Abstract
Assisted reproductive technology (ART) has yielded vast amounts of information and knowledge on human embryonic development in vitro; however, still images provide limited data on dynamic changes in the developing embryos. Using our high-resolution time-lapse cinematography (hR-TLC) system, we were able to describe normal human embryonic development continuously from the fertilization process to the hatched blastocyst stage in detail. Our hR-TLC observation also showed the embryonic abnormality of a third polar body (PB)-like substance likely containing a small pronucleus being extruded and resulting in single-pronucleus (1PN) formation, while our molecular biological investigations suggested the possibility that some 1PN embryos could be diploid, carrying both maternal and paternal genomes. Furthermore, in some embryos the extruded third PB-like substance was eventually re-absorbed into the ooplasm resulting in the formation of an uneven-sized, two-PN zygote. In addition, other hR-TLC observations showed that cytokinetic failure was correlated with equal-sized, multi-nucleated blastomeres that were also observed in the embryo showing early initiation of compaction. Assessment combining our hR-TLC with molecular biological techniques enables a better understanding of embryonic development and potential improvements in ART outcomes.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Assisted reproductive technology (ART) allows us to observe and monitor human embryonic development in vitro and to evaluate embryo quality before transfer, with several ART-based assessments of the developmental potential of human embryos previously reported [1–4]. The most common method of assessment during ART is morphology-based analysis of specific embryonic characteristics, which can be scored at various stages (pronuclear, cleavage, and blastocyst) [5, 6]. However, this quality control approach needs improvement with implantation rates of good quality embryos limited to 30–40 % per embryo transfer (ET) [7]. Indeed, based on the standard morphological assessment, ET with early cleavage-stage embryos has a better chance of achieving pregnancy than ET with blastocysts [8, 9]. On the other hand, embryos at the blastocyst stage are less likely to be aneuploid, and reported implantation rates are higher when blastocysts have been transferred [10]. Therefore, many facilities offering ART extend in vitro culture of embryos up to the blastocyst stage and then transfer blastocysts on day 5 after oocyte retrieval. However, these prolonged cultures can cause adverse effects in the gamete and embryos, such as epigenetic changes in the gametes [11, 12], and the additional procedures substantially increase both the workload of embryologists and associated laboratory costs.
In 1997, Payne et al. [13] developed time-lapse video cinematography to overcome the limitations of intermittent observation using still images by providing continuous imaging, in which various cellular events could be distinguished in real time and monitored during the observation period. However, this initial system had a limited observation period of 17–20 h. Based on the original report of Payne et al. [13], we developed a new in vitro culture system for high-resolution time-lapse cinematography (hR-TLC) by which clear images of embryonic development could be obtained for a long period of time (up to 5 days) by maintaining optimal culture conditions on the stage of an inverted microscope (Fig. 1) [14, 15]. Using this system, we have demonstrated various novel phenomena during embryonic development in human embryos from the fertilization process to the hatched blastocyst stage without any damage to the embryos [16–20].
High-resolution time-lapse cinematography (hR-TLC). An inverted microscope (IX-71; Olympus, Tokyo, Japan) with Nomarski differential interference contrast optics (Olympus) was equipped with a CCD digital camera (Roper Scientific Photometrics, USA) connected to a computer, and the images were displayed via Metamorph (Universal Imaging Co., USA). In this system, the optimal culture conditions (temperature 37 ± 0.2 °C, pH 7.37 ± 0.05) were maintained by continuously monitoring and adjusting the flow of CO2, the air temperature in the large chamber, and the thermoplate temperature on the microscope stage. Digital images of cultured embryos were acquired continuously for 2–5 days with frame exposure time of 50 ms. In total, 2,000–8,000 images were taken during the observation period. The time interval of image storage was 10 s during fertilization and 2 min thereafter until the end of the observation
Based on our hR-TLC imaging to date, we have determined the precise timing of second polar body (PB) extrusion and pronuclei (PN) formation, as well as the time course from emergence until disappearance of the PN. Although many key events in the early stages of embryonic development have been identified by still imaging or short-term TLC, our hR-TLC results demonstrated that daily checking of embryos would miss key changes in the developing embryo, such as changes in fragmentation patterns, that might prevent the best-quality embryo being selected for transfer [21–23].
Here, we present data on the abnormal phenomena observed in real time during embryonic development using hR-TLC, including the dynamic formation of zygotes with uneven-sized PN, the formation of multinucleated blastomeres (MNBs) at the cleavage stage of embryos, and the association between MNBs and compaction.
Normal fertilization and following embryonic development in vitro
Donated oocytes from conventional in vitro fertilization (c-IVF) were randomly selected for hR-TLC. An oocyte was inseminated with the male sperm, and then transferred into a pre-equilibrated microdrop of fertilization medium in the hR-TLC chamber to observe the site of sperm penetration into the zona pellucida (ZP). Once the sperm had entered the ZP, we focused the microscope on the sperm and time-lapse images were acquired at 10-s intervals. After the sperm reached the surface of the oocyte membrane, hR-TLC observation was then performed at 2-min intervals for approximately 40 h after the sperm attached to the oolemma. After a further 40 min, the equatorial segment of the sperm head initiated incorporation into the oocyte membrane (Fig. 2). Then, the mid-piece of the sperm head sank underneath the oocyte membrane and the whole sperm head disappeared. The second (2nd) PB was extruded shortly after sperm fusion, within 30 min. Concurrently with or shortly (<30 min) after extrusion of the 2nd PB, a protrusion of the oocyte membrane, which is called the ‘fertilization cone’, appeared and persisted for approximately 2 h. This formation of the fertilization cone in a human oocyte after c-IVF was observed for the first time by using hR-TLC [16].
Time-lapse series representing normal embryonic development. A single sperm entered in zona pellucida (a, an arrow). Forty hours after the sperm attached to the oolemma (b). The equatorial segment of the sperm head initiated to be incorporated into the oocyte membrane, and approximately 1 h after the observation commenced, the mid-piece of the sperm head sank underneath the oocyte membrane followed by its disappearance (c). The second polar body was extruded shortly after sperm fusion (d). Concurrently with or shortly after extrusion of the second polar body, a protrusion of the oocyte membrane, which is called the fertilization cone, appeared and persisted for 2 h (e). The flare appeared in the ooplasm 30 min after the disappearance of the fertilization cone (f). Approximately 1 h after the appearance of the flare, male and female PN were formed and appeared in the embryo (g). A translucent zone (halo) was observed in the peripheral ooplasm (h–j). Two PN became apparent and enlarged with the addition of two nucleolar precursor bodies (j, k). The embryo underwent syngamy, and the halo disappeared (l). The first cleavage started at approximately 23 h after the start of imaging and was completed within 30 min (m, n). Just after completion of the first cleavage, nuclei were observed in the blastomeres (o). Thereafter, the second cleavage started, and it was completed by 41 h on the second day of observation (p–t)
In oocytes obtained for intra-cytoplasmic sperm injection (ICSI), the cumulus cells were chemically removed by using recombinant human hyaluronidase at 2–4 h after oocyte retrieval. Surprisingly, a fertilization cone also formed at the site of the sperm injection, once the sperm was located in the peripheral ooplasm, and although the biological function of the fertilization cone in human oocytes is still unknown, this feature suggests a role for the cone in the interaction between sperm and oocyte membrane. At this point in c-IVF and ICSI oocytes, cytoplasmic flare (which describes a radial movement of the cytoplasmic granules from the sperm head located to the peripheral region) corresponding to the movement of sperm aster movement, appeared in the ooplasm 30 min after disappearance of the fertilization cone. In c-IVF oocytes, approximately 6.1 h after insemination, male PN appeared and approximately 10 min later, female PN appeared and abutted. As two PN moved toward the center of the embryo, a translucent zone (halo) was observed in the peripheral ooplasm. The two PN disappeared (syngamy) followed by disappearance of the halo, and the first cleavage started approximately 23 h after insemination. Nuclei were observed in the blastomeres immediately after completion of the first cleavage, and 6.5 h later, the second cleavage started.
Aberrant behavior of female PN (fPN) during the pronuclear stage
Single PN zygote
ART procedures routinely define the occurrence of normal fertilization by the appearance of two PN and whether the 2nd PB has been extruded. In clinical settings, we often encounter abnormal zygotes with a single pronucleus (1PN), generally described as aneuploidy [24–29]. These abnormal embryos are excluded from embryo transfer, especially when normally fertilized embryos are available. Although the majority of 1PN zygotes are incapable of further development, a small number develop to the blastocyst stage. Moreover, they successfully progress to a live birth in cases where no other embryos exist of better quality [30–32] and despite the low pregnancy rate. Nevertheless, because of the uncertainty of their genetic normality, transferring such embryos is controversial among ART laboratories.
The etiology of zygotes forming with 1PN remains unknown; however, several plausible mechanisms have been proposed after IVF or ICSI as follows—(1) parthenogenetic activation [24, 26, 33, 34], (2) asynchronous formation of male PN (mPN) and fPN [24, 34, 35], and (3) early fusion of both PN prior to syngamy [36]. In addition, we observed additional PB-like substance extruded into the perivitelline space after the 2nd PB extrusion, forming zygotes carrying a single PN (manuscript in preparation). This is quite an aberrant phenomenon, and there is no information supporting the possible mechanisms underlying such a phenotype. Based on our observations, we hypothesize that half of the genome in such zygotes is incorrectly extruded, leading to formation of the third PB-like substance and an embryo carrying only 1PN. This finding was established based on highly accurate analysis of hR-TLC whereby both mPN and fPN were analyzed in the same microscopic field. Therefore, we established a molecular biological approach for distinguishing the PN origin.
The paternal genome carries both 5-methylcytosine (5mC) and 5-hydroxymethylcytosine (5hmC), while the maternal genome has 5mC only, and animal studies have demonstrated that the 5mC in the paternal genome is specifically converted to 5hmC during the pronuclear stage [37–39]. Based on these phenomena, we can distinguish mPN from fPN using immunohistochemistry in human abnormal zygotes. In our observation, approximately 50 % of 1PN zygotes had both 5mC and 5hmC in a single PN [40]. The data suggest that 1PN zygotes derived from ICSI could result from PN fusion, although the possible role of androgenesis remains. Furthermore, it was reported that only 13.1 % of 1PN zygotes derived from c-IVF showed haploidy [41], and such zygotes are likely to contain both paternal and maternal genome, and to be diploid. Therefore, we need to reconsider our assessments of 1PN embryos.
Zygote carrying uneven-sized two PN (2PN)
Some 2PN embryos have uneven-sized PN, which have been reported to correlate with ooplasmic immaturity, chromosomal abnormalities, and poor development [42–44]. However, the developmental potential, normality of the embryos, and the mechanisms determining PN size disparity are still unknown.
To investigate the relationship between embryo quality and the formation of uneven-sized PN, we measured the PN diameters 30 min before syngamy. When the difference in PN diameters within a zygote was >10 µm, we categorized the embryos as zygotes carrying uneven-sized 2PN.
Surprisingly, using hR-TLC observation of the oocytes after an ICSI procedure, we also observed a third PB-like substance extruded next to the 2nd PB, as shown in the 1PN zygotes, and approximately one hour later, PN-like material formed within the third PB-like substance. After a single PN emerged in the ooplasm, PN-like material was absorbed into the ooplasm and migrated to abut the emerged PN (Figs. 3, 4). The mean diameter of PN derived from the third PB-like substance was significantly shorter than that of the emerged PN (17.5 ± 3.2 vs 29.9 ± 2.8 μm). Although there is no direct evidence, it seems that the third PB-like substance includes the fPN based on the following observations—(1) in normal embryos, the mean fPN diameter was slightly less than that of mPN (26.4 ± 2.0 vs 28.0 ± 2.1 μm) and the size of re-entered PN was smaller than that of the other, (2) the third PB-like substance was extruded close to a 2nd PB, which is reminiscent of delivery from female genomes rather than that from male and female genomes, and (3) in normal development, PBs include female genomes not male, and only female genomes could be extruded from the oocyte.
Sequential images of uneven-sized PN formation in human embryos. An intracytoplasmic sperm injection (ICSI) procedure was successfully performed on a matured oocyte (a). The oocyte started to extrude a 2nd PB (b). Coincidentally with the 2nd PB extrusion (c), another PB-like substance started to extrude beside the 1st and 2nd PB (d–f). After the male PN was formed, female PN-like material formed (g), stayed in the perivitelline space for 6.14 h (median time) (g), and was then absorbed into the cytoplasm (h, i). Then, a small female PN formed at the point of absorption (j) and migrated toward the male PN (k–n). Finally, the embryo showed 2PN of different sizes (o)
Interestingly, the timings of fPN and mPN formation were almost synchronous (3.4 ± 0.8 vs 3.3 ± 0.9 h) in equivalent-sized 2PN zygotes. However, in zygotes with uneven-sized 2PN, the timing of fPN formation was delayed compared to mPN formation (6.2 ± 0.5 vs 4.2 ± 0.1 h). Both PN abutted and disappeared synchronously. In addition, these zygotes did not cleave normally and they formed MNBs or showed fragmentation. Our hR-TLC analyses thus demonstrated for the first time the formation of uneven-2PN zygotes and implied that even if a zygote had 2PN, uneven-sized PN could lead to abnormalities in mitosis or further development. Therefore, these zygotes should be given special consideration before transfer or cryopreservation.
In association with the formation of uneven-2PN zygotes, we alternatively hypothesize that the fPN was extruded and that a common underlying mechanisms could drive formation of both a 1PN zygote carrying the third PB-like substance and an uneven-2PN zygote. We also demonstrated the existence of 1PN zygotes containing a diploid genome, which would be discarded only if morphological assessment was conducted. This finding should lead to the efficient use of 1PN zygotes containing a diploid genome in clinical practice.
Formation of multinucleated blastomeres
In morphological assessments of day-2 or -3 embryos, we evaluated blastomere size and the fragmentation rate based on the modified Veeck criteria [45]. At that time, we often observed MNBs, and although there are many reports of abnormalities in embryos with MNBs, the developmental potential and normality of these embryos are still controversial. Indeed, we experienced a live healthy baby born from a 2-cell stage of embryo carrying MNBs. By hR-TLC, we have now identified the process underlying the formation of human embryos with MNBs.
Of 335 donated embryos, 272 embryos cleaved and were analyzed at the 2- to 8-cell stages by hR-TLC. We observed MNBs in 26.8 % (73/272) of day-2 and -3 embryos, and classified them into two groups—embryos with multiple small nuclei (46.6 %, 34/73), and those with two equal-sized nuclei (43.8 %, 32/73). In the first group of embryos, the mean diameter of multiple unequal-sized nuclei was significantly less (13.4 ± 5 μm) than that of the two equal-sized nuclei in embryos (24.2 ± 1.9 μm). Of the first group of MNB embryos, 51.9 % (14/27) developed into good quality blastocysts (3BB or greater according to the Gardner grading system [46]), compared to only 25 % (8/32) of the second group, which also showed interrupted cytokinesis after the cleavage furrow was formed. In the second group of embryos, the cleavage furrow disappeared and MNBs with two equal-sized nuclei were formed. The remaining seven embryos also presented cytokinetic failure. Our TLC analysis thus revealed two separate mechanisms for the formation of two types of MNBs—multiple small nuclei appearing during the first cleavage (nuclear fragmentation) and two equal-sized nuclei resulting from incomplete cleavage (cytokinetic failure with karyokinesis) (Fig. 5).
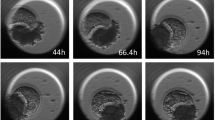
Cytokinetic failure and MNB formation. A single nucleus was observed in the upper blastomere (a). Approximately 22 h into the time-lapse recording (b), the blastomere started to cleave (c), gradually formed the cleavage furrow (d, e), but then failed to cleave (f, g). The cleavage furrow disappeared and MNBs with two equal-sized nuclei were formed 51.5 h later (h). Blue arrow head cleavage furrow, yellow arrow MNB
Initiation of early compaction
After several cellular divisions in the initial stages of development, an embryo undergoes a process called compaction, which is the first morphologically evident differentiation event in mammalian embryos. Compaction in turn has an important influence on the subsequent processes of blastocyst formation, initiation of inner cell mass formation, and trophectoderm differentiation. During compaction, the intercellular boundaries become obscured, maximizing intercellular contact, increasing cell-to-cell adhesion, and allowing formation of the morula. Mechanistically, compaction involves microvilli redistribution, changes to the gap and tight junctions, mitotic proliferation, and cytoplasmic polarization. Furthermore, the key adhesion protein, E-cadherin, is first expressed during compaction, enabling even tighter cell-to-cell attachment [47–51]. The obvious morphological changes are accompanied by functional changes due to a shift in gene transcription profile from the maternal to the zygotic genome [52, 53]. The transcriptional changes induce cell differentiation processes that result in the inner cell mass and trophectoderm, both essential for blastocyst formation. The onset of compaction varies among species. It is the most prominent in the mouse, appearing as cell-to-cell attachment at the 8-cell stage, whereas in bovines it begins at the 16- to 32-cell stage, and in rabbit it commences at the 32- to 64-cell stage [47, 54, 55]. Compaction is less marked in the rhesus monkey and baboon, appearing at the 16- to 32-cell stage, and in pig embryos compaction is not established until shortly before blastocyst formation [52, 56–58]. Microstructural analyses of cell surfaces during compaction in primate embryos including those of humans revealed blastomeres flattened against each other with increased distinctiveness of the intervening cleft, while the length and density of the microvilli gradually increased until the embryos gained a ‘lumpy’ appearance at day 4 of development [47, 48]. However, little is known regarding the exact details of this critical event in human embryogenesis, and both the precise timing of compaction and the underlying mechanisms controlling the process have yet to be clarified [47]. By hR-TLC, we analyzed the initiation of compaction in human embryos in vitro, and observed several novel phenomena during the initiation of compaction that were closely related to the formation of MNBs in human embryos.
Our hR-TLC imaging confirmed that as the developmental process of cleavage progresses in human embryos, the blastomeres became more flattened, and the intercellular boundaries became obscured, with blastulation occurring after compaction was complete. Although the initiation of compaction occurred from the 4-to 16-cell stage, compaction most commonly commenced at the 8-cell stage (26/115 embryos; 22.6 %). Furthermore, 86.1 % (99/115) of embryos initiated compaction at the 8-cell stage or later, and of those embryos, 49.5 % (49/99) developed into good quality blastocysts. In contrast, only 13.9 % (16/115) of embryos initiated compaction before the 8-cell stage, and only 18.8 % (3/16) of these developed into good quality blastocysts (Table 1). Moreover, 93.8 % (15/16) of embryos that initiated compaction before the 8-cell stage showed multinucleation within at least one blastomere (Table 2), and 62.5 % (10/16) of the embryos that exhibited early initiation of compaction showed cytokinetic failure after formation of the cleavage furrow (Table 2; Fig. 6).
Early initiation of compaction in human embryo. Still images from the hR-TLC imaging of an embryo in which compaction initiated before the 8-cell stage. The embryo started the third mitotic division and reached the 6-cell stage (a–e). Then, the lower left blastomere started to form a cleavage furrow (f), but it did not cleave and subsequently returned to its original shape (g–i). This embryo started compaction without further cleavage and formed two equal-sized MNBs (j), which eventually degraded. Arrow: cleavage furrow
Discussion
Using our hR-TLC system, we could represent the entire course of early embryonic development with a short movie. Furthermore, in these real-time series of acquired images, the changes that occur in the hours after fertilization are clearly distinguishable by visual analysis. This technique improves the morphological assessment of human embryogenesis and, by extension, our understanding of the exact developmental processes involved.
One phenomenon we observed was extrusion of a third PB-like substance into the perivitelline space of some 2PN zygotes, and surprisingly, an fPN-like material formed within this substance in zygotes carrying uneven-2PN before being reabsorbed into the cytoplasm. This event was followed by migration of a small amount of fPN-like material towards the mPN and subsequent abutment to the mPN. Such events might represent abnormal PN formation, and further investigation is needed.
We also demonstrated two separate mechanisms of MNB formation (nuclear fragmentation and cytokinetic failure with karyokinesis) during human embryonic development. These events may be understood in more detail by cytoskeletal and/or chromosomal analyses, and clinically, such assessments of embryos with MNBs before embryo transfer could translate to an improvement in ART outcome.
By using our hR-TLC technique, we further observed that initiation of compaction in human embryos occurred at or just after the 8-cell stage in nearly 90 % of embryos analyzed, indicating that compaction seemed to coincide physiologically at or after the third mitotic division in human embryos. In addition, while nearly half of all embryos that initiated compaction after the 8-cell stage developed into good quality blastocysts, only 18.8 % that compacted earlier became good quality blastocysts. Furthermore, the embryos that underwent early compaction displayed a high incidence of MNBs (average 93.8 %), and embryos with one or more MNBs did not develop into good quality or hatched blastocysts. These data indicate that early initiation of compaction is strongly associated with the incidence of MNBs, which in turn is related to polyploidy of the blastomeres. Moreover, 68.8 % of the early compacting embryos displayed cytokinetic failure after the cytoplasmic furrow had formed, indicating that the embryos with MNBs were generated by a novel mechanism whereby the blastomeres showed cytokinetic failure with karyokinesis during mitotic division. Together, these findings suggest that embryos with MNBs appear to have poor developmental potential due to the presence of abnormal blastomeres (i.e., aberrant ploidy) [59]. Based on the incidence of MNBs and theoretical considerations, we hypothesize that embryos initiating compaction at the 4-cell stage have cytokinetic failure with karyokinesis in all four blastomeres, embryos initiating compaction at the 5-cell stage are derived from one blastomere that cleaves normally and then undergoes cytokinetic failure, embryos initiating compaction at the 6-cell stage are derived from two blastomeres that cleave normally and then undergo cytokinetic failure, and embryos initiating compaction at the 7-cell stage are derived from three blastomeres that cleave normally and have one with cytokinetic failure. However, as two-dimensional hR-TLC is not able to automatically adjust the focus on all blastomeres, we could not evaluate morphokinesis in all blastomeres.
In our hR-TLC study, we used donated early stage embryos that had been frozen then thawed. The clinical backgrounds of the couples who donated embryos for the study were representative of those couples undergoing ART; however, because we used only embryos that were viable after thawing and remained in good quality for 24–48 h, selection bias cannot be ruled out. In addition, we were not able to determine the exact time required for the initiation of compaction from insemination, because the embryos had been frozen in the middle of the development stage before compaction. Taken together with our finding that MNBs were sometimes observed in embryos undergoing early compaction (Table 2), the findings warrant further investigation and we need to reconsider using such embryos in clinical practice.
Time-lapse microscopy techniques have dramatically improved morphological and chronological analyses of embryonic development, which in turn makes an important contribution to ART. However, there is no consensus on the best way to determine the competency of human embryos derived from ART or how to select the most competent embryos for transfer despite the recent advances in both invasive and non-invasive techniques. Thus, we must continuously verify the safety and efficacy of ART, as they are used clinically, according to stringent evidence-based medicine.
References
Scott LA, Smith S. The successful use of pronuclear embryo transfers the day following oocyte retrieval. Hum Reprod. 1998;13:1003–13.
Tesarik J, Greco E. The probability of abnormal preimplantation development can be predicted by a single static observation on pronuclear stage morphology. Hum Reprod. 1999;14:1318–23.
Wittemer C, Bettahar-Lebugle K, Ohl J, Rongières C, Nisand I, Gerlinger P. Zygote evaluation: an efficient tool for embryo selection. Hum Reprod. 2000;15:2591–7.
Zollner U, Zollner KP, Hartl G, Dietl J, Steck T. The use of a detailed zygote score after IVF/ICSI to obtain good quality blastocysts: the German experience. Hum Reprod. 2002;17:1327–33.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessments: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83.
Baczkowski T, Kurzawa R, Głabowski W. Methods of embryo scoring in in vitro fertilization. Reprod Biol. 2004;4:5–22.
Ferraretti AP, Goossens V, Kupka M, Bhattacharya S, de Mouzon J, Castilla JA, Korsak V, Kupka M, Nygren KG, Nyboe Andersen A, European IVF-monitoring (EIM), Consortium for European Society of Human Reproduction and Embryology (ESHRE). Assisted reproductive technology in Europe, 2009: results generated from European registers by ESHRE. Hum Reprod. 2013;28:2318–31.
van Montfoort AP, Dumoulin JC, Kester AD, Evers JL. Early cleavage is a valuable addition to existing embryo selection parameters: a study using single embryo transfers. Hum Reprod. 2004;19:2103–8.
Glujovsky D, Blake D, Farquhar C, Bardach A. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology (Review). Cochrane Database Syst Rev. 2012;7. doi:10.1002/14651858.
Borini A, Lagalla C, Cattoli M, Sereni E, Sciajno R, Flamigni C, Coticchio G. Predictive factors for embryo implantation potential. Reprod Biomed Online. 2005;10:653–68.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Olausson PO. Blastocyst versus cleavage stage transfer in in vitro fertilization: differences in neonatal outcome? Fertil Steril. 2010;94:1680–3.
el Hajj N, Haaf T. Epigenetic disturbances in in vitro cultured gametes and embryos: implications for human assisted reproduction. Fertil Steril. 2013;99:632–41.
Payne D, Flaherty SP, Barry MF, Matthews CD. Preliminary observations on polar body extrusion and pronuclear formation in human oocytes using time-lapse video cinematography. Hum Reprod. 1997;12:532–41.
Adachi Y, Takeshita C, Wakatsuki Y, Iwata K, Kato Y, Ueno Y, Mio Y. Analysis of physiological process in early stage of human embryos after ICSI using time-lapse cinematography. J Mamm Ova Res. 2005;22:64–70.
Mio Y. Morphological analysis of human embryonic development using time-lapse cinematography. J Mamm Ova Res. 2006;23:27–36.
Mio Y, Maeda K. Time-lapse cinematography of dynamic changes occurring during in vitro development of human embryos. Am J Obstet Gynecol. 2008;199:660.e1-5.
Mio Y, Maeda K. The beginning of human life under time-lapse cinematography. Period Biol. 2009;111:324–7.
Mio Y, Iwata K, Yumoto K, Ueda M, Iba Y, Nishikori K. Possible mechanism of polyspermy block in human oocytes observed by time-lapse cinematography. J Assist Reprod Genet. 2012;29:951–6.
Mio Y, Iwata K, Yumoto K, Maeda K. Human embryonic behavior observed with time-lapse cinematography. J Health Med Inform. 2014;5:143.
Iwata K, Yumoto K, Sugishima M, Mizoguchi C, Kai Y, Iba Y, Mio Y. Analysis of compaction initiation in human embryos using time-lapse cinematography. J Assist Reprod Genet. 2014;4:421–6.
Chavez SL, Loewke KE, Han J, Moussavi F, Colls P, Munne S, Behr B, Reijo Pera RA. Dynamic blastomere behavior reflect human embryo ploidy by the four-cell stage. Nat Commun. 2012;3:1251.
Pribenszky C, Matyas S, Kovacs P, Losonczi E, Zadori J, Vajta G. Prediction of in vitro developmental competence of early cleavage-stage mouse embryos with compact time-lapse equipment. Reprod Biomed Online. 2010;20:371–9.
Hardarson T, Lofman C, Coull G, Sjogren G, Hamberger L, Edwards RG. Internalization of cellular fragments in a human embryo: time-lapse recordings. Reprod Biomed Online. 2002;5:36–8.
Staessen C, Janssenwillen C, Devroey P, Van Steirteghem AC. Cytogenetic and morphological observations of single pronucleated human oocytes after in vitro fertilization. Hum Reprod. 1993;8:221–3.
Kola I, Trounson A, Dawson G, Rogers P. Tripronuclear human oocytes: altered cleavage patterns and subsequent karyotypic analysis of embryos. Biol Reprod. 1987;37:395–401.
Taylor AS, Braude PR. The early development and DNA content of activated human oocytes and parthenogenetic human embryos. Hum Reprod. 1994;9:2389–97.
Palermo GD, Munné S, Colombero LT, Cohen J, Rosenwaks Z. Genetics of abnormal human fertilization. Hum Reprod. 1995;1:120–7.
Balakier H, Cadesky K. The frequency and developmental capability of human embryos containing multinucleated blastomeres. Hum Reprod. 1997;12:800–4.
Rosenbusch B, Schneider M, Kreienberg R, Brucker C. Cytogenetic analysis of human zygotes displaying three pronuclei and one polar body after intracytoplasmic sperm injection. Hum Reprod. 2001;16:2362–7.
Otsu E, Sato A, Nagaki M, Araki Y, Utsunomiya T. Developmental potential and chromosomal constitution of embryos derived from larger single pronuclei of human zygotes used in in vitro fertilization. Fertil Steril. 2004;81:723–4.
Dasig D, Lyon J, Behr B, Milki AA. Monozygotic twin birth after the transfer of a cleavage stage embryo resulting from a single pronucleated oocyte. J Assist Reprod Genet. 2004;21:427–9.
Gras L, Trounson AO. Pregnancy and birth resulting from transfer of a blastocyst observed to have one pronucleus at the time of examination for fertilization. Hum Reprod. 1999;14:1869–71.
Balakier H, Squire J, Casper RF. Characterization of abnormal one pronuclear human oocytes by morphology, cytogenetics and in situ hybridization. Hum Reprod. 1993;8:402–8.
Sultan KM, Munne S, Palermo GD, Alikani M, Cohen J. Chromosomal status of uni-pronuclear human zygotes following in vitro fertilization and intracytoplasmic sperm injection. Hum Reprod. 1995;10:132–6.
Nagy ZP, Liu J, Joris H, Devroey P, Van Steirteghem A. Time-course of oocyte activation, pronucleus formation and cleavage in human oocytes fertilized by intracytoplasmic sperm injection. Hum Reprod. 1994;9:1743–8.
Leveron J, Munne S, Willadsen S, Rosenwaks Z, Cohen J. Male and female genomes associated in a single pronucleus in human zygotes. Biol Reprod. 1995;52:653–7.
Iqbal K, Jin SG, Pfeifer GP, Szabó PE. Reprogramming of the paternal genome upon fertilization involves genome-wide oxidation of 5-methylcytosine. Proc Natl Acad Sci USA. 2011;108:3642–7.
Wossidlo M, Nakamura T, Lepikhov K, Marques CJ, Zakhartchenko V, Boiani M, Arand J, Nakano T, Reik W, Walter J. 5-Hydroxymethylcytosine in the mammalian zygote is linked with epigenetic reprogramming. Nat Commun. 2011;2:241.
Gu TP, Guo F, Yang H, Wu HP, Xu GF, Liu W, Xie ZG, Shi L, He X, Jin SG, Iqbal K, Shi YG, Deng Z, Szabó PE, Pfeifer GP, Li J, Xu GL. The role of Tet3 DNA dioxygenase in epigenetic reprogramming by oocytes. Nature. 2011;477:606–10.
Kai Y, Iwata K, Iba Y, Mio Y. Diagnosis of abnormal human fertilization status based on pronuclear origin and/or centrosome number. J Assist Reprod Genet. 2015;32:1589–95.
Staessen C, Van Steirteghem AC. The chromosomal constitution of embryos developing from abnormally fertilized oocytes after intracytoplasmic sperm injection and conventional in vitro fertilization. Hum Reprod. 1997;12:321–7.
Gamiz P, Rubio C, de los Santos MJ, Mercader A, Simon C, Remohi J, Pellicer A. The effect of pronuclear morphology on early development and chromosomal abnormalities in cleavage-stage embryos. Hum Reprod. 2003;18:2413–9.
Sadowy S, Tomkin G, Munne S, Ferrara-Congedo T, Cohen J. Impaired development of zygotes with uneven pronuclear size. Zygote. 1998;63:137–41.
Manor D, Drugan A, Stein D, Pillar M, Itskovitz-Eldor J. Unequal pronuclear size-A powerful predictor of embryonic chromosome anomalies. J Assist Reprod Genet. 1999;16:385–9.
Veeck LL. Preembryo grading and degree of cytoplasmic fragmentation. In: An atlas of human gametes and conceptuses: an illustrated reference for assisted reproductive technology. New York: Parthenon Publishing; 1999. p. 46–51.
Gardner DK, Schoolcraft WB. In-vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: fertility and genetics beyond. Lancashire: Carnforth Parthenon Press; 1999. p. 378–88.
Enders AC, Lantz KC, Schlafke S. The morula-blastocyst transition in two old world primates: the baboon and rhesus monkey. J Med Primatol. 1990;19:725–47.
Nikas G, Ao A, Winston RML, Handyside AH. Compaction and surface polarity in the human embryo in vitro. Biol Reprod. 1996;55:32–7.
Fleming TP, Sheth B, Fesenko I. Cell adhesion in the preimplantation mammalian embryo and its role in trophectoderm differentiation and blastocyst morphogenesis. Front Biosci. 2001;6:D1000–7.
Larue L, Ohsugi M, Hirchenhain J, Klemler R. E-cadherin null mutant embryos fail to form a trophectoderm epithelium. Proc Natl Acad Sci USA. 1994;91:8263–7.
Bell CE, Calder MD, Watson AJ. Genomic RNA profiling and the programme controlling preimplantation mammalian development. Mol Hum Reprod. 2008;14:691–701.
Hurst PR, Jefferies K, Eckstein P, Wheeler AG. An ultrastructural study of preimplantation uterine embryos of the rhesus monkey. J Anat. 1978;126:209–20.
Alikani M, Calderon G, Tomkin G, Garrisi J, Kokot M, Cohen J. Cleavage anomalies in early human embryos and survival after prolonged culture in-vitro. Hum Reprod. 2000;15:2634–43.
Fleming TP, Hay M, Javed Q, Citi S. Localization of tight junction protein cingulin is temporally and spatially regulated during early mouse development. Development. 1993;117:1135–44.
Koyama H, Suzuki M, Yang X, Jiang S, Foote RH. Analysis of polarity of bovine and rabbit embryos by scanning electron microscopy. Biol Reprod. 1994;50:163–70.
Pratt HP, Ziomek CA, Reeve WJ, Johnson MH. Compaction of the mouse embryo: an analysis of its components. J Embryol Exp Morphol. 1982;70:113–32.
Ducibella T, Albertini DF, Anderson E, Biggers JD. The preimplantation mouse embryo: characterization of intercellular junctions and their appearance during development. Dev Biol. 1975;45:231–50.
Reeve WJD. Cytoplasmic polarity develops at compaction in rat and mouse embryos. J Embryol Exp Morphol. 1981;62:351–67.
Hardy K, Winston RML, Handyside AH. Binucleate blastomeres in preimplantation human embryos in vitro: failure of cytokinesis during early cleavage. J Reprod Fertil. 1993;98:549–58.
Acknowledgments
We would like to express our particular thanks to Ms. D. Payne and Dr. S. Flaherty in Adelaide, Australia, for their invaluable support in the development of a new in vitro culture system for hR-TLC. We also thank all the laboratory staff of Mio Fertility Clinic, Reproductive Centre for their excellent work, especially, Mr. K. Yumoto for his continuous cooperation and support on this work and Dr. M. Tsuneto for critical reading of the manuscript, helpful discussion, and encouragement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kyoko Iwata and Yasuyuki Mio declare that they have no conflict of interest.
Ethical approval
The study design and studies proposed were reviewed and approved by the ethics committee of JISART (Japanese Institution for Standardizing Assisted Reproductive Technology). We used donated embryos cryopreserved at an early stage (pronuclear stage to 4-cell stage) in the patients who agreed with our experimental use of their gametes and embryos. Since the study was for a scientific research, we did not transfer any embryos used in this research to patients.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and its later amendments. Informed consent was obtained from all patients for being included in the study.
Animal rights
This article does not contain any studies with animal subjects performed by the any of the authors.
About this article
Cite this article
Iwata, K., Mio, Y. Observation of human embryonic behavior in vitro by high-resolution time-lapse cinematography. Reprod Med Biol 15, 145–154 (2016). https://doi.org/10.1007/s12522-015-0231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12522-015-0231-7