Abstract
This paper was aimed at determining a way to create an EMG signal in muscle tissue, and identify factors that affect this signal. We also studied the methods for recording and filtering this signal in order to control a prosthetic limb such as a hand. A new method is discussed for controlling a prosthetic limb capable of interacting with brain and the nervous system. In this system, which is called IMES (Implantable Myoelectric Sensor), EMG signals were recorded using a series of Implantable Myoelectric Sensors. These signals were then transmitted to a telemetry controller for analysis using a wireless system. The system developed here allows the acquired data to be sent to a prosthetic limb controller and move the prosthetic limb toward patient's desired directions without wiring or a surgical procedure to implant the controller under the skin. It is also possible to monitor the data from EMG signals via a USB port or an external computer connected to the IMES system. Our results indicate that we can record the EMG signals without noise via implantable myoelectricsensors and telemetry controller in an IMES system. This allows to control a prosthetic hand based on the brain and nervous system's commands.

ᅟ
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Biomechatronics is the connection between human and machine. It is an interdisciplinary science, which encompasses biology, neuroscience, mechanics, electronics, and robotics. Biomechatronics attempts to design devices, which interact with muscles, skeleton, and the human nervous system. Such devices help those whose motion control has been disrupted and/or those who have lost an organ congenitally or due to a disease in order to continue their normal lives. However, this requires the analysis of human motions, which is very challenging. To control a Biomechatronics system, such as hand prosthesis, a multifunctional system with different modules is required. Figure 1 shows such a block scheme with a multifunctional system containing different modules for hand prosthesis.
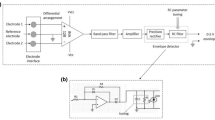
The study on how such Mechatronic devices may interface with the human nervous system is conducted based on recording of the control signals released from the brain to control muscles and body organs. These signals are called electromyography (EMG) signals. The EMG signals for controlling hand prosthesis require several processing steps. Figure 2 shows the block scheme of analysis of EMG signals for control of hand prosthesis [1, 2].
An EMG signal includes recording of the electric activity of a muscle, which is usually performed using a needle electrode. In addition, surface electrodes are used when recording of the overall activity of a muscle is required. Figure 3a and b show the surface and needle electrode. EMG is used to assess and record the physiological characteristics of muscles at rest and during contraction. The EMG records an image called electromyogram using an electromyograph. An electromyograph specifies the electric potentials generated by muscle cells at rest and during contraction. Figure 4 shows an EMG signal [3].
The electrical source for the EMG signal is the muscle membrane potential with a voltage of about 70 mV. The measured potentials obtained from the applied method has a range of about less than 50 μV to 20–30 mV. The iteration rate is a type of 7–20 Hz muscle stimulation unit whose accurate value depends on muscle size. Figure 5 shows the EMG signal in a muscle when it is contracted. A range of 450–780 mV can be expected when stimulation units are exposed to injuries [4].
In previous studies, to receive EMG signals some implantable myoelectric sensors were required to be implanted under the skin. Unfortunately, these invasive procedures are associated with infection and pain. In addition, the data transaction between prosthetics hand and EMG signals remain obscure. In this study, we utilized Otto Bock6 13E200 sensors to receive EMG signals. These sensors are more tolerable to external noises and can be used without a surgical procedure and damage to muscle tissues. In addition, it is possible to monitor the data transaction via a USB port or an external computer connected to the IMES system.
2 Methods
2.1 The EMG signal recording
A needle electrode is inserted through the skin into the muscle tissue for recording an intramuscular EMG signal. A neurologist/chiropractor observes the electric activity accurately while the electrode is inserted into the body. This activity during insertion of an electrode contains valuable data on muscle’s condition and its attached nerves. If a needle electrode is connected to the muscles while resting they will generate certain normal electric waves under normal conditions. An abnormal activity will indicate nerve and/or muscle injury. In this condition, a patient is requested to contract the muscle slowly for examining the shape, size, and frequency of the potentials obtained from the stimulation unit. The electrode is then inserted a few more millimeters into the muscle and the activity is reevaluated. This continues until collecting the responses of at least 10 to 20 units.
The effect of each electrode only provides a highly localized image of the activity of the whole muscle. As skeletal muscles vary in terms of their internal structure, the electrodes should be placed in different areas in order to obtain accurate information. However, an intramuscular EMG signal recording may be considered extremely aggressive and painful for most patients. Thus, a surface electrode can be used to demonstrate an overall image of muscle activity. This technique is used in some circumstances; for instance, the activity of a muscle is shown by a surface EMG in a physiotherapy clinic and patients realize when they activated a muscle using an audio-visual stimulation (biofeedback).
A stimulation unit is a stimulating neuron and all the muscle fibers connecting to it. When a stimulation unit is suddenly triggered, action potential of the stimulating neuron is transferred to the muscle. The area where a nerve connects to a muscle is called a neuromuscular junction or motor endplate. When the action potential was sent across the neuromuscular junction, a potential action is generated in all the muscle fibers connecting to the stimulating unit. Sum of all the electrical activity is known as a motor unit action potential (MUAP). The electrophysiological activity, which is obtained from several stimulating units is typically evaluated during the EMG signal. Stimulating unit structure, type of the muscle tissues of stimulating unit, metabolic type of muscle tissues, and many other factors affect the magnitude of the potentials in a stimulating unit [5].
2.2 The muscle membrane excitability
Muscle tissue excitability in neural control indicates the major factor of muscle physiology; an ionic balance between the inner and outer space of a muscle cell forms the resting potential in a muscle fiber membrane (when it is not at rest; i.e. in 80–90 mV range). Such a potential difference, which is maintained by physiological processes, leads to the negative charge inside the cell compared with outside of the cell surface. An endplate potential is formed in a muscle tissue with the release of neurotransmitters in the endplate of motor unit or neuromuscular junction. The propagation characteristics of muscle tissue membrane are adjusted briefly and +Na ions are flooded. This process leads to membrane depolarization, which is immediately replaced by the reverse exchange of ions in depolarization mechanism. This stimulation releases calcium ions in the intracellular space. An EMG signal is based on the action potentials of muscle fiber membranes, which are resulted from the described depolarization and depolarization process. The extent of depolarization area is shown in Fig. 6 that is almost 1–3 mm2 [6].
2.3 The nature of EMG signal
A raw EMG signal is the unfiltered and unprocessed signal, which tracks consistent MUAPs. Figure 7 shows a sample recording of a raw surface EMG signal for three static contractions of biceps. The utilized protocol was approved by the biomedical engineering faculty of Science and Research Branch-Islamic Azad University (SRBIAU), and all patients were consent and informed. Six able bodied subjects (mean age between 20 and 50) including three males and three females were enrolled in this study. We first evaluated patients for skin and tissue condition, and muscle strength and range of motion of the amputee limb. We next recorded EMG signals via surface electrodes. Figures 4 and 7 show EMG signals of three contractions for a bicep. Also, we utilized Otto Bock6 13E200 sensors to record EMG signals because this sensor is simply used as an electrode. Otto Bock’s 13E200 electrodes use a 100–400 Hz band pass filter and a 60 Hz notch filter. The resulting signal is then rectified and low-pass filtered. Figure 8 shows the steps for calibrating signal thresholds.
In the absence of depolarization and action potential, a healthy muscle at rest shows no specific EMG activity. Naturally, the drawn raw EMG signals are random shapes. This means that a signal recording cannot be exactly rebuilt again. This reveals that a set of employed motor unit consistently change in the matrix and/or diameter of the available motor units. If two or more motor units start activity at the same time with some electrodes in the vicinity they generate some bold lines, which are close to each other. By applying a paving algorithm and/or selecting a suitable domain parameter (absolute values of EMG signal), unrecognizable value of signals are removed or minimized (Fig. 8) [2, 5, 7].
2.4 The factors that affect EMG signal
An EMG signal is under the influence of different environmental factors on its course from the muscle membrane to electrodes, which alter its shape and characteristic. These factors are basically divided into the following groups:
-
a.
Texture characteristics
Human body is a good conductor of electricity, but this conductivity varies with respect to the type of tissue, thickness, physiological changes, and temperature. These conditions change considerably from one part to another, and prevent the quantitative comparison of the calculated parameters of the unprocessed amplitude of EMG signals.
-
b.
Physiological cross talk
Adjacent muscles generate a considerable amount of EMG signal, which are recorded at an electrode position. Normally, the cross link never exceeds 10–15 % of the whole EMG and/or there is no cross talk. However, precautions must be observed for the accurate adjustment in a muscle group. This way, the interference caused by the ECG signal while recording an EMG is identified and removed from the EMG signal by a series of algorithms, especially when the EMG is related to the upper limbs and shoulders. Figure 9 shows a raw EMG signal with conflicting ECG signal [7].
-
c.
Changes in geometry between ventricular muscle and range of electrodes
Any change in the distance between source of signal and tracking range affects reading signals. This is one of the major problems in dynamic motion studies and it can be affected by the outlet pressure.
-
d.
External noise
Necessary precautions should be observed in the environments with excessive noise. Maximum noise is generated due to inappropriate grounding and/or other external electronic equipment.
-
e.
Electrode and amplifiers
Quality of electrodes and internal noise of amplifiers may add some signal to baseline EMG. The internal noise of an amplifier should not exceed 5v rms. Most of these factors can be controlled and minimized by accurately preparing and controlling test conditions [8].
2.5 The method of controlling a prosthetic limb using an IMES system
EMG signal can be used for controlling Biomechatronic prosthetic limbs such as a hand after becoming familiar with the nature of EMG signal and its recording method. A multichannel EMG system was used in this method, which is capable of receiving and recording EMG signals by a series of Myoelectric sensors that can be implanted under the skin of an amputated limb. The system is known as “Implantable Myoelectric Sensor” (IMES).
An EMG signal is received by these implanted Myoelectric sensors. The signal is then transmitted to a (wireless) external telemetry controller, which is responsible for analyzing EMG signals. Needing no implantation of wires for the communication between sensors and controllers is considered an important advantage of this system, eliminating the need for fracture and surgery, and perhaps infection. In this system, each implantable sensor consists of an integrated circuit packed in a RFBION capsule. Figure 10 shows performance method of an IMES system [6, 9].
Eighteen external muscles in the hand and wrist control the arm, and the IMES system records the EMG signals of these muscles. As the signals are collected from several muscles, the system’s telemetry controller may perform a better and more accurate analysis of the received signals and consequently better estimate of issuing the required commands for moving the prosthetic limb in different directions. Figure 11 shows the diagram applied in the IMES system [10, 11].
3 Results and discussion
An IMES system consists of approximately 30 implantable Myoelectric sensors with an outer loop force, a receiving antenna, and a telemetry controller. The telemetry controller transmits data directly from connections to a controller or an external recording device. The prosthetic limb controller is responsible for executing the commands received from the telemetry controller. The telemetry data are used for determining a user’s intention and the messages, which control the prosthetic limb motor, are used for moving the prosthetic limb in different directions. The robust outer loop, receiving antenna, telemetry controller, and prosthetic limb controller are all placed in a prosthetic joint, and the user uses the mechanic interface in prosthetic components. The telemetry controller in the prosthetic limb coordinates RF transfer with any connection at the time of frequency division. In this way, the data from each connection may be collected using a receiver in the prosthetic limb. The telemetry controller rectifies the received messages and transfers the multichannel EMG data to the prosthetic limb [12, 13].
A USB port with an external computer is used in the test specimen for communicating with the telemetry controller. Consequently, it allows controlling the external computer, displaying connection parameters, and collecting EMG data. Figure 12 shows the diagram for the performance of telemetry controller [11, 14, 15]. These results also indicate that it is possible to control other prosthesis such as foot utilizing the method described here. Thus, the IMES system can be developed for other prosthetic limbs and it is a new subject for future research.
4 Conclusion
The tests carried out by the IMES system revealed that the implantable Myoelectric sensors create minimum aggression on the muscle tissue connecting to, and can record and accurately collect the EMG signals generated in the arm and forearm. Furthermore, no noise and interference were observed on the system’s recording data with respect to the use of the telemetry and wireless system for receiving EMG signals by the controller. The necessary commands were transmitted from telemetry controller to the controller of prosthetic limb for controlling prosthetic limb motion, which can be seen through the USB and an external computer.
Change history
20 December 2017
In the version of this article initially published, the affiliations of the authors were incorrectly written. The correct presentation is indicated in this paper.
References
C Freudenrich. How biomechatronics works. University of MIT; 2007.
Zecca M, Micera S, Carrozza MC, Dario P. Control of multifunctionalprosthetic hands by processingtheelectromyographic signal. ARTS Lab, ScuolaSuperioreSant’Anna, Pontedera, Italy; 2002.
Electronic Publication: www.bleng.com.
Ferris DP, Sawicki GS, Domingo AR. Powered lower limb orthoses for gait rehabilitation. University of Michigan; 2005.
Ajiboye AB, Weir RF. A heuristic fuzzy logic approach to EMG pattern recognition for multifunctional prosthesis control. IEEE Trans Neural Syst Rehabil Eng. 2005;13(3).
Lowery MM, Weir RF, Kuiken TA. Simulation of intramuscular EMG signals detected using Implantable Myoelectric Sensors (IMES). IEEE Trans Biomed Eng. 2006;53(10).
Chowdhury RH, Reaz MBI, Ali MABM, Bakar AAA, Chellappan K, Chang TG. Surface electromyography signal processing andclassification techniques. Department of Electrical, Electronic and Systems Engineering, UniversitiKebangsaan Malaysia, Bangi, Selangor 43600, Malaysia; 2013.
Arieta AH, Katoh R, Yokoi H, Wenwei Y. Development of a multi-DOF electromyography prosthetic system using the adaptive joint mechanism. Hongo: Laboratory of Bioinstrumentation and Biomechatronics, University of Chiba; 2006.
Dellon B, Matsouka Y. Prosthetics, exoskeletons, and rehabilitation. IEEE Robot Autom. 2007
Atzori M, Müller H. Control capabilities of myoelectric robotic prostheses by hand amputees: a scientific research and market overview. Information Systems Institute, University of Applied Sciences Western Switzerland, Sierre, Switzerland; 2015.
Rajangam S, Tseng P, Yin A, Lehew G, Schwarz D, Lebedev MA, et al. Wireless cortical brain-machine interface for whole-body navigation in primates. Duke University Medical Center, Durham, NC; 2016.
ParadaPuig JE, Rodriguez NEN, Ceccarelli M. A methodology for the design of robotic hands with multiple fingers, University of Los Andes, Faculty of Engineering, School of Mechanical Engineering. Int J Adv Robot Syst. 2008;5(2).
Moulianitis VC, Syrimpeis VN, Kokkinos V, Aspragathos NA, Panagiotopoulos EC. A closed-loop drop-foot correction system with gait event detection using fuzzy logic. Mechanical Engineering and Aeronautics Dept. University of Patras Greece; 2008.
Sensinger JW, Weir RF. User-modulated impedance control of a prosthetic elbow in unconstrained, perturbed motion. IEEE Trans Biomed Eng. 2008;55(3).
Ciancio AL, Cordella F, Barone R, Antonio Romeo R, Bellingegni AD, Sacchetti R, et al. Control of prosthetic hands via the peripheral nervous system. Unit of Biomedical Robotics and Biomicrosystems, Department of Engineering, Università Campus Bio-Medico di Roma, Roma, Italy; 2016.
Acknowledgments
We thank Dr. N. Sheibani with the preparation and editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
All human subjects were healthy adults and agreed to the parameters of this study by signing a consent form based on the Helsinki guidelines and approved by the Institutional Review Board of Science and Research Branch-Islamic Azad University (SRBIAU).
Six able bodied subjects (mean age between 20 and 50) including three males and three females were enrolled in this study. In the first step we evaluated patients such as observation of skin condition, tissue condition, muscle strength and rang of motion an amputee limb. After this step, we recorded EMG signal via surface electrodes. Also, we utilize Otto Bock6 13E200 sensors to record EMG signals because this sensor is used simply as an electrode. Otto Bock’s 13E200 electrodes use a 100–400 Hz band pass filter and a 60 Hz notch filter.
A correction to this article is available online at https://doi.org/10.1007/s12553-017-0213-3.
Rights and permissions
About this article
Cite this article
Sheibani, A., Pourmina, M.A. Study and analysis of EMG signal and its application in controlling the movement of a prosthetic limb. Health Technol. 6, 277–284 (2016). https://doi.org/10.1007/s12553-016-0142-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-016-0142-6