]. [cited 2023 Oct 21]. Available from: https://pubmed.ncbi.nlm.nih.gov/33117612/
Artificial Intelligence for Glaucoma: Creating and Implementing Artificial Intelligence for Disease Detection and Progression - PubMed [Internet]. [cited 2023 Oct 21]. Available from: https://pubmed.ncbi.nlm.nih.gov/35218987/
Siala H, Wang Y. SHIFTing artificial intelligence to be responsible in healthcare: A systematic review. Soc Sci Med. 2022;296:114782.
Stöger K, Schneeberger D, Kieseberg P, Holzinger A. Legal aspects of data cleansing in medical AI. Comput Law Secur Rev. 2021;42:105587.
Askin S, Burkhalter D, Calado G, El Dakrouni S. Artificial intelligence applied to clinical trials: opportunities and challenges. Health Technol (Berl). 2023;13:203–13.
Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing [Internet]. Federal Register. 2023 [cited 2023 Oct 16]. Available from: https://www.federalregister.gov/documents/2023/04/18/2023-07229/health-data-technology-and-interoperability-certification-program-updates-algorithm-transparency-and
Ethical guidelines for application of Artificial Intelligence in Biomedical Research and Healthcare | Indian Council of Medical Research | Government of India [Internet]. [cited 2023 Oct 16]. Available from: https://main.icmr.nic.in/content/ethical-guidelines-application-artificial-intelligence-biomedical-research-and-healthcare
Health C for D and R. Artificial Intelligence and Machine Learning in Software as a Medical Device. FDA [Internet]. 2023 [cited 2023 Oct 18]; Available from: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device
EMA Regulatory Science to 2025 Strategic Reflection. https://www.ema.europa.eu/en/documents/regulatoryprocedural-guideline/ema-regulatory-science-2025-strategic-reflection_en.pdf.
Commissioner O of the. U.S. Food and Drug Administration [Internet]. FDA. FDA; 2023 [cited 2023 Nov 23]. Available from: https://www.fda.gov/
Research C for DE and. Digital Health Technologies (DHTs) for Drug Development. FDA [Internet]. 2023 [cited 2023 Oct 18]; Available from: https://www.fda.gov/science-research/science-and-research-special-topics/digital-health-technologies-dhts-drug-development
Commissioner O of the. Real-World Evidence [Internet]. FDA. FDA; 2023 [cited 2023 Oct 18]. Available from: https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence
EMA. Reflection paper on the use of artificial intelligence in lifecycle medicines [Internet]. European Medicines Agency. 2023 [cited 2023 Oct 18]. Available from: https://www.ema.europa.eu/en/news/reflection-paper-use-artificial-intelligence-lifecycle-medicines
The future of clinical trials and drug development: 2050 - PMC [Internet]. [cited 2023 Oct 18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10259497/
EMA. Artificial intelligence in medicine regulation [Internet]. European Medicines Agency. 2021 [cited 2023 Oct 18]. Available from: https://www.ema.europa.eu/en/news/artificial-intelligence-medicine-regulation
Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: A review - PMC [Internet]. [cited 2023 Oct 18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6092479/
He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30–6.
Privacy Protection in Using Artificial Intelligence for Healthcare: Chinese Regulation in Comparative Perspective - PMC [Internet]. [cited 2023 Oct 18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9601726/
Salalli R, Dange JR, Dhiman S, Sharma T. Vaccines development in India: advances, regulation, and challenges. Clin Exp Vaccine Res. 2023;12:193–208.
Clinical-Trials-in-India.pdf [Internet]. [cited 2023 Oct 19]. Available from: https://www.nishithdesai.com/fileadmin/user_upload/pdfs/Research_Papers/Clinical-Trials-in-India.pdf
Indian Council of Medical Research | Government of India [Internet]. [cited 2023 Nov 23]. Available from: https://main.icmr.nic.in/
Kaur H, Kaur M, Bhattacharyya A, Prajapat M, Thota P, Sarma P, et al. Indian contribution toward biomedical research and development in COVID-19: A systematic review. Indian J Pharmacol. 2021;53:63–72.
Guidelines | Indian Council of Medical Research | Government of India [Internet]. [cited 2023 Oct 19]. Available from: https://main.icmr.nic.in/content/guidelines-0
Herring FB Deeona R Gaskin, Josefine Sommer, Atiq Chowdhury, Maria-Oraiozili Koutsoupia, George. EU, U.S., and UK Regulatory Developments on the Use of Artificial Intelligence in the Drug Lifecycle [Internet]. Data Matters Privacy Blog. 2023 [cited 2023 Oct 18]. Available from: https://datamatters.sidley.com/2023/09/06/eu-u-s-and-uk-regulatory-developments-on-the-use-of-artificial-intelligence-in-the-drug-lifecycle/
EMA. Human medicines: regulatory information [Internet]. European Medicines Agency. 2018 [cited 2023 Oct 18]. Available from: https://www.ema.europa.eu/en/human-medicines-regulatory-information
Vijayananthan A, Nawawi O. The importance of Good Clinical Practice guidelines and its role in clinical trials. Biomed Imaging Interv J. 2008;4:e5.
Cascini F, Beccia F, Causio FA, Melnyk A, Zaino A, Ricciardi W. Scoping review of the current landscape of AI-based applications in clinical trials. Front Public Health. 2022;10:949377.
Weissler EH, Naumann T, Andersson T, Ranganath R, Elemento O, Luo Y, et al. The role of machine learning in clinical research: transforming the future of evidence generation. Trials. 2021;22:537.
Zhou B, Yang G, Shi Z, Ma S. Natural Language Processing for Smart Healthcare. IEEE Rev Biomed Eng. 2022;17:1–17. https://doi.org/10.1109/RBME.2022.3210270.
Dash S, Shakyawar SK, Sharma M, Kaushik S. Big data in healthcare: management, analysis and future prospects. Journal of Big Data. 2019;6:54.
Application of artificial intelligence in medical technologies: A systematic review of main trends - Olga Vl Bitkina, Jaehyun Park, Hyun K. Kim, 2023 [Internet]. [cited 2023 Oct 18]. Available from: https://journals.sagepub.com/doi/10.1177/20552076231189331
Reddy S. Navigating the AI revolution: the case for precise regulation in health care. J Med Internet Res. 2023;25:e49989.
Cestonaro C, Delicati A, Marcante B, Caenazzo L, Tozzo P. Defining medical liability when artificial intelligence is applied on diagnostic algorithms: a systematic review. Front Med. 2023. https://doi.org/10.3389/fmed.2023.1305756.
Naik N, Hameed BMZ, Shetty DK, Swain D, Shah M, Paul R, Aggarwal K, Ibrahim S, Patil V, Smriti K, Shetty S, Rai BP, Chlosta P, Somani BK. Laegal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front Surg. 2022;9(862322):1–6. https://doi.org/10.3389/fsurg.2022.862322.
Acknowledgements
The authors would like to acknowledge colleagues and faculties for their valuable inputs.
Funding
The authors disclose having no funding for the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The manuscript did not require any ethical approval.
Consent to participate
No consents were required for the manuscript.
Consent to publish
All authors of the manuscript have consented for its publication.
Conflict of interest
The authors do not have any conflict of interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mourya, A., Jobanputra, B. & Pai, R. AI-powered clinical trials and the imperative for regulatory transparency and accountability. Health Technol. (2024). https://doi.org/10.1007/s12553-024-00904-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12553-024-00904-0