Abstract
Both attention-deficit/hyperactivity disorder (ADHD) and catechol-O-methyltransferase (COMT) genotype have been linked to altered dopaminergic transmission and possible impairment in frontal lobe functioning. This study offers an investigation of a possible interaction between ADHD diagnosis and COMT genotype on measures of working memory and executive function. Thirty-five adults with ADHD, who were recruited from the ADHD outpatient clinic at the Department of Psychiatry, Psychosomatics and Psychotherapy, University of Würzburg, and thirty-five matched healthy controls completed the Digit Span test and the Stroop Color Word Test. While there were no main effects of ADHD or COMT, the two factors interacted on both Digit Span subtests with the two groups’ met/met carriers showing significantly different performance on the Digit Span Forward subtest and the val/val carriers showing significantly different performance on the Digit Span Backward subtest. Findings provide preliminary support for a differential impact of COMT genotype on working memory measures in adult patients with ADHD compared to healthy controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
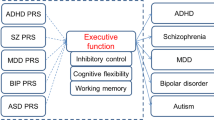
Attention-deficit/hyperactivity disorder (ADHD) is known to impair the regulation of activity, behavioral impulses, and attention as well as various higher-order cognitive processes like inhibitory control (Boonstra et al. 2005) and working memory (Barkley 1997; Martinussen et al. 2005; Willcutt et al. 2005). Etiological models link ADHD to abnormalities in corticostriatal dopaminergic circuits (Sonuga-Barke 2005). Neuroimaging findings support these theories by showing altered dopamine turnover in the striatum of ADHD patients, with methylphenidate—a medication known to counteract symptoms of ADHD—acting in the striatum by blocking dopamine reuptake and thereby increasing synaptic dopamine levels (Krause et al. 2000, 2003).
The gene coding the enzyme catechol-O-methyltransferase (COMT), which degrades neurotransmitters such as dopamine (Axelrod 1957), has previously been studied as a potential candidate gene for ADHD and for possible neuropsychological phenotypes with conflicting results (Caylak 2012; Kebir and Joober 2011; Kebir et al. 2009). Due to the low expression of the dopamine transporter in the prefrontal cortex, the COMT enzyme plays a critical role in clearing dopamine from the synaptic cleft in this area (Dickinson and Elvevag 2009; Lewis et al. 2001, 1997; Meyer-Lindenberg and Weinberger 2006; Tunbridge et al. 2004). Furthermore, the activity of COMT has been hypothesized to influence striatal dopamine levels by acting on dopamine that has diffused from the synaptic cleft (Bilder et al. 2004). Within the COMT gene, a functional single nucleotide polymorphism (rs4680) causes a valine (val) to methionine (met) substitution at codon 158 (val 158 met) (Lachman et al. 1996), which leads to COMT isoforms that differ greatly in thermolability (Lotta et al. 1995). Two met alleles lead to a three to four times lower activity of COMT compared to two val alleles, with heterozygosity leading to intermediate COMT activity (Chen et al. 2004; Weinshilboum et al. 1999).
According to the tonic-phasic model of subcortical dopaminergic functioning, the sustained tonic release of dopamine can regulate the intensity of the transient phasic dopaminergic response to relevant stimuli (Grace 1991). In the cortex, the lower COMT activity associated with two met alleles has furthermore been hypothesized to lead to increased cortical dopamine concentrations and thus increased stimulation of D1 receptors (Bilder et al. 2004). This might result in increased stability of the neural networks underlying working memory functions in met/met carriers. In contrast, the lower concentrations of cortical dopamine caused by two val alleles should lead to increased D2 transmission and thus increased flexibility of these networks in val/val carriers (Bilder et al. 2004; Levy 2007).
The influence of the COMT polymorphism on higher-order cognitive functioning was previously explored in behavioral studies: Healthy met/met carriers showed better performance on a letter-number-sequencing test (Bruder et al. 2005), an n-back task (Goldberg et al. 2003), and the Wisconsin Card Sorting Test (Egan et al. 2001) than val/val carriers, with val/met carriers usually performing in between. A recent meta-analysis showed a positive association of two met alleles with IQ score. Associations for n-back performance were less clear, with two met alleles being associated with better performance for patient populations but one val allele being associated with better performance for non-patient populations (Barnett et al. 2008). The clinical studies reviewed in this meta-analysis examined the performance of schizophrenic patients. One of these studies found worse performance for all val/val carriers irrespective of diagnostic status (Diaz-Asper et al. 2008), while the other study focused on fMRI activation and suspected a left shift of the inverted-U response curve of schizophrenic patients, leading to less efficient prefrontal functioning (Bertolino et al. 2006).
To our knowledge, only one study examined a sample of adults with ADHD to investigate the influence of COMT genotype on various measures of neurocognitive performance. This study found a positive association of the val/met genotype and full-scale IQ as assessed with the Wechsler Adult Intelligence Scale (WAIS) (Boonstra et al. 2008). The authors report no main effect of COMT genotype on the WAIS subtests Digit Span Forward or Digit Span Backward or the Stroop Color Word Test. Two similar studies of children with ADHD found no effect of COMT genotype on performance on various measures of executive function (Mills et al. 2004; Taerk et al. 2004). However, a third study reports a negative association of val/val genotype and a delayed-match-to-sample task in children (Matthews et al. 2012), while a fourth study with children found a negative association of the met allele and a measure of sustained attention (Bellgrove et al. 2005). Overall, studies of the impact of COMT in ADHD patients show greatly differing results. This heterogeneity of results either might be caused by the different types of working memory measures used in these studies (Matthews et al. 2012) or might point to an effect of COMT on cognition that is less robust than originally assumed. Our review of the literature yielded only one study that examined COMT genotype and neurocognitive performance in adult ADHD (aADHD) patients, while four studies investigated children and adolescents. None of the above-mentioned studies investigated a healthy control group.
Our study included carefully diagnosed adult ADHD patients and a healthy control group comparable with regard to age, gender, and years of formal schooling. All participants completed neuropsychological measures of verbal short-term memory, verbal working memory, and inhibitory control. The aim was to preliminarily investigate whether a possible influence of COMT genotype on task performance interacted with participants’ ADHD diagnosis. The tasks were the same as in a previous study on aADHD and COMT (Boonstra et al. 2008). However, contrary to this study, we also included a well-matched healthy control group to investigate possible interactive effects of these two factors. As COMT might influence performance on cognitive tasks across both patients and healthy controls, our study aimed to investigate whether adult patients with ADHD—a disorder known to affect dopaminergic transmission (Krause et al. 2000)—might be at an additional disadvantage caused by their COMT genotype. Furthermore, aADHD patients in our study were medication naïve or without medication for at least 3 months, meaning that any observed effects would likely not be induced by present stimulant treatment or the short-term discontinuation thereof.
Based on previous studies (Boonstra et al. 2005; Martinussen et al. 2005; Willcutt et al. 2005), we expected aADHD patients to perform worse than healthy controls on all investigated measures of higher-order cognitive functioning. Furthermore, according to the tonic-phasic model of dopaminergic functioning (Bilder et al. 2004; Grace 1991), the COMT val allele should be more detrimental to aADHD patients than to healthy controls in a gene dosage fashion, with val/val aADHD patients showing the worst performance.
Methods
Participants
A total of 70 participants (thirty-five patients with ADHD and thirty-five healthy controls) of Caucasian ethnicity took part in a larger study that comprised fMRI measurements and neuropsychological assessments and were included in the analysis. The results of the fMRI measurements will be published elsewhere. Forty-one patients with aADHD were originally recruited from the ADHD outpatient clinic at the Department of Psychiatry, Psychosomatics, and Psychotherapy of the University of Würzburg. Of all recruited aADHD patients, three did not meet full inclusion criteria. Three more patients decided not to proceed with the study after inclusion. Diagnoses were made by an experienced psychiatrist according to DSM-IV-TR (2000). Patients had to be medication naïve or without medication for at least 3 months prior to testing. Of the investigated sample, 29 % (10 patients) had previously been treated with methylphenidate and/or atomoxetine, and 11 % (4 patients) had previously been treated with an antidepressant or antipsychotic. For 7 patients, no data regarding previous psychopharmacological treatment could be obtained.
To corroborate the initial diagnosis, all patients were administered the Wender-Reimherr-Interview (WRI) (Corbisiero et al. 2010), the Conners’ Adult ADHD Rating Scales (CAARS) (Conners et al. 1999), and the Wender Utah Rating Scale (WURS) (Ward et al. 1993). To assess possible comorbid axis I disorders (an exclusion criterion) and axis II disorders, all patients were assessed with the Structured Clinical Interview for DSM-IV (SCID-I and SCID-II) (Wittchen et al. 1997), the Hamilton Depression Rating Scale (HAM-D) (Hamilton 1960), and the Hamilton Anxiety Rating Scale (HAM-A) (Hamilton 1959). Of the investigated sample, 17 % (6 patients) fulfilled diagnostic criteria for an axis II disorder. Unfortunately, no reliable data regarding comorbid axis II disorders could be obtained for 4 of the investigated patients.
Healthy controls without a past or present diagnosis of ADHD were recruited from a previously established sample (see also Biehl et al. 2013; Gschwendtner et al. 2012) as well as through university advertisement. All participants had normal or corrected-to-normal vision, and control participants were free of neurological or psychiatric diseases. A subset of 35 healthy control participants was chosen from all recruited participants to match the patient group most closely in a case–control design (p > .1 for age, gender, and years of schooling; see Table 1 for sample characteristics). All participants completed the Adult ADHD Self-Report Scale (ASRS) to obtain an estimate of any current ADHD-related symptomatology (Kessler et al. 2005).
Procedure
All participants completed the Digit Span subtest from the German version of the WAIS (Aster et al. 2006). This test consists of increasingly long strings of 2–9 digits (forward) or 2–8 digits (backward), which are read to the participants at a speed of one digit per second. The participant is then asked to repeat these digits back to the examiner, either in the presented order (Digit Span Forward) or in backward order (Digit Span Backward). If the participant can give the correct answer for at least one of two presented strings, the examiner moves on to the next longer string. The number of correctly repeated strings for each of the two subtests is used as performance measure.
Participants also completed a German version of the Stroop Color Word Test (Bäumler 1985). This test comprises three different subtasks: Naming the color of color blocks, reading color words, and naming the color that was used to print color words (e.g., if the word “blue” is printed in red ink, the participant is required to say “red”). Each subtask is completed three times, and the median completion times are used in the analysis. We analyzed the time for naming the color of color blocks as a measure of psychometric speed. The time for naming the color of color words was then divided by the psychometric speed to obtain a measure of inhibitory control.
In addition, the standard progressive matrices (Kratzmeier and Horn 1988) were administered to obtain an estimate of intellectual functioning. All participants were genotyped for the COMT val 158 met polymorphism. Blood was taken and DNA was extracted using a standard desalting procedure. A standard PCR procedure (slightly modified from the protocol used by Egan et al. 2001) was used to determine COMT genotypes, which did not deviate from Hardy–Weinberg equilibrium. Eighteen participants were genotyped as met/met (control group: 8; patient group: 10), thirty-five as val/met (control group: 17; patient group: 18), and seventeen as val/val (control group: 10; patient group: 7).
Statistical analysis
Given the unequal cell sizes caused by the distribution of the COMT genotype in the general population, data were analyzed using a nonparametric equivalent of a two-way analysis of variance (ANOVA) that ranks observations for the levels of one factor within the levels of the other factor (Prescott and Shahlaee 1999; Shirley 1987). Number of correctly reproduced strings in Digit Span Forward, number of correctly reproduced strings in Digit Span Backward, and the median time for naming the color of color words divided by psychometric speed each served as dependent variables. ADHD diagnosis and COMT genotype were entered as fixed factors in all analyses. Mann–Whitney U tests for independent samples were used for post hoc comparisons, and Cohen’s d is reported to provide a measure of effect size for the post hoc tests. For all analyses, p < .05 was considered significant.
Results
For Digit Span Forward (verbal short-term memory), we found no significant main effect of ADHD diagnosis (p = .16) or COMT genotype (p = .28). There was, however, a trend level interaction of ADHD diagnosis and COMT genotype (F (2,64) = 2.81, p = .07). Post hoc tests revealed a significant difference between the two groups for carriers of the met/met genotype (p = .03, d = 1.0), with the group with ADHD performing significantly worse than the healthy control group (see Fig. 1; see Table 2 for all means and standard deviations). There were no comparable differences for carriers of the val/met genotype (p = .25, d = 0.4) or the val/val genotype (p = .54, d = 0.3).
For Digit Span Backward (verbal working memory), we similarly found no significant main effect of ADHD diagnosis (p = .24) or COMT genotype (p = .85). However, there was a significant interaction of ADHD diagnosis and COMT genotype (F (2,64) = 3.27, p = .04). Post hoc tests revealed a significant difference between the two groups for carriers of the val/val genotype (p = .03, d = 1.3), with the group with ADHD performing significantly worse than the healthy control group (see Fig. 1). There were no comparable differences for carriers of the met/met genotype (p = .83, d = 0.3) or the val/met genotype (p = .37, d = 0.5).
For the Stroop Color Word Test (inhibitory control), we found neither a significant main effect of ADHD diagnosis (p = .64) nor COMT genotype (p = .37) nor a significant interaction (p = .40).
Discussion
This study aimed to investigate a possible interaction effect of COMT genotype and adult ADHD on different measures of working memory and executive function. A possible limitation of this investigation concerns the selection of the patient sample. As inclusion criteria were rather strict, the obtained results might only apply to a subgroup of aADHD patients, who are still comparably well adjusted.
A further limitation of this study is the small sample size for some of the cells. Caused by the distribution of the val and met alleles in Caucasian populations (Palmatier et al. 1999), we investigated fewer homozygous than heterozygous participants. Especially for the homozygous participants, it is therefore possible that some other factor might have differed between the investigated groups and was not sufficiently counterbalanced, thus affecting the reported results. Although our results can therefore only be regarded as preliminary, we still found interaction effects of genotype and ADHD diagnosis on measures of verbal short-term memory and verbal working memory. Interestingly, the results show substantial effect sizes for a differential impact of COMT genotype and ADHD depending on the nature of the task: While met/met carriers with ADHD seemed to be at a disadvantage on the measure of verbal short-term memory compared to the other genotypes and healthy controls, val/val carriers with ADHD did not seem to profit in the same way as healthy val/val carriers on the measure of verbal working memory. There were no significant effects for the Stroop Color Word Test.
This pattern of results is more complex than initially hypothesized. Still, our results can be interpreted in terms of the tonic-phasic model of increased stability or flexibility, depending on COMT genotype (Barnett et al. 2008; Bilder et al. 2004; Durstewitz and Seamans 2008; Matthews et al. 2012): The measure of verbal short-term memory (Digit Span Forward) required the reproduction on increasingly long strings of numbers. It would therefore seem logical for met/met carriers to show better performance, as increased tonic dopamine—and thereby increased representational stability—would be advantageous in this task. However, compared to the healthy control group, the group with ADHD did not show this advantage. This finding is in line with another study that reported worse performance for met allele carriers with ADHD on a measure of sustained (i.e., stable) attention (Bellgrove et al., 2005). In contrast, the measure of verbal working memory (Digit Span Backward) required retention of lists of numbers as well as internal manipulation of these lists before reproduction. It could therefore be expected to favor val/val carriers as this genotype affords increased phasic dopamine and thereby increased mental flexibility. Compared to healthy controls, patients with ADHD again did not show the expected advantage.
To summarize, although we did not find main effects of COMT or ADHD on the investigated measures, two of the three tasks showed interactions of COMT genotype and ADHD diagnosis. Our results therefore point to a possible shift in the hypothesized inverted-U response curve of dopaminergic functioning in adults with ADHD compared to healthy controls (Bellgrove et al. 2005; Mattay et al. 2003).
Given our relatively small overall sample size, the achieved power was certainly not sufficient to detect more subtle differences. These results do, however, point to the possibility of differential COMT effects in patients with ADHD compared to healthy controls. Given this effect of COMT in patients and in non-patients found in our study and also in the general COMT literature (Barnett et al. 2008), future patient studies would likely benefit from including healthy control groups.
References
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Publishing, Arlington
Aster M, Neubauer A, Horn R (2006) Wechsler Intelligenztest für Erwachsene (WIE). Deutschsprachige Bearbeitung und Adaptation des WAIS-III von David Wechsler. London, Harcourt Assessment
Axelrod J (1957) O-Methylation of epinephrine and other catechols in vitro and in vivo. Science 126(3270):400–401
Barkley RA (1997) Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 121(1):65–94. doi:10.1037/0033-2909.121.1.65
Barnett JH, Scoriels L, Munafo MR (2008) Meta-analysis of the cognitive effects of the catechol-O-methyltransferase gene val158/108met polymorphism. Biol Psychiatry 64(2):137–144. doi:10.1016/j.biopsych.2008.01.005
Bäumler G (1985) Farbe-Wort-Interferenztest (FWIT) nach J. R. Stroop - Handanweisung. Göttingen, Verlag für Psychologie
Bellgrove MA, Domschke K, Hawi Z, Kirley A, Mullins C, Robertson IH et al (2005) The methionine allele of the COMT polymorphism impairs prefrontal cognition in children and adolescents with ADHD. Exp Brain Res 163(3):352–360. doi:10.1007/s00221-004-2180-y
Bertolino A, Caforio G, Petruzzella V, Latorre V, Rubino V, Dimalta S et al (2006) Prefrontal dysfunction in schizophrenia controlling for COMT Val(158)Met genotype and working memory performance. Psychiatry Res Neuroimaging 147(2–3):221–226. doi:10.1016/j.pscychresns.2006.04.001
Biehl SC, Ehlis AC, Müller LD, Niklaus A, Pauli P, Herrmann MJ (2013) The impact of task relevance and degree of distraction on stimulus processing. BMC Neurosci 14:107. doi:10.1186/1471-2202-14-107
Bilder RM, Volavka J, Lachman HM, Grace AA (2004) The catechol-O-methyltransferase polymorphism: relations to the tonic-phasic dopamine hypothesis and neuropsychiatric phenotypes. Neuropsychopharmacology 29(11):1943–1961. doi:10.1038/sj.npp.1300542
Boonstra AM, Oosterlaan J, Sergeant JA, Buitelaar JK (2005) Executive functioning in adult ADHD: a meta-analytic review. Psychol Med 35(8):1097–1108. doi:10.1017/s003329170500499x
Boonstra AM, Kooij JJS, Buitelaar JK, Oosterlaan J, Sergeant JA, Heister JGAMA et al (2008) An exploratory study of the relationship between four candidate genes and neurocognitive performance in adult ADHD. Am J Med Genet B Neuropsychiatr Genet 147B(3):397–402. doi:10.1002/ajmg.b.30595
Bruder GE, Keilp JG, Xu HY, Shikhman M, Schori E, Gorman JM et al (2005) Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry 58(11):901–907. doi:10.1016/j.biopsych.2005.05.010
Caylak E (2012) Biochemical and genetic analyses of childhood attention deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 159B(6):613–627. doi:10.1002/ajmg.b.32077
Chen JS, Lipska BK, Halim N, Ma QD, Matsumoto M, Melhem S et al (2004) Functional analysis of genetic variation in catechol-O-methyltransferase (COMT): effects on mRNA, protein, and enzyme activity in postmortem human brain. Am J Hum Genet 75(5):807–821. doi:10.1086/425589
Conners CK, Erhardt D, Sparrow EP (1999) Conners’ Adult ADHD Rating Scales (CAARS). Multi-Health Systems, North Tonawanda
Corbisiero S, Buchli-Kammermann J, Stieglitz RD (2010) Reliability and validity of the Wender-Reimherr-Interview (WRI)—an instrument for the diagnostic of the ADHD in adulthood. Zeitschrift für Psychiatrie, Psychologie und Psychotherapie 58(4):323–331. doi:10.1024/1661-4747/a000043
Diaz-Asper CM, Goldberg TE, Kolachana BS, Straub RE, Egan MF, Weinberger DR (2008) Genetic variation in catechol-O-methyltransferase: effects on working memory in schizophrenic patients, their siblings, and healthy controls. Biol Psychiatry 63(1):72–79. doi:10.1016/j.biopsych.2007.03.031
Dickinson D, Elvevag B (2009) Genes, cognition and brain through a COMT lens. Neuroscience 164(1):72–87. doi:10.1016/j.neuroscience.2009.05.014
Durstewitz D, Seamans JK (2008) The dual-state theory of prefrontal cortex dopamine function with relevance to catechol-O-methyltransferase genotypes and schizophrenia. Biol Psychiatry 64(9):739–749. doi:10.1016/j.biopsych.2008.05.015
Egan MF, Goldberg TE, Kolachana BS, Callicott JH, Mazzanti CM, Straub RE et al (2001) Effect of COMT val(108/158) met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci USA 98(12):6917–6922. doi:10.1073/pnas.111134598
Goldberg TE, Egan MF, Gscheidle T, Coppola R, Weickert T, Kolachana BS et al (2003) Executive subprocesses in working memory—relationship to catechol-O-methyltransferase Val158Met genotype and schizophrenia. Arch Gen Psychiatry 60(9):889–896. doi:10.1001/archpsyc.60.9.889
Grace AA (1991) Phasic versus tonic dopamine release and the modulation of dopamine system responsivity—a hypothesis for the etiology of schizophrenia. Neuroscience 41(1):1–24. doi:10.1016/0306-4522(91)90196-U
Gschwendtner KM, Biehl SC, Mühlberger A, Sommer C, Kübler A, Reif A et al (2012) The relationship between valence, task difficulty, and the COMT val(158)met polymorphism in disengagement processes. J Psychophysiol 26(3):124–131. doi:10.1027/0269-8803/a000075
Hamilton M (1959) The assessment of anxiety-states by rating. Br J Med Psychol 32(1):50–55
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23(1):56–62. doi:10.1136/jnnp.23.1.56
Kebir O, Joober R (2011) Neuropsychological endophenotypes in attention-deficit/hyperactivity disorder: a review of genetic association studies. Eur Arch Psychiatry Clin Neurosci 261(8):583–594. doi:10.1007/s00406-011-0207-5
Kebir O, Tabbane K, Sengupta S, Joober R (2009) Candidate genes and neuropsychological phenotypes in children with ADHD: review of association studies. J Psychiatry Neurosci 34(2):88–101
Kessler RC, Adler L, Ames M, Delmer O, Faraone S, Hiripi E et al (2005) The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med 35(2):245–256. doi:10.1017/S0033291704002892
Kratzmeier H, Horn R (1988) Standard progressive matrices. Beltz Test Gesellschaft, Weinheim
Krause KH, Dresel SH, Krause J, Kung HF, Tatsch K (2000) Increased striatal dopamine transporter in adult patients with attention deficit hyperactivity disorder: effects of methylphenidate as measured by single photon emission computed tomography. Neurosci Lett 285(2):107–110. doi:10.1016/S0304-3940(00)01040-5
Krause KH, Dresel SH, Krause J, la Fougere C, Ackenheil M (2003) The dopamine transporter and neuroimaging in attention deficit hyperactivity disorder. Neurosci Biobehav Rev 27(7):605–613. doi:10.1016/j.neubiorev.2003.08.012
Lachman HM, Papolos DF, Saito T, Yu YM, Szumlanski CL, Weinshilboum RM (1996) Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics 6(3):243–250. doi:10.1097/00008571-199606000-00007
Levy F (2007) What do dopamine transporter and catechol-o-methyltransferase tell us about attention deficit-hyperactivity disorder? Pharmacogenomic implications. Aust N Z J Psychiatry 41(1):10–16. doi:10.1080/00048670601050432
Lewis DA, Sesack SR, Levey AI, Rosenberg DR (1997) Dopamine axons in primate prefrontal cortex: specificity of distribution, synaptic targets, and development. Adv Pharmacol 42:703–706
Lewis DA, Melchitzky DS, Sesack SR, Whitehead RE, Auh S, Sampson A (2001) Dopamine transporter immunoreactivity in monkey cerebral cortex: regional, laminar, and ultrastructural localization. J Comp Neurol 432(1):119–136. doi:10.1002/cne.1092
Lotta T, Vidgren J, Tilgmann C, Ulmanen I, Melen K, Julkunen I et al (1995) Kinetics of human soluble and membrane-bound catechol O-methyltransferase: a revised mechanism and description of the thermolabile variant of the enzyme. Biochemistry 34(13):4202–4210. doi:10.1021/bi00013a008
Martinussen R, Hayden J, Hogg-Johnson S, Tannock R (2005) A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 44(4):377–384. doi:10.1097/01.chi.0000153228.72591.73
Mattay VS, Goldberg TE, Fera F, Hariri AR, Tessitore A, Egan MF et al (2003) Catechol O-methyltransferase val(158)-met genotype and individual variation in the brain response to amphetamine. Proc Natl Acad Sci USA 100(10):6186–6191. doi:10.1073/pnas.0931309100
Matthews N, Vance A, Cummins TDR, Wagner J, Connolly A, Yamada J et al (2012) The COMT val158 allele is associated with impaired delayed-match-to-sample performance in ADHD. Behav Brain Funct 8:25. doi:10.1186/1744-9081-8-25
Meyer-Lindenberg A, Weinberger DR (2006) Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat Rev Neurosci 7(10):818–827. doi:10.1038/nrn1993
Mills S, Langley K, Van den Bree M, Street E, Turic D, Owen MJ et al (2004) No evidence of association between catechol-O-methyltransferase (COMT) val(158)met genotype and performance on neuropsychological tasks in children with ADHD: a case-control study. BMC Psychiatry 4:15. doi:10.1186/1471-244x-4-15
Palmatier MA, Kang AM, Kidd KK (1999) Global variation in the frequencies of functionally different catechol-O-methyltransferase alleles. Biol Psychiatry 46(4):557–567. doi:10.1016/s0006-3223(99)00098-0
Prescott P, Shahlaee R (1999) The analysis of ranked data in blocked factorial experiments. Metrika 50:37–54. doi:10.1007/s001840050034
Shirley EAC (1987) Applications of ranking methods of multiple comparison procedures and factorial experiments. Appl Stat, 205–213. doi:10.2307/2347552
Sonuga-Barke EJS (2005) Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry 57(11):1231–1238. doi:10.1016/j.biopsych.2004.09.008
Taerk E, Grizenko N, Amor LB, Lageix P, Mbekou V, Deguzman R et al (2004) Catechol-O-methyltransferase (COMT) val108/158 met polymorphism does not modulate executive function in children with ADHD. BMC Med Genet 5(1):30
Tunbridge EM, Bannerman DM, Sharp T, Harrison PJ (2004) Catechol-O-methyltransferase inhibition improves set-shifting performance and elevates stimulated dopamine release in the rat prefrontal cortex. J Neurosci 24(23):5331–5335. doi:10.1523/jneurosci.1124-04.2004
Ward MF, Wender PH, Reimherr FW (1993) The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry 150(6):885–890
Weinshilboum RM, Otterness DM, Szumlanski CL (1999) Methylation pharmacogenetics: catechol O-methyltransferase, thiopurine methyltransferase, and histamine N-methyltransferase. Ann Rev Pharmacol Toxicol 39:19–52. doi:10.1146/annurev.pharmtox.39.1.19
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF (2005) Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 57(11):1336–1346. doi:10.1016/j.biopsych.2005.02.006
Wittchen H-U, Zaudig M, Fydrich T (1997) SKID—Strukturiertes Klinisches Interview für DSM-IV. Hogrefe, Achse I und II. Göttingen
Acknowledgments
The authors wish to thank Inge Gröbner for coordinating the patient appointments. This work was supported by the Deutsche Forschungsgemeinschaft (DFG; Grants HE 4531/1-1 and RTG 1253/1).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
Ethical approval was obtained through the Ethical Review Board of the Medical Faculty of the University of Würzburg; all procedures involved were in accordance with the 2008 Declaration of Helsinki. Participants gave written informed consent after full explanation of procedures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biehl, S.C., Gschwendtner, K.M., Guhn, A. et al. Does adult ADHD interact with COMT val 158 met genotype to influence working memory performance?. ADHD Atten Def Hyp Disord 7, 19–25 (2015). https://doi.org/10.1007/s12402-014-0148-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-014-0148-8