Abstract
The present study aimed at identifying the full range of mental disorders comorbid to attention-deficit/hyperactivity disorder (ADHD) in children and adolescents (age 4–17) diagnosed in Danish psychiatric hospitals between 1995 and 2010. A total of 14,825 patients were included in the study and comorbid disorders diagnosed concurrent with ADHD were identified. Associations of comorbid disorders with sex, age, and other mental disorders were investigated by logistic regression analysis. In the total sample, 52.0 % of the patients had at least one psychiatric disorder comorbid to ADHD and 26.2 % had two or more comorbid disorders. The most frequent comorbid disorders were disorders of conduct (16.5 %), specific developmental disorders of language, learning and motor development (15.4 %), autism spectrum disorders (12.4 %), and intellectual disability (7.9 %). Male sex was generally associated with an increased risk for neuropsychiatric disorders while female sex was associated more frequently with internalizing disorders. The analysis of associations between the various comorbid disorders identified several clusters highlighting the differential developmental trajectories seen in patients with ADHD. The study provides evidence that comorbidity with mental disorders is developmentally sensitive. Furthermore, the study shows that particular attention should be given to patients with neurodevelopmental disorders such as autism and intellectual disability in future longitudinal analyses. These disorders are very frequent in patients with ADHD, and the affected patients might follow a different course than patients without these disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both epidemiological and clinical studies have found that non-comorbid attention-deficit/hyperactivity disorder (ADHD) occurs in only 13–32.3 % of cases, and that most patients with ADHD have multiple comorbid disorders (Ghanizadeh 2009; Larson et al. 2011; Kraut et al. 2013; Kadesjo and Gillberg 2001). Although the concept of comorbidity is often used in both research and in everyday practice, there is considerable diversity both in the use and the definition of the construct. Comorbidity can refer to both the co-occurrence of disorders temporally separate from ADHD (sequential comorbidity) or can be defined as temporally concurrent with ADHD (concurrent comorbidity). The time span of co-occurrence of ADHD and other disorders also varies with some studies investigating lifespan prevalence rates of disorders, whereas others assess past year prevalence rates or past three-month prevalence rates, etc. (Angold et al. 1999; Pliszka 2000; Taurines et al. 2010).
Among the most frequently observed comorbidities in children and adolescents with ADHD are conduct disorders and oppositional defiant disorder, which across a wide range of studies from both clinical and epidemiological settings and age ranges, are seen in some 4–60 % of children and adolescents with ADHD (Bauermeister et al. 2007; Elia et al. 2009; Freitag et al. 2012; Ghanizadeh 2009; Jensen et al. 1997; Kraut et al. 2013; Kadesjo and Gillberg 2001; Larson et al. 2011; Levy et al. 2005; Wichstrom et al. 2012). The second most frequently studied group of comorbidities in ADHD deals with the coexistence with anxiety disorders and affective disorders. Various reviews report an average 25 % coexistence rate between anxiety disorders and ADHD with prevalence rates ranging from 10 to 35 % (Spencer 2006; Taurines et al. 2010; Pliszka 2000). According to these reviews, affective disorders are found in 15–75 and 10–40 % of patients with ADHD, respectively (Spencer 2006; Pliszka 2000). In various studies, the prevalence rates of bipolar disorders comorbid with ADHD ranged quite substantially from 0 to 20 %, which may be partly due to differences in epidemiological and clinical populations and partly due to differences in the criteria for bipolar disorder and the diagnostic culture (Taurines et al. 2010).
Comorbid developmental disorders of learning have been studied less frequently and have been found to coexist in 10–92 % of patients with ADHD (August and Garfinkel 1990; Germano et al. 2010; Kadesjo and Gillberg 2001; Spencer 2006; Larson et al. 2011; Willcutt et al. 2000). The rates of intellectual disability have been reported less frequently in ADHD samples with ranges from 4 to 13 % (Faber et al. 2010; Kadesjo and Gillberg 2001; Kraut et al. 2013). Only a few studies have addressed the prevalence of comorbid autism spectrum disorder and reports range from 5 to 52 % (Larson et al. 2011; Smalley et al. 2007).
Many patients with ADHD also show language impairments (Bellani et al. 2011) with one study reporting a prevalence of 11.8 % (Bellani et al. 2011; Larson et al. 2011). Tic disorders comorbid with ADHD have also been investigated less frequently with one review reporting prevalence rates between 20 and 30 % (Taurines et al. 2010), but some studies find even lower prevalence rates in the 6–14 % range (Ghanizadeh 2009; Smalley et al. 2007).
The emergence of personality disorders and substance abuse problems is less relevant to the study of comorbidity in ADHD in children, but crucial for late adolescence on the brink of early adulthood. Patients with ADHD are considered to experience an elevated risk of antisocial and borderline personality disorders often associated with persistent ADHD, preceding conduct disorder, and a frequent co-occurrence with substance use disorders (Biederman et al. 2006; Costello et al. 1999; Miller et al. 2008; Taurines et al. 2010). Substance use disorders are co-occurring in up to 25–50 % of adolescents with ADHD (Taurines et al. 2010).
Although there is an abundance of studies on ADHD and comorbidity reporting quite divergent findings, studies with large samples, studies of girls and studies investigating associations among the various comorbid disorders are sparse. There is a lack of studies reporting the whole spectrum of disorders comorbid to ADHD and studies often overlook or even exclude patients with common disorders such as pervasive developmental disorders or intellectual disability. Furthermore, knowledge about patterns of comorbidity in patients identified by ICD-10 criteria is limited, although the ICD-10 classification is the most widely used diagnostic system worldwide (Mezzich 2002).
The diverse use of the construct of comorbidity and the above-mentioned limitations of the existing literature may distort clinicians’ expectations as to how many children and adolescents visiting the clinics with ADHD will experience additional psychopathology. It is important to clearly delineate which disorders were preceding, which are concurrent, and which are consequent to ADHD, and to know which psychiatric disorders are clustering in which individuals.
The objectives of the present study are (1) to study the entire spectrum of concurrent mental comorbidities diagnosed according to ICD-10 criteria in a large cohort of newly diagnosed patients with ADHD, (2) the identification of potential differences by sex and age at onset in this pattern of comorbidities, and (3) the study of the associations among these various comorbid disorders.
Methods
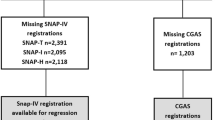
Although the terms hyperkinetic disorder (HD) and ADHD are not fully exchangeable, the term ADHD will be used predominantly in this article given the fact that the wider construct of ADHD includes all HD patients. In the present study, all first time diagnosed children and adolescents (age 4–18) with HD (F90-F90.9) diagnosed using ICD-10 criteria in the time period 1995–2010 in Danish psychiatric inpatient or outpatient clinics were identified from the Danish Psychiatric Central Research Registry (DPCRR) (Mors et al. 2011). In Danish child and adolescent psychiatry, children and adolescents are seen several times before a diagnosis is made. They are assessed in a multidisciplinary setting by psychiatrists and psychologists with special training in child and adolescent psychiatry. Most children are both seen for psychological assessment (general intelligence testing and testing for specific neuropsychological strengths and difficulties) and somatic assessment and when indicated observed in their natural environments. A multi-informant procedure is used and often both parents and teachers are asked to provide information on the everyday behavior and functioning of the child.
In the present study, concurrent comorbidity was defined as disorders registered within a three-month period before and after the date of the contact that led to the first time diagnosis of ADHD. The disorders investigated in the present study can be seen from Box 1. The restrictive definition of comorbidity in the present study was chosen to study those disorders that children and adolescents present with at close temporal proximity to their first contact in clinical practice relating to ADHD. Wider definitions of comorbidity might have inflated the results.
Danish studies of registries have a long-standing tradition and reputation in psychiatric epidemiological research because the data is close to complete since the registries are formed for administrative purposes (Munk-Jorgensen and Ostergaard 2011). Data from the DPCR provides good coverage of the patient population since the access to assessment and intervention in Denmark is free and available in all regions of Denmark.
Statistical analysis
In addition to the calculation of descriptive statistics, Mann–Whitney U-tests, independent t-tests, and Chi square tests were used to analyze data. To measure age at onset of comorbid disorders more precisely, it was defined as the age at which the disorder was diagnosed for the first time even if the first time registration was outside the 3-month-time window used to define concurrent comorbidity. Logistic regression models were used to estimate the risk associated with sex for a given comorbid disorder and both crude and age-adjusted models were specified. Logistic regression models were also used to identify associations among various comorbidities within the ADHD population. The results of the logistic regression analyses are presented as odds ratios (OR) with 95 % confidence intervals (95 % CI). Associations among comorbid disorders were investigated for disorders with a prevalence rate of 5 % or more in the ADHD sample. Covariates included in these models were disorders with a prevalence of at least 2 % within in the groups with the comorbidity in order to ensure sufficient sample size. In addition, these models were also controlled for age. Separate analyses for the two sexes were carried out to allow for the investigation of potential sex differences in the patterns of associations. The SPSS 19th version was used for the analyses (IBM Corp., 2010), and Stata 11th edition (StataCorp., 2009) was used for the production of figures. Non-corrected, two-tailed hypothesis testing was carried out with the alpha level set to 0.05.
Results
Sex and age distributions
A total of 14, 825 patients in the time period from 1995 to 2010 were diagnosed for the first time with ADHD in the age range of 4–17 years. The sex distribution was 79.4 % males vs. 20.6 % females (χ2 = 5118.5, df = 1; p ≥ 0.01). Males were significantly younger than females at the first time of ADHD diagnosis (Mean = 9.6, SD = 3.4 vs. Mean = 10.7, SD = 3.9 years; t = −15.0, df = 14.823, p > 0.01). When looking at the subcategories of the ICD-10 classification in the total population, 70.1 % were diagnosed with disturbance of activity and attention (F90.0), 12.5 % with hyperkinetic conduct disorder (F90.1), 1.1 % with other hyperkinetic disorders (F90.8), and 16.5 % with hyperkinetic disorder, unspecified (F90.9).
Frequencies of comorbidities
In the sample, 48.0 % had none of the investigated comorbidities, 52 % had at least one comorbid disorder, and 26.2 % had two or more disorders. The distribution of comorbid disorders in the total sample and the two sexes can be seen in Table 1 and Fig. 1. The most prevalent comorbid disorders were conduct disorders (16.5 %), specific developmental disorders of language, learning and motor skills (15.4 %), autism spectrum disorder (12.4 %), and intellectual disability (7.9 %).
Effects of age and sex on prevalence of comorbidities
The median age at onset for the various comorbid disorders is shown in Table 1 and Fig. 2. Elimination disorders, autism spectrum disorder, intellectual disability, and attachment disorders were among the disorders diagnosed in early childhood, whereas other disorders including anxiety disorders, reactions to stress, conduct disorder, tics, and the specific disorders of development manifested only in late childhood or early adolescence. A third group of disorders including substance use disorders, psychotic disorders, affective disorders, and personality disorders occurred only in later adolescence. Significant differences in age at onset of the disorders were found between the two sexes, and females were generally diagnosed later than males. Males had a 1- to 2-fold higher risk than females for specific disorders of development, autism spectrum disorder, conduct disorder, and tic disorders, and females were at increased risk for a range of disorders. However, after controlling for age, some of these findings disappeared. The results showed that females were at increased risk for comorbid affective disorders, anxiety disorders, reactions to severe stress, and eating disorders, whereas males were at a particular risk for comorbid autism spectrum disorder, conduct disorder, tic disorders, and specific disorders of development (Table 1).
Median age and interquartile range (IQR) at first time diagnosis of disorders comorbid with ADHD by sex. AFF affective disorder, ANX anxiety disorder, ASD autism spectrum disorder, ATTACH attachment disorder, BD bipolar disorder, CD conduct disorder, DEP depression, DisDev disorder of language, learning and motor development, EAT eating disorder, ELIM elimination disorders, ID intellectual disability, LANG specific developmental disorders of language, LEARN specific developmental disorders of learning, MIXED mixed specific developmental disorders, MOTOR specific developmental disorders of motor function, OCD obsessive–compulsive disorder, PD personality disorder, SUD substance use disorder, SZ schizophrenia/psychosis, RS severe reactions to stress, TIC tic disorder
Associations (OR with 95 % CI) between ADHD/CD, ADHD/ASD, ADHD/ID, ADHD/DevDis ADHD/TIC, ADHD/RS, and ADHD/ATTACH and other comorbid disorders for males and females. AFF affective disorder, ASD autism spectrum disorder, ATTACH attachment disorder, CD conduct disorder, DisDev disorder of language, learning and motor development, ELIM elimination disorder, ID Intellectual disability, OCD obsessive–compulsive disorder, PD personality disorder, SUD substance use disorder, SZ schizophrenia/psychosis, RS severe reactions to stress, TIC tic disorder
Associations among comorbid disorders
Table 2 and Fig. 3 presents the significant associations between the major types of comorbidity. ADHD/conduct disorder was uniquely associated with substance use disorders and had significant associations with attachment disorders and elimination disorders in both sexes. Having an autism spectrum disorder was negatively associated with ADHD/conduct disorder in both sexes, in males specific disorders of development were positively associated with ADHD/conduct disorder and intellectual disability was weakly negatively associated with ADHD/conduct disorder in males.
In both sexes, patients with intellectual disability and tic disorders had higher risk of ADHD/autism spectrum disorder. Furthermore, in males a significant association between ADHD/autism spectrum disorder and elimination disorders was identified. Negative association between ADHD/autism spectrum disorder and conduct disorder and attachment disorders were found in both sexes.
The risk of having ADHD/disorders of language, learning and motor development was associated with comorbid attachment disorders and tic disorder in both sexes, with reactions to severe stress, conduct disorder and elimination disorders in males, and was associated with affective disorders in females. Patients with autism spectrum disorder and attachment disorders had an increased risk of having comorbid ADHD/intellectual disability. In males, there was a negative association between conduct disorder and ADHD/intellectual disability.
The association of ADHD/tic disorder was only analyzed for males because the frequencies were too low for females. The analyses showed that obsessive compulsive disorder, specific disorders of development, and autism spectrum disorder were associated with ADHD and tic disorder. In females, ADHD/reaction to severe stress was associated with having comorbid psychotic disorders, affective disorders, and personality disorders. Associations between ADHD/attachment disorders and intellectual disability, disorders of language, learning and motor development, and conduct disorders were identified in females.
Discussion
In the present study, we analyzed the overall pattern of comorbid mental disorders in a nationwide large sample of patients diagnosed with hyperkinetic disorders according to ICD-10 criteria over a sixteen-year period. Approximately 50 % of the sample had at least one comorbid disorder and the prevalence of patients with more than one comorbid disorder was around 25 %. This overall rate is lower than in many studies, and a range of factors might have led to this finding. Before discussing the findings in more detail, a few general considerations regarding the relevance and interpretation of the present study shall be made.
Research on ADHD and comorbidity is often based on results from rather small samples studied with highly structured assessments; a clear definition of exclusion criteria and the assessment of impaired functioning are often ignored. In contrast, the present register-based study reflects the assessments in daily clinical routine work with disorders only diagnosed if they are the primary reason for the patient’s mental problems and if they are associated with impairments. By definition, the present study contained only individuals with both mental problems and impairment present because otherwise they would not have passed first-line assessments by pediatricians and general practitioners before being referred to public mental health services.
In addition, the age of the sample under investigation is relevant because various comorbid disorders might not yet have developed at first time diagnosis of ADHD as pointed out in the recent review on developmental comorbidity in ADHD (Taurines et al. 2010). Furthermore, the present study used only a 6-month window for registering comorbid disorders. Thus, prevalence rates of comorbid disorders are expected to be lower than in studies investigating larger time spans. Furthermore, the focus of the study on all major comorbid mental disorders and the lack of exclusion of any patients with intellectual disability or autism spectrum disorder might have made findings less comparable to previous studies which mostly exclude these patients.
Finally, clinical practice is less prone to cover, according to Rutter, “absurdly large number of diagnostic categories” listed in the contemporaneous classification systems which “… has resulted in an equally ridiculous, very high rate of co-occurrence of conditions misleadingly labeled as ‘comorbidity’, because much of the supposed comorbidity is artifactual” (Rutter 2011). Thus, the findings based on the present clinical data set may have been not only more conservative but also more representative than previous studies. However, it may not be fully dismissed that under-recognition of comorbid disorders in the patients did occur. The assessments of patients with ADHD in everyday clinical practice only rarely include the use of a fully structured diagnostic interview which could have identified psychiatric disorders not otherwise noticed by the clinician.
Prevalence and the effect of sex
In accordance with the findings of the literature, the most frequently observed comorbid mental disorder in the present study was conduct disorder/oppositional defiant disorder, which occurred in 16.5 % of the sample. Of these, 12.5 % were diagnosed with hyperkinetic conduct disorder and the rest received both the diagnosis of hyperkinetic disorder and the registration of either ICD-10 F91 (Conduct disorder) or F92 (Mixed disorders of conduct and emotion) within the specified observation period. These results are somewhat comparable to a series of studies with prevalence rates of comorbid conduct disorder ranging between 9.9 and 19.0 % (Bauermeister et al. 2007; Ghanizadeh 2009; Kraut et al. 2013; Levy et al. 2005; Wichstrom et al. 2012) and the 13.9 % prevalence rate of comorbid conduct disorder at baseline in the multimodal treatment study of ADHD (MTA) where the patients had a similar mean age as in the current study (1999). Similar to findings from both community-based (Costello et al. 2003) and patient population studies (Kraut et al. 2013; Levy et al. 2005), males had an increased risk for comorbid conduct disorder. It is unclear whether this is a true sex difference or caused by a male bias in the diagnostic criteria for conduct disorder since females compared to males are less likely to engage in aggressive and rule breaking behavior, but more likely to express relational aggression (Abikoff et al. 2002; Hinshaw 2002).
The second most frequently observed comorbid mental disorders in the present study were the specific disorders of development such as disorders of language, learning and motor development with a prevalence rate of 15.4 %. This diagnostic group represents a composite category with most patients having the mixed category of the specific developmental disorders. The group of mixed disorders can be compared to the literature on both comorbid disorders of learning and speech and language disorders with some caution. Reading disorders are expected to exist in 18–40 % of the patients with ADHD (Germano et al. 2010) and disorders of language development have been found to coexist with ADHD in 11.8 % of the patients (Larson et al. 2011). Thus, the prevalence rates of these disorders in the present study are lower than in previous studies. In ordinary clinical practice, clinicians might be reluctant to diagnose the specific developmental disorders before ADHD symptoms have been sufficiently treated, leading to the low prevalence in the present study. Furthermore, in Denmark the assessment of these disorders are often conducted by school psychologist and speech and language professionals rather than in child and adolescent psychiatry. In accordance with the literature on speech and language impairments and learning disabilities, the study also identified an increased risk for males for the specific disorders of development (Germano et al. 2010).
Contrary to the findings from other studies, autism spectrum disorders were the third most prevalent comorbid disorder in the present sample with a prevalence of 12.4 %. This finding adds to more recent studies of comorbidity documenting the coexistence of autism spectrum disorder and ADHD with a wide prevalence findings ranging between 2 and 52 % (Faber et al. 2010; Kraut et al. 2013; Larson et al. 2011; Smalley et al. 2007). These results clearly indicate that clinicians have abandoned the exclusion criterion of ADHD in autism spectrum disorder as set out in the ICD-10 guidelines for diagnosis. The exclusion criterion of autism spectrum disorder for the diagnosis of ADHD is now formally abandoned in the DSM-5 criteria for ADHD. In addition to autism spectrum disorder, the present study also documented a high rate of 7.9 % comorbid intellectual disability in patients with ADHD which is in line with findings from other studies including a prevalence rate of intellectual disability of 3–5 % in methylphenidate-treated children and adolescents in Germany (Kraut et al. 2013) and a prevalence rate of intellectual disability at 13 % in an epidemiological study of Swedish school-aged children (Kadesjo and Gillberg 2001). As expected, both intellectual disability and autism spectrum disorder were diagnosed early in life and, in accordance with the literature; the present study also found that males compared to females were at an increased risk for having autism spectrum disorder and intellectual disability (Newschaffer et al. 2007; Roeleveld et al. 1997).
Although anxiety disorders and affective disorders were among the most prevalent comorbid disorders in patients with ADHD in previous studies, the prevalence rates of 1.3 % for anxiety disorders and of 2.0 % for affective disorders in the present study were rather low. These low rates may be related both to diagnostic traditions in clinical practice and the narrow temporal definition of comorbidity. Anxious and depressive symptoms in children and adolescents with ADHD and the accompanying psychosocial impairment are often regarded by clinicians as a reaction to stressful life conditions and, thus, are often coded as a reaction to stress rather than an anxiety or affective disorder. Furthermore, the developmental context of comorbidity may help to explain the low rates. In accordance with the literature, the age at onset of the two groups of disorders most frequently was in adolescence (Costello et al. 2003) and the present sample only contained few patients diagnosed with ADHD at this age.
The 4.8 % prevalence rate of tic disorders in the present study is lower than the most frequently reported rates ranging between 20 and 30 % in previous studies (Spencer 2006; Taurines et al. 2010). Besides subject selection biases in other studies, the reason for the relatively low rate of tics in the present study might again be due to the narrow definition of comorbidity, since tics are considered to have their onset frequently only after the occurrence of ADHD (Pliszka 2000; Taurines et al. 2010). Furthermore, the study replicated findings from the literature suggesting that males are at increased risk of developing tic disorders (Freeman 2007).
As expected, the prevalence rates of substance use disorder and personality disorders were low due to the young age of the sample. There was no significant sex effect in the prevalence rates of comorbid substance use disorders in this sample after controlling for age. However, because the disorders were very rare in this large sample and because patients were in general still very young, firm conclusions must be established in studies based on older cohorts of patients with ADHD.
The findings of low rates of schizophrenia/psychosis and eating disorders in the sample confirms earlier findings (Kraut et al. 2013) and suggest that at least at this age, rates of the disorders do not exceed the rates that may be observed in the general population (Gillberg et al. 1986; Hoek and van Hoeken 2003). The prevalence rate of elimination disorders were lower than expected from the review of preceding studies of enuresis in patients with ADHD (Taurines et al. 2010). It may well be that elimination disorders had been diagnosed mainly by other health care professionals outside psychiatry such as pediatricians. Furthermore, a large part of the sample might have had outgrown elimination disorders at the time of assessment of ADHD.
Associations among comorbid disorders
An aim of the study was the investigation of the associations among the various comorbid disorders. The present study found a unique association of ADHD/conduct disorder with substance use disorders in both sexes. This finding is in line with expectations since conduct problems are well-known risk factors for substance abuse (Barkley et al. 2004; Biederman et al. 2006; Elkins et al. 2007). Due to the focus of the present study on a wide variety of comorbid disorders, the strength of this association between ADHD/conduct disorder and substance use disorder was further amplified by proving that no other comorbid disorder was positively associated with substance use disorder.
The findings that attachment disorders were associated with ADHD/conduct disorder in both sexes is in accordance with existing knowledge that attachment disorders emerge early in life (Zeanah and Smyke 2009) and are associated with social and relational adversities which in turn are well-known risk factors for the development of antisocial behaviors (Boden et al. 2010; Biederman et al. 2008) although the present study cannot make conclusions about causality. Furthermore, elimination disorders were positively associated with ADHD/conduct disorder as found in previous studies (Ellington and McGuinness 2012; Ghanizadeh 2010).
There was a clear bidirectional association between autism spectrum disorder and intellectual disability in this sample of ADHD patients replicating the findings of a previous study (Campbell and Malone 1991). Furthermore and in line with findings from the literature (Simonoff et al. 2008), ADHD/autism spectrum disorder was associated with tic disorders. ADHD/intellectual disability but not ADHD/autism spectrum disorder was associated with an increased risk for attachment disorders. Although some studies have found less secure attachment behaviors in children with autism spectrum disorder and intellectual disability (van Ijzendoorn et al. 2007; Rutgers et al. 2007), attachment disorders were not associated with autism spectrum disorder in the current study. This finding was most probably due to the fact that attachment disorders serve as an exclusion criterion for autism spectrum disorder in ICD-10 and because the lack of age appropriate social and interpersonal reciprocity are core symptoms in autism spectrum disorder.
Most of the associations of comorbid disorders with ADHD/disorders of language, learning and motor development were rather sex-specific but proved that the specific developmental disorders were associated with specifically the disorders characterized by emotional problems. The present study found that the association among ADHD, autism spectrum disorder, and tics is bidirectional. Furthermore, ADHD/tic disorder was strongly related to obsessive compulsive disorder and with anxiety disorders. This finding replicates the strong relation between tics/Tourette syndrome with obsessive compulsive disorder found in a previous study (Freeman 2007).
In females with ADHD/reactions to severe stress, significant associations with schizophrenia/psychosis, affective disorders, and personality disorders were found. These associations may reflect either stressful life events and subjective stress inherent to these disorders, or the rather limited clinical specificity of reactions to severe stress as a diagnostic category. In females, the reciprocal relationship between attachment disorders, intellectual disability, and conduct disorder was also established.
The present results based on multiple comorbid associations with ADHD at first time diagnosis allow the delineation of various potential developmental trajectories and risks. In general, any developmental disorder increased the risk of co-occurring of other developmental disorders. Both for intellectual disability and autism spectrum disorder, a negative relationship was found with conduct disorder in ADHD cases. ADHD/disorders of language, learning and motor development was associated with internalizing disorders and tics. Both ADHD/conduct disorder and ADHD/intellectual disability were associated with attachment disorders, but ADHD/CD showed a unique relation with substance use disorders, and ADHD/intellectual disability had a unique relation with autism spectrum disorder. While the ADHD/Conduct disorder and ADHD/intellectual disability subgroups had the risk of attachment disorders in common, the two groups might follow different trajectories because ADHD/conduct disorder and ADHD/intellectual disability were negatively associated with each other. Finally, tic disorders were associated with disorders of development highlighting the fact that neurodevelopmental disorders are highly frequent in patients with tics.
Strengths and limitations
The present study has a number of strengths including the large, nationwide, and representative sample of both males and females, and the wide focus on all clinically relevant disorders coexisting with ADHD. Furthermore, the present study had a strong focus on how the range of comorbid mental disorders relate to each other leading to clusters within the heterogenic group of patients with ADHD. However, some limitations also apply to the present study. First, the study is limited by the fact that the data came from registries. Although the validity of the DPCR data has been documented for childhood autism (Lauritsen et al. 2010), schizophrenia (Loffler et al. 1994), and affective disorders (Kessing 1998), data on patients with ADHD has not been validated yet.
However, it should be kept in mind that the diagnosis of ADHD in Danish psychiatric institutions is performed by trained and experienced child and adolescent psychiatrists and psychologists. Assessments of ADHD are thorough and include both somatic and psychological assessments, patients are seen several times and multiple informants are included before a diagnosis is made. Preliminary findings from an ongoing validation study of childhood and adolescent ADHD cases in the DPCR by the authors so far supports the notion that ADHD diagnoses in the DPCR are valid. As mentioned above, the assessments do, however, rarely include the use of standardized diagnostic interviews. Thus, there might occur under-reporting of the less severe and not very visible disabilities at the first assessments of the patients. Another limitation of the study might stem from a referral bias with the most severely affected patients with ADHD sent to child and adolescent psychiatric services, so that the findings may not generalize fully to non-referred patients with ADHD in the community and to patients seen in private mental health care facilities or by pediatricians, general practitioners, and neurologists only.
Conclusions
Despite the limitations, the findings of the present study are important in various ways. They document comorbidity rates of mental disorders in children and adolescents with ADHD using ICD-10 criteria, they provide more knowledge about age and sex effects on the rates of comorbidity in patients with ADHD and they point to the clustering of comorbid disorders in patients with ADHD. The current study highlights that comorbidity in ADHD is both dynamic and developmental. Risk patterns associated with sex and comorbidity at first time diagnosis of ADHD might also be early risk markers of later developmental trajectories thus making comorbidity an important area of assessment. The differential validity of these emerging developmental trajectories in ADHD as early phenotypic markers may be confirmed by long-term outcome studies. Furthermore, since the study identified very low rates of disorders otherwise thought to be highly prevalent among children and adolescents with ADHD, such as affective disorders, learning, and language disabilities, it might be worthwhile for clinicians to consider whether under-recognition of certain comorbid disorders is occurring in order to secure that patients receive the best possible intervention.
References
A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal treatment study of children with ADHD (1999). Arch Gen Psychiatry 56:1073–1086
Abikoff HB, Jensen PS, Arnold LL, Hoza B, Hechtman L, Pollack S et al (2002) Observed classroom behaviour of children with ADHD: relationship to gender and comorbidity. J Abnorm Child Psychol 30:349–359
Angold A, Costello EJ, Erkanli A (1999) Comorbidity. J Child Psychol Psychiatry 40:57–87
August GJ, Garfinkel BD (1990) Comorbidity of ADHD and reading disability among clinic-referred children. J Abnorm Child Psychol 18:29–45
Barkley RA, Fischer M, Smallish L, Fletcher K (2004) Young adult follow-up of hyperactive children: antisocial activities and drug use. J Child Psychol Psychiatry 45:195–211
Bauermeister JJ, Shrout PE, Ramirez R, Bravo M, Alegria M, Martinez-Taboas A et al (2007) ADHD correlates, comorbidity, and impairment in community and treated samples of children and adolescents. J Abnorm Child Psychol 35:883–898
Bellani M, Moretti A, Perlini C, Brambilla P (2011) Language disturbances in ADHD. Epidemiol Psychiatr Sci 20:311–315
Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM et al (2006) Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med 36:167–179
Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC et al (2008) The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med 38:1027–1036
Boden JM, Fergusson DM, Horwood LJ (2010) Risk factors for conduct disorder and oppositional/defiant disorder: evidence from a New Zealand birth cohort. J Am Acad Child Adolesc Psychiatry 49:1125–1133
Campbell M, Malone RP (1991) Mental retardation and psychiatric disorders. Hosp Community Psychiatry 42:374–379
Costello EJ, Erkanli A, Federman E, Angold A (1999) Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. J Clin Child Psychol 28:298–311
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60:837–844
Elia J, Arcos-Burgos M, Bolton KL, Ambrosini PJ, Berrettini W, Muenke M (2009) ADHD latent class clusters: DSM-IV subtypes and comorbidity. Psychiatry Res 170:192–198
Elkins IJ, McGue M, Iacono WG (2007) Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry 64:1145–1152
Ellington EE, McGuinness TM (2012) Mental health considerations in pediatric enuresis. J Psychosoc Nurs Ment Health Serv 50:40–45
Faber A, Kalverdijk LJ, de Jong-van den Berg LT, Hugtenburg JG, Minderaa RB, Tobi H (2010) Co-morbidity and patterns of care in stimulant-treated children with ADHD in the Netherlands. Eur Child Adolesc Psychiatry 19:159–166
Freeman RD (2007) Tic disorders and ADHD: answers from a world-wide clinical dataset on Tourette syndrome. Eur Child Adolesc Psychiatry 16(Suppl 1):15–23
Freitag CM, Hanig S, Schneider A, Seitz C, Palmason H, Retz W et al (2012) Biological and psychosocial environmental risk factors influence symptom severity and psychiatric comorbidity in children with ADHD. J Neural Transm 119:81–94
Germano E, Gagliano A, Curatolo P (2010) Comorbidity of ADHD and dyslexia. Dev Neuropsychol 35:475–493
Ghanizadeh A (2009) Psychiatric comorbidity differences in clinic-referred children and adolescents with ADHD according to the subtypes and gender. J Child Neurol 24:679–684
Ghanizadeh A (2010) Comorbidity of enuresis in children with attention-deficit/hyperactivity disorder. J Atten Disord 13:464–467
Gillberg C, Wahlstrom J, Forsman A, Hellgren L, Gillberg IC (1986) Teenage psychoses–epidemiology, classification and reduced optimality in the pre-, peri- and neonatal periods. J Child Psychol Psychiatr 27:87–98
Hinshaw SP (2002) Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. J Consult Clin Psychol 70:1086–1098
Hoek HW, van Hoeken D (2003) Review of the prevalence and incidence of eating disorders. Int J Eat Disord 34:383–396
IBM Corp (2010) IBM SPSS statistics for windows. (Version 19.0) [Computer software]. Armonk, NY
Jensen PS, Martin D, Cantwell DP (1997) Comorbidity in ADHD: implications for research, practice, and DSM-V. J Am Acad Child Adolesc Psychiatry 36:1065–1079
Kadesjo B, Gillberg C (2001) The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatr 42:487–492
Kessing L (1998) Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry 13:392–398
Kraut AA, Langner I, Lindemann C, Banaschewski T, Petermann U, Petermann F et al (2013) Comorbidities in ADHD children treated with methylphenidate: a database study. BMC Psychiatry 13:11
Larson K, Russ SA, Kahn RS, Halfon N (2011) Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics 127:462–470
Lauritsen MB, Jorgensen M, Madsen KM, Lemcke S, Toft S, Grove J et al (2010) Validity of childhood autism in the Danish Psychiatric Central Register: findings from a cohort sample born 1990–1999. J Autism Dev Disord 40:139–148
Levy F, Hay DA, Bennett KS, McStephen M (2005) Gender differences in ADHD subtype comorbidity. J Am Acad Child Adolesc Psychiatry 44:368–376
Loffler W, Hafner H, Fatkenheuer B, Maurer K, Riecher-Rossler A, Lutzhoft J et al (1994) Validation of Danish case register diagnosis for schizophrenia. Acta Psychiatr Scand 90:196–203
Mezzich JE (2002) International surveys on the use of ICD-10 and related diagnostic systems. Psychopathology 35:72–75
Miller CJ, Flory JD, Miller SR, Harty SC, Newcorn JH, Halperin JM (2008) Childhood attention-deficit/hyperactivity disorder and the emergence of personality disorders in adolescence: a prospective follow-up study. J Clin Psychiatry 69:1477–1484
Mors O, Perto GP, Mortensen PB (2011) The Danish Psychiatric Central Research Register. Scand J Public Health 39:54–57
Munk-Jorgensen P, Ostergaard SD (2011) Register-based studies of mental disorders. Scand J Public Health 39:170–174
Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE et al (2007) The epidemiology of autism spectrum disorders. Annu Rev Public Health 28:235–258
Pliszka SR (2000) Patterns of psychiatric comorbidity with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am 9:525–540, vii
Roeleveld N, Zielhuis GA, Gabreels F (1997) The prevalence of mental retardation: a critical review of recent literature. Dev Med Child Neurol 39:125–132
Rutgers AH, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Swinkels SH et al (2007) Autism, attachment and parenting: a comparison of children with autism spectrum disorder, mental retardation, language disorder, and non-clinical children. J Abnorm Child Psychol 35:859–870
Rutter M (2011) Response: growing consensus on classification needs. J Child Psychol Psychiatry 52(6):673–675
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G (2008) Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 47:921–929
Smalley SL, McGough JJ, Moilanen IK, Loo SK, Taanila A, Ebeling H et al (2007) Prevalence and psychiatric comorbidity of attention-deficit/hyperactivity disorder in an adolescent Finnish population. J Am Acad Child Adolesc Psychiatry 46:1575–1583
Spencer TJ (2006) ADHD and comorbidity in childhood. J Clin Psychiatry 67(Suppl 8):27–31
StataCorp (2009) Stata statistical software: release 11. StataCorp LP, College Station, TX
Taurines R, Schmitt J, Renner T, Conner AC, Warnke A, Romanos M (2010) Developmental comorbidity in attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord 2:267–289
van Ijzendoorn MH, Rutgers AH, Bakermans-Kranenburg MJ, Swinkels SH et al (2007) Parental sensitivity and attachment in children with autism spectrum disorder: comparison with children with mental retardation, with language delays, and with typical development. Child Dev 78:597–608
Wichstrom L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH (2012) Prevalence of psychiatric disorders in preschoolers. J Child Psychol Psychiatry 53:695–705
Willcutt EG, Pennington BF, DeFries JC (2000) Twin study of the etiology of comorbidity between reading disability and attention-deficit/hyperactivity disorder. Am J Med Genet 96:293–301
Zeanah CH, Smyke AT (2009) Attachment Disorders. In: Zeanah CH (ed) Handbook of infant mental health, 3rd edn. Guilford Press, New York, pp 421–434
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jensen, C.M., Steinhausen, HC. Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. ADHD Atten Def Hyp Disord 7, 27–38 (2015). https://doi.org/10.1007/s12402-014-0142-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-014-0142-1