Abstract
Purpose of Review
To summarize the current state-of-the-art of intracoronary imaging with a focus on clinical outcomes, novel approaches, and anticipated future developments.
Recent Findings
Multiple randomized trials have demonstrated that intravascular ultrasound (IVUS) guidance of percutaneous coronary intervention (PCI) significantly reduces major cardiac adverse events (MACE), and in particular, rates of target lesion failure or clinical restenosis. High-definition IVUS enhances the ability to visualize stent struts and plaque components. Optical coherence tomography (OCT) offers a greater resolution and can image many plaque morphology and stent characteristics that are not visualized with IVUS. Image guidance should be considered strongly in complex PCI lesions and potentially in all-comers. Multimodality imaging using near-infrared spectroscopy or fluorescence, combined with IVUS or OCT, is an exciting new approache to image plaque lipid, intraplaque hemorrhage, inflammation, and fibrin deposition.
Summary
Intravascular imaging guidance of PCI utilizing IVUS or OCT definitively improves outcomes in many patient subsets but remains heavily underutilized. Emerging intravascular imaging modalities, such as near-infrared spectroscopy and near-infrared fluorescence imaging, will allow for improved plaque and stent characterization. As cath lab integration, automated image segmentation, and x-ray co-registration evolve further, we envision that intravascular imaging will become a routine for the vast majority of PCI patients, with resultant benefits in clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary angiography (CAG) is the clinical gold standard in the diagnosis of coronary artery disease (CAD) but remains limited by its focus on lumenology, and its inability to assess the arterial wall, where CAD originates. To overcome these limitations of CAG, multiple high-resolution clinical intracoronary imaging modalities have been developed.
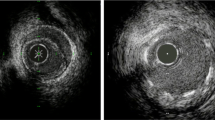
Intravascular ultrasound (IVUS) has been employed for several decades and revolutionized the ability to assess the efficacy of percutaneous coronary intervention (PCI) (e.g., stent expansion) and complications of PCI (e.g., arterial wall dissection, tissue prolapse), and characterize atherosclerosis (e.g., plaque calcification, plaque burden, and severity of left main CAD) and vessel geometry (Fig. 1). More recently, intracoronary optical coherence tomography (OCT) has emerged to overcome some limitations of IVUS by providing very high–resolution images (ten times higher than conventional IVUS, five times higher than high-definition (HD) IVUS), allowing spectacular visualization of stent struts and arterial wall dissections, and the ability to assess plaque composition of the fibrous cap, lipid, calcium and calcified nodules, and thrombus. Mechanisms of stent failure such as fracture, deformation, or recoil are also better illuminated by OCT.
Comparison of optical coherence tomography (OCT) and intravascular ultrasound (IVUS) from the same lesions. A) Lumen area measured 8.40 mm2 by OCT and B) 8.83 mm2 by IVUS. External elastic membrane (EEL) diameter (yellow double arrowhead) measured 3.86 mm by OCT and 4.09 mm by IVUS. Lumen diameter (white double arrowhead) measured 3.28 mm by OCT and 3.54 mm by IVUS. Magnified details of A) and B) are shown in A′) and A″) for OCT and in B′) and B″) for IVUS (EEL: red dotted line, internal elastic lamina: yellow dotted line, lumen surface: blue dotted line. C) EEL border is not visualized with OCT at the lesion (white arrowheads) due to plaque attenuation and limited penetration depth, but clearly visualized by D) IVUS (white double head arrows, 5.2 and 4.4 mm). E) Stent area measured 8.10 mm2 by OCT and F) 8.24 mm2 by IVUS. White arrow indicates stent strut. Reprinted from Maehara et al.40 with permission from Elsevier
Newer imaging modalities include near-infrared spectroscopy (NIRS) and near-infrared fluorescence (NIRF) imaging that not only display structural characteristics of the vessel wall but also assay specific plaque characteristics such as lipid cores (NIRS) or biomolecular processes such as inflammation (NIRF molecular imaging) or intraplaque hemorrhage (near-infrared autofluorescence (NIRAF)) to better assess high-risk plaques at elevated risk of plaque progression and atherothrombosis.
Historically, most intravascular imaging (IVI)–based studies have been descriptive or otherwise non-randomized studies. However, in the last several years, there is a new body of evidence comprising multiple large-scale prospective randomized controlled trials (RCTs) that demonstrate that IVUS not only improves stent implantation characteristics but actually improves clinical outcomes [1]. In particular, IVUS-guided PCI resoundingly reduces clinical restenosis, with greater benefit seen in more complex lesion subsets [2••, 3, 4]. OCT and NIRS-IVUS have also begun to demonstrate the potential to improve hard clinical endpoints. These recent trials provide a groundswell for routine IVI to be performed and motivation for interventional fellowship training to provide greater learning opportunities for improved IVI acquisition and image interpretation. Despite these benefits, IVI is not routinely performed in clinical practice, and its use is highly heterogeneous by the operator and geographic region [5].
In this review, we highlight the current evidence supporting the use of IVI, current limitations, and future directions. We focus on IVUS, OCT, and newer multimodal imaging techniques.
Advances in IVUS Imaging
Clinical Outcome Studies
Intracoronary IVUS was introduced in 1990 into the clinical setting and allowed for the first time visualization of intracoronary morphology and plaque characteristics [6].
Early Studies
Early RCTs comparing IVUS-guided PCI to CAG-guided PCI showed a neutral effect on major outcomes. The HOME DES IVUS trial did not show any difference in major adverse cardiovascular events (MACE) or stent thrombosis at 18 months with first-generation DES and IVUS, but higher pressure post-dilation was noted in the IVUS group [7]. The trial was likely underpowered to detect MACE. Kim et al. did not find a significant difference in MACE at 1 year, which was likely due to a relatively low overall number of patients combined with a high rate of crossover from both groups, given that on-treatment analysis of the same trial favored IVUS [8]. Given the failure of earlier trials to show significant differences in MACE, post-procedural minimal lumen diameter (MLD) was chosen as a primary endpoint in the AVIO trial, which randomized patients with complex lesions to IVUS or CAG-guided PCI and demonstrated a larger MLD, but no significant difference in MACE [9]. Subsequently, multiple RCTs were conducted to investigate the effects of IVUS-utilization in specific lesion subsets.
RCT of IVUS in Long Lesions
Multiple trials have investigated the value of IVUS during PCI of long lesions. The Impact of Intravascular Ultrasound Guidance on Outcomes of Xience Prime Stents in Long Lesions (IVUS-XPL) enrolled 1400 patients with target lesion length ≥ 28 mm and typical chest pain or ischemia to receive PCI with everolimus-eluting stents under IVUS or CAG-guidance [3•]. The primary outcome of MACE (cardiac death, myocardial infarction (MI), target lesion revascularization (TLR)) was reduced from 5.8 to 2.9% in the IVUS group driven by a 50% reduction in TLR. Similarly, Kim et al. investigated IVUS-guided intervention in long lesions and demonstrated a neutral effect in the intention-to-treat analysis most likely due to high crossover rates [8]. The on-treatment analysis of this trial showed a similar reduction of MACE (cardiac death, MI, target-vessel revascularization [TVR]) from 8.1 to 4.0% driven by a reduction in TVR [8].
RCT of IVUS in Chronic Total Occlusion PCI
Two major IVUS trials focused on patients with chronic total occlusions (CTOs) [10, 11]. Clinical Impact of Intravascular Ultrasound–Guided Chronic Total Occlusion Intervention With Zotarolimus-Eluting Versus Biolimus-Eluting Stent Implantation (CTO-IVUS) randomized 402 patients with CTOs to either IVUS or CAG-guided PCI. At 12 months, there was no difference in the primary endpoint of cardiac death but there was a significant > 50% reduction of MACE (cardiac death, MI, TVR) from 7.1% to 2.6% in the IVUS group driven by a reduction in cardiac death and MI, but not in TVR. These trial results were particularly notable because most other trials of IVUS since have shown a reduction in TVR but not the other components of MACE. The Comparison of Angiography- versus IVUS- guided Stent Implantation for Chronic Total Coronary Occlusion Recanalization. (AIR-CTO) randomized 230 patients with successfully crossed CTOs to either IVUS or CAG-guided PCI [11]. At 12 months, there was a significant reduction of the primary endpoint of in-stent late lumen loss, but no significant reduction in MACE, although the study was underpowered for this endpoint. It should be noted that there are benefits of IVUS use in CTO procedures beyond optimal stent expansion, stent placement, and detection of edge dissections. IVUS can additionally be utilized to resolve proximal cap ambiguity, to enable real-time wire traversal of CTO proximal caps, and to confirm wire position in the true versus false lumen during dissection/entry maneuvers.
RCT of IVUS in All-Comers
Most published IVUS studies were non-randomized or reported purely anatomical endpoints such as gains in the MLD. Randomized studies such as IVUS-XPL, CTO-IVUS, and AIR-CTO demonstrated benefits of IVUS guidance as discussed above, however, these studies were limited to specific populations and lesion subsets.
As a result, the Intravascular Ultrasound Guided Drug Eluting Stents Implantation in “All-Comers” Coronary Lesions (ULTIMATE) trial was performed and enrolled all-comers who required DES PCI, without specific inclusion criteria for particular lesion subsets [2••]. The strength of this trial was its adequate power to detect reductions in the clinically important outcome of target-vessel failure (TVF), rather than focusing on surrogate markers such as MLA/MLD. In ULTIMATE, a total of 1448 patients predominantly presenting with acute coronary syndrome (ACS) were randomized to either IVUS or CAG-guided PCI. There was a minimal crossover between the groups. The complexity of coronary disease overall was high with multivessel disease present in > 50% of patients, mean lesion length of 34.5 mm, 25% bifurcation lesions, and 67% of lesions characterized as B2/C. In the IVUS-guided group, stent diameter was selected based on IVUS assessment of the lesion. After post-dilation IVUS-guided stent deployment, optimization was performed to achieve three predefined criteria. As a result, 1-year TVF was significantly reduced by almost 50% from 5.4 to 2.9%. MACE was also reduced significantly, mainly driven by TVR and numerically lower rates of cardiac death and target-vessel MI [2••].
A very recent IVUS-guided PCI meta-analysis incorporating the ULTIMATE trial demonstrated a 38% reduced risk of MACE, 49% reduced risk of CV death, and 42% reduced risk of TLR, and a trend towards reduction of MI [12].
RCT of IVUS in the Left Main Coronary Artery
Multiple observational studies demonstrated both the value of IVUS in diagnosis of clinically significant left main stenosis [13] and for improving outcomes for LM PCI [14]. These studies provided the foundation for IVUS to be granted a Class IIa recommendation in both the US (indeterminate left main assessment) and European (left main PCI guidance) guidelines.
Recently, IVUS-guided left main coronary intervention has been studied in two small single-center RCTs. One trial enrolled a moderate number of elderly patients (N = 123, > 70 years old) and demonstrated that IVUS reduced MACE at 2 years, driven by a reduction in TLR [15]. A second more recent RCT (N = 336 patients) demonstrated a significant reduction in the 1-year primary composite MACE endpoint from 21.9 to 13.2% with IVUS use [16].
A recent left main IVUS meta-analysis of 4592 including the first RCT above and 6 observational studies demonstrated reductions in MACE (39%), all cause-death (45%), cardiac death (55%), MI (34%), and stent thrombosis (52%) [17]. While the reduction in TLR and TVR in this analysis was lower but not statistically significant, the two RCTs above both consistently showed reductions in revascularization rates.
Additional IVUS Prospective, Non-randomized Outcomes Studies of Importance
Bifurcations
Stented bifurcation lesions have been reported to have an increased risk of target lesion failure compared to non-bifurcation lesions [18]. IVUS has been studied to elucidate whether its application is beneficial during bifurcation PCI. Chen et al. studied IVUS versus CAG-guided two-stent techniques for coronary bifurcation lesions and found a significant reduction in stent thrombosis and MI but no difference in MACE, including TLR [4]. In a second trial with 7-year follow-up, Chen et al. enrolled 1465 patients with unstable angina and Medina 1,1,1 or 0,1,1 bifurcation lesions. MACE (cardiac death, MI, TVR) was significantly reduced with IVUS use, from 15 to 10% at 1 year and from 22.4 to 15% at 7 years. IVUS also resulted in a decreased rate of cardiac death from 6.5 to 1.3% and MI from 8.4 to 2.3% [19].
Cost-Effectiveness
IVUS has been shown to be cost-effective in several studies [20,21,22]. Most of these were performed prior to the most recent RCTs demonstrating reduced MACE and therefore probably underestimate the overall cost-effectiveness of IVUS. There was a slight increase in contrast use of 17 ml in the ULTIMATE trial, which is in line with other IVUS trials but may also be due to the specific study protocol. In routine clinical use, IVUS can often be used to reduce contrast exposure [2••]. In light of the clinical benefits and cost-effectiveness, we see an increase in the procedural time of 15 min as acceptable for most complex patients but would argue that this time may also decrease with routine use as operator experience increases [2••].
Advancements in IVUS
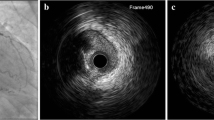
High-definition (HD) IVUS imaging catheters use 60-MHz frequency compared to 40 MHz of standard IVUS. These catheters offer a better resolution, higher pull-back speeds up to 10 mm/s, and higher frame rates of 60 frames/s. The higher resolution allows the evaluation of fibrous and lipidic plaque, tissue prolapse, and improved visualization of stent struts to identify malapposition, while maintaining the known advantages of IVUS of greater depth penetration compared to OCT [23] (Fig. 2). HD-IVUS has been shown to better visualize struts of bioresorbable scaffolds compared to standard IVUS [24]. Stent thrombotic material, stent malapposition, and fibrous cap and calcium thickness are still better evaluated with OCT [25].
High-definition (HD) intravascular ultrasound (IVUS, top row) compared to optical coherence tomography (OCT, bottom row). A) The intima, media, and adventitia are clearly visualized with both HD-IVUS and OCT. B) Fibrous plaque. C) Lipidic plaque. D) Tissue prolapse and subtle stent malapposition are visible after stent implantation, particularly with OCT. E) Calcium underlying stent struts. F) A distal edge dissection is seen clearly visualized by OCT but on IVUS only appears as discontinuation of the intimal layer without a visible flap or hematoma. Reprinted from Chin et al.23 with permission from Elsevier
Stent Optimization Criteria by IVUS Optimization after Stent Implantation
One of the major benefits of IVI is the ability to interrogate and optimize implanted stents. Criteria employed in clinical trials to assess successful IVUS-guided PCI include optimal stent expansion, low plaque burden and no lipid pool at the stent edges, and minimal or no edge dissection [26,27,28, 29••]. Avoidance of malapposition and tissue protrusion are also potentially desirable but difficult to assess with IVUS due to the relatively low resolution. Stent underexpansion is a major predictor of stent failure [30]. Optimal stent expansion has been defined variably in clinical trials from minimal stent area (MSA) > 80% average reference lumen area (RLA), > 90% average RLA, or > distal RLA. It remains unclear if a MSA > 80% is truly beneficial, but most recent consensus documents have suggested that it may be sufficient and most realistically achievable [29••]. Plaque burden > 50% at the stent edge has been shown to be associated with higher MACE [31, 32]. Large edge dissections are associated with early stent thrombosis [29••]. Optimization after stent implantation is important as trials such as ULTIMATE and IVUS-XPL have shown better clinical outcomes when criteria are met at the end of PCI.
Given these findings and the fact that IVUS has now been shown to reduce MACE in three major RCTs (ULTIMATE, IVUS-XPL, Chen et al.) each enrolling over 1000 patients, we offer that IVUS is ready for prime-time and its use should be considered in a wider array of patients. Use of IVUS should be strongly considered in patients at greater risk for restenosis with diabetes, CKD, or ACS and in patients with high-risk anatomy such as multivessel disease, bifurcation lesions, long lesions, and CTOs, and perhaps even in all-comers.
Advances in OCT Imaging
Optical coherence tomography (OCT) employs near-infrared light excitation (e.g., 1310 nm) to generate reflected interference waves that are intensity- and time-dependent based on the arterial wall composition and depth location. Its advantages over IVUS include a higher resolution of 10–20 μm compared to 100–200 μm of IVUS, allowing for better detection and assessment of the endothelial surface and assessment of plaque fibrous caps, thrombus, dissections, and stent strut coverage [28, 33, 34] (Fig. 1). Due to its superior resolution, OCT also may be able to distinguish plaque erosion from plaque rupture [35, 36, 37•]. Higher resolution and contrast also allow better detection of lipid-rich plaques, and in some cases better assessment of the volume of plaque calcium, whereas IVUS assessments are limited by acoustic shadowing. A major limitation of OCT compared to IVUS is the lack of full wall assessment which can limit measurements of plaque burden and result in lower deployed stent sizes compared to IVUS [38,39,40]. In addition, OCT requires contrast flushing which may be detrimental to patients at risk for contrast-induced acute renal failure.
Major recent trials to assess the benefits of OCT have compared OCT to either IVUS, CAG, or both. To date, there have not been RCTs demonstrating improved clinical outcomes with OCT-guided PCI; the actively enrolling ILLUMIEN-IV trial aims to address this gap (discussed below).
RCTs of OCT
RCT of OCT Vs. CAG with a Surrogate Endpoint of FFR
Does Optical Coherence Tomography Optimize Results of Stenting (DOCTORS) randomized 240 patients with non-ST-elevation ACS to either OCT use pre- and post-PCI, or CAG-guided PCI [41]. The primary end point was post-PCI FFR. There was an improvement in FFR from 0.92 in the CAG-alone group to 0.94 with OCT use. Periprocedural complications including AKI were identical between groups. Post-PCI OCT detected significantly more stent underexpansion, stent malapposition, and edge dissection, which led to more post-dilation in the OCT-guided group with lower residual stenosis. While likely desirable to achieve better surrogate endpoints, it is remarkable that FFR increased only by 0.02. Furthermore, it is questionable if a change in FFR from 0.92 to 0.94 is clinically meaningful. Whether invasive physiological assessment after stent implantation is an appropriate marker for PCI success is being actively tested by the DEFINE PCI study (NCT03084367).
RCT of OCT Vs. IVUS—Clinical Endpoints
In the OPtical fre- quency domain imaging vs. INtravascular ultrasound in percutane- ous coronary InterventiON (OPINION) study, 829 patients with stable and unstable angina were randomized to OCT versus IVUS-guided PCI employing a second-generation DES [42•]. The primary endpoint of 1-year TVF was comparable between OCT and IVUS, and there was no significant difference in MACE between the two groups. This was mainly due to a low number of events overall, but likely also because post-PCI MLD between OCT and IVUS groups was similar.
RCT of OCT Vs. IVUS Vs. CAG—Clinical Endpoints
The Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III) study randomized 450 to CAG-guided, IVUS-guided, or OCT-guided PCI and demonstrated that OCT resulted in a MSA that was non-inferior to IVUS, but also not superior to CAG [43]. In addition, OCT detected more surrogate markers of possible future adverse events such as stent malapposition and dissection. It remains unclear if this will translate into clinically meaningful improvements.
Future OCT Studies
Given the lack of data to demonstrate a positive effect of clinical outcomes versus surrogate markers, further trials are necessary. The ILUMIEN IV trial is currently randomizing up to 3650 high-risk patients 1:1 to OCT-guided versus CAG-guided PCI with an everolimus-eluting DES. The primary outcome is a composite of cardiac death, TV-MI, and TVR at 2 years [44]. A major emphasis of this trial will be to size implanted stents based on EEL-derived measurements [44]. Outcomes of this trial will likely be critical to driving greater adoption of OCT.
In addition, OCT use may become more prevalent if unique features detectable by OCT, such as plaque erosion, prove to be of clinical importance [45]. Plaques complicated by erosion are pathobiologically distinct from plaques complicated by rupture, and preliminarily, eroded plaques underlying ACS may not require PCI, but possibly can be managed successful with dual-antiplatelet therapy and IIb/IIIa inhibitors [46, 47].
Multimodality Imaging of Arterial Lipid and Pathobiology
Both IVUS and OCT are insufficient to detect vulnerable plaques and predict the likelihood of future events. In the PROSPECT trial IVUS-derived variables had an 18.2% positive predictive value to detect lesions that would cause future events [48, 49]. In the PREDICTION trial, IVUS-derived variables including endothelial shear stress provided a 41% positive predictive value to predict lesions that progressed and required revascularization [50], representing a significant but not yet clinically meaningful advance in predictive ability. This highlights the need for more advanced imaging techniques, including multimodal imaging [49] that is able to accurately detect plaques that are at high likelihood to cause future events. Development of these is currently the subject of multiple ongoing investigations.
NIRS-IVUS
NIRS can determine the presence of lipid-rich plaques [51] but is limited in its standalone ability to detect structural information, and has therefore been combined with 50-MHz rotational IVUS on a single 3.2 Fr catheter (Fig. 3). This system is the only one currently approved for clinical use in the USA, Europe, Japan, and Korea. Initial studies demonstrated that culprit lesions in patients with ACS have specific characteristics such as an increased lipid component [52, 53] and a recent study suggested that NIRS-IVUS may be able to identify vulnerable plaques associated with future events [54]. Two major trials are investigating this hypothesis. The recently presented prospective Lipid-Rich Plaque (LRP) Study (NCT02033694) enrolled stable patients with ACS, stable angina, or a positive functional study and found that patients with a maximum lipid core burden index in a 4-mm length of artery (maxLCBI4mm) > 400 experience an 87% higher risk of experiencing non-culprit MACE (NC-MACE) at 24 months, and that a coronary segment with maxLCBI4mm > 400 is at a more than 4-fold risk for NC-MACE. NIRS-IVUS may potentially be used to identify patients and non-culprit arteries at high risk for future events, although final publication and further details are needed regarding the lesion-specific positive predictive value.
Near-infrared spectroscopy (NIRS) of lipid core plaques underlying acute STEMI. A) Culprit lesion (block arrow) is seen on initial angiogram in the right coronary artery. B) Following balloon angioplasty, the flow has been re-established. C) NIRS shows prominent signs of lipid core plaque at the culprit segment (located between lines). Reprinted from Madder et al.53 with permission from Elsevier
In addition, a second prospective observational trial, PROSPECT II (NCT02171065), is enrolling patients with ACS and will report on NC-MACE at 24 months in 2020. While NIRS-IVUS appears to be a promising approach to better characterize coronary pathology, future studies are needed to demonstrate that vulnerable plaques identified with NIRS-IVUS can be treated successfully to improve outcomes. Early research indicates that this may be possible with either medical therapy [55] or stenting [56]. A limitation of NIRS based on light absorption is its inability to distinguish superficial from deep lipid due to its lack of depth information, which is partially offset by the additional depth information of IVUS.
NIRF Molecular and Intraplaque Hemorrhage (IPH) Imaging
NIRF allows for molecular imaging of coronary arteries by injecting specific near-infrared fluorescence imaging agents that are then visualized by an intravascular NIRF catheter. To simultaneously detect structural information, NIRF has been integrated into hybrid systems with NIRF-IVUS [57] and NIRF-OCT [58] (Fig. 4). The NIRF signal is then displayed over the anatomy as it lacks depth information. OCT-NIRF has been used in pre-clinical studies to quantify plaque inflammation and identify macrophage-rich atheroma [59]. NIRF imaging is distinct from NIRS, in that NIRF imaging is highly versatile based on the employed molecular imaging agent and the availability of detecting near-infrared autofluorescence (NIRAF) of plaques.
Intravascular molecular imaging using near-infrared fluorescence (NIRF)-intravascular ultrasound (IVUS) or NIRF-optical coherence tomography (OCT). In vivo NIRF-IVUS imaging of vascular injury in a swine iliac artery following injection of indocyanine green (ICG), a vascular injury NIRF imaging agent. A) Longitudinal IVUS image of the injured vessel and matching NIRF image of ICG (red pseudocolor)-labeled injury induced by an angioplasty balloon. NIRF clearly shows the ICG-labeled injured region that is not appreciated on IVUS. B) Axial view of the NIRF-IVUS signal from within the lesion and C) anatomically matched segment under fluorescence microscopy (FM) demonstrating ICG positive areas in red. Note that while injured areas cannot readily be distinguished from normal areas by IVUS, they are clearly outlined by ICG deposition recognized by the NIRF-IVUS. (D, E, F) NIRF-OCT was used to assess fibrin deposition on a bare metal stent (BMS) and a drug-eluting stent (DES) in a rabbit model on day 7 in vivo by FTP11-CyAm7 fibrin NIRF imaging. DES exhibits greater fibrin deposition than BMS. D) In vivo 2D near-infrared fluorescence map with BMS (left) and DES (right) and E) corresponding fluorescence microscopy on longitudinally cut stents. F) Representative in vivo axial NIRF-OCT images of BMS (left) and DES (right) at the distal edge (arrowhead in D). FITC, fluorescein isothiocyanate autofluorescence. Parts A–C reprinted from European Heart Journal – Cardiovascular Imaging, Vol. 18, 2017:1253–61, Bozhko et al., Quantitative intravascular biological fluorescence-ultrasound imaging of coronary and peripheral arteries in vivo, Copyright (2017), with permission from Oxford University Press. Parts D–F reprinted from Hara et al.61 with permission from Oxford University Press.
NIRF-OCT and NIRF-IVUS Molecular Imaging
Possibilities for imaging are countless due to a multitude of NIRF imaging agents that are able to detect plaque protease activity, plaque macrophages, abnormal endothelial permeability, and fibrin deposition on stents [60, 61•].
NIRAF-OCT Detection of IPH in CAD Patients
Intraplaque hemorrhage is a key driver of plaque progression and complications [62, 63], but is not routinely imageable in patients with CAD. Recently, our group collaboratively developed an NIRAF-OCT imaging approach and demonstrated the ability to image coronary IPH in 12 patients [64]. Compared to NIRF molecular imaging, NIRAF uses more blue-shifted NIR light (e.g., 633-nm excitation rather than 750 nm) and does not require injection of an imaging agent, as it detects endogenous plaque autofluorescence. Recently, mechanistic data demonstrated that sources of NIRAF include breakdown products of hemoglobin such as bilirubin, occurring in regions of IPH [65], although the full NIRAF profile may encompass other molecular moieties.
Emerging Intravascular Imaging Systems
Other combinations of imaging approaches such as integrated IVUS-OCT [66, 67], fluorescence-IVUS-OCT [68], and NIRS-OCT [69] systems have also been developed and will likely be studied more broadly in the future.
Conclusions
Several RCTs have shown benefit of IVUS-guided coronary intervention with a reduction of MACE that is mainly driven by a reduction in TLR rates. While individual trials showed a neutral effect on mortality and MI, meta-analyses suggest a reduction in cardiovascular mortality, MI, and stent thrombosis in all patients, patients with newer generation DES, and patients with complex lesions [12, 29••]. Overall, patients with ACS or complex lesions (left main, bifurcation, CTO, long lesions) appear to benefit most.
A limitation of these studies is that there are heterogeneous stent optimization protocols, and imaging catheters with variable characteristics from different vendors were used in these studies. Furthermore, imaging alone is insufficient to improve outcomes and requires both adequate interpretation skills and appropriate therapeutic reactions to imaging findings, which is currently largely operator dependent. That the benefit of IVUS is seen even with variable protocols and with many patients not reaching optimization targets [29••] likely suggests that visualization of vessel and lesion as well as the intent of the operator to achieve an optimized result contribute to better outcomes. Whether this is driven by intermediate markers such as increased minimum stent area or other optimization characteristics is currently unknown. Further efforts are necessary to establish standardized imaging interpretation protocols and to validate practical algorithms for lesion preparation, stent positioning, and stent optimization. These protocols, including automatic lumen, plaque, and stent image segmentation, and angiographic co-registration, should then be incorporated into the imaging software to assist less-experienced operators in appropriate interpretation and decision-making.
Given the reductions of TLR of about 50% using IVUS guidance, minimal complications rates, and established cost-effectiveness, the current evidence currently strongly supports use of IVUS in more complex lesions subsets, and potentially in all-comers. Other imaging modalities currently still lack the strong evidence supporting their routine use, but clinical trials for OCT and NIRS-IVUS are currently ongoing and will shed new light on how intravascular imaging may improve outcomes for PCI and CAD patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gao X-F, Wang Z-M, Wang F, Gu Y, Ge Z, Kong X-Q, et al. Intravascular ultrasound guidance reduces cardiac death and coronary revascularization in patients undergoing drug-eluting stent implantation: results from a meta-analysis of 9 randomized trials and 4724 patients. Int J Card Imaging. 2019;35:239–47. https://doi.org/10.1007/s10554-019-01555-3.
•• Zhang J, Gao X, Kan J, Ge Z, Han L, Lu S, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. J Am Coll Cardiol Intv. 2018;72:3126–37. https://doi.org/10.1016/j.jacc.2018.09.013. This is a very recent randomized controlled trial of IVUS in an all-comers population. It showed that DES implantation guided by IVUS decreased MACE by approximately 50%, primarily driven by reduced rates of target-vessel failure.
• Hong S-J, Kim B-K, Shin D-H, Nam C-M, Kim J-S, Ko Y-G, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015;314:2155–63. https://doi.org/10.1001/jama.2015.15454. First large randomized controlled trial of PCI of long lesions using ≥ 28-mm stents that demonstrated a reduction in MACE after IVUS-guided DES implantation, due to decreased need for target lesion revascularization.
Chen S-L, Ye F, Zhang J-J, Tian N-L, Liu Z-Z, Santoso T, et al. Intravascular ultrasound-guided systematic two-stent techniques for coronary bifurcation lesions and reduced late stent thrombosis. Catheter Cardiovasc Interv. 2013;81:456–63. https://doi.org/10.1002/ccd.24601.
Koskinas KC, Nakamura M, Räber L, Colleran R, Kadota K, Capodanno D, et al. Current use of intracoronary imaging in interventional practice - results of a European Association of Percutaneous Cardiovascular Interventions (EAPCI) and Japanese Association of Cardiovascular Interventions and Therapeutics (CVIT) clinical practice Sur Circ J. 2018;82:1360–8. https://doi.org/10.1253/circj.CJ-17-1144.
Potkin BN, Bartorelli AL, Gessert JM, Neville RF, Almagor Y, Roberts WC, et al. Coronary artery imaging with intravascular high-frequency ultrasound. Circulation. 1990;81:1575–85.
Jakabcin J, Spacek R, Bystron M, Kvasnák M, Jager J, Veselka J, et al. Long-term health outcome and mortality evaluation after invasive coronary treatment using drug eluting stents with or without the IVUS guidance. Randomized control trial. HOME DES IVUS. Catheter Cardiovasc Interv. 2010;75:578–83. https://doi.org/10.1002/ccd.22244.
Kim J-S, Kang T-S, Mintz GS, Park B-E, Shin D-H, Kim B-K, et al. Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv. 2013;6:369–76. https://doi.org/10.1016/j.jcin.2012.11.009.
Chieffo A, Latib A, Caussin C, Presbitero P, Galli S, Menozzi A, et al. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions: the AVIO trial. Am Heart J [Internet]. 2013;165:65–72. https://doi.org/10.1016/j.ahj.2012.09.017.
Kim B-K, Shin D-H, Hong M-K, Park HS, Rha S-W, Mintz GS, et al. Clinical impact of intravascular ultrasound-guided chronic total occlusion intervention with zotarolimus-eluting versus biolimus-eluting stent implantation: randomized study. Circ Cardiovasc Interv. 2015;8:e002592. https://doi.org/10.1161/CIRCINTERVENTIONS.115.002592.
Tian N-L, Gami S-K, Ye F, Zhang J-J, Liu Z-Z, Lin S, et al. Angiographic and clinical comparisons of intravascular ultrasound- versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions: two-year results from a randomised AIR-CTO study. EuroIntervention. 2015;10:1409–17. https://doi.org/10.4244/EIJV10I12A245.
di Mario C, Koskinas KC, Räber L. Clinical benefit of IVUS guidance for coronary stenting: the ULTIMATE step toward definitive evidence? J Am Coll Cardiol Intv. 2018;72:3138–41. https://doi.org/10.1016/j.jacc.2018.10.029.
de la Torre Hernandez JM, Hernández Hernandez F, Alfonso F, Rumoroso JR, Lopez-Palop R, Sadaba M, et al. Prospective application of pre-defined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions results from the multicenter LITRO study. J Am Coll Cardiol. 2011;58:351–8. https://doi.org/10.1016/j.jacc.2011.02.064.
Andell P, Karlsson S, Mohammad MA, Götberg M, James S, Jensen J, et al. Intravascular ultrasound guidance is associated with better outcome in patients undergoing unprotected left main coronary artery stenting compared with angiography guidance alone. Circ Cardiovasc Interv. 2017;10. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004813.
Tan Q, Wang Q, Liu D, Zhang S, Zhang Y, Li Y. Intravascular ultrasound-guided unprotected left main coronary artery stenting in the elderly. Saudi Med J. 2015;36:549–53. https://doi.org/10.15537/smj.2015.5.11251.
Liu XM, Yang ZM, Liu XK, Zhang Q, Liu CQ, Le HQ, et al. Intravascular ultrasound-guided drug-eluting stent implantation for patients with unprotected left main coronary artery lesions: a single-center randomized trial. Anatol J Cardiol. 2019;21:83–90. https://doi.org/10.14744/AnatolJCardiol.2018.21447.
Wang Y, Mintz GS, Gu Z, Qi Y, Wang Y, Liu M, et al. Meta-analysis and systematic review of intravascular ultrasound versus angiography-guided drug eluting stent implantation in left main coronary disease in 4592 patients. BMC Cardiovasc Disord. 2018;18:115. https://doi.org/10.1186/s12872-018-0843-z.
Romagnoli E, De Servi S, Tamburino C, Colombo A, Burzotta F, Presbitero P, et al. Real-world outcome of coronary bifurcation lesions in the drug-eluting stent era: results from the 4,314-patient Italian Society of Invasive Cardiology (SICI-GISE) Italian Multicenter Registry on Bifurcations (I-BIGIS). Am Heart J. 2010;160:535–542.e1. https://doi.org/10.1016/j.ahj.2010.06.028.
Chen L, Xu T, Xue X-J, Zhang J-J, Ye F, Tian N-L, et al. Intravascular ultrasound-guided drug-eluting stent implantation is associated with improved clinical outcomes in patients with unstable angina and complex coronary artery true bifurcation lesions. Int J Card Imaging. 2018;34:1685–96. https://doi.org/10.1007/s10554-018-1393-2.
Gaster AL, Slothuus Skjoldborg U, Larsen J, Korsholm L, von Birgelen C, Jensen S, et al. Continued improvement of clinical outcome and cost effectiveness following intravascular ultrasound guided PCI: insights from a prospective, randomised study. Heart. 2003;89:1043–9.
Alberti A, Giudice P, Gelera A, Stefanini L, Priest V, Simmonds M, et al. Understanding the economic impact of intravascular ultrasound (IVUS). Eur J Health Econ. 2016;17:185–93. https://doi.org/10.1007/s10198-015-0670-4.
Gaster AL, Slothuus U, Larsen J, Thayssen P, Haghfelt T. Cost-effectiveness analysis of intravascular ultrasound guided percutaneous coronary intervention versus conventional percutaneous coronary intervention. Scand Cardiovasc J. 2001;35:80–5.
Chin CY, Maehara A, Fall K, Mintz GS, Ali ZA. Imaging comparisons of coregistered native and stented coronary segments by high-definition 60-MHz intravascular ultrasound and optical coherence tomography. JACC Cardiovasc Interv. 2016;9:1305–6. https://doi.org/10.1016/j.jcin.2016.04.011.
Okada K, Kitahara H, Mitsutake Y, Tanaka S, Kimura T, Yock PG, et al. Assessment of bioresorbable scaffold with a novel high-definition 60 MHz IVUS imaging system: comparison with 40-MHz IVUS referenced to optical coherence tomography. Catheter Cardiovasc Interv. 2018;91:874–83. https://doi.org/10.1002/ccd.27197.
Ataka R, Saito N, Tsujimura A, Kato ET, Kimura T. Direct comparison of optical coherence tomography and high-definition 60-MHz intravascular ultrasound imaging of intra-procedural stent thrombosis in a patient with acute coronary syndrome. Cardiovasc Revasc Med. 2018;20:365–7. https://doi.org/10.1016/j.carrev.2018.10.011.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American College of Cardiology task force on clinical expert consensus do. J Am Coll Cardiol. 2001;37:1478–92.
Mintz GS, Garcia-Garcia HM, Nicholls SJ, Weissman NJ, Bruining N, Crowe T, et al. Clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound regression/progression studies. EuroIntervention. 2011;6(9):1123–30. https://doi.org/10.4244/EIJV6I9A195.
Safian RD, Goldstein JA. Expert consensus statement on FFR, IVUS, and OCT: focus on physiology and luminology. Catheter Cardiovasc Interv. 2014;83:519–20. https://doi.org/10.1002/ccd.25399.
•• Räber L, Mintz GS, Koskinas KC, Johnson TW, Holm NR, Onuma Y, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018;39:3281–300. https://doi.org/10.1093/eurheartj/ehy285 Recent consensus document comparing IVUS and OCT with many specific examples for each technique.
Hong M-K, Mintz GS, Lee CW, Park D-W, Choi B-R, Park K-H, et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006;27:1305–10. https://doi.org/10.1093/eurheartj/ehi882.
Calvert PA, Brown AJ, Hoole SP, Obaid DR, West NEJ, Bennett MR. Geographical miss is associated with vulnerable plaque and increased major adverse cardiovascular events in patients with myocardial infarction. Catheter Cardiovasc Interv. 2016;88:340–7. https://doi.org/10.1002/ccd.26275.
Choi S-Y, Maehara A, Cristea E, Witzenbichler B, Guagliumi G, Brodie B, et al. Usefulness of minimum stent cross sectional area as a predictor of angiographic restenosis after primary percutaneous coronary intervention in acute myocardial infarction (from the HORIZONS-AMI Trial IVUS substudy). Am J Cardiol. 2012;109:455–60. https://doi.org/10.1016/j.amjcard.2011.10.005.
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol Intv. 2012;59:1058–72. https://doi.org/10.1016/j.jacc.2011.09.079.
Prati F, Guagliumi G, Mintz GS, Costa M, Regar E, Akasaka T, et al. Expert review document part 2: methodology, terminology and clinical applications of optical coherence tomography for the assessment of interventional procedures. Eur Heart J. 2012;33:2513–20. https://doi.org/10.1093/eurheartj/ehs095.
Hu S, Yonetsu T, Jia H, Karanasos A, Aguirre AD, Tian J, et al. Residual thrombus pattern in patients with ST-segment elevation myocardial infarction caused by plaque erosion versus plaque rupture after successful fibrinolysis: an optical coherence tomography study. J Am Coll Cardiol. 2014;63:1336–8. https://doi.org/10.1016/j.jacc.2013.11.025.
Higuma T, Soeda T, Abe N, Yamada M, Yokoyama H, Shibutani S, et al. A combined optical coherence tomography and intravascular ultrasound study on plaque rupture, plaque Erosion, and calcified nodule in patients with ST-segment elevation myocardial infarction: incidence, morphologic characteristics, and outcomes after perc. JACC Cardiovasc Interv. 2015;8:1166–76. https://doi.org/10.1016/j.jcin.2015.02.026.
• Jia H, Dai J, Hou J, Xing L, Ma L, Liu H, et al. Effective anti-thrombotic therapy without stenting: intravascular optical coherence tomography-based management in plaque erosion (the EROSION study). Eur Heart J. 2017;38:792–800. https://doi.org/10.1093/eurheartj/ehw381 This study demonstred that OCT-detected plaque erosions underlying acute coronary syndromes might be able to be managed without stenting.
Bezerra HG, Attizzani GF, Sirbu V, Musumeci G, Lortkipanidze N, Fujino Y, et al. Optical coherence tomography versus intravascular ultrasound to evaluate coronary artery disease and percutaneous coronary intervention. JACC Cardiovasc Interv. 2013;6:228–36. https://doi.org/10.1016/j.jcin.2012.09.017.
Kim I-C, Nam C-W, Cho Y-K, Park H-S, Yoon H-J, Kim H, et al. Discrepancy between frequency domain optical coherence tomography and intravascular ultrasound in human coronary arteries and in a phantom in vitro coronary model. Int J Cardiol. 2016;221:860–6. https://doi.org/10.1016/j.ijcard.2016.07.080.
Maehara A, Matsumura M, Ali ZA, Mintz GS, Stone GW. IVUS-guided versus OCT-guided coronary stent implantation: a critical appraisal. JACC Cardiovasc Imaging. 2017;10:1487–503. https://doi.org/10.1016/j.jcmg.2017.09.008.
Meneveau N, Souteyrand G, Motreff P, Caussin C, Amabile N, Ohlmann P, et al. Optical coherence tomography to optimize results of percutaneous coronary intervention in patients with non-ST-elevation acute coronary syndrome: results of the multicenter, randomized DOCTORS study does optical coherence tomography optimize results of S. Circulation. 2016;134:906–17. https://doi.org/10.1161/CIRCULATIONAHA.116.024393.
• Kubo T, Shinke T, Okamura T, Hibi K, Nakazawa G, Morino Y, et al. Optical frequency domain imaging vs. intravascular ultrasound in percutaneous coronary intervention (OPINION trial): one-year angiographic and clinical results. Eur Heart J. 2017;38:3139–47. https://doi.org/10.1093/eurheartj/ehx351 This trial of OCT vs IVUS guidance vs PCI showed similar MACE rates between IVUS and OCT. There was also no difference in post-PCI minimum lumen diameter. This was an important finding as most other trials showed that OCT undersizes stents compared to IVUS.
Ali ZA, Maehara A, Généreux P, Shlofmitz RA, Fabbiocchi F, Nazif TM, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet (London, England). 2016;388:2618–28. https://doi.org/10.1016/S0140-6736(16)31922-5.
ILUMIEN IV [Internet]. [cited 2019 Jan 17].
Libby P, Pasterkamp G, Crea F, Jang I-K. Reassessing the mechanisms of acute coronary syndromes. Circ Res. 2019;124:150–60. https://doi.org/10.1161/CIRCRESAHA.118.311098.
Xing L, Yamamoto E, Sugiyama T, Jia H, Ma L, Hu S, et al. EROSION study (effective anti-thrombotic therapy without stenting: intravascular optical coherence tomography-based management in plaque erosion): a 1-year follow-up report. Circ Cardiovasc Interv. 2017;10. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005860.
Sugiyama T, Xing L, Yamamoto E, Fracassi F, Lee H, Yu B, et al. Thrombus resolution with tirofiban in the conservative management of patients presenting with plaque erosion. Coron Artery Dis. 2018;29:301–8. https://doi.org/10.1097/MCA.0000000000000614.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35. https://doi.org/10.1056/NEJMoa1002358.
Bourantas CV, Jaffer FA, Gijsen FJ, van Soest G, Madden SP, Courtney BK, et al. Hybrid intravascular imaging: recent advances, technical considerations, and current applications in the study of plaque pathophysiology. Eur Heart J. 2017;38:400–12. https://doi.org/10.1093/eurheartj/ehw097.
Stone PH, Saito S, Takahashi S, Makita Y, Nakamura S, Kawasaki T, et al. Prediction of progression of coronary artery disease and clinical outcomes using vascular profiling of endothelial shear stress and arterial plaque characteristics: the PREDICTION study. Circulation. 2012;126:172–81. https://doi.org/10.1161/CIRCULATIONAHA.112.096438.
Gardner CM, Tan H, Hull EL, Lisauskas JB, Sum ST, Meese TM, et al. Detection of lipid core coronary plaques in autopsy specimens with a novel catheter-based near-infrared spectroscopy system. JACC Cardiovasc Imaging. 2008;1:638–48. https://doi.org/10.1016/j.jcmg.2008.06.001.
Madder RD, Husaini M, Davis AT, VanOosterhout S, Harnek J, Götberg M, et al. Detection by near-infrared spectroscopy of large lipid cores at culprit sites in patients with non-ST-segment elevation myocardial infarction and unstable angina. Catheter Cardiovasc Interv. 2015;86:1014–21. https://doi.org/10.1002/ccd.25754.
Madder RD, Goldstein JA, Madden SP, Puri R, Wolski K, Hendricks M, et al. Detection by near-infrared spectroscopy of large lipid core plaques at culprit sites in patients with acute ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2013;6:838–46. https://doi.org/10.1016/j.jcin.2013.04.012.
Oemrawsingh RM, Cheng JM, García-García HM, van Geuns R-J, de Boer SPM, Simsek C, et al. Near-infrared spectroscopy predicts cardiovascular outcome in patients with coronary artery disease. J Am Coll Cardiol. 2014;64:2510–8. https://doi.org/10.1016/j.jacc.2014.07.998.
Kini AS, Baber U, Kovacic JC, Limaye A, Ali ZA, Sweeny J, et al. Changes in plaque lipid content after short-term intensive versus standard statin therapy: the YELLOW trial (reduction in yellow plaque by aggressive lipid-lowering therapy). J Am Coll Cardiol Intv. 2013;62:21–9. https://doi.org/10.1016/j.jacc.2013.03.058.
Calfon Press MA, Mallas G, Rosenthal A, Hara T, Mauskapf A, Nudelman RN, et al. Everolimus-eluting stents stabilize plaque inflammation in vivo: assessment by intravascular fluorescence molecular imaging. Eur Heart J Cardiovasc Imaging. 2017;18:510–8. https://doi.org/10.1093/ehjci/jew228.
Dixon AJ, Hossack JA. Intravascular near-infrared fluorescence catheter with ultrasound guidance and blood attenuation correction. J Biomed Opt. 2013;18:56009. https://doi.org/10.1117/1.JBO.18.5.056009.
Yoo H, Kim JW, Shishkov M, Namati E, Morse T, Shubochkin R, et al. Intra-arterial catheter for simultaneous microstructural and molecular imaging in vivo. Nat Med. 2011;17:1680–4. https://doi.org/10.1038/nm.2555.
Verjans JW, Osborn EA, Ughi GJ, Calfon Press MA, Hamidi E, Antoniadis AP, et al. Targeted near-infrared fluorescence imaging of atherosclerosis: clinical and intracoronary evaluation of indocyanine green. JACC Cardiovasc Imaging. 2016;9:1087–95. https://doi.org/10.1016/j.jcmg.2016.01.034.
Osborn EA, Jaffer FA. The advancing clinical impact of molecular imaging in CVD. JACC Cardiovasc Imaging. 2013;6:1327–41. https://doi.org/10.1016/j.jcmg.2013.09.014.
• Hara T, Ughi GJ, McCarthy JR, Erdem SS, Mauskapf A, Lyon SC, et al. Intravascular fibrin molecular imaging improves the detection of unhealed stents assessed by optical coherence tomography in vivo. Eur Heart J. 2017;38:447–55. https://doi.org/10.1093/eurheartj/ehv677 This experimental study demonstrated specific molecular imaging of fibrin to understand unhealed stents using NIRF-OCT. DES exhibited greater fibrin compared to BMS. Further standalone OCT could not distinguish fibrin coverage from endothelial coverage; NIRF molecular imaging was required.
Kolodgie FD, Gold HK, Burke AP, Fowler DR, Kruth HS, Weber DK, et al. Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med. 2003;349:2316–25. https://doi.org/10.1056/NEJMoa035655.
Saam T, Hetterich H, Hoffmann V, Yuan C, Dichgans M, Poppert H, et al. Meta-analysis and systematic review of the predictive value of carotid plaque hemorrhage on cerebrovascular events by magnetic resonance imaging. J Am Coll Cardiol. 2013;62:1081–91. https://doi.org/10.1016/j.jacc.2013.06.015.
Ughi GJ, Wang H, Gerbaud E, Gardecki JA, Fard AM, Hamidi E, et al. Clinical characterization of coronary atherosclerosis with dual-modality OCT and near-infrared autofluorescence imaging. JACC Cardiovasc Imaging. 2016;9:1304–14. https://doi.org/10.1016/j.jcmg.2015.11.020.
Htun NM, Chen YC, Lim B, Schiller T, Maghzal GJ, Huang AL, et al. Near-infrared autofluorescence induced by intraplaque hemorrhage and heme degradation as marker for high-risk atherosclerotic plaques. Nat Commun. 2017;8:75. https://doi.org/10.1038/s41467-017-00138-x.
Yin J, Li X, Jing J, Li J, Mukai D, Mahon S, et al. Novel combined miniature optical coherence tomography ultrasound probe for in vivo intravascular imaging. J Biomed Opt. 2011;16:060505. https://doi.org/10.1117/1.3589097.
Sheth TN, Pinilla-Echeverri N, Mehta SR, Courtney BK. First-in-human images of coronary atherosclerosis and coronary stents using a novel hybrid intravascular ultrasound and optical coherence tomographic catheter. JACC Cardiovasc Interv. 2018;11:2427–30. https://doi.org/10.1016/j.jcin.2018.09.022.
Liang S, Ma T, Jing J, Li X, Li J, Shung KK, et al. Trimodality imaging system and intravascular endoscopic probe: combined optical coherence tomography, fluorescence imaging and ultrasound imaging. Opt Lett. 2014;39:6652–5. https://doi.org/10.1364/OL.39.006652.
Fard AM, Vacas-Jacques P, Hamidi E, Wang H, Carruth RW, Gardecki JA, et al. Optical coherence tomography--near infrared spectroscopy system and catheter for intravascular imaging. Opt Express. 2013;21:30849–58. https://doi.org/10.1364/OE.21.030849.
Funding
The study received financial support from NIH R01 HL137913.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bode has no conflict of interest to disclose.
Dr. Jaffer is sponsored research from Canon and Siemens; he is a consultant for Boston Scientific, Abbott Vascular, Siemens, Philips, and Acrostak. Massachusetts General Hospital has a patent licensing arrangement with Canon, and Dr. Jaffer has the right to receive royalties.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Intravascular Imaging
Rights and permissions
About this article
Cite this article
Bode, M.F., Jaffer, F.A. IVUS and OCT: Current State-of-the-Art in Intravascular Coronary Imaging. Curr Cardiovasc Imaging Rep 12, 29 (2019). https://doi.org/10.1007/s12410-019-9503-7
Published:
DOI: https://doi.org/10.1007/s12410-019-9503-7