Abstract
Background
Menarche is a substantial milestone of female puberty. Timing of age at menarche is considered the key to understanding the potential linkages with women’s health outcomes later in life. This study aimed to explore the secular trends and urban‒rural disparities in the median age at menarche among Chinese Han girls from 1985 to 2019.
Methods
Data were extracted from the 1985, 1995, 2005, 2014, and 2019 Chinese National Surveys on Students’ Constitution and Health, which were nationally representative cross-sectional studies, and a total of 173,535 Han girls aged 9–18 years were examined. Girls were asked whether menarche had occurred. The median age at menarche was estimated by probit analysis. Z tests were used to compare the differences between survey years and between urban and rural areas.
Results
The median age at menarche among Chinese Han girls decreased from 13.37 years in 1985 to 12.00 years in 2019, and the overall decrease was more significant in rural areas (1.77 years) than in urban areas (0.99 years). The average five-year change in the decrease in the median age at menarche showed an accelerating and then slowing pace; and it was observed similarly in both urban and rural areas. The urban‒rural disparities shrank from 0.64 years in 1985 to 0.44 years in 1995, then to 0.27 years in 2005, 0.24 years in 2014, and finally to − 0.14 years in 2019.
Conclusions
The median age at menarche among Chinese Han girls continued to decline from 1985 to 2019 but at a slowing pace in the last five years. Urban‒rural disparities gradually narrowed. Sexual and reproductive health education and interventions to prevent the decline in the age of menarche are needed, especially in rural areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Menarche is a substantial milestone of female sexual maturation, which marks dramatic physiological changes associated with reproductive and various biological functions in female individuals [1]. Timing of age at menarche is considered the key to understand the potential linkages with health outcomes later in life because of the repercussions on sexual initiation and age at marriage and, consequently, fertility [2]. Many studies have confirmed that an earlier age at menarche is associated with higher risks of breast cancer, ovarian cancer, diabetes, cardiovascular disease, depression, and others [3,4,5,6,7].
Many previous studies from various countries worldwide have shown a declining trend in age at menarche over the past two centuries [8, 9]. However, controversial findings have been presented in the past few decades. For example, a decreasing secular trend of age at menarche in females born between 1920 and 1995 was observed in Korea [10]. Nevertheless, in the United States, it was noted that the age of menarche changed little from 1951 to 2010 [11]. Poland experienced a reversal between 1978 and 1988, with a general downward trend from 1966 to 2012 [12]. In China, two nationally representative studies also showed that the median age at menarche of Chinese Han girls declined from 1973 to 2010, while another study demonstrated a stable trend from 2005 to 2012 [13,14,15]. Moreover, while some previous studies have suggested that urban‒rural disparities in median age at menarche among Chinese girls persisted over the last few decades, others found that the difference seemed to gradually narrow between 1985 and 2014 [14, 16]. However, these studies are outdated or contain only local data, and an updated estimate of the median age of menarche among Chinese Han girls and the urban‒rural disparity with nationally representative samples are still needed.
We hypothesized that the median age at menarche among Chinese Han girls continued to decline in the past 35 years, and urban‒rural disparities narrowed gradually. The Chinese National Surveys on Students’ Constitution and Health (CNSSCH), which were nationally representative surveys of health status among Chinese children and adolescents conducted every five years since 1985, provided data on menarche among Chinese Han girls, allowing researchers to study the age at menarche among Chinese girls. This study aimed to analyze the secular trends and urban‒rural disparities in the median age at menarche among Chinese Han girls from 1985 to 2019.
Methods
Study design and participants
Data were obtained from the 1985, 1995, 2005, 2014, and 2019 CNSSCHs, which were nationally representative cross-sectional studies about the health status of Chinese children and adolescents. The surveys covered 31 provinces, autonomous regions, and municipalities, excluding Taiwan, Hong Kong, and Macao. A consistent multistage stratified cluster sampling procedure was used in these five surveys. In stage one, three prefecture-level cities (i.e., upper, moderate, and low) were selected according to their socioeconomic status in each province. In stage two, children and adolescents from the three selected prefecture-level cities were stratified by urban and rural areas based on their residence location. In stage three, within each of these stratified areas, schools covering students aged 7 to 18 years attending primary, middle, and high schools were randomly selected in 1985 and subsequently kept uniform. In stage four, all students from these schools’ randomly selected classes by grade were included in the survey. Only data from Han children and adolescents were used in this study to eliminate the influence of ethnic groups on research, and a total of 173,535 Han girls aged 9 to 18 years from 20 provinces (autonomous regions and municipalities, including Beijing, Tianjin, Hebei, Inner Mongolia, Liaoning, Jilin, Heilongjiang, Shanghai, Zhejiang, Anhui, Fujian, Jiangxi, Shandong, Henan, Hunan, Guangdong, Guangxi, Guizhou, Yunnan, and Shaanxi) with information on menarche in all five surveys were included. The sample size for each survey is shown in Table 1. This study was approved by the Medical Research Ethics Committee of the Peking University Health Science Center (IRB00001052-19095).
Measures
In each survey, girls aged ≥ 9 years were interviewed by a female physician or school nurse and asked whether menarche had occurred. The physicians and nurses had been trained before the survey to help girls distinguish menstruation from other bleeding phenomena, such as bleeding of the perineum due to injury. Their answers were divided into “yes” or “no”.
Statistical analysis
The median ages at menarche and their 95% confidence intervals (CIs) were estimated by using probit analysis. This analysis comprised ten age groups with one-year intervals. A cumulative normal curve was fitted to the proportion of girls within each age group who had reached menarche, and the median age at menarche was the corresponding age at which 50% of girls in the population were predicted to have reached menarche. We calculated the average five-year change to quantify the change in median age at menarche in different time periods. Urban‒rural disparities were defined as the median age at menarche in urban girls minus that in rural girls. Z tests were used to compare the difference in the median age at menarche between two survey years, as well as between urban and rural areas. All statistical analyses were conducted in SPSS 26.0 (SPSS Inc., Chicago, IL, USA). P values of < 0.05 were considered statistically significant.
Results
Secular trends of the median age at menarche from 1985 to 2019
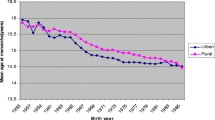
The median menarche age of Chinese Han girls was 13.37 (13.25, 13.50) years in 1985, 13.03 (12.40, 13.62) years in 1995, 12.66 (12.35, 12.96) years in 2005, 12.09 (11.81, 12.37) years in 2014 and 12.00 (10.68, 13.06) years in 2019, with a significant decrease of 1.37 years from 1985 to 2019. In urban areas, the median age of menarche declined from 13.06 (12.81, 13.30) years in 1985 to 12.07 (10.49, 13.25) years in 2019, with an overall decrease of 0.99 years. In rural areas, the median age of menarche declined from 13.70 (13.59, 13.80) years in 1985 to 11.93 (11.22, 12.57) years in 2019, with an overall decrease of 1.77 years (Fig. 1).
Table 2 shows the average five-year change in age at menarche among Chinese Han girls in different periods. Between 1985 and 2014, the decline in the age of menarche among Chinese Han girls gradually accelerated. In the period from 1985 to 1995, the average five-year change was − 0.17 years, while in the period from 2005 to 2014, it was − 0.32 years. However, from 2014 to 2019, the average five-year change was only − 0.09 years, which suggested a slowdown in decline. The average five-year changes in both urban and rural areas were similar to the total population, with an accelerating and then slowing trend. However, from 2014 to 2019, the age at menarche increased by 0.10 years for average five-year changes in urban girls, but it continued to decline rapidly in rural girls, with – 0.28 years for average five-year changes.
Urban‒rural disparities in the median age at menarche
From 1985 to 2014, the median age at menarche of Chinese Han girls in urban areas was always earlier than that in rural areas, and the differences between urban and rural areas were 0.64 years in 1985, 0.44 years in 1995, 0.27 years in 2005, and 0.24 years in 2014 (all P < 0.001). However, in 2019, the median age at menarche in rural girls was 11.93 years, which was earlier than that in urban girls (12.07 years, Z = 14.581, P < 0.001, Table 3). Figure 2 presents the urban‒rural disparities in the median age at menarche across provinces. In the four surveys from 1985 to 2014, only in no more than three provinces was the median age at menarche in rural girls earlier than that in urban girls. In 2019, however, the same urban‒rural disparities were shown in 11 provinces and cities (including Beijing, Hebei, Inner Mongolia, Liaoning, Heilongjiang, Shanghai, Zhejiang, Jiangxi, Shandong, Guangdong and Guizhou).
Discussion
In five nationally representative cross-sectional surveys from China, we found that the median age at menarche among Chinese Han girls continued to decline from 1985 to 2019 but at a slower rate. Urban and rural areas differed in secular trends in the median age at menarche, i.e., urban areas had a smaller overall decrease between 1985 and 2019 and a rebound from 2014 to 2019, while rural areas had a larger overall decrease between 1985 and 2019 and a sustained rapid declining rate. Moreover, the urban‒rural disparities in median age at menarche gradually narrowed, with urban girls reaching menarche earlier from 1985 to 2014 and rural girls reaching menarche earlier in 2019.
The present study showed a decrease in the median age at menarche among Chinese Han girls. Another cohort study of 3199 girls conducted in 15 provinces in China also presented similar trends, in which the median age at menarche declined from 14.25 years in Chinese girls born before 1976 to 12.60 years in girls born after 2000, with a decline of 0.26 years per five years [13]. Age at menarche is influenced by many factors, such as genetics, ethnicity, height, weight, body mass index (BMI), and socioeconomic circumstances [1]. In the past 35 years, China has experienced tremendous economic development. According to the World Bank, the GDP per capita has increased by over 30-fold from 1985 to 2019 in China, which might contribute to this decrease. For example, the girls in Jiangxi province had a later age at menarche compared with their peers in Shanghai at each survey point. When comparing the GDP per capita of these two provinces, we can observe that Shanghai has had a better economic status than Jiangxi [17, 18]. However, a greater decline was observed in Jiangxi, accompanied by its faster growth rate of GDP per capita. Specifically, from 1995 to 2019, the GDP per capita of Shanghai and Jiangxi increased by 8 times and 18 times, which corresponded to the decline in the median age at menarche by 0.74 years and 1.22 years, respectively[18]. Meanwhile, Chinese Han school-aged girls’ nutritional status improved as they grew taller and transitioned from a high prevalence of thinness to a high prevalence of overweight and obesity [19, 20]. Some studies have suggested that higher adherence to the modern dietary pattern, which is characterized by high intakes of fast foods, milk, fruits, and eggs and low intakes of grains and vegetables, was also associated with an earlier age at menarche among Chinese girls [21]. In addition, another potential reason might be increased exposure to endocrine-disrupting chemicals (EDCs), especially in Chinese children, both in urban and rural areas, with more than 90% of them exposed to EDCs, and an existing study has observed the association between peripubertal methylparaben concentration and earlier onset of breast gland development [22, 23]. Although the median age at menarche continued to decline, we found that the rate of decline has slowed in recent years, especially in urban areas. In some developed countries and regions, this phenomenon may occur earlier. For example, only a small decrease of about 1.5 months was observed in the Netherlands from 1980 to 1997 [24]. In Japan, women born in the 1980s were already at the same age at menarche as women born in the 1970s [25]. In Guangzhou, a highly economically developed city in China, the median age at menarche also appeared to level off for urban girls [15]. Many studies have suggested that the achievement of an optimal level of nutritional conditions contributed to the secular trend toward an earlier age at menarche slackening [26, 27]. Furthermore, from an evolutionary perspective, the “target-seeking growth model” in physical anthropology indicated that genetic determinants would exert a repressive effect on excessively decreased trends in pubertal timing [28]. Specifically, if the timing of age at menarche decreased to a certain age, this declining trend would slow or even stop due to genetic factors [15].
This study also revealed the difference in the median age at menarche between urban and rural areas. From 1985 to 2014, our study had the same results as previous studies, which found that urban girls always reached menarche earlier than rural girls [14, 29]. Meanwhile, a narrowing urban‒rural disparity was seen in this study. This might be due to rapid urbanization and the convergence of urban and rural lifestyles in recent years [30]. According to official statistics, the rate of urbanization increased from 23.71% in 1985 to 62.71% in 2019[18]. The consequent reduction in urban‒rural disparity in overweight and obesity also contributed to the narrowing disparity in the median age at menarche [31]. However, due to the rapid rate of decline in rural areas, the urban‒rural disparity in median age at menarche reversed in 2019, with rural girls reaching menarche earlier. Although few studies had reported similar results before ours, since it was found in more than half of the provinces, rather than being affected by individual provinces, we consider that it would characterize the new urban‒rural disparity. However, more studies are needed to confirm this hypothesis.
Substantial evidence suggests that early menarche increases the vulnerability of adolescent girls to negative sexual and reproductive health outcomes and increases the risk of long-term health impairments [4, 5, 32, 33]. Therefore, given the declining age of menarche among Chinese adolescents, preventive health measures would be necessary to reduce the health damage caused by early pubertal onset. We called for earlier and more comprehensive sexual and reproductive health education to help them gain the necessary knowledge and skills to make safe choices related to sex and reproduction. In addition, policies and interventions to prevent the decline in the age of menarche would be necessary, especially in rural areas. For example, comprehensive interventions to prevent overweight and obesity, including education on balanced diets and healthy eating habits, diet environment improvement in society, and encouraging physical activities, might be effective.
This study had several limitations. First, the median age at menarche might not reflect the exact situation in the population because of the cross-sectional study design. Second, information about the actual date of menarche was not obtained. Instead, we only asked whether the participants had started menstruating and estimated the age at menarche by probit regression. However, this status quo method with no memory bias was considered to be more reliable than the recall method in a large study population. In addition, only 20 provinces were included in this study for comparison across years; most of the excluded provinces had a later median age at menarche, which may lead to an underestimation of the national median age at menarche[34]. However, since this study mainly focused on secular trends and urban‒rural disparities, we believed that this underestimation had little impact on the conclusions. Finally, this study only presented the declining secular trends of the median age at menarche and did not explore the potential reasons, such as dietary changes over time, due to data limitations, which deserve further research.
In conclusion, the median age at menarche among Chinese Han girls continued to decline from 1985 to 2019 at a slowing rate. However, the slowing rate mainly occurred in urban areas, and rural areas still had a relatively rapid rate of decline. Urban‒rural disparities in the median age at menarche gradually narrowed. Corresponding policies are needed in China, including earlier and more comprehensive sexual and reproductive health education and interventions to prevent the decline in the age of menarche, especially in rural areas.
Data availability
The data analyzed in this study are subject to the following licenses/restrictions: All individual (de-identified) participant data collected in the surveys can be shared with investigators whose proposed use of the data has been approved by an independent review committee identified for this purpose by contacting the corresponding author. Proposals should be directed to songyi@bjmu.edu.cn.
References
Karapanou O, Papadimitriou A. Determinants of menarche. Reprod Biol Endocrinol. 2010;8:115.
Leone T, Brown LJ. Timing and determinants of age at menarche in low-income and middle-income countries. BMJ Glob Health. 2020;5:e003689.
Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13:1141–51.
Gong TT, Wu QJ, Vogtmann E, Lin B, Wang YL. Age at menarche and risk of ovarian cancer: a meta-analysis of epidemiological studies. Int J Cancer. 2013;132:2894–900.
Janghorbani M, Mansourian M, Hosseini E. Systematic review and meta-analysis of age at menarche and risk of type 2 diabetes. Acta Diabetol. 2014;51:519–28.
Prentice P, Viner RM. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes (Lond). 2013;37:1036–43.
Sequeira ME, Lewis SJ, Bonilla C, Smith GD, Joinson C. Association of timing of menarche with depressive symptoms and depression in adolescence: mendelian randomisation study. Br J Psychiatry. 2017;210:39–46.
Gohlke B, Woelfle J. Growth and puberty in German children: is there still a positive secular trend? Dtsch Arztebl Int. 2009;106:377–82.
Wyshak G, Frisch RE. Evidence for a secular trend in age of menarche. N Engl J Med. 1982;306:1033–5.
Cho GJ, Park HT, Shin JH, Hur JY, Kim YT, Kim SH, et al. Age at menarche in a Korean population: secular trends and influencing factors. Eur J Pediatr. 2010;169:89–94.
Finer LB, Philbin JM. Trends in ages at key reproductive transitions in the United States, 1951–2010. Womens Health Issues. 2014;24:e271–9.
Gomula A, Koziel S. Secular trend and social variation in age at menarche among Polish schoolgirls before and after the political transformation. Am J Hum Biol. 2018;30:e23048.
Meng X, Li S, Duan W, Sun Y, Jia C. Secular trend of age at menarche in Chinese adolescents born from 1973 to 2004. Pediatrics. 2017;140:e20170085.
Song Y, Ma J, Wang HJ, Wang Z, Hu P, Zhang B, et al. Trends of age at menarche and association with body mass index in Chinese school-aged girls, 1985–2010. J Pediatr. 2014;165:1172-7.e1.
Deng Y, Liang J, Zong Y, Yu P, Xie R, Guo Y, et al. Timing of spermarche and menarche among urban students in Guangzhou, China: trends from 2005 to 2012 and association with Obesity. Sci Rep. 2018;8:263.
Liang J, Mai J, Yang W, Lin J, Yao Z. Median-age secular trend of first spermatorrhea and menarche among adolescents in Guangzhou city during 1985–2014. Chin J Sch Health. 2016;37:1670–2.
World Bank. World Bank Open Data. 2022. https://data.worldbank.org/. Accessed 10 Feb 2023.
National Buraeu of Statistics. National data. 2022. http://https--data--stats--gov--cn--e4192.proxy.www.stats.gov.cn/easyquery.htm?cn=C01. Accessed 10 Feb 2023.
Yan X, Liu Y, Ma N, Zhang J, Dang J, Hu P, et al. Regional inequality of height among Chinese Han students aged 7 to 18 years from 1985 to 2014. Chin J Prev Med. 2021;55:752–8.
Song Y, Agardh A, Ma J, Li L, Lei Y, Stafford RS, et al. National trends in stunting, thinness and overweight among Chinese school-aged children, 1985–2014. Int J Obes (Lond). 2019;43:402–11.
Duan R, Chen Y, Qiao T, Duan R, Chen M, Zhao L, et al. Modern dietary pattern is prospectively associated with earlier age at menarche: data from the CHNS 1997–2015. Nutr J. 2020;19:95.
Dong Y, Gao D, Li Y, Yang Z, Wang X, Chen M, et al. Effect of childhood phthalates exposure on the risk of overweight and obesity: a nested case-control study in China. Environ Int. 2022;158:106886.
Harley KG, Berger KP, Kogut K, Parra K, Lustig RH, Greenspan LC, et al. Association of phthalates, parabens and phenols found in personal care products with pubertal timing in girls and boys. Hum Reprod. 2019;34:109–17.
Mul D, Fredriks AM, van Buuren S, Oostdijk W, Verloove-Vanhorick SP, Wit JM. Pubertal development in The Netherlands 1965–1997. Pediatr Res. 2001;50:479–86.
Hosokawa M, Imazeki S, Mizunuma H, Kubota T, Hayashi K. Secular trends in age at menarche and time to establish regular menstrual cycling in Japanese women born between 1930 and 1985. BMC Womens Health. 2012;12:19.
Rigon F, Bianchin L, Bernasconi S, Bona G, Bozzola M, Buzi F, et al. Update on age at menarche in Italy: toward the leveling off of the secular trend. J Adolesc Health. 2010;46:238–44.
Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003;24:668–93.
Tanner JM. Human growth: a comprehensive treatise volume 1 developmental biology prenatal growth. New York: Plenum Press, 1986.
de Muinich Keizer SM, Mul D. Trends in pubertal development in Europe. Hum Reprod Update. 2001;7:287–91.
Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, et al. Urbanisation and health in China. Lancet. 2012;379:843–52.
Dong Y, Ma Y, Dong B, Zou Z, Hu P, Wang Z, et al. Geographical variation and urban-rural disparity of overweight and obesity in Chinese school-aged children between 2010 and 2014: two successive national cross-sectional surveys. BMJ Open. 2019;9:e025559.
Deardorff J, Gonzales NA, Christopher FS, Roosa MW, Millsap RE. Early puberty and adolescent pregnancy: the influence of alcohol use. Pediatrics. 2005;116:1451–6.
Copeland W, Shanahan L, Miller S, Costello EJ, Angold A, Maughan B. Outcomes of early pubertal timing in young women: a prospective population-based study. Am J Psychiatry. 2010;167:1218–25.
Song Y, Ma J, Hu P, Zhang B. Geographic distribution and secular trends of menarche in 9–18 year-old Chinese Han girls. J Peking Univ Health Sci. 2011;43:360–4.
Acknowledgements
We would like to acknowledge the support from all team members and the participating students, parents, teachers, and local education and health staff in the program. And we would like to acknowledge Prof. Patrick W.C. Lau for proofreading the manuscript.
Funding
The present study was funded by National Natural Science Foundation (82273654 to Y.S.)
Author information
Authors and Affiliations
Contributions
NM: Conceptualization, Formal analysis, Writing—original draft, Writing—review & editing; YS: Conceptualization, Funding acquisition, Methodology, Project administration, Writing—review & editing; DS, JD, PZ, YL, SC, YD, PH, and JM: Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
This study was approved by the Medical Research Ethics Committee of the Peking University Health Science Center (IRB00001052 -19095).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, N., Shi, D., Dang, JJ. et al. Secular trends and urban–rural disparities in the median age at menarche among Chinese han girls from 1985 to 2019. World J Pediatr 19, 1162–1168 (2023). https://doi.org/10.1007/s12519-023-00723-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-023-00723-9