Abstract
This study investigates the process of operating room scheduling at a surgery department in a Midwestern hospital. A comprehensive process map was developed to depict the existing scheduling process and enhance understanding of the complexity of hospital operations. Close examination of the process map suggests several obstacles and bottlenecks that impede operation efficiency of the investigated surgery department. The implications for IS research are also discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The hospital industry is struggling with diminishing investment returns. On one side, rising cost of health maintenance, more regulations on government reimbursements for Medicare and Medicaid services, and changing policies from insurers have increased the burden on hospital management [23]; on the other side, the public have increasingly criticized the hospital industry for the rising health care expenditures, making it sensitive for hospitals to increase service charges. As a result, the hospital industry in general operates on low profit margins, and 30 % hospitals are in fact losing money [2]. Thus, hospital CEOs have to pay “day-to-day attention to operations and logistics” for improving their financial bottom lines [31; p. 77].
Researchers have also pinpointed operation inefficiency as the main obstacle in the development of the hospital industry. For example, the Frontiers of Health Services Management journal devoted a special issue addressing the patient flow/capacity management problem; the issue concluded that “the repetitive theme that problems initially misconstrued as an apparent limitation of capacity are instead caused by inefficiencies in clinical hospital operations” [49; p. 34]. The international management consulting firm McKinsey & Company suggests the hospital industry redesigning its operation processes in order to enhance operation efficiency and boost up the declining profit margin, arguing that “today’s challenges demand nothing less than a fundamental rethinking of the health system in the United States” [19]. Given that the evolution of information technology is driven by operation efficiency and collaboration [40], there is an urgent need for more IS research in the hospital industry.
This study investigates the operating room scheduling process of typical US hospitals. The need for this study emanates from the purported impact of operating room scheduling on inefficiencies in clinical operations in the surgery department of a Midwestern mid-sized hospital; selected as the research target. This hospital faces the following problems of significance at the operation level which have the potential cascading effect of causing inefficiencies throughout the hospital operations.
-
1.
Conflict among physician’s requirement for operating rooms which arises due to unique scheduling demands made by Physicians for this scarce resource.
-
2.
Conflict among other resources’ allocation which support Physicians at the operating room. For example, trained operating room staff, such as nurses.
-
3.
Rescheduling problems for the operating rooms due to exigencies, such as a procedure taking longer than planned in the schedule, cancellations etc.
-
4.
Operating room capacity utilization problems due to uneven scheduling, such as a majority of procedures performed during morning hours, leading to unutilized capacities and thus lost revenue stream and accumulated overhead costs due to non-utilization and thus idling of available supporting resources.
A common thread in the characterization of the above problems is lack of information sharing among stakeholders, such as hospital administrators, physicians, and nurse managers; leading to unmanageable schedules that cause inefficiencies in clinical operations.
The objective of this study is to investigate whether the established scheduling theories can be complemented with IS theories relating to information sharing in a collaborative environment that can improve operational efficiencies and optimize utilization of scarce resources, such as operation rooms in a hospital.
To this end, the study attempts to finalize a process map to depict the existing scheduling process at the target hospital. The premise is that the process map will identify obstacles in the investigated operating room scheduling process, enhance our understanding of hospital operations, and provide insights on areas of fruitful research for improving operation efficiency in the hospital industry. We aim to clearly identify the underlying issues of information sharing, relationships among actions of entities, and how decisions can be influenced in a complex organization, such as a hospital through adoption of proven IS based best practices to contribute to betterment of clinical operations in the hospital industry.
We have preliminarily identified established IS theories in group decision-making leading to collaboration among various stakeholders in the decision-making processes; business process reengineering (BPR) to identify the flow of decision and thus information, the bottlenecks creating impediment in the execution of smooth hospital operations; creation of information sharing environment and the contribution of information technology in its realization. We feel these factors have not been adequately investigated in the promise that healthcare industry holds in its evolution over the coming decades.
The paper is structured as follows. First, the IS literature is briefly reviewed on the current status of IS research in healthcare. The complex nature of hospital operations is discussed with regard to the relationship between hospitals and physicians. Then, employing process map is proposed as the main research method. The resulting process map is presented with brief explanations of key activities. The study ends with a discussion of the distinct features of the investigated operating room scheduling process, and make recommendations on some promising areas of IS research.
2 Current IS research in healthcare
Healthcare practitioners are increasingly relying on information technologies (IT) for managing healthcare costs and improving the quality of care [29]. IS researchers are aware of the trend. In 2004, the Association for Information Systems (AIS), the premier professional association for the study and the practice of information systems worldwide, formed a special interest group on IT in healthcare, or SIG-Health. SIG-Health has supported numerous tracks dedicated to healthcare topics in major IS conferences (http://www.aissighealth.com/wordpress/). Many IS research outlets have increased publication opportunities for research in this important field. For example, the journal of Communications of the Association for Information Systems has introduced a special healthcare department to support researchers to “conduct studies crossing IS and healthcare disciplines” [48; p. 456]; special issues devoted to healthcare have been published with leading IS journals, including the journal of the Association for Information Systems [39], Information Systems Research [15], and the Journal of Strategic Information Systems [35]. IS researchers have studied a variety of healthcare topics, ranging from the build of information infrastructure [1, 30], system design [36] and system implementation [16, 46], to the use of technology among healthcare service providers [24, 37].
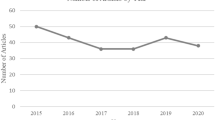
With the growing interest and awareness of healthcare information systems among IS researchers, however, publication of health-related IS research is sporadic. A review of IS journals suggests that the study of healthcare represents a very small fraction of published papers, and there are rare attempts to study healthcare as a specialized context in which IS theories need to be re-examined on the underlying assumptions that work for other industries, but may not hold for healthcare [8].
The application of IT in healthcare may not be straight-forward due to the distinctiveness and complexities of healthcare settings [35]. Fichman and colleagues highlighted the need for IS researchers to understand the special features of healthcare. They pointed out “research anchored in the healthcare context must begin by reflecting on what is distinctive … Distinctiveness of the context drives us toward new theory or theoretical extensions that hold greater promise to explain IS phenomenon” [15; p. 419]. To echo with the call, we start this research with the examination of a distinct feature that is rarely observed in other industries—the equivocal relations between hospitals and physicians.
3 The complex nature of hospital-physician relationships
Unlike other industries, physicians generally are not salaried employees of hospitals; rather, they are independent health services providers with loose contracts with hospitals. Therefore, physicians enjoy “privileges” that entitles them to provide medical services within the respective hospital facility. In exchange for these privileges, physicians are often expected to provide certain service on behalf of the hospital (e.g. serving on hospital committees, pledging on-call ER availability). In turn, hospitals are dependent on these physicians as a referral base for patient volume. This arrangement in the US health care system is a long-standing tradition [4, 17] that has only recently shown signs of changing with the rise of hospitalist physicians [6, 34]. Under such an arrangement, physicians benefit financially from the facility and services of hospitals but do not bear direct responsibility for the fiscal health of these institutions.
The complex nature of hospital-physician relationship has profound consequences on the economics and management of hospitals. Hospitals barely interfere with physicians’ clinical decisions even on the use of hospital facilities [17]. In its special investigation on healthcare costs, the New Jersey Commission on Rationalizing Health Care Resources has concluded that “physicians face little accountability for consumption of hospital resources” and “hospital costs are generally unknown to providers and patients” [34]. Because hospitals and physicians operate on different sets of practices with incompatible financial concerns, the link between the provision of medical service and the consumption of hospital resources is ambiguous, and the cost structure of medical treatment lacks transparency to both service providers and patients. This phenomenon is rarely observed in other industries and causes public criticisms of the health care system [6, 17].
As for the management of operating rooms (ORs), the unique hospital-physician relationship adds complexity to the scheduling process. Since surgeons are not officially affiliated with hospitals, they enjoy greater flexibility in booking ORs without bearing economic consequences. The practice inevitably leads to poor management of ORs, one of the hospitals’ scarce and expensive resources. As pointed out by Grote and colleagues [19], “the hospitals’ common practice of granting doctors block time in operating rooms, with individual surgeons reserving particular rooms on a set day and time each week, imposes large opportunity costs because not all surgeons fill up every minutes of their block time.”
4 Research method
The first step in gaining control over an organization is to know and understand the basic processes [12, 25, 43]. To understand the scheduling process of OR, the study adopts process map as the main research method to depict the operations of a selected hospital surgery department. Process map illustrates key activities involved in the investigated scheduling process. By defining what an entity does, who is responsible, to what standard a scheduling process should be completed and how the success of the process can be determined; the ambiguity of surgery department operations can be largely reduced or eliminated. A more complete understanding of the process will support further research endeavors, such as activity analysis and process reengineering for improving the operation efficiency of hospitals.
4.1 Research site and process
The surgery department of a Midwestern hospital was selected as the research site. The hospital is midsized with about 2,000 employees. The surgery department has nine ORs and employs 26 registered nurses (RNs). For each surgery, there will be about six RNs assisting the operation.
Like many other hospitals, the investigated hospital contracts with independent physicians (hereinafter referred to as surgeons for the special research context) for the use of hospital facility and services. Planning the use of ORs is affected by the availability of hospital facility (i.e., ORs) and services (e.g., anesthesia), as well as the schedules of surgeons. On the hospital side, an OR is operationally available when an anesthesia team is assigned to the room. Of the nine ORs, six to eight ORs are operationally available on a normal business day, and the other one to three ORs remain unassigned without anesthesia service. An OR without anesthesia can only be used for certain basic surgeries, and is rarely utilized. On the surgeons’ side, ORs are reserved for certain time blocks based on personal schedules and preferences. A surgeon can freely schedule a surgery within the reserved time blocks. Not surprisingly, certain time blocks such as weekday mornings are often overbooked, while others such as late afternoons and weekend time blocks always wait to be filled up. The hospital has tried to encourage surgeons to take these “unfavorable” time blocks for an even distribution and a better management of the usage of ORs. But with limited incentives to surgeons, little improvement on OR usage has been achieved.
The surgery department has various process flow charts to guide the execution of key activities, such as registration and scheduling for anesthesia tests, of the scheduling process. However, these flow charts are fragmented in that they each address a focal activity without connection to others. Several flow charts conflict with others in terms of the timeframe of required paperwork, and some are ambiguous for what documents/activities are prerequisite and what will follow. In addition, the RNs are split into three shifts to assure OR availability on a 24 × 7 basis. Some activities are handled differently from shift to shift. The RNs have never thought these fragmented flow charts as a problem in that they have implicit knowledge of how to deal with different cases.
To develop the process map of OR scheduling, the authors visited the surgery department several times, and interviewed all RNs in the department regarding their job responsibilities and relationships with each other in the scheduling process. With generous support from both the top management of the hospital and the department managers (managers of the surgery department are also RNs), we were able to develop a process map that is comprehensive enough to map all scheduling activities. The process map has been approved by the department managers as accurately depicting the scheduling process in the surgery department.
4.2 Results
The research resulted in the development of a comprehensive process map to depict the OR scheduling process in practice. The scheduling process is overwhelmingly comprehensive, involving many different parties (e.g., surgeons, patients and patient families, RNs of the surgery department, other hospital departments, and insurers), retrieving information from various sources (e.g., within-hospital systems, surgeon’s office, and interview with the patient), and demanding different tests (e.g., allergy tests, anesthesia tests, and cardiac tests). In general, the process can be divided into three stages as illustrated in Fig. 1.
The three stages include registration, pre-operation preparation, and surgery operation. The scheduling process starts with the registration stage. The initiation of scheduling is prompted by surgeon’s request on behalf of a patient, and is justified by the patient’s medical history and current health condition (e.g., allergies and results of medical tests). After medical examination and during the 24–48 h before the scheduled operation, major paperwork takes place in the pre-operation stage, in which all necessary documents, including the consent form, are prepared and signed. Then, the patient arrives on the scheduled surgery date for the operation. The last stage includes the pre-surgery preparation (e.g., another review of medical information and double-check on the status of the patient), the surgery operation, and after-surgery recovery care. Upon the discharge of the patient from a recovery room (after the surgery operation), the scheduling process is considered completed.
Although the above description suggests a logical proceeding, the scheduling process is overwhelmingly comprehensive, involving many discrete activities contingent upon various decisions. Taking the first stage of registration as an example, there are three different procedures based on the patient’s medical conditions, including the need for anesthesia and pre-operation testing. This is illustrated in Fig. 2.
Each procedure is distinct with unique set of activities. Procedure 1 is designed for patients who need pre-operation testing. Major activities include scheduling pre-operation testing, scheduling surgery operation, interviewing, testing, reviewing testing results, and releasing medical clearance and cardiac clearance. These activities are illustrated in Fig. 3.
Procedure 2 is designed for patients whose surgery operations require anesthesia but personal medical records suggest the waiver of pre-operation testing. Major activities include contacting surgeon’s office, interviewing patient, scheduling surgery operation, reviewing medical record, and releasing medical clearance. The surgeon can recommend additional pre-testing after reviewing a patient’s medical conditions. In this case, the testing needs to be scheduled and conducted in a timely fashion to avoid re-scheduling the surgery operation.
Procedure 3 is designed for patients whose surgery operations do not require anesthesia. This may be the simplest procedure for the registration stage. Still, much work is required for the assurance of correct patient information. Major activities include contacting surgeon’s office, checking medical record, interviewing patient on phone, and releasing medical clearance on medications and allergies.
The second stage is pre-operation that handles surgery preparations on the scheduled operation day. Major activities include patient registration and documentation (e.g., signing the consent form), preparing for the operating suite, facilitate patient and patient’s family to proper areas (e.g., lobby, pre-operation bay), anesthesia (i.e., local anesthesia or general anesthesia), checking for treatment orders, contacting surgeon, and checking on patient status. The operation could be canceled upon the review of patient’s status.
The third stage centers on the surgery operation. Before the patient being transported to OR, another round of status check is conducted using the SBAR (Situation-Background-Assessment-Recommendation) technique to assure accurate patient information and safety. After the operation, the patient will be transported to a recovery room for observation. When certain criteria are met, the patient is discharged and the whole scheduling process is considered completed.
The high level process map is further decomposed at greater levels of fidelity. The diversity among patient backgrounds adds complexity to the whole process. There are three types of patients: in-house patients who are transferred from other departments of the hospital, outside patients who have no previous record with the hospital, and local patients who have surgery and leave the hospital same day. Each type of patients receives different treatment during the scheduling process due to the availability of medical records and various surgery requirements. In addition, payment issues such as the eligibility for Medicare need to be addressed during the interview in the second stage of pre-operation. Discharge also involves different procedures based on patient types and surgery results. The patient may walk away or be transferred to a different department of the hospital.
The actual process map involves 102 discrete activities and 12 decisions. The process map has been approved by the researched hospital as valid, accurate, and complete. Due to the large degree of details at several levels, the complete process map cannot be presented here. Interested readers can contact the authors for further explanation of the scheduling process.
The process map allows us to depict a holistic picture of the scheduling process. With enhanced understanding of hospital operations, we are able to identify main issues that impede the performance of the investigated surgery department. Examination of these issues suggests several promising areas for IS research in the hospital industry. These issues are discussed in the following section.
5 Discussion
During the development of the process map, we have identified several areas that IS research can provide solutions or recommendations for enhancing operation efficiency. We have also found that hospital operations have distinct features that are rarely observed in other industries. Without justifications based on careful examination of its special operation environment, the hospital industry may not be able to replicate the best practices of other industries with success.
For the investigated OR scheduling process, we have found:
5.1 Collaborative decision making in scheduling
Surgeons play an important role in surgery scheduling. The investigated scheduling process is initiated at surgeon’s request. During the scheduling process, RNs contact the surgeon’s office several times for collecting patients’ data, sending patients’ tests results and other medical information for review, and receiving recommendations on following procedures. Also, the actual schedule of a surgery cannot be decided without the surgeon’s confirmation.
The hospital owns the surgery operation facility. The actual use of the facility, however, is largely determined by surgeons. The relationship between hospital and surgeons, as afore-discussed in section 2, adds complexity to the scheduling process. Although major scheduling activities are conducted by RNs at the hospital, the scheduling process must incorporate flexibility to allow overrides from surgeons. Also, frequent communication with surgeons requires intensive data and information exchange between the hospital and surgeon’s office. Such data exchange is far from seamless and demands heavy human involvement on both sides. If the surgeon’s office and the hospital are using different information systems for patient data, a common situation in reality; additional work is required on both sides for manually collecting, retrieving, and sharing data.
With the joint involvement of surgeons and RNs, the scheduling process can be viewed as a collaborative decision making process in which the hospital and a surgeon collectively schedule a surgery operation upon the availability of OR, the surgeon’s schedule, and the patient’s medical situations. Thus, IS research on group decision support system (e.g., [3, 13, 14, 42]) may provide a valuable reference for rethinking the scheduling process. For example, Dennis [13] studied information exchange and use in group decision making and found that the use of group support systems enhanced the efficiency of information exchange by about 50 %. Barkhi [3] approved that group decision support systems with features supporting problem modeling outperformed systems without such features. Sasaki [42] examined the critical point of strategy selection during group decision making process and proposed a computing theory for collaborative and transparent decision making under time constraint. Turban and colleagues [44] studied the use of social software in virtual group decision making. These studies provide valuable insights on how to improve decision making process, especially with the help of advanced group decision support systems. However, the hospital industry does have unique features, such as different interests/preferences within the group (i.e., between surgeons and RNs), and unbalanced distribution of authority in decision making, that have not been well studied in the existing literature. The area of collaborative decision making in hospital operations will be an interesting and challenging arena for IS researchers.
5.2 Process reengineering for operation efficiency
The efficiency of OR scheduling process is critical to the full usage of OR resources. The nature of the hospital-physicians relationship implies that the hospital does not have direct control on the planning and the actual scheduling of OR usage. Either surgeons or patients can easily switch to a different hospital. Therefore, a smooth and easy scheduling process that facilitates the completion of surgery operations will unquestionably enhance OR usage and increase revenues for the hospital. It is not rare that patients decide to switch to a different hospital due to the delay or harassment in the scheduling process.
Recognizing its importance to the overall organizational performance, the hospital of study has spent significant resources on the scheduling process. On average, one patient will receive assistance from 3 RNs and spend more than 90 min to go through the scheduling process in addition to any medical treatments. The cumbersomely complicated process, as illustrated in Figs. 1, 2 and 3, may be considered as an industry standard. But from a business process reengineering perspective, the scheduling process can be simplified and streamlined for increased efficiency.
The IS community has long concluded the importance of having streamlined processes for operation efficiency. Worldwide competition and changing business environments, such as globalization, political realignments, and the rapid advance of information technology, encourage companies to consider business process reengineering as a powerful means for improving performance [7, 28]. Various methods and tools of restructuring existing processes have been developed and tested [27]. However, existing literature has not placed much attention to the unique context of the hospital industry. Introducing business process reengineering in healthcare in general, and in the operating room scheduling in particular, is another promising area for IS research.
5.3 System integration for information sharing
There are different information systems being used in the scheduling process. With a significant overlap in information coverage (for example, all systems provide basic information of patients), these information systems are used for different purposes and are not integrated. Therefore, RNs often access different information systems for patient data, operation schedule, staff availability, and OR status. Obviously, the coexistence of various systems has increased the workload of RNs and lowered operation efficiency of the surgery department. An integrated system will solve the problem.
IS researchers have long recognized the importance of system integration and its derivative of data integration to the success of modern organizations. For example, Goodhue and colleagues [18] have discussed the benefits of data integration in improving communication and operational coordination across subunits within an organization. Having different systems coexist leads to “informational fragmentation” [33] or “functional silos” [5], and results in the loss of operation efficiency as “dysfunction, redundancy, and waste” [41; p. 502]. The need for system integration has been widely accepted among IS researchers and business practitioners, as concluded by Hasselbring [20] that “to support the intraorganizational business processes within organizations effectively, the existing information systems must be integrated” (p. 33–34).
In the hospital industry, however, system integration may have a different meaning. Miller [32] described four types of system integration in healthcare: the creation of integrated firms and contractual networks, clinical integration, physician/system integration, and functional integration. Of the four types, only functional integration suggests an integration of key support functions and activities for coordination across operating units; other types of system integration deal with the collaboration among healthcare networks, hospitals, clinic offices, and other health-service providers. The healthcare system integration literature has emphasized the broad-scope integration beyond the boundary of one hospital or one healthcare facility (e.g., [22, 29, 38, 47]). In contrast, within-organization system integration has received less attention among healthcare researchers. It will be desirable for IS researchers to study system integration especially in hospital operations.
5.4 Technology adoption
In the surgery department of study, we have observed that RNs prefer reading paper-based reports to reading on screen. Although the information can be retrieved from computers that are conveniently located at every corner of the department area; RNs repeatedly print out hardcopies for reviewing patient information or surgery schedules. RNs in the surgery department have even developed and standardized a special practice for handling the print copies: every morning a designated RN prints all patient forms and archives them into different folders; these folders are placed in the order of surgery schedules in a designated cart located next to the center desk of the department. A folder will be discarded only when the surgery is completed and the patient is discharged from the recovery room.
The information technology trend suggests that more information will be digitized in future. Not only does efficient operation require fast and accurate acquisition, process, transmission, and presentation of information through digital media; the increasing concerns of social responsibilities and environmental impacts have driven many organizations to adopt “paperless office” and other “green IT” practices. It can be foreseen that more information technologies will be implemented in the hospital operation floors. Healthcare workers need to adapt their behaviors accordingly. Taking the consumption of paper as an example, print-out copies, if not totally disappear, will see reduced use in workplace.
IS researchers have established a solid tradition of studying the adoption of new technologies. Theories, such as technology acceptance model [11, 45], innovation diffusion theory [26], and computer self-efficacy [9, 10, 21] have already served as references for researchers of other disciplines to study the impacts of technology on individual behavior and organizational practices. The issue of how to facilitate the adoption of new technologies among healthcare workers should be of interest to many IS researchers.
In summary, hospital operations are complex and have many distinct features that are not common in other industries. There are several promising areas for fruitful IS research. But before committing significant research endeavors, we need to develop a good understanding of the special operations and practices in the hospital industry.
References
Aanestad M, Jensen TB. Building nation-wide information infrastructures in healthcare through modular implementation strategies. J Strateg Inf Syst. 2011;20(2):161–76.
American Hospital Association. Chartbook: trends affecting hospitals and health systems. 2012. http://www.aha.org/research/reports/tw/chartbook/index.shtml. Accessed 21 Oct 2012.
Barkhi R. The effects of decision guidance and problem modeling on group decision-making. J Manag Inf Syst. 2002;18(3):259–82.
Berenson RA, Ginsburg PB, May JH. Hospital-physician relations: cooperation, competition, or separation? Health Aff. 2007;26(1):w31–43.
Beretta S. Unleashing the integration potential of ERP systems: the role of process-based performance measurement systems. Bus Process Manag J. 2002;8(3):254–77.
Carlson G, Greeley H. Is the relationship between your hospital and your medical staff sustainable? J Health Manag. 2010;55(3):158–73.
Caron JR, Jarvenpaa SL, Stoddard DB. Business reengineering at CIGNA corporation: experiences and lessons learned from the first five years. MIS Q. 1994;18(3):233–50.
Chiasson MW, Davidson E. Pushing the contextual envelope: developing and diffusing IS theory for health information. Inf Organ. 2004;14(3):155–88.
Compeau DR, Higgins CA, Huff S. Social cognitive theory and Individual reactions to computing technology: a longitudinal study. MIS Q. 1999;23(2):145–58.
Compeau DR, Higgins CA. Computer self-efficacy: development of a measure and initial test. MIS Q. 1995;19(2):189–211.
Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13(3):319–39.
Deming WE. Out of the crisis. Cambridge: Cambridge University Press; 1982.
Dennis AR. Information exchange and use in group decision making: you can lead a group to information, but you can’t make it think. MIS Q. 1996;20(4):433–57.
Dennis AR, Hilmer KM, Taylor NJ. Information exchange and use in GSS and verbal group decision making: effects of minority. J Manag Inf Syst. 1998;14(3):61–88.
Fichman RG, Kohli R, Krishnan R. The role of information systems in healthcare: current research and future trends. Inf Syst Res. 2011;22(3):419–28.
Goh JM, Gao G, Agarwal R. Evolving work routines: adaptive routinization of information technology in healthcare. Inf Syst Res. 2011;22(3):565–85.
Goldsmith J. Hospitals and physicians: not a pretty picture. Health Aff. 2007;26(1):w72–5.
Goodhue DL, Wybo MD, Kirsch LJ. The impact of data integration on the costs and benefits of information systems. MIS Q. 1992;16(3):293–311.
Grote J, Mango J, Sutaria S. Transforming U.S. hospitals. McKinsey Q. 2007. https://www.mckinseyQ.com/Transforming_US_hospitals_1937. Accessed 21 Oct 2012.
Hasselbring W. Information system integration. Commun ACM. 2000;43(6):32–8.
He J, Freeman L. Understanding the formation of general computer self-efficacy. Commun Assoc Inf Syst. 2010;26(12):225–44.
Holm CE, Burns LR. The future of physician-health system integration. J Health Manag. 2000;45(6):356–8.
Ibold K. Ailing hospital industry. Fla Trend. 1999;42(4):26.
Jensen TB, Aanestad M. Hospitality and hostility in hospitals: a case study of an EPR adoption among surgeons. Eur J Inf Syst. 2007;16(6):672–80.
Juran JM. Juran on planning for quality. New York: Free Press; 1988.
Karahanna E, Straub DW. The psychological origins of perceived usefulness and ease of use. Inf Manag. 1999;35(4):237–50.
Kettinger WJ, Teng JTC, Guha S. Business process change: a study of methodologies, techniques, and tools. MIS Q. 1997;21(1):55–80.
Kim BO. Business process reengineering: building a cross-functional information architecture. J Syst Manag. 1994;45(12):30–5.
Kolodner RM, Cohn SP, Friedman CP. Health information technology: strategic initiatives, real progress. Health Aff. 2008;27:w391–5.
Li L, Xu L, Jeng HA, Naik D, Allen T, Frontini M. Creation of environmental health information system for public health service: a pilot study. Inf Sys Front. 2008;10(5):531–42.
Mango PD, Shapiro LA. Hospitals get serious about operations. McKinsey Q. 2001;2001(2):74–85.
Miller RH. Health system integration: a means to an end. Health Aff. 1996;15(2):92–106.
Muscatello JR, Small MH, Chen IJ. Implementing enterprise resource planning (ERP) systems in small and midsize manufacturing firms. Int J Oper Prod Manag. 2003;23(8):850–71.
New Jersey commission on rationalizing health care resources, final report. 2008. http://www.nj.gov/health/rhc/finalreport/index.shtml. Accessed 21 Oct 2012.
Newell S. Special section on healthcare information systems. J Strateg Inf Syst. 2011;20(2):158–60.
Ngai EWT, Poon JKL, Suk FFC, Ng CC. Design of an RFID-based healthcare management system using an information system design theory. Inf Syst Front. 2009;11(4):405–17.
Oborn E, Barrett M, Davidson E. Unity in diversity: electronic patient record use in multidisciplinary practice. Inf Syst Res. 2011;22(3):547–56.
Ogles BM, Trout SC, Gillespie DK, Penkert KS. Managed care as a platform for cross-system integration. J Behav Health Serv Res. 1998;25(3):252–68.
Payton FC, Pare G, Le Rouge CM, Reddy M. Health care IT: process, people, patients and interdisciplinary considerations. J Assoc Inf Syst. 2011;12(2/3):i–xiii.
Pinsonneault A, Kraemer KL. Middle management downsizing: an empirical investigation of the impact of information technology. Manag Sci. 1997;43(5):659–79.
Raymond L, Uwizeyemungu S. A profile of ERP adoption in manufacturing SMEs. J Enterp Inf Manag. 2007;20(4):487–502.
Sasaki H. A computing theory for collaborative and transparent decision making under time constraint. Inf Syst Front. 2011;13(2):207–20.
Taylor FW. The principles of scientific management. New York: Harper and Brothers; 1911.
Turban E, Liang T, Wu SPJ. A framework for adopting collaboration 2.0 tools for virtual group decision making. Group Decis Negot. 2011;20(2):137–54.
Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–78.
Venkatesh V, Zhang X, Sykes TA. “Doctors do too little technology”: a longitudinal field study of an electronic healthcare system implementation. Inf Syst Res. 2011;22(3):523–46.
Wan TH, Wang BL. Integrated healthcare networks’ performance: a growth curve modeling approach. Health Care Manag Sci. 2003;6(2):117–24.
Wilson EV. Editorial statement: information systems and healthcare department. Commun Assoc Inf Syst. 2004;13(27):456–8.
Zimmerman RS. Hospital capacity, productivity, and patient safety—it all flows together. Front Health Serv Manag. 2004;20(4):33–8.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chandra, C., He, J., Liu, Z. et al. Some promising areas for IS research in the hospital industry: implications from a case study of operating room scheduling. Health Technol. 3, 65–72 (2013). https://doi.org/10.1007/s12553-013-0042-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-013-0042-y