Abstract
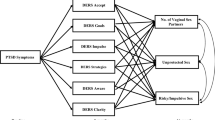
Previous research demonstrates that ADHD symptoms are related to increased risky sexual behavior. Distress intolerance (DIT) has also been linked to risk behavior and may also be related to increased risky sexual behavior. Thus, we evaluated the degree to which DIT moderated the link between ADHD symptoms and number of casual and monogamous sexual partners. Participants were undergraduate psychology students (N = 660; 30 % male; M = 20.23, SD = 1.40; 47 % European American) who completed an online assessment. Hierarchical multiple regression revealed that several DIT constructs, specifically tolerance, appraisal, and regulation, moderated the link between ADHD symptoms and casual sex partners. Only regulation moderated the association between ADHD symptoms and monogamous sex partners. Results suggest that difficulty managing distress moderates the link between ADHD symptoms and number of sexual partners. These results have important implications for prevention and intervention program development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
College matriculation may be associated with increased risky sexual activity. Number of sexual partners often increases when young adults transition from high school to college (Fromme et al. 2008). Although college students report an average of two new sexual partners per year, (Cooper 2002) almost 9 % of sexually active students report having four or more sexual partners within the last year (Buhi et al. 2010). The fact that only about 50 % of sexually active undergraduates report consistent condom use within the last month (American College Health Association 2013) amplifies the risk associated with having multiple sexual partners.
Unprotected sexual activity with multiple partners exposes students to sexually transmitted infections (STIs) and unintended pregnancy. Among the estimated 19 million new STI cases per year in the US, nearly half occur among youth ages 15–24 years (Centers for Disease Control and Prevention 2012). Rates of STIs among US college students range from 12 to 25 % with prevalence among women twice as high as among men (Patrick et al. 1997). STIs can be lifelong diagnoses and sometimes have serious medical repercussions, such as infertility, dementia, and cancer (Parkin and Bray 2006). Compared to other age groups, women between 18 and 24 experience two times the rate of unintentional pregnancy (5 vs. 10 %; Finer and Henshaw 2006), which more than doubles the risk of college dropout (Raley et al. 2012) reducing earning potential throughout one’s life span (Schneider and Yin 2011).
Risky sexual behaviors may also contribute to negative psychological outcomes. College students with low rates of depressive symptoms and loneliness often report significant increases in these symptoms after engaging in casual sex (Owen et al. 2011). Men and women who have ever engaged in casual sex report lower self-esteem than those who have not (Paul et al. 2000). Multiple casual sex partners may also increase the risk for sexual victimization; college students report that most of their unwanted sex experiences occurred in the context of a “hookup” (Flack et al. 2007). Further, over 7 % of a college sample indicated that their most recent casual sex encounter was unwanted or non-consensual (Lewis et al. 2011).
Multiple serial monogamous sexual partners (i.e., partners within the context of a romantic relationship) may also increase risk for negative outcomes. Number of monogamous sex partners is related to increased risk of both STIs and unintentional pregnancies (Ott et al. 2011). College students report decreased condom use with regular sexual partners as trust in their partner increases, which reduces perceptions of risk for negative outcomes (Pedra et al. 1999) However, this sense of safety is likely misplaced; in only 52 % of couples do both partners report agreeing to monogamy, and only 71 % of these couples remain monogamous (Warren et al. 2012). The fact that less than one-third of couples display fidelity highlights the significant exposure to risk partners experience when decreasing condom use in a monogamous relationship. Thus, we included number of monogamous sexual partners as an indicator of risky sex, alongside number of casual sexual partners.
These findings indicate that engagement in risky sex places college students at risk for adverse outcomes across health, educational, and psychological domains. Identifying factors that contribute to risky sex may contribute to developing effective prevention and intervention approaches to reducing these negative outcomes among college students.
ADHD symptoms and risky sexual behavior
ADHD symptoms contribute to other risky behaviors, such as substance use (Lee et al. 2011) and unsafe driving (Olazagasti et al. 2013), and may also increase engagement in risky sex. Several studies demonstrate that ADHD diagnosis in childhood predicts increased number of casual and lifetime sexual partners in young adulthood (Barkley et al. 2006; Flory et al. 2006b; Hosain et al. 2012; Ramrakha et al. 2007). However, several of these studies have not included the effects of conduct problems (CPs), which include symptoms of conduct disorder and/or antisocial personality disorder (Barkley et al. 2006; Hosain et al. 2012). CP interacted with ADHD symptoms to predict increased risky sex in some studies (Galéra et al. 2010). When CP are included as a covariate, ADHD and number of sexual partners appear related in some studies (Flory et al. 2006a, b) and are no longer related in other studies (Ramrakha et al. 2007). These studies support a link between ADHD symptoms and risky sex and demonstrate the lack of clarity that exists regarding the role of CP. Further, few, if any, studies have examined moderators other than CP that may elucidate the link between ADHD symptoms and risky sex.
Distress intolerance, ADHD symptoms, and risky sexual behavior
Distress intolerance (DIT) refers to the perception of tolerating the aversiveness of negative affect. Individuals with high DIT may experience negative affect as unbearable (tolerance), perceive themselves as less capable of managing distress than others (appraisal), find negative affect to be intense and all-encompassing (absorption), and report being willing to do anything to stop their distress (Simons and Gaher 2005) (regulation). DIT is conceptually and empirically related to negative urgency, (Anestis et al. 2012; Kaiser et al. 2012) a well-studied component of impulsivity (Whiteside and Lynam 2001). DIT is hypothesized to increase impulsiveness and risk behavior as an escape from distress. At one’s tolerance threshold for distress, an individual will indiscriminately engage in risk behavior to escape the aversiveness of negative affect. Thus, individuals with a lower threshold for distress experience greater vulnerability for engaging in risk behavior, including substance use and gambling (Buckner et al. 2007; Daughters et al. 2005), and potentially risky sex as well.
Distress intolerance (DIT) may significantly increase engagement in risk behavior for young adults with ADHD. Not only is DIT closely linked to impulsive behavior, a core feature of ADHD (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association 2000), extensive research demonstrates that ADHD symptoms are associated with difficulty managing negative emotionality, a construct similar to DIT. For instance, in a follow-up study, Barkley and Fischer (2010) found that young adults with persistent ADHD were more likely to display “emotional impulsivity,” defined as being more impatient, quick tempered, frustrated, and emotionally over reactive than controls. Several other studies demonstrate that adults with ADHD display increased impulsivity when distressed (Edel et al. 2010; Reimherr et al. 2010). In one study, negative emotionality mediated the link between ADHD symptoms and the urge to act impulsively when distressed (i.e., negative urgency) for young adult college students (Mitchell et al. 2012). Thus, DIT may be one pathway through which ADHD symptoms impact risky behavior, such as risky sex.
The current study
The current study examined the joint effects of ADHD symptoms, CP, and DIT on risky sexual behavior, represented by number of lifetime casual and monogamous sexual partners, within a large sample of college students. We hypothesized that both CP and DIT would moderate the relations between ADHD symptoms and number of sexual partners, such that students with high levels of ADHD symptoms and CP as well as high levels of ADHD symptoms and DIT would have the highest number of casual and monogamous lifetime partners.
Methods
Participants and procedures
Participants were college students (N = 660; 30 % male) between the ages of 18 and 25 years (M = 20.23, SD = 1.40) who enrolled in a psychology course at a public university in the South. Many students were in their first year in school (43 %). Nearly half (47 %) identified as European American, 12 % as African American, 3 % as Asian, and 3 % as Latino. About 4 % did not specify race/ethnicity, 31 % identified as multi-racial. Also, 14 % of participants had a childhood household income of <$40,000/year, compared to 48 % of participants with a childhood household income of >$100,000/year. About 41 % of the mothers of participants had completed at least some college coursework. Recruitment occurred through class announcements. Participants read a consent form approved by the university institutional review board before completing the online survey in May of 2011; students received extra credit as compensation.
Measures
ADHD symptoms
The current symptoms scale—self-report form (CSS) (Barkley et al. 2008) have 36 self-report items using a 4-point scale (0 = “never or rarely” to 3 = “very often”) and correspond to the DSM–IV–TR criteria for ADHD. Eighteen items asked about current symptoms, and 18 items assessed childhood symptoms. Validity concerns about retrospective self-report (Mannuzza 1993) led us to use only current symptoms. Items were summed for a total scale score, given the multicollinearity between inattention and hyperactivity (r = .78, p < .05). Reliability for this sample was strong (α = .92). Self-report scores correspond to parent and spousal report (r = 0.76), and research with a normative sample indicates that a CSS total score ≥27.8 is the clinical cutoff for ADHD for those 17–29 years old (Barkley et al. 2008). Among our participants, current and childhood ADHD symptoms were highly correlated (r = 0.63, p < 0.001), and rates of diagnosis were comparable with 8 % of participants reporting childhood ADHD symptoms above the clinical cutoff compared to 9.3 % for current symptoms, a rate of clinical symptoms that is comparable to prevalence rates of ADHD in other studies with college students (2–8 %) (DuPaul et al. 2009).
Conduct problems
The Self-Reported Delinquency Scale (SRD; Elliott et al. 1985) is an 18 item self-report survey that corresponds to CD diagnostic criteria in the DSM–IV–TR and provides assessment of antisocial personality disorder. Participants answered 1 “yes” or 0 “no” regarding engagement in each behavior in the past 6 months. Responses were summed for a total score of CP that ranged from 0 to 11. The SRD has been used in several large-scale studies (Lochman et al. 2010; Loeber et al. 1998) and corresponds to court records and parent and teacher report (Farrington et al. 1996).
Distress tolerance
The distress tolerance scale (DTS; Simons and Gaher 2005) is a 15-item self-report measure of one’s tolerance for experiencing emotional distress. Items have a 5-point response scale (1 = “disagree” to 5 = “agree”) with a few items reverse coded. The DTS includes a total score and four subscales—tolerance (3 items; “Feeling distressed or upset is unbearable to me.”), appraisal (5 items; “Other people seem to be able to tolerate feeling distressed or upset better than I can.”), Absorption (3 items; “My feelings of distress are so intense that they completely take over.”), and Regulation (5 items; “I’ll do anything to stop feeling distressed or upset.”). Tolerance refers to how aversive the experience of emotional distress is. Appraisal indicates how one evaluates one’s ability to cope with distress. Absorption represents the capacity to distract from distress. Regulation refers to impulsively engaging in activities to reduce emotional distress. Reliability for all scales was satisfactory (Total Score: α = .94, tolerance: α = .84, appraisal: α = .87, Absorption: α = .91, and Regulation: α = .84), and the measure displays strong construct and predictive validity (Simons and Gaher 2005). High scores on all DTS scales represent greater DIT.
Number of sexual partners
The Sexuality and Consequences (Bearman et al. 1997) measure, originally developed for the National Longitudinal Study of Adolescent Health Wave III (Bearman et al. 1997), was used to assess sexual behavior. In four open-ended items, participants were asked how many individuals had been their sexual partners within a monogamous relationship and within casual sexual encounters. Questions were asked separately regarding the number of same sex and opposite sex partners. We summed the number of reported same sex and opposite sex monogamous and casual partners to create two variables: total number of casual partners and total number of monogamous partners.
Analytic procedures
SPSS 19.0 was used to conduct hierarchical multiple regressions with ADHD symptoms, CP, and DIT scales, as well as the interaction of ADHD symptoms with DIT scales and CP. Independent models were used for CP and each DIT scale for a total of five separate models for each outcome. The two dependent variables were number of casual partners and number of monogamous partners. All independent variables were mean centered (Cohen et al. 2003). Covariates included sex (0 = “male,” 1 = “female”), household income during childhood, and race/ethnicity (0 = “European American (EA),” 1 = “non-EA”). CP was included as a covariate in models with DIT constructs.
Only 4.4 % of data were missing, which corresponded to 29 participants who chose not to disclose their racial/ethnic background. Missingness was related only to slightly higher CP. Given the small proportion of missing data and its lack of association with dependent measures, we used list-wise deletion to manage missing data.
Results
Descriptive statistics
Descriptive statistics and correlations (Table 1) were assessed for continuous variables. Nearly 20 % of the sample (n = 129) had never had sex; 73 % reported having had only opposite sex partners (n = 484), five men and nine women reported only same sex partners, and 32 individuals reported both opposite and same sex partners. The average number of casual sexual partners was 1.178 (SD = 2.515) and ranged from 0 to 25, whereas the number of monogamous sexual partners ranged from 0 to 8 (M = 1.036, SD = 1.265). Given that casual and monogamous sexual partners variables are count variables, poisson regression was also explored. However, both variables displayed overdispersion, where the variance was greater than the mean, suggesting that a model based on a normal distribution fit would fit better than one based on a poisson distribution. Given the high skew and kurtosis of casual and monogamous sexual partners variables, these variables were log transformed, resulting in skew and kurtosis that were still outside of the acceptable range. Results conducted with these transformed variables were not different from results reported herein.
Correlations of ADHD symptoms and DIT scales ranged from .111 to .326, and the range of correlations among DIT scales was from .526 to .750. The wide range of correlations among ADHD symptoms and DIT scales suggests that ADHD symptoms relate differently to various aspects of DIT. The moderating effect of DIT scales on the link between ADHD symptoms and number of sexual partners may also differ. Further, the high collinearity among DIT scales would impede drawing accurate conclusions about their effects if they were included simultaneously in the same model. ADHD symptoms and CP were related (r = 0.27, p < 0.001), supporting the decision to evaluate the moderating effect of CP on the link between ADHD and number of sexual partners.
Casual sexual partners
Results indicated that CP had a positive main effect on number of causal sexual partners (β = .346, SE = .060, t = 5.72, p < 0.001), but CP and ADHD symptoms did not interact. ADHD symptoms did interact with several DIT scales (see Table 2), including disregulation, tolerance, and appraisal (ADHD × disregulation: β = .026, SE = .009, t = 2.926, p = 0.004; ADHD × tolerance: β = .023, SE = .009, t = 2.661, p = 0.008; ADHD × appraisal: β = .033, SE = .011, t = 3.040, p = 0.002, see Fig. 1). These interactions indicated that individuals who were high on both ADHD and disregulation, tolerance, or appraisal showed the highest number of casual sexual partners. Tests of the simple slopes for these interactions indicated that number of casual sexual partners significantly increased as disregulation, tolerance, or appraisal increased at both high and low levels of ADHD symptoms (see Table 4). However, no main effects of DIT scales or ADHD symptoms were significant, although CP remained a significant predictor in all models.
Monogamous sexual partners
Results indicated that CP had a positive main effect on number of causal sexual partners (β = .081, SE = .031, t = 2.616, p = 0.009), but the interaction of ADHD symptoms and CP was not significant. Only the interaction of ADHD symptoms and Disregulation was significantly associated with the number of monogamous sexual partners (β = .010, SE = .005, t = 2.074, p = 0.038; see Table 3). Results of this interaction indicated that college students with high ADHD symptoms and disregulation reported the highest number of monogamous partners (see Fig. 2). Tests of the simple slopes of the interactions indicated that number of monogamous partners significantly increased as disregulation increased at both high and low levels of ADHD symptoms (see Table 4). Main effects of DIT subscales and ADHD symptoms were not significant, although CP was significant in all models.
Comments
In this study, we evaluated the moderating effects of DIT and CP on the link between ADHD symptoms and number of sexual partners. We found that, although CP made a strong independent contribution to number of sex partners, CP did not increase risky sex for those with ADHD symptoms. Analyses indicated that several facets of DIT, specifically disregulation, appraisal, and tolerance, moderated the link between number of sex partners and ADHD symptoms.
This study addresses gaps in the literature in several ways. First, although some research shows that ADHD symptoms are associated with risky sex for young adults, little research identifies factors that contribute to risky sex for those with ADHD symptoms. Second, the role of CP in risky sex for those with ADHD symptoms remains unclear. Third, the link between DIT and risky sex has also received little attention, despite strong links between DIT and risky behavior in general. Fourth, it is unclear how these factors relate specifically to number of casual or monogamous sex partners. Number of sex partners is important as each additional partner incrementally increases exposure to the possibility of negative outcomes, such as unwanted pregnancy or an STI.
Results extend previous research on DIT by indicating that together ADHD symptoms and DIT contribute to risky sex, although results also conflict with previous research since the main effect of DIT was not significant. Previous research indicates that DIT increases a wide variety of risk behaviors, such as substance use (Buckner et al. 2007) and gambling addiction (Daughters et al. 2005). Several factors may contribute to discrepancies between previous research and our findings. It is possible that risky sex may have contextual differences from other risk behaviors, such as gambling or substance use. Although individual can immediately engage in many risky behaviors, the goal-oriented behavior necessary to identify a partner who will agree to engage in sexual activity may make risky sex a less feasible risky behavior when DIT is high. Also, previous research on the link between DIT and risky behaviors has not included impulsivity or ADHD symptoms. Both factors are strongly related to risk behavior (Daughters et al. 2005; Olazagasti et al. 2013), and recent research demonstrates that DIT may be closely related to impulsivity (Anestis et al. 2012), a primary feature of ADHD. These findings indicate that ADHD symptoms and DIT increase risky sex more together than either factor alone, suggesting that DIT may be an important component in risk behavior associated with ADHD symptoms.
Identifying the context of distress that impacts casual sex for individuals with ADHD symptoms may clarify the moderating effect of DIT. The possibility of acceptance or rejection from a potential partner may create distress that is particularly salient for this population. The concept of DIT stems from a negative reinforcement model of risk behavior, where individuals engage in behaviors to escape the distress or negative affect associated with specific stimuli. Given that individuals with ADHD frequently experience social impairment and rejection (Flory et al. 2006a, b; Barkley et al. 2006), these individuals may experience sensitivity to rejection when meeting potential sexual partners and may engage in casual sex to escape the anticipated distress of rejection. In fact, some research indicates that rejection sensitivity moderates the link between ADHD diagnosis and number of lifetime sexual partners (Canu and Carlson 2007), lending support to this interpretation of our findings. Alternatively, ADHD is associated with delay aversion, where waiting for rewarding stimuli is aversive (Wilbertz et al. 2013). Once individuals with ADHD symptoms identify their physical attraction to someone, they may experience the time period between meeting a potential sexual partner and being physically intimate as aversive. To escape this aversive experience, these individuals may be more likely to engage in sexual activity than those without ADHD symptoms. Identifying factors that contribute to increases in DIT difficulties for those with ADHD symptoms is an important next step to understand how this construct relates to risky sex.
It is unclear if the results regarding DIT suggest a risk or protective effect on number of monogamous partners for individuals with ADHD symptoms. On the one hand, engaging in sexual activity with a monogamous partner when distressed may carry fewer negative outcomes than other risk behaviors, such as illicit drug use, binge drinking, or delinquent behavior. Further, sexual activity in the context of a committed relationship may lead to increased intimacy, contributing to the stability of the relationship and enhancing social support. Conversely, monogamous sexual relationships may still carry risks for pregnancy and STIs, given preference for contraception rather than condom use among couples (Corbin and Fromme 2002) and the frequency of infidelity (Warren et al. 2012).
Number of monogamous sex partners may be a proxy for number of romantic relationships, indicating difficulty maintaining a stable romantic relationship. Consistent with this interpretation, young adults with ADHD display more conflict and volatility in romantic relationships (Canu and Carlson 2007). According to our results, it is possible that difficulties managing distress may contribute to difficulties negotiating the interpersonal demands of a romantic relationship for young adults with ADHD symptoms.
ADHD symptoms did not have a main effect on number of sex partners in any of the models. Although few studies have evaluated the association between ADHD symptoms and number of sex partners, these findings conflict with previous research (Barkley et al. 2006; Flory et al. 2006a, b). The role of CP in the link between ADHD symptoms and risky sex may change depending on the type of risky sexual behavior. Future research should further evaluate the role of CP in risky sexual behavior for those with ADHD symptoms.
Limitations
Several limitations should be noted. First, symptoms, not diagnosis, were used for ADHD and CP. We took this approach given evidence that disruptive behavior is best represented on a continuum of symptom severity rather than with discrete diagnoses (Marcus and Barry 2011). Further, dichotomized continuous variables have well-known methodological shortcomings that would have limited the statistical validity of our findings (MacCallum et al. 2002). Subthreshold ADHD symptom severity may also contribute to increases in risky sexual behavior that would be lost if diagnosis had been used rather than symptom severity. Second, we exclusively used self-reported measures. However, self-reported ADHD symptoms display strong concurrent validity with parent and spousal report of symptoms (Barkley et al. 2011), and self-reported CP is associated with higher rates of delinquent behavior than parent report (Cashel 2003).
Conclusions and future directions
These findings could be used to inform intervention development for risky sex for college students with ADHD symptoms. For example, building both competence and efficacy regarding one’s capacity to cope with distress may be crucial for helping young adults with ADHD to avoid the negative outcomes associated with risky sex.
Future research should also explore the influence of sensation-seeking and peer influence on risky sex for young adults with ADHD symptoms. Current research indicates that sensation-seeking increases substance use for those with ADHD symptoms (Van Eck et al. 2012), and it may also play a role in risky sex for this population. Further, peer influences also appear to shape decision-making processes that favor substance use for those with ADHD (Marshal and Molina 2006); these findings may extend to risky sex as well.
References
American College Health Association (2013) American college health association-national college health assessment II: reference group undergraduates executive summary spring 2013. American College Health Association
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (4th ed., text rev.).Washington, DC
Anestis MD, Lavender JM, Marshall-Berenz EC, Gratz KL, Tull MT, Joiner TE (2012) Evaluating distress tolerance measures: interrelations and associations with impulsive behaviors. Cogn Ther Res 36:593–602
Barkley RA, Fischer M (2010) The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J Am Acad Child Adolesc Psychiatry 49:503–513
Barkley RA, Fischer M, Smallish L (2006) Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry 45:192–202
Barkley RA, Murphy KR, Fischer M (2008) ADHD in adults: what the science says. Guilford, New York
Barkley RA, Knouse LE, Murphy KR (2011) Correspondence and disparity in the self-and other ratings of current and childhood ADHD symptoms and impairment in adults with ADHD. Psychol Assess 23:437
Bearman PS, Jones J, Udry JR (1997) The national longitudinal study of adolescent health: research design. Available from: http://www.cpcp.unc.edu/projects/addhealth/design.html
Buckner JD, Keough ME, Schmidt NB (2007) Problematic alcohol and cannabis use among young adults: the roles of depression and discomfort and distress tolerance. Addict Behav 32:1957–1963
Buhi ER, Marhefka SL, Hoban MT (2010) The state of the union: sexual health disparities in a national sample of US college students. J Am Coll Health 58:337–346
Canu WH, Carlson CL (2007) Rejection sensitivity and social outcomes of young adult men with ADHD. J Atten Disord 10:261–275
Cashel ML (2003) Validity of self-reports of delinquency and socio-emotional functioning among youth on probation. J Offender Rehabil 37:11–23
Centers for Disease Control and Prevention (2012) Sexually transmitted disease surveillance. Department of Health and Human Services
Cohen J, Cohen P, West SG, Aiken LS (2003) Applied multiple regression/correlation analysis for the behavioral sciences, 3rd edn. Erlbaum, Mahwah
Cooper ML (2002) Alcohol use and risky sexual behavior among college students and youth: evaluating the evidence. J Stud Alcohol Drugs S14:101–117
Corbin WR, Fromme K (2002) Alcohol use and serial monogamy as risks for sexually transmitted diseases in young adults. Health Psychol 21:229–236
Daughters SB, Lejuez CW, Strong DR, Brown RA, Breen RB, Lesieur HR (2005) The relationship among negative affect, distress tolerance, and length of gambling abstinence Attempt. J Gambl Stud 21:363–378
DuPaul GJ, Weyandt LL, O’Dell SM, Varejao M (2009) College students with ADHD: current status and future directions. J Atten Disord 13:234–250
Edel MA, Rudel A, Hubert C, Scheele A, Brϋne M, Juckel G, Assion HJ (2010) Alexithymia, emotion processing and social anxiety in adults with ADHD. Eur J Med Res 15:403–409
Elliott D, Huizinga D, Ageton S (1985) Explaining delinquency and drug use. Sage, CA
Farrington DP, Loeber R, Stouthamer-Loeber M, Van Kammen WB, Schmidt L (1996) Self-reported delinquency and a combined delinquency seriousness scale based on boys, mothers, and teachers: concurrent and predictive validity for African-Americans and Caucasians. Criminology 34:493–517
Finer LB, Henshaw SK (2006) Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health 38:90–96
Flack WF, Daubman KA, Caron ML, Asadorian JA, D’Aureli NR, Gigliotti SN, Stine ER (2007) Risk factors and consequences of unwanted sex among university students: hooking up, alcohol, and stress response. J Interpers Violence 22:139–157
Flory K, Milich R, Lorch EP, Hayden AN, Strange C, Welsh R (2006a) Online story comprehension among children with ADHD: which core deficits are involved? J Abnorm Child Psychol 34:853–865
Flory K, Molina BSG, Pelham WE, Gnagy E, Smith B (2006b) Childhood ADHD predicts risky sexual behavior in young adulthood. J Clin Child Adolesc Psychol 35:571–577
Fromme K, Corbin WR, Kruse MI (2008) Behavioral risks during the transition from high school to college. Dev Psychol 44:1497–1504
Galéra C, Bouvard MP, Melchior M, Chastang JF, Lagarde E, Michel G, Fombonne E (2010) Disruptive symptoms in childhood and adolescence and early initiation of tobacco and cannabis use: the Gazel youth study. Eur Psychiatry 25:402–408
Hosain GM, Monawar AB, Tennen H, Bauer LO, Wu ZH (2012) Attention deficit hyperactivity symptoms and risky sexual behavior in young adult women. J Women’s Health 21:463–468
Kaiser AJ, Milich R, Lynam DR, Charnigo RJ (2012) Negative urgency, distress tolerance, and substance abuse among college students. Addict Behav 37:1075–1083
Lee SS, Humphreys KL, Flory K, Liu R, Glass K (2011) Prospective association of childhood ADHD and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev 31:328–341
Lewis MA, Granato H, Blayney JA, Lostutter TW, Kilmer JR (2011) Predictors of hooking up sexual behavior, and emotional reactions among U.S. college students. Arch Sex Behav 41:1219–1229
Lochman JE, Bierman KL, Coie JD, Dodge KA, Greenberg MT, McMahon RJ, Pinderhughes EE (2010) The difficulty of maintaining positive intervention effects: a look at disruptive behavior, deviant peer relations, and social skills during the middle school years. J Early Adolesc 30:593–624
Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB (1998) Antisocial behavior and mental health problems: explanatory factors in childhood and adolescence. Erlbaum, Mahwah
MacCallum RC, Zhang S, Preacher KJ, Rucker DD (2002) On the practice of dichotomization of quantitative variables. Psychol Methods 7:19–40
Mannuzza S (1993) Adult outcome of hyperactive boys educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 50:565–576
Marcus DK, Barry TD (2011) Does ADHD have a dimensional latent structure? A taxometric analysis. J Abnorm Psychol 120:427
Marshal MP, Molina B (2006) Antisocial behaviors moderate the deviant peer pathway to substance use in children with ADHD. J Clin Child Adolesc Psychol 35:216–226
Mitchell J, Robertson C, Anastopolous A, Nelson-Gray RO, Kollins SH (2012) Emotion dysregulation and emotional impulsivity among adults with attention-deficit/hyperactivity disorder: results of a preliminary study. J Psychopathol Behav Assess 34:510–519
Olazagasti M, Klein R, Mannuzza S, Roizen Belsky E, Hutchison JA, Lashua-Shriftman EC, Castellanos FX (2013) Does childhood attention-deficit/hyperactivity disorder predict risk-taking and medical illnesses in adulthood? J Am Acad Child Adolesc Psychiatry 52:153–162
Ott MA, Katschke A, Tu W, Fortenberry JD (2011) Longitudinal associations among relationship factors, partner change, and sexually transmitted infection acquisition in adolescent women. Sex Transm Dis 38:153–157
Owen J, Fincham FD, Moore J (2011) Short-term prospective study of hooking up among college students. Arch Sex Behav 40:331–341
Parkin DM, Bray F (2006) The burden of HPV-related cancers. Vaccine 24:11–25
Patrick K, Covin JR, Fulop M, Calfas K, Lovato C (1997) Health risk behaviors among California college students. J Am Coll Health 45:265–273
Paul EL, McManus B, Hayes A (2000) “Hook-ups”: characteristics and correlates of college students’ spontaneous and anonymous sexual experiences. J Sex Res 37:76–88
Pedra MP, Pérez MEG, Mora JS, Mayolas SF (1999) HIV heterosexual transmission and serial monogamy in university students. Psiquis 20:55–57
Raley RK, Kim Y, Daniels K (2012) Young adults’ fertility expectations and events: associations with college enrollment and persistence. J Marriage Fam 74:866–879
Ramrakha S, Bell ML, Paul C, Dickson N, Moffitt TE, Caspi A (2007) Childhood behavior problems linked to sexual risk taking in young adulthood: a birth cohort study. J Am Acad Child Adolesc Psychiatry 4:1272–1279
Reimherr FW, Marchant BK, Olson JL, Halls C, Kondo DG, Williams ED, Robison RJ (2010) Emotional dysregulation as a core feature of adult ADHD: its relationship with clinical variables and treatment response in two methylphenidate trials. J ADHD Relat Disord 1:53–64
Schneider M, Yin L (2011) The high cost of low graduation rates: How much does dropping out of college really cost?. American Institutes for Research, Washington, DC
Simons JS, Gaher RM (2005) The distress tolerance scale: development and validation of a self-report measure. Motiv Emot 29:83–104
Van Eck K, Markle R, Flory K (2012) Do conduct problems and sensation-seeking moderate the association between ADHD and three types of stimulant use in a college population? Psychol Addict Behav 26:939–947
Warren JT, Harvey SM, Agnew CR (2012) One love: explicit monogamy agreements among heterosexual young adult couples at increased risk of sexually transmitted infections. J Sex Res 49:282–289
Whiteside SP, Lynam DR (2001) The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personal Individ Differ 30:669–689
Wilbertz G, Trueg A, Sonuga-Barke EJS, Blechert J, Philipsen A, van Elst LT (2013) Neural and psychophysiological markers of delay aversion in attention-deficit hyperactivity disorder. J Abnorm Psychol 122:566–572
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Eck, K., Flory, K. & Willis, D. Does distress intolerance moderate the link between ADHD symptoms and number of sexual partners?. ADHD Atten Def Hyp Disord 7, 39–47 (2015). https://doi.org/10.1007/s12402-014-0140-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-014-0140-3