Abstract
Purpose of Review
Coronary artery anomalies (CAA) are a commonly encountered entity on computer tomography angiography (CTA) with observational studies suggesting a prevalence of 1–3%. The purpose of this pictorial review is to succinctly review the recent literature in regards to their individual prevalence, assessment and management strategies when indicated.
Recent Findings
Clinically, the most important anomalies are those with either a malignant course or origin. Recent studies have suggested that anomalous coronary arteries arising from the opposite sinus (ACAOS) are best detected on CTA. In particular, those found in asymptomatic patients over the age of 35, even with high-risk features, do not necessarily mandate revascularisation. We propose a new investigative framework. Additionally, new CTA prevalence data has emerged of individual anomalies which are further discussed.
Summary
Computer tomography angiography has emerged as the gold standard for the assessment of CAAs, and as a result, they are being encountered more frequently in clinical practice. It is important that reporting physicians have a comprehensive knowledge of these anomalies, how they are best described and categorised and particularly recognition of malignant variants that may require intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rapid growth in the use of computer tomography angiography (CTA) for the assessment of chest pain, given its non-invasive nature and very high sensitivity (95%) and negative predictive value (nearing 100%) in assessing obstructive coronary stenosis, has resulted in improvement in the management of patients with chest pain. This increased use of CTA has also significantly increased the number of incidental findings detected, including coronary artery anomalies (CAA) [1, 2••, 3, 4].
Many CAA classification schemes have been proposed; however, no single classification scheme has been widely accepted. Despite this, the majority are broadly classified as anomalies of coronary artery origin, course, termination and intrinsic anatomy [5,6,7]. The prevalence of CAA on CTA studies varies widely with prevalence documented between 0.8 and 10.4% of patients presenting for CTA [8,9,10]. Larger observational studies suggest a prevalence between 1 and 3% [11,12,13]. However, that the vast majority of prevalence data is derived from patients undergoing imaging based on clinical symptoms and therefore the true prevalence of these anomalies in the general population remains unknown.
CTA has seen significant recent advances, particularly with improved spatial resolution, temporal resolution, cranio-caudal coverage and reduction in radiation exposure, with newer scanners routinely using very low radiation doses (< 2 mSv) [14, 15]. Trials consistently demonstrate the increased diagnostic yield associated with CTA and its place as a gatekeeper for coronary angiography. The recent randomised controlled trial by Dewey et al. showed cardiac CT reduced the need for invasive coronary angiography from 100 to 14% and was associated with a significantly greater angiographic diagnostic yield from 15 to 75% patients requiring intervention [16], with no significant increase in long-term clinical events in the two groups at median follow-up of 3.3 years. Other studies have also consistently shown that CTA is at least equivalent to other imaging modalities (MRI/coronary angiogram) for detection of CAA [17] and is generally more widely available and cheaper than other anatomical tests. As a result, CTA has a class I indication for the initial assessment of patients either found to have or are suspected of having coronary artery anomalies as it allows a detailed visualisation of anatomical course and subsequent risk stratification [18].
Given the significant uptake in the use of CTA in clinical practice in low and intermediate risk patients presenting with chest pain [19], it is expected that the incidental detection of CAA will increase. It is inevitable that referring cardiologists and physicians will be confronted more commonly with this entity. Describing every coronary artery anomaly is beyond the scope of this review; however, we will outline commonly encountered anomalies, particularly those of clinical significance with CTA pictorial examples to aid CT readers in interpretation. Prevalence and management strategies will be briefly discussed where known.
Normal Coronary Anatomy and Variation
The aortic root represents the outflow tract from the left ventricle and has three coronary cusps. Located anteriorly is the right coronary sinus, giving rise to the right coronary artery (RCA), with the left main coronary artery (LMCA) arising from the left coronary cusp, then bifurcating into the left circumflex (LCx) and left anterior descending (LAD) arteries (Fig. 1). The RCA runs down the right atrioventricular groove with the conal branch arising as the first branch; however, in up to 22% of people, the conus arises directly from the aorta. In approximately 85% of individuals, the RCA gives rise to the posterior descending artery (PDA), known as right dominance. In 7% of patients, the LCx gives rise to the PDA, known as left dominance. In the remaining 8%, the RCA and LCx both provide supply to the PDA, known as co-dominance. The LMCA, usually 1–2 cm in length, arises from the aorta dividing beneath the left atrial appendix. In approximately 30% of cases, the LMCA gives rise to the third vessel between the LAD and LCx called the intermediate artery (or ramus intermedius artery).
By definition, the distinction between coronary artery anomalies and variants is based on their population prevalence. Any anatomic finding found in > 1% of the general population is defined as normal, with a normal variant describing an alternative, relatively usual finding that is found in > 1% of the same population. An anomaly is a morphological feature seen in < 1% of the population [6, 7]. However, recent studies have challenged this strict definition as some particular CAA prevalence rates have been greater than 1% of the selected populations. Normal variants of coronary arteries are considered benign entities with very limited clinical significance [11,12,13, 20, 21]. In contrast, CAAs range from being benign to those associated with a high risk of sudden cardiac death (SCD). In particular, new evidence is emerging that age plays a significant role in prognosis with various studies and authors suggesting patients with CAA under the age of 30–35 are at higher risk of events than those with CAA found later in life incidentally [18, 22••].
Anomalies of Aortic Origin
Single Coronary Artery
SCA is a rare entity with a prevalence ranging between 0.024 and 0.066% in the general population [23] in which the RCA or LMCA is absent from its respective coronary sinus of Valsalva, with one coronary artery providing blood supply to the entire heart (Fig. 2). First described posthumously in 1699 by Fantoni, SCA was only described antemortem in 1967 through the use of coronary angiography [24]. Since that time, there have been multiple classification schemes developed, however Lipton et al. [25••] modified scheme has been widely accepted and divides SCA into three groups according to the location of the ostium, anatomical distribution and the course of its branches resulting in a three letter code. The first letter refers to the originating sinus of Valsalva [i.e. left (L) or right (R)]. Second, a Roman numeral (I, II or III) describes the anatomical course of the artery. In group I, the artery follows the anatomic course of the normal LMCA or RCA. In group II, one coronary artery arises from the proximal segment of the normally located other coronary artery. In group III, the LAD and LCx each arise separately from the normally positioned RCA. The final letter refers to the relation of the coronary arteries to the great vessels (i.e., anterior (A), posterior (P), between the great vessels (B), passing through the interventricular septum (S) and combined (C)) (Supplementary Table 1).
SCA is diagnosed based on two criteria [26]: (1) the presence of a single ostium from a single coronary sinus combined with the absence of an ostium in the opposite sinus and (2) a lack of origination of another coronary artery from an ectopic location. SCA can arise from any of the three coronary sinuses, with the following order of decreasing frequency: right coronary sinus, left coronary sinus and very rarely the non-coronary sinus [27].
Prognosis of persons with SCA is unclear; however, it has been associated with major adverse cardiac events in 15% of patients before the age of 40 [28]. In particular, when the anomalous artery course is interatrial and or traverses between the aorta and pulmonary arterial trunk, this can be associated with SCD and angina [24]. It has also been postulated that given the high arterial flow of a single coronary supplying a large territory, this predisposes to development of atherosclerosis and endothelial injury. Revascularisation is only recommended in patients with significant documented atherosclerosis and medically resistant ischaemia [29]. As there are currently no treatment guidelines, the best management approach in either symptomatic or asymptomatic patients with an interarterial course is unknown and should be individually tailored to patients based on symptoms and reason for presentation. In the majority of cases, SCA remains asymptomatic and the finding is benign. Note that SCA may be dually considered as an anomaly of course, however is only discussed in this section.
Multiple Ostia
Three or more ostia from any of the coronary sinuses is considered multiple. With studies showing a prevalence of between 0.19 and 0.6%, this represents a commonly encountered anomaly [12, 30–31]. This is most commonly seen as the absence of the LMCA with the LAD and LCx and intermediate artery, if present, arising directly from the left sinus of Valsalva (Fig. 3). Additionally, the RCA and conus branch may arise from the right sinus of Valsalva, or an artery may arise from the non-coronary cusp. This anomaly in isolation causes no haemodynamic compromise and is benign with no specific treatment required.
Anomalous Coronary Artery Arising from the Opposite Sinus
ACAOS is a heterogeneous group of anomalies with variable presentation from benign incidental findings to causing SCD, especially in young athletes [32]. Prevalence estimates vary between studies and are likely to be in the range of 0.19–2.16% of all patients referred for non-invasive coronary imaging [21, 33,34,35,36]. A recent systematic review and meta-analysis showed a pooled population prevalence of 0.83%, with CTA revealing the highest pooled prevalence of all modalities assessed (ultrasound, cardiac MRI and catheter angiography) [37].
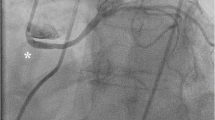
There are four different recognised types of ACAOS in order of decreasing prevalence: anomalous origin of the RCA from the left coronary sinus (Fig. 4), the LCx or Intermediate arteries from the right coronary sinus (Fig. 5), or the RCA itself, origin of the LMCA from the right coronary sinus (Fig. 6) and either the RCA or LMCA from the non-coronary sinus (Fig. 7) as the rarest variant [38]. Further sub-classification is based on the proximal course of the vessel. Courses include interarterial course (IAC), retro-aortic, trans-septal or subpulmonic and pre-pulmonic course. Only the IAC is haemodynamically significant with a well documented increased risk of SCD [32]. Further, a combination of any of the following anatomical features: acute angle of ostium, slit-like orifice or intramural course, is known to confer an increased risk and are poor prognostic markers (Supplementary Table 2) [39, 40].
a VRR of RCA (black arrow) originating from the left coronary cusp (LCC) anterior to the origin of the left main with proximal portion with an intraarterial course between the aortic and pulmonary trunks. b Axial image of RCA (white arrow) arising from the LCC. c Axial image of proximal RCA showing compression (white arrow), note inferior relation to pulmonary valve (black arrow)
There is currently considerable debate regarding the functional assessment and optimal management strategy of patients with either symptomatic or incidentally found ACAOS. Patients with ACAOS with a non-IAC, in the absence of symptoms, typically have an excellent prognosis, and intervention is not warranted. However, assessment and management of a vessel with an IAC are vital (Supplementary Table 3). Consensus in the literature focuses on thorough history taking, risk stratification, symptoms on presentation (syncope, angina or aborted SCD), anatomical factors (e.g. proximal narrowing) and individual patient factors (age, individual preference for management). Notwithstanding this, various protocols have been proposed. These mandate CTA or CMR for anatomical assessment, with varying protocols for the functional dynamic assessment with all involving invasive angiography aided by either IVUS or FFR and intra-coronary stress testing [37, 41•]. If assessed by a heart team to be clinically significant, surgical re-implantation remains the recommended treatment of choice with percutaneous coronary intervention not considered routine [37]. Current guideline recommendations for surgical revascularisation and functional assessment are shown in Supplementary Table 4 (18).
Despite the aforementioned recommendations, often focused in young patients, a recent study by Grani et al. has cast doubt on the necessity for ACAOS with IAC requiring treatment incidentally found first in middle age. In their small, retrospective matched 1:2 case control study with a mean age of 56 years, there was no significant difference in MACE rates at mean follow-up of 49 months in any of the three groups assessed (ACAOS with IAC, ACAOS without IAC and matched controls) [42•]. Despite its inherent limitations, and the absence of randomised controlled trials, this study suggests that investigation and aggressive corrective treatment should be dependent on the age of presentation or symptoms onset, not simply the anomaly itself. Similar studies and authors have supported this position [37, 43, 44].
Ectopic Origin from Non-coronary Sinus
Either the LMCA or the RCA can arise from the non-coronary sinus of Valsalva (Fig. 8), and this represents a very rare entity with no published prevalence data. Scant case reports have been documented, with contention remaining regarding its clinical significance [45, 46]. In cases found which are non-intramural and asymptomatic, it is likely a benign entity.
Ectopic Origin from Ascending Aorta
Ectopic origin of coronary arteries from the ascending aorta is a rare entity with no published prevalence. It is defined as a vessel having its ostium originating more than 5 mm above the supravalvular ridge, or 10 mm above the sinotubular junction of the proximal ascending aorta (Fig. 9) [7]. This entity does not have any inherent haemodynamic consequence, but may present technical issues in relation to coronary catheterisation (i.e. difficulty with coronary engagement) and cardiothoracic surgery (i.e. cross-clamp placement below the high origin coronary may result in unsuccessful cardioplegia) [5]. Despite the general consensus of its benign nature, others have suggested that the high location of the ectopic ostium decreases coronary perfusion due to the angle at which it leaves the aorta, resulting in a flap like mechanism restricting flow at the ostium which can cause ischaemia [47]. In the absence of symptoms, however, this anomaly should be considered benign.
Anomalies of Non-aortic Origin
Anomalous RCA from Pulmonary Artery
ARCAPA is a very rare congenital heart defect with an incidence of 0.002% in the general population, most often diagnosed incidentally [48, 49]. Most are isolated anomalies; however, 25–30% can be associated with other structural heart defects such as ventricular septal defect, aortopulmonary window, tetralogy of Fallot and aortic stenosis [50]. Clinical presentation is variable with the most common presentations being a murmur for investigation, followed by chest pain and symptoms of congestive cardiac failure. Given the lower oxygen demands of the right ventricle, ischaemia and other symptoms are often dependant on collateral supply, coronary dominance and shunt size with the majority remaining asymptomatic (Fig. 10). Despite this, in the paediatric population, surgical correction is indicated even in asymptomatic patients to prevent the development of ischaemia and to reduce the risk of SCD. Treatment in asymptomatic adults is debated; however, most would favour surgical repair despite the paucity of long-term follow-up data [51].
Anomalous LCA from Pulmonary Artery (Bland-White-Garland Syndrome)
This is a rare congenital coronary anomaly with a reported incidence of 1 in every 300,000 live births and constitutes 0.24–0.46% of all congenital cardiac disease. It is one of the most severe coronary anomalies with infant mortality rates reaching 90% if left untreated [52]. Due to the equivalent blood pressure and oxygen concentration in both left and right systems in utero, effects of this anomaly are not seen until birth, where pulmonary pressure and flow decrease resulting in low LAD blood flow and pressure. At this point, ischaemia stimulates formation of collateral supply between the RCA and LAD, with the left system subsequently draining into the low pressure pulmonary trunk leading to a ‘steal phenomenon’.
Clinical suspicion should remain high as symptoms in the paediatric population are often non-specific with colicky like crying bouts, failure to thrive, feeding difficulties and heart failure symptoms often present. In the 10% that survive to adulthood undetected, symptoms of angina, reduced exercise tolerance, smaller stature, syncope and SCD may be part of the presenting complaint. There are case reports of first diagnosis of ALCAPA in an elderly patient in their seventies [53]; however, this is extremely rare. Surgical intervention is the definitive treatment and is recommended in all, with studies showing long-term survival at 20 years nearing 95% with varying surgical techniques [54].
Anomalous Course Variation
Duplicated LAD
This increasingly recognised anomaly was initially thought to be present in approximately 1% [54] of the population; however, a more recent CTA study has demonstrated a prevalence of 4.18% [55••]. In this anomaly, two distinct segments of the LAD occupy the anterior interventricular sulcus (AIVS) of the heart. Depending on the origin, site of termination and course and location of the arteries in relation to the other anatomical structures, multiple distinct types have been reported. Currently, nine recognised variations have been described as determined by CTA with all having a ‘short’ and ‘long’ LAD. Type 1 (short LAD—origin is LAD proper, terminates high in AIVS, and Long LAD—origin LAD proper, descends LV side of AIVS and re-enters distal AIVS) is the most common variant (Fig. 11), representing 74–86% of cases [56, 57]. Rare case reports have documented origin of one branch of the LAD from the pulmonary artery with other variants possible [58].
There is no documented clinical consequence for this anomaly; however, awareness and recognition of its existence are important. In patients requiring revascularisation, issues may arise regarding surgical planning in regards to avoiding incorrect placement of arteriotomy and may impact on the number of grafts needed in the event of both LADs requiring revascularisation [57].
Myocardial Bridge
A myocardial bridge (MB) is a segment of the myocardium which overlies a coronary artery, while the coronary artery that tunnels referred to as the mural coronary artery (MCA) [59]. If the myocardium does not completely surround the whole circumference of the tunnelled segment, it is termed a ‘superficial’ bridge. If the complete circumference is surrounded, this is described as a ‘complete’ bridge (Fig. 12).
In the age of CTA, MB detection rates have increased significantly with prevalence estimated to be between 14 and 58%, compared to 0.5–16% on conventional coronary angiography [60]. Symptoms attributed to MB vary. Symptoms consistent with ischaemia may occur; however, the vast majority of patients remain asymptomatic. Multiple studies have demonstrated that atherosclerosis often accompanies MB, in particular in the proximal segment prior to the bridge, thought likely related to increased shear forces predisposing to plaque development [62••]. Recent studies have suggested that the degree of atherosclerosis was not responsible for symptoms and outcomes in patients, but was rather an epiphenomenon with no difference in the prevalence of atherosclerosis found between symptomatic and asymptomatic patients [60].
The most common site for MB is the LAD artery with incidence of between 64 and 79.4%, with the majority of these (39.3–60.4%) occurring in the mid-LAD [60, 61]. The remaining occur either in the diagonal branches of the LAD, LCX including the obtuse marginal branches or RCA, in descending order. In asymptomatic patients, this entity does not require treatment. In those with symptoms, calcium channel blockers or B-blockers are first-line treatment. Nitroglycerin should be used with caution, as reduction of pre-load can worsen symptoms by intensifying systolic compression of the bridged segment and vasodilating segments proximal to the bridge, exacerbating retrograde flow and reducing myocardial ischaemic threshold. In patients not responsive to medical management, MB resection or bypass grafting could be considered, although is rarely required. Percutaneous coronary intervention with drug eluting stents is inferior and is not routinely recommended [62••].
Intracavitary Course
Intracavitary coronary artery (ICCA) is defined as a coronary artery that courses through the myocardium and into a cardiac chamber. CTA studies have estimated a prevalence of 0.33% with two variants described. The majority (0.29%) occur in the mid to distal RCA and 0.039% in the distal LAD [63]. ICCA is thought to be a benign anomaly with no reported clinical symptoms, however does pose a challenge to invasive cardiac procedures. It can seriously complicate coronary artery bypass grafting, pacemaker insertion, ablation procedures and right heart catheterisation.
Anomalies of Termination
Coronary Fistula
Coronary artery fistula (CAF) is a rare anomaly resulting in an abnormal communication between the coronary artery and either the cardiac chambers, superior vena cava, coronary sinus or pulmonary artery or veins, bypassing the myocardial capillary bed. It has an estimated prevalence of 0.9% in CTA studies, significantly more than the previously accepted rate of 0.05–0.25% as found on coronary angiography [64]. CAF is an isolated finding in the majority of cases, however may be associated with other congenital anomalies such as atrial septal defects (ASD)/VSD, tetralogy of Fallot, aortic or pulmonary atresia and patent ductus arteriosus (PDA). The majority of patients with CAF are asymptomatic and are usually detected incidentally (Fig. 13). However, some patients may become symptomatic with the degree of symptoms often dependent on the size of the CAF and the amount of myocardium supplied.
The incidence of CAF is as follows: both coronary arteries (45.5%), from the left coronary artery (42.4%) and the right coronary artery (12.1%). Further, almost a quarter are associated with aneurysms of the coronary arteries and routinely show increased tortuosity [65]. Regardless of their point of origin, nearly 90% of fistulas drain to the right chambers of the heart. The majority of cases do not require any intervention; however, in those with medically resistant symptoms or existence of a significant right-to-left shunt causing ventricular overload, surgical repair could be considered. If detected in paediatric patients, they are usually repaired to avoid late onset complications, with registries showing very low post operative long-term mortality and morbidity rates [66, 67].
Systemic termination of a coronary artery should be distinguished from CAF. In this related condition, there is no associated enlargement or tortuosity in particular at the terminal end of the affect artery as there is no significant pressure difference between the coronary artery and the systemic artery into which it terminates. In absence of a pressure difference, which can be caused by the presence of atherosclerosis, systemic termination is unlikely to be clinically significant [5].
Coronary Artery Arcade
This is a rare anomaly involving inter-coronary communication between the terminal ends of two coronary arteries resulting in two-way blood flow with prevalence estimated at 0.02% [68]. Two types have been described, with communication between the RCA and LCx in the posterior atrioventricular groove, and communication between the LAD and PDA in the interventricular groove [69]. Unlike collaterals, these are found in otherwise angiographically smooth coronary arteries and have a well-defined muscular layer and are larger in diameter. The functional and clinical importance of this anomaly is not clear, and in the absence of symptoms does not require any intervention or treatment.
Anomalies of Intrinsic Coronary Anatomy
Congenital Coronary Stenosis
The majority of coronary artery stenoses are acquired; however, congenital coronary stenosis has been described. These can either be ostial, due to a valve-like ridge of the aortic wall or fusion of the aortic leaflets and aortic wall, or may be peripheral [70]. There is a paucity of prevalence data and management guidelines in the literature for this entity.
Congenital Coronary Ectasia or Aneurysm Formation
Coronary artery ectasia (CAE) has been reported to have a prevalence of between 0.3 and 5.3% as diagnosed on coronary angiography and is defined as a dilatation of an arterial segment diameter of > 1.5 times that of the adjacent normal coronary anatomy and can be either focal or diffuse (Fig. 14). The main aetiology is believed to be congenital (20–30%) or inflammatory (10–20%) with the remainder likely due to connective tissue disorders such as Ehlers-Danlos syndrome, Kawasaki disease and scleroderma [71].
In contrast, coronary artery aneurysm (CAAN) is defined as a diffuse focal arterial dilatation with a diameter of 2 or more times larger than that of its normal contiguous segment. CAAN are termed giant if they are > 4 times the size of the reference vessel diameter. Recent CTA studies have reported a prevalence of 2.31% of CAAN [72]. The most common cause is atherosclerosis (50%), congenital anomalies (20–30%), inflammatory or vasculitis (10–20%) and connective tissue disorders (5–10%) [73]. CAE and CAAN differ in that CAAN often involve shorter segments, their beginning and end points are sharper, and are generally encountered with a larger diameter. Both entities occur most frequently in the RCA with a 2 to 1 ratio compared to the left system [71]. Optimal management is debated with both PCI and surgery an option dependent on size, symptoms and location.
Conclusion
Coronary artery anomalies are being detected with increasing frequency given the more widespread use of CTA, so it is important for physicians reading CTA to have a comprehensive knowledge of these anomalies, in particular malignant variants that may require intervention. Previously, catheter coronary angiography was considered the gold standard for CAA assessment in those with known anomalies; however, CTA has now emerged as the preferred method given its non-invasive nature and its ability to provide excellent spatial and temporal resolution, and more accurate and reproducible anatomical assessment.
As CTA-based prevalence and long-term follow-up data become available, clinicians will be better able to estimate the risk associated with each type of CAA. In addition, given that most clinical management guidelines are based on retrospective registries and expert consensus, appropriately powered randomised controlled trials are required to better define optimal management strategies in all age groups, particularly for anomalies with a malignant course in whom surgery may be safe to avoid. Well-constructed clinical registries with long-term follow-up should also be developed to further add to the evidence base.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Schuetz GM, Zacharopoulou NM, Schlattmann P, Dewey M. Meta-analysis: noninvasive coronary angiography using computed tomography versus magnetic resonance imaging. Ann Intern Med. 2010;152:167–77.
•• von Ballmoos MW, Haring B, Juillerat P, Alkadhi H. Meta-analysis: diagnostic performance of low-radiation-dose coronary computed tomography angiography. Ann Intern Med. 2011;154:413–20. Meta-analysis of 16 studies including 960 patients suggesting that low-dose coronary CTA matches the sensitivity of catheter-based angiography, and is a potential alternative
Verdini D, Lee AM, Prabhakar AM, Abbara S, Ghoshhajra B. Detection of cardiac incidental findings on routine chest CT: the impact of dedicated training in cardiac imaging. J Am Coll Radiol. 2016;(30):1–5. S1546-1440(16)00140-X
De Graaf FR, Schuijf JD, van Velzen JE, Kroft LJ, de Roos A, Reiber JHC, et al. Diagnostic accuract of 320-row multidetector computed tomography coronary angiography in non-invasive evaluation of significant coronary artery disease. Eur Heart J. 2010;35:1908–15.
Shriki JE, Shinbone JS, Rashid MA, Hindoyan A, Withey JG, DeFrance A, Cunningham M, OliveiraGR, Warren BH, Wilcox A. Identifying, characterizing, and classifying congenital anomalies of the coronary arteries. Radiographics. 2012;32(2):453–68.
Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007;115:1296–305.
Angelini P. Normal and anomalous coronary arteries: definitions and classification. Am Heart J. 1989;117:418–34.
Rao A, Pimpalwar Y, Yadu N, Yadav RK. A study of coronary artery variants and anomalies ovserved at a tertiary care armed forces hospital using 64-slice MDCT. Indian Heart J. 2017;69(1):81–6.
Tongut A, Ozyedek Z, Cerezci I, Erenturk S, Hatemi AC. Prevalence of congenital coronary artery anomalies as shown by multi-slibe computer tomography coronary angiography: a single-centre study from Turkey. J Int Med Res. 2016;44(6):1492–505.
Krupinsli M, Urbanczyk-Zawadzka M, Laskowicz B, Irzyk M, Banys R, Klimeczek P, et al. Anomalous origin of the coronary artery from the wrong coronary sinus elevated with computed tomography: “high risk” anatomy and its clinical relevance. Eur Radiol. 2014;24(10):2353–9.
Grani C, Benz DC, Schmied C, Vontobel J, Possner M, Clerc OF, et al. Prevalence and characteristics of coronary artery anomalies detected by coronary computer tomography angiography in 5634 consecutive patients in a single centre in Switzerland. Swiss Med Wkly. 2016;146:w14294.
Namgung J, Kim JA. The prevalence of coronary anomalies in a single centre in Korea: origination, course, and termination anomalies of aberrant coronary arteries detected by ECG-gated cardiac MDCT. BMC Cardiovasc Disord. 2014;14:48.
Cheng Z, Wang X, Duan Y, Wu L, Wu D, Lian C, et al. Detection of coronary artery anomalies by dual-source CT coronary angiography. Clin Radiol. 2010;65(10):815–22.
Fuchs TA, Stehli J, Bull S, Dougoud S, Clerc OF, Herzog BA, et al. Coronary computed tomography angiography with model-based iterative reconstruction using a radiation exposure similar to chest X-ray examination. Eur Heart J. 2014;35(17):1131–6.
Halliburton SS, Abbara S, Chen MY, et al. For Society of Cardiovascular Computed Tomography. SCCT guidelines on radiation dose and dose optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr. 2011;5:198–224.
Dewey M, Rief M, Martus P, Kendziora B, Feger S, Dreger H, et al. Evaluation of computer tomography in patients with atypical angina or chest pain clinically referred for invasive coronary angiography: randomised controlled trial. BMJ. 2016;355:i5441.
Raval A, Jadhav N, Prajapati J, Rawal J, Garg R, Shah K, et al. Distribution of coronary artery anomalies and their evaluation with different imaging modalities. Int J Med Res Rev. 2016;10:1807–19.
Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to develop guidelines on the Management of Adults with Congenital Heart Disease): developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e143–263.
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949–3003.
McLarry J, Maros F, Shapiro MD. Coronary artery anomalies: a pictorial review. Curr Cardiovasc Imaging Rep. 2015;8:23.
Nasis A, Machado C, Cameron JD, Troupis JM, Meredith IT, Seneviratne SK. Anatomic characteristics and outcome of adults with coronary arteries arising from an anomalous location detected with coronary computed tomography angiography. Int J Cardiovasc Imaging. 2015;31(1):181–91.
•• Cheezum MK, Libertson RR, Shah NR, Villines TC, O’Gara PT, Landzberg MJ. Blankstein. Anomalous aortic origin of a coronary artery from the inappropriate sinus of valsalva. JACC. 2017;69:1592–608. Excellent comprehensive state of the art review discussing ACAOS
Desmet W, Vanhaecke J, Vrolix M, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. 1992;13:1637–40.
Mandal S, Sameh ST, Shephaly S, Shobhit M. Single coronary artery anomaly: classification and evaluation using multidetector computed tomography and magnetic resonance angiography. Pediatr Cardiol. 2014;35:441–9.
•• Lipton MJ, Barry WH, ORbez I, et al. Isolated single coronary artery: diagnosis, angiographic classification, and clinical significance. Radiology. 1979;130:39–47. Sentinel paper and description of classification criteria of single coronary artery
Angelini P, Fairchild VD. Coronary artery anomalies: a comprehensive approach. Philadelphia: Lippincott Williams & Wilkins; 1999.
Smith JC. Review of single coronary artery with report of 2 cases. Circulation. 1950;1(5):1168–75.
Sharabaugh AH, White RS. Single coronary artery/ analysis of the anatomic variation, clinical importance, and report of five cases. JAMA. 1974;230:243–6.
Aldana-Sepulveda N, Restrepo S, Kimura-Hayama E. Single coronary artery: Spectrum of imaging and findings with multi-detector CT. J Cardiovasc Comput Tomogr. 2013;7:391–9.
Pan C, Azhati G, Xing Y, Wang Y, Liu W. Comparison of congenital artery anomalies between Uyghur and Han: a multi-slice computed tomography study in Xinjiang, China. Chin Med J. 2015;128:15–9.
Graidis C, Dinitriadis D, Karasavvidis V, Dimitriadis G, Argyropoulou E, Economou F, et al. Prevalence and characteristics of coronary artery anomalies in an adult population undergoing multi-detector-row computed tomography for the evaluation of coronary artery disease. BMC Cardiovasc Disord. 2015;15:112.
Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden cardiac death in competitive athletes. J Am Coll Cardiol. 2000;35:1493–501.
Ripley DP, Saha A, Teis A, Uddin A, Bijsterveld P, Kidambi A, et al. The distribution and prognosis of anomalous coronary arteries identified by cardiovascular magnetic resonance: 15 year experience from two tertiary centres. J Cardiovasc Magn Reson. 2014;16:34.
Cheezum MK, Ghoshhajra B, Bittencourt MS, Hulten EA, Bhatt A, Mousavi N, et al. Anomalous origin of the coronary artery arising from the opposite sinus: prevalence and outcomes in patients undergoing coronary CTA. Eur Heart J Cardiovasc Imaging. 2017;18:224–35.
Opolski MP, Pregowski J, Kruk M, Witkowski A, Kwiecinska S, Lubienska E, et al. Prevalence and characteristics of coronary anomalies originating from the opposite sinus of valsalve in 8522 patients referred for coronary computed tomography angiography. Am J Cardiol. 2013;9:1361–7.
Ghadri JR, Kazakauskaite E, Braunschweig S, Burger IA, Frank M, Fiechter M, et al. Congenital coronary anomalies detected by coronary computed tomography compared to invasive coronary angiography. BMC Cardiovasc Disord. 2014;14:81.
Heermann P, Heindel W, Shulke C. Coronary artery anomalies: diagnosis and classification based on cardiac CT and MRI (CMR) - from ALCAPA to anomalies of termination. Rofo. 2017;1:29–38.
Shuaib W, Arepalli C, Vijayasarathi A, Gunn ML, Nicolau S, Mehta AS, Johnson JO, Khosa F. Coronary anomalies encountered in the acute setting: an imaging review Emerg Radiol. 2014;21(6):631–41.
Lorenz EC, Mookadam F, Mookadam M, Moustafa S, Zehr KJ. A systematic review of anomalous coronary anatomy and an examination of the association with sudden death. Rev Cardiovasc Med. 2006;7:205–13.
Sintek MA, Singh J, Billadello JJ. Dynamic evaluation of coronary anomalies originating from the opposite sinus of valsalva (ACAOS). Curr Treat Options Cardiovasc Med. 2015;17:47.
• Van Hare GF, Ackermann MJ, Evangelista JA, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task Fforce 4: congenital heart disease: a scientific statement form the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66:2372–84. Most recent guideline recommendations for athletes with CAA
• Grani C, Benz DC, Steffen DA, Clerc OF, Schmied C, Possner M, et al. Outcome in middle-aged individuals with anomalous origin of the coronary artery from the opposite sinus: a matched cohort study. Eur Heart J. 2017;0:1–8. Albeit a small case-control study of 68 patients, showed that new incidental diagnosis of middle-aged individuals with ACAOS did not have a statistically different outcome to matched controls with no coronary artery anomalies regardless of whether there was IAC or not
Furbatto F, Esposito G, Raffaele P. Coronary angioplasty and stenting for acute coronary syndrome in patients with isolated single coronary artery: a report of two cases. J Cardiovasc Med. 2009;10(7):550–3.
Clark RA, Marler AT, Lin CK, McDonough RJ, Prentice RL, Malik JA, et al. A review of anomalous origination of coronary artery from an opposite sinue of Valsalva (ACAOS) impact on major adverse cardiovascular events based on coronary computerized tomography angiography: a 6-year single centre review. Ther Adv Cardiovasc Dis. 2014;8:237–41.
Adebo D, Jacobson Z, Harris MA. Anomalous origin of the right coronary artery from the posterior, non-coronary sinus of Valsalva diagnosed by cardiac magnetic resonance imaging. Cardiol Young. 2015;25:1006–8.
Eren B, Turkmen N, Senel B. Ectopic high origin of a coronary artery from the aorta – a possible cause of sudden cardiac death. Acta Med Austriaca. 2009;52(4):171–2.
Williams IA, Gersony WNm Hellengrand WE. Anomalous right coronary artery arising from the pulmonary artery: a report of 7 cases and a review of the literature. Am Heart J. 2006;152:1004 e1009–17 e1009.
Gibernau JMA, Recalde AA, Marques RB. ARCAPA syndrome in adulthood. Rev Esp Cardiol. 2017;20:S1885–5857.
Gupta R, Marwah A, Shrivastava S. Anomalous origin of the right coronary artery from the pulmonary artery. Ann Pediatr Cardiol. 2012;5:95–6.
Al-Dairy A, Rezaei Y, Pouraliakbar H, Mahdavi M, Bayati P, Gholampour-Dehaki M. Surgical repair for anomalous origin of the right coronary artery from the pulmonary artery. Korean Circ J. 2017;47(1):144–7.
Pena E, Nguyen ET, Merchant N, Dennie C. ALCAPA syndrome: not just a pediatric disease. Radiographics. 2009;29(2):553–65.
Yew KL, Kang Z, Anum A. Late presentation of ALCAPA syndrome in an elderly Asian lady. Med J Malaysia. 2016;71(4):217–9.
Lange R, Vogt M, Horer J, Cleuziou J, Menzel A, Holper K, et al. Long-term results of repair of anomalous origin of the left coronary artery from the pulmonary artery. Ann Thorac Surg. 2007;83(4):1463–71.
Spindola-Franco H, Grose R, Solomon N. Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Am Heart J. 1983;105:445–55.
•• Bozlar U, Ugurel MS, Sari S, Akgun V, Ors F, Tasar M. Prevalence of dual left anterior descending artery variations in CT angiography. Diagn Interv Radiol. 2015;21:34–41. Comprehensive review and original data of dual LAD variations describing 9 types
Agarwal PP, Kazerooni EA. Dual left anterior descending coronary artery: CT findings. AJR. 2008;191(6):1698–701.
Vohra A, Narula H. Dual left anterior descending artery with anomalous origin of long LAD from pulmonary artery – rare coronary anomaly detected on computed tomography coronary angiography. Indian J Radiol Imagin. 2016;26(2):201–5.
Alegria JR, Herrmann J, Holmes JDR, et al. Myocardial bridging. Eur Heart J. 2005;26:1159–68.
Liu G, Qu Y, Chen X, Liao M, Hu H, Cao Y, et al. Measurements of myocardial bridges on computed tomography predict presence of clinical symptoms and outcomes of adverse heart events: a retrospective study in a large population from China. Acta Radiol. 2017;58(9):1068–1076; 284185116682380
Ma E, Ma G, Yu H, Wu W, Li K. Assessment of myocardial bridge and mural coronary artery using gated 256-slice CT angiography: a retrospective study. Sci World J. 2013:1–6; 947876
Nakaura T, Nagayoshi Y, Awai K, Utsunomiya D, Kawano H, Ogawa H, et al. Myocardial bridging is associated with coronary atherosclerosis in the segment proximal to the site of bridging. J Cardiol. 2014;63(2):134–9.
•• Corban MT, Hung OY, Eshtehardi P, Rasoul-Arzrumly E, McDaniel M, Mekonnen G, et al. Myocardial bridging: contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. JACC. 2014;63(22):2346–55. A comprehensive review of the pathophysiology, diagnostic modalities and therapeutic options for myocardial bridging
Masoomi R, Shah Z, Surineni K, Rosamond T. The prevalence and anatomical patterns of intracavitary coronary arteries: detection by coronary computed tomographic angiography. JACC. 2016;65(10S):A1128.
Lim JJ, Jung JI, Lee BY, et al. Prevalence and types of coronary artery fistulas detected with CT angiography. Am J Roentgenol. 2014;203(3):W237–43.
Dashottar S, Singh RK, Malani SK, Sarin A, Arora HS. Role of 256-slice MDCT in the evaluation of coronary artery fistula: a case series with review of the literature. Med J Armed Forces India. 2016;72(4):393–9.
Loukas M, Germain AS, Gabriel A, John A, Rubbs RS, Spicer D. Coronary artery fistula: a review. Cardiovasc Pathol. 2015;24(3):141–8.
Zhang W, Hu R, Zhang L, Zhu H, Zhang H. Outcomes of surgical repair of pediatric coronary artery fistulas. J Thorac Cardiovasc Surg. 2016;152(4):1123–30.
Abreu G, Nabais S, Enes V, Marques J, Costa J, Correia A. Coronary arcade: a rare anomaly of coronary circulation. Rev Port Cardiol. 2014;33(4):241.e1–5.
Gur M, Yilmaz R, Demirbag R. Unidirectional communication between the circumflex and right coronary arteries: a very rare coronary anomaly and cause for ischaemia. Int J Cardiovasc Imaging. 2006;22:339–42.
Montaudon M, Latrabe V, Iriart X, et al. Congenital coronary arteries anomalies: review of the literature and multidetector computer tomorgraphy (MDCT) appearance. Surg Radiol Anat. 2007;29:343–55.
Morrad B, Yazici HU, Aydar Y, Ovali V, Nadir A. Role of gender in types and frequency of coronary artery aneurysm and ectasia. Medicine (Baltimore). 2016;95(31):e4395.
Forte E, Aiello M, Inglese M, Infante T, Soricelli A, Tedeschi C, et al. Coronary artery aneurysms detected on computed tomography coronary angiography. Eur Heart J Cardiovasc Imaging. 2016;
Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 1983;67:134–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cardiac Computed Tomography
Rights and permissions
About this article
Cite this article
Nogic, J., Nerlekar, N. & Nasis, A. Anomalous Coronary Arteries on Computer Tomography Angiography: a Pictorial Review. Curr Cardiovasc Imaging Rep 10, 35 (2017). https://doi.org/10.1007/s12410-017-9430-4
Published:
DOI: https://doi.org/10.1007/s12410-017-9430-4