Abstract
This multi-centre, open-label, non-interventional study evaluates effectiveness, safety and adherence to treatment of a specific extended-release methylphenidate with a 50 % immediate and a 50 % extended-release component (Medikinet® retard) in the clinical routine treatment of 381 adolescents with ADHD and a mean age of 14.0 ± 1.9 years. ADHD and associated psychiatric symptoms, medication status and dosage frequency, treatment adherence and adverse events were assessed at baseline and after a median treatment length with Medikinet® retard of 70 days. Primary outcome criterion was the change of ADHD symptom severity from baseline to endpoint according to the ADHD–KGE (German: ADHS–Klinische Gesamteinschätzung) change score. At baseline, 4.2 % of the patients were treatment naïve, 92.7 % had previously received different methylphenidate formulations and 3.1 % had received atomoxetine or amphetamine. During the study, patients received a mean daily dose of 35.7 ± 15.1 mg Medikinet® retard. At endpoint, in 78 % of patients, the total ADHD symptom severity was reduced, in 20.4 %, it remained unchanged and in 1.6 %, it was worsened. The mean ADHD–KGE total ADHD symptom score was reduced from 1.8 ± 0.7 (moderate) at baseline to 0.8 ± 0.5 (mild; p < 0.001) at endpoint; the mean ADHD–KGE total-associated symptom score was reduced from 1.9 ± 0.7 (moderate) at baseline to 1.0 ± 0.6 (mild; p < 0.0001) at endpoint. After the medication switch from previous methylphenidate formulation to Medikinet® retard, multiple dosing with ≥3 daily medication intakes was reduced from 12.9 % at baseline to 3.1 % at endpoint (p < 0.001). Adherence to treatment was improved in 37 % of patients. Most frequent adverse events were loss of appetite and gastrointestinal problems. The findings suggest that pharmacologically treated adolescents with ADHD and insufficient symptom reduction and/or treatment adherence benefit from switching to Medikinet® retard and that it is well tolerated when given in clinical routine care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to a meta-analysis of 102 studies worldwide, the average prevalence rate of attention deficit hyperactivity disorder (ADHD) in children and adolescents is 5.2 % (Polanczyk et al. 2007). Numerous double-blind randomized controlled trials (RCTs) as well as meta-analyses have shown methylphenidate (MPH) to be an effective treatment of ADHD in children and adolescents and to reduce symptoms in about 75 % of patients (Banaschewski et al. 2006; Faraone et al. 2004). In Germany, different MPH formulations are available, including immediate release MPH (MPH-IR) formulations with a drug action duration of 3–4 h and extended-release MPH (MPH-ER) formulations with a drug action duration of 7–12 h. MPH-ER formulations contain MPH-IR and MPH-ER and differ in their release mechanisms, proportion of MPH-IR and MPH-ER and their drug action duration (MPH sustained release, MPH-SR; MPH long sustained release, MPH-LSR) (Lopez 2006; Prince 2006). Medikinet® retard is an MPH-SR formulation that consists of 50 % MPH-IR and of 50 % MPH-ER and has a drug action duration of about 7 h. The effectiveness of Medikinet® retard for ADHD in children and adolescents has been shown in numerous RCTs (Döpfner et al. 2003, 2004, 2011a; Sinzig et al. 2004, 2007). RCTs with both highly selected patients and highly controlled, standardized study procedures, which ensure that the patients being compared differ only in their exposure to the intervention under study, are seen by many as the ‘gold standard’ to prove drug efficacy and safety. However, RCTs reflect clinical reality and diversity of patients only insufficiently and lack external validity. This reduces the extent to which results from RCTs are generalizable to all potentially treated patients. Since uncontrolled open-label, non-interventional, observational, post-marketing surveillance studies are less rigorous in their experimental design and less selective in their sample selection, they allow the evaluation of a drug’s effectiveness and safety in real-world clinical settings and extent the results of RCTs (Rothenberger and Döpfner 2011). However, to date, there are only few observational studies evaluating effectiveness and safety of treatment with methylphenidate under naturalistic conditions. These studies have primarily focused on school-aged children with ADHD that had an average age from 9.5 to 11.4 years (Remschmidt et al. 2005; Heger et al. 2006; Gau et al. 2008; Döpfner et al. 2011a, b, c). The prospective, uncontrolled, non-interventional study (NIS) presented in the following investigates effectiveness, administration of medication, treatment adherence and safety of Medikinet® retard for treatment of adolescent ADHD patients under clinical routine conditions.
Methods
Participants
The study included male and female patients between 12 and 17 years and confirmed ADHD diagnosis according to ICD-10 (WHO 1991; ICD-10 code F90.0: disturbance of activity and attention, which equals ADHD, combined type according to DSM-IV code 314.01; APA 2000; ICD-10-code F90.1: hyperkinetic conduct disorder; and ICD-10-code F90.9: hyperkinetic disorder, unspecified, which equals ADHD, predominately inattentive type according to DSM-IV code 314.00). Treatment-naïve patients with indication for treatment with Medikinet® retard or previously treated patients with indication for switch of medication to Medikinet® retard were eligible for study participation. Exclusion criteria included contraindications against Medikinet® retard according to the summary of product characteristics (SPCs). Comorbid psychiatric or somatic disorders, concomitant medication or non-pharmacological therapies were no exclusion criteria.
Study design
This was a prospective, uncontrolled, multicentre, NIS. The study was approved by the ethical committee of the state of the Saarland, Germany. The study design is in accordance with Sects. 4, 23 and 67, 6 German Drug Law, which requires a NIS to be strictly observational. Informed consent was not required for this study. All procedures during study including medication must be based on clinical requirements as appraised by the responsible physicians and not on a rigorous predefined study design. Participating physicians were asked to include 1–4 patients and received a financial compensation of 75€ per patient. According to the SPC, physicians were recommended not to exceed a maximum dosage of 60 mg Medikinet® retard once daily in the morning. Data were collected at T1 (baseline) and at T2 (study endpoint) after 6–12 weeks treatment with Medikinet® retard. Study assessments at T1 and T2 are shown in Table 1. The primary outcome criterion, which was used to evaluate treatment effectiveness, was the change of ADHD symptom severity between T1 and T2 according to the ADHD–KGE (German: ADHS–Klinische Gesamteinschätzung) change scale. Treatment effectiveness was defined a priori as no change or reduction in total ADHD symptom severity on the ADHD–KGE change scale in ≥80 % of the patients of the study population at T2. Further research goals were to assess dosing regimen, treatment adherence and side effects of Medikinet® retard compared to previous treatment. Results are displayed in accordance with the STROBE criteria (von Elm et al. 2008).
Assessments
All assessments were performed by physicians who were well experienced in diagnosing and treating patients with ADHD. The physicians were trained to use the rating scales and asked to assess symptom severity of ADHD core and associated symptoms, effectiveness (ADHD–KGE) and adherence (6-point scale) on the synopsis of the patients’ and parents’ clinical interviews and the physician’s clinical assessment of the current symptoms compared to other patients with ADHD.
ADHD and associated symptoms
ADHD Global Clinical Impression Scale
The ADHD Global Clinical Impression Scale (German: ADHS–Klinische Gesamteinschätzung [ADHD–KGE]; (Döpfner et al. 2006) was used to quantify ADHD and associated symptoms. It assesses on a 4-point scale (0 = not at all, 1 = mild, 2 = moderate, 3 = severe) cross-sectional severity of the ADHD core symptoms cluster inattention, hyperactivity and impulsivity, of the five frequently associated symptom cluster aggression, depression, anxiety, tics, learning disabilities and of overall severity of ADHD and associated symptoms. Additionally, it assesses treatment effectiveness by a 7-point change scale (+3 to +1 = very much to slightly improved, 0 = no change, −1 to −3 = slightly to severely worse).
Adherence
In accordance with previously published non-interventional studies (Rothenberger et al. 2011), adherence was assessed on a 6-point scale following German school grades (1 = excellent adherence to 6 = insufficient adherence).
Adverse events
Adverse events were assessed by spontaneous report during the clinical interview at each visit.
Statistics
The data management checked whether data were complete, plausible and consistent. If data were missing or implausible, the physicians were queried. The data were analysed descriptively. To check for a possible bias by the physicians’ specialty (paediatrics, child and adolescent psychiatry), the ADHD–KGE total ADHD symptom score at baseline was compared between the medical specialties in the intention-to-treat (ITT)-population. The patients’ characteristics were also analysed in the ITT population. The primary outcome criterion (ADHD–KGE change score) was calculated in the ITT- and the per-protocol (PP)-population. A sensitivity analysis with worst-case scenario was used to examine the results. Missing values were replaced with the lowest possible score on the ADHD–KGE change scale (severely worse = −3). A chi-square test was used to analyse nominal variables. A Wilcoxon test or a Kruskal–Wallis test was used to analyse ordinal or continuous variables. Changes to the base values were analysed with a paired t-test.
Results
Sample
Demographic and clinical characteristics
In total, 97 office-based physicians participated in the NIS of whom 60.1 % were paediatricians, 34.4 % were child and adolescent psychiatrists and 5.5 % pertained to other specialties, mostly psychiatry. Three hundred eighty-one patients were enrolled in the NIS (ITT population). The ADHD–KGE total ADHD symptom score at baseline did not vary across the different medical specialties with an ADHD–KGE total ADHD symptom baseline score of 1.8 ± 0.6 (moderate) as assessed by paediatricians and of 1.8 ± 0.8 (moderate; n. s.) as assessed by child and adolescent psychiatrists. Of the ITT population, 347 patients were included in the PP analysis. The main reason for excluding patients from the PP population was disregarding the age criterion of ≥12 years (n = 22/34).
The mean patients’ age was 14.0 ± 1.9 years. Twenty-two patients were <12 years (5.8 %), 217 patients were 12–14 years (57 %), and 140 patients were ≥15 years (36.8 %). Age was not provided for two patients (0.5 %). Three hundred and seven patients were male (81 %) and 74 (19 %) were female. The average height was 161.4 ± 13.1 cm; the average weight was 53.2 ± 16.2 kg, and the average BMI was 20.1 ± 4.3. Twenty-one patients attended elementary school (5.5 %) and 303 secondary school (79.5 %), 31 received special education (8.1 %) and 8 other schooling (2.1 %), 8 had graduated (2.1 %), and for 10, information on schooling was not provided (2.6 %).
Two hundred and forty-seven (64.8 %) patients were diagnosed with disturbance of activity and attention (ICD-10 code F90.0), which equals ADHD, combined type (DSM-IV-code 314.01); 123 (32.3 %) were diagnosed with hyperkinetic conduct disorder (ICD-10 code F90.1), and 10 (2.6 %) were diagnosed with unspecified hyperkinetic disorder (ICD-10 code F90.9), which equals ADHD, predominately inattentive type (DSM-IV code 314.00). Information regarding the diagnosis was missing for 1 (0.3 %) patient. On average, the patients were first diagnosed with ADHD 3.7 ± 2.8 years before being included in the NIS. Fifty-eight patients (15.2 %) had one or more comorbid mental disorders. The most frequent-associated psychiatric disorders were speech and language disorders and learning disabilities (34; 8.9 %), depressive disorders (12; 3.1 %) and anxiety disorders (9; 2.4 %). Four patients were diagnosed with Asperger’s syndrome (1 %) and 5 had tic disorders (1.3 %). In total, 42 patients (11 %) received medication for a comorbid disorder, of whom 19 (5 %) received psychiatric medications. Four patients received anticonvulsants (lamotrigine, valproate), 13 antipsychotics (risperidone, pipamperone, tiapride), 1 citalopram and 1 melatonin. The most common medications for physical disorders were asthma medications (10 patients took ß-2 adrenergic agonists, 10 glucocorticoids) and allergy medications (4 patients took antihistamines, 4 cortisone/cromoglicic acid eye drops or nasal sprays). Eight patients took other internal medications (levothyroxin, pyridostigmine, insulin, enalapril, macrogol, iodine).
In total, 304 (79.7 %) patients received non-pharmacological treatments; 63 (16.5 %) received behaviour therapy and 50 (13.1 %) some other type of psychotherapy, 56 families (14.7 %) participated in parent counselling, parent coaching or family therapy, 53 (13.9 %) patients received psychoeducation, 31 (8.1 %) were treated for learning disabilities, 28 (7.3 %) received school-based interventions and 23 (6.0 %) occupational therapy.
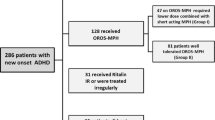
Administration of medication
At baseline (T1), 353 patients (92.7 %) received MPH, 10 (2.6 %) atomoxetine, 2 (0.5 %) amphetamine and 16 (4.2 %) patients were treatment naïve. Of the patients, pre-treated with MPH, 24 (6.3 %) received MPH-IR once and 114 (29.9 %) multiple doses daily, 102 (26.8 %) received MPH-SR once and 15 (3.9 %) multiple doses daily, 36 (9.4 %) received MPH-LSR once daily and 62 (16.3 %) received a combination of one or more doses of MPH-IR/-SR, MPH-IR/-LSR and MPH-SR/-LSR. The reasons for multiple doses throughout the day (counting multiple responses) were a lot of homework (10 %), difficult class work (5 %), studying for a test (4.5 %), afternoon classes (4.2 %), all-day school (2.1 %) and others (5.5 %).
The main reasons for switching therapy (counting multiple responses) were too short drug action duration (172; 45.1 %), forgetting the second or third dose (132; 34.6 %), one dose not sufficient (125; 32.8 %), unwillingness to take medication at school (121; 31.8 %), too late onset of drug action (31; 8.1 %), lack of effectiveness (26; 6.8 %) and side effects (14; 3.7 %). The most common reason for switching to Medikinet® retard when patients had been treated with a single dose of MPH-IR was a too short drug action duration (18; 4.7 %). The two most common reasons for switching when patients had been treated with multiple doses of MPH-IR daily were forgetting the second or third dose (74; 19.4 %) and unwillingness to take the medication at school (73; 19.2 %). The most common reason for switching when patients were treated with MPH-LSR was the too late onset of drug action (11; 2.9 %).
The median observational period for the treatment with Medikinet® retard was 70 days. At T2, 76.4 % of patients were treated with Medikinet® retard and 23.6 % were treated with a combination of Medikinet® retard and MPH-IR. All patients received Medikinet® retard in the morning, 16 % received a second dose at lunchtime and 4 % on a pro re nata basis. Of the patients treated with combination therapy, 7.9 % received an additional dose of MPH-IR in the morning, 9.7 % at lunchtime, 0.5 % in the evening and 5.5 % on a pro re nata basis. The percentage of patients that took the medication twice daily did not change with the switch to Medikinet® retard (T1: 122 (32.0 %); T2: 136 (35.7 %); n. s.). The percentage of patients, who took ≥3 daily doses of their medication was significantly reduced by the switch to Medikinet® retard (T1: 49 (12.9 %); T2: 12 (3.1 %); p < 0.001). The average daily dose of MPH at T1 was 31.2 ± 15.0 (5–120) mg/d and 0.6 ± 0.3 (0.2–2.2) mg/kg of the body weight. The average dose of Medikinet® retard at T2 was 35.7 ± 15.1 (5–120) mg/d and 0.7 ± 0.3 (0.2–2.8) mg/kg of the body weight and thus significantly higher (p < 0.001). Eleven patients received a dose that exceeded the daily limit of 60 mg recommended by the SPC. Most patients continued taking Medikinet® retard after T2 and 13 patients (3.4 %) stopped taking it. The reasons for not continuing Medikinet® retard were medication was not effective (n = 1), scheduled end of therapy (n = 1) and sleeping problem (n = 1); for 10 patients, a reason for discontinuation was not provided. No information was given about subsequent medication for 24 patients.
Effectiveness
ADHD and associated symptoms
At T2, the ADHD–KGE ADHD total symptom change score was rated in the ITT-population as improved or unchanged in 318 patients (98.4 %; 95 %-confidence interval [CI]: 96.4–99.4 %) and worse in 5 patients (1.6 %; 95 % CI interval: 0.5–3.6 %). Information regarding the change in the ADHD symptoms was missing for 58 patients. When the 58 missing values were replaced by the worst possible score (-3 severely worse) during a worst-case analysis, the ADHD symptoms were judged worse in 63 patients (16.5 %; 95 % CI interval: 13–21 %). Using the PP population, the ADHD symptoms were rated as improved or unchanged in 294 patients (98.3 %; 95 % CI interval: 96.1–99.5 %) and worse in 5 patients (1.7 %; 95 % CI interval: 0.5–3.9 %). Information regarding the change in the ADHD symptoms was missing for 48 patients. During a worst-case analysis, the ADHD symptoms were judged worse in 53 patients (15.3 %; 95 % CI interval: 12–19 %). Thus, the predefined criterion for effectiveness as no change or reduction in total ADHD symptom severity on the ADHD–KGE change scale in ≥80 % of patients at T2 was met when using the ITT and PP population and confirmed with the worst-case analyses. Results are shown in Table 2.
The ADHD–KGE total ADHD symptom scores were reduced from 1.8 ± 0.7 (moderate) with previous medication at T1 to 0.8 ± 0.5 (mild) under Medikinet® retard at T2 (p < 0.001). Of the three ADHD core symptom, cluster inattention was reduced strongest from 2.0 ± 0.7 (moderate) at T1 to 1.0 ± 0.6 (mild) at T2 (p < 0.0001). Hyperactivity and impulsivity were also reduced statistically significant by the switch but clinically assessed at both time points as mild (Impulsivity 1.4 ± 0.9 vs. 0.7 ± 0.7, p < 0.0001; hyperactivity 1.2 ± 0.6 vs. 0.6 ± 0.7, p < 0.0001). The ADHD–KGE total-associated symptom scores were reduced from 1.9 ± 0.7 (moderate) at T1 to 1.0 ± 0.6 (mild; p < 0.0001) at T2. Learning disabilities (1.8 ± 0.8 vs. 1.0 ± 0.7, p < 0.0001) and aggression (0.8 ± 0.9 vs. 0.4 ± 0.6, p < 0.0001) were reduced significantly form moderate to mild; symptom severity of depression, anxiety and tics remained unchanged and was rated as mild at T1 and T2. The results are shown in Fig. 1.
The stratification according to previous treatment, ADHD subtype and ADHD with or without comorbid mental disorders showed a significant reduction in ADHD and associated symptoms at T2 compared to T1 on the ADHD–KGE ratings. Besides in patients, that were previously treated with MPH-IR and patients with primarily inattentive symptoms, overall severity of ADHD was reduced from moderate to mild. The results are shown in Table 3.
Adherence
At T2, adherence was improved in 142 patients (37.3 %), unchanged in 116 patients (30.4 %) and worsened in 25 patients (6.6 %). Information regarding adherence was missing for 98 patients (25.7 %). Mean adherence increased by 0.7 ± 1.2 points (p < 0.001). Patients that had been previously treated with multiple doses of MPH-IR improved their adherence strongest by 1.5 ± 1.2 points (p < 0.001) with Medikinet® retard compared to previous treatment. Patients that had been previously treated with MPH-LSR improved their adherence by 0.2 ± 0.8 points (n. s.), patients previously treated with MPH-LSR/IR by 0.3 ± 0.7 points (n. s.) and patients previously treated with one daily dose of MPH-IR by 0.4 ± 0.5 points (n. s) and thus did not change medication adherence significantly.
Safety
A total of 61 adverse events (AEs) occurred under previous medication and 33 AEs occurred under treatment with Medikinet® retard. Under previous medication/Medikinet® retard, the following AEs occurred ≥5 times: loss of appetite (n = 9/6), weight loss (n = 5/2), gastrointestinal problems (n = 5/1). AEs were regarded as associated or most likely associated with the medication in 78.8 % during the previous treatment and in 78.8 % during the treatment with Medikinet® retard. Under the previous treatment, 14 AEs (23 %) and under Medikinet® retard 8 AEs (24.2 %) were judged as severe. Under the previous medication, the treatment was discontinued seven times because of AEs (nausea, stomach ache, loss of appetite, weight loss and depression). The treatment with Medikinet® retard was discontinued 5 times because of AEs (sleep problems, inattention, loss of appetite, weight loss and increase of comorbid tics). With the exception of weight loss, all AEs, including worsening of pre-existenting tics, disappeared after discontinuing Medikinet® retard. No critical cardiovascular AEs were recorded under previous medication or during the study. A serious, adverse event (SAE) under Medikinet® retard was a worsening of an anxiety disorder that was already present during the previous therapy and led to hospitalization during the NIS. An association between the SAE and Medikinet® retard was judged as unlikely by the treating physician.
Discussion
The present NIS evaluates the effectiveness of Medikinet® retard in the routine treatment of adolescents with ADHD. The a priori defined criterion for effectiveness (≥80 % of patients with reduction or no change in ADHD symptoms on the ADHD–KGE total ADHD change scale at T2) was met by 98.4 % of the ITT population, by 98.3 % of the PP population and was confirmed by worst-case analyses. ADHD symptoms were reduced from moderate to mild in treatment-naïve patients, patients that previously received MPH-SR, MPH-LSR, multiple daily doses of MPH-IR and combination therapy with different MPH formulations, patients with disturbance of activity and attention and with hyperkinetic conduct disorder and in patients with and without comorbid mental disorders. Inattentive symptoms were reduced from moderate under previous medication to mild under Medikinet® retard, while hyperactivity and impulsivity were both rated as mild under previous medication and Medikinet® retard. Of the associated symptoms, learning problems and aggression were also reduced from moderate to mild by the treatment with Medikinet® retard. Hence, patients profited in two associated symptom clusters that cause considerable impairment in school and social contacts. As MPH doses at T1 and T2 varied significantly, the question arises if the increase in dose at T2 resulted in the observed effects. This possibility cannot completely ruled out as meta-analyses has shown an association of larger MPH effect sizes with use of higher doses (Faraone et al. 2004). However, as the average body weight–adjusted doses of 0.6 ± 0.3 mg MPH/kg previous MPH formulation at T1 and 0.7 ± 0.3 mg Medikinet® retard/kg body at T2 are both in the mean dosage range, we assume no relevant clinical difference in effectiveness due to different doses. The switch to Medikinet® retard significantly reduced the dosing frequency of ≥3 times daily from 12.9 to 3.1 % of patients. However, the frequency of bi-daily doses did not change after switching to Medikinet® retard and thus provided no additional benefit for patients who received bi-daily doses of methylphenidate formulations before the NIS in terms of reduced dosing frequency. The most common reasons for multiple daily doses were a lot of and difficult homework or long school days. This emphasizes the need to control ADHD symptoms throughout the day in adolescents with ADHD with managing daily life becoming more demanding and complex during development. Nonetheless, to date, no RCTs have been conducted that evaluated efficacy and safety of a twice daily dosage of Medikinet® retard. Two studies investigated bi-daily application of Medikinet® adult, which has the same galenic formulation as Medikinet® retard and which has been recently approved in Germany for treatment of adult ADHD. In these studies, middle-aged adults with ADHD were treated over 8 and 24 weeks with a dosage of up to 1 mg Medikinet® adult/kg body weight and the medication was shown to be efficient and safe (Retz et al. 2010; Rösler et al. 2009).
In our study, the treatment with Medikinet® retard increased the adherence in 37.3 % of the patients. The highest increase of 1.5 ± 1.2 points was found in patients that had previously been treated with multiple doses of MPH-IR. There was no significant change in adherence after switching to Medikinet® retard in patients that previously received one daily dose of MPH-LSR or MPH-IR. This finding corresponds to the findings of Rothenberger et al. (2011), who also report from a NIS that adherence improved the most in patients previously treated with multiple daily doses of MPH-IR (57.7 %) and that adherence remained unchanged in 60.2 % of patients previously treated with MPH-IR once daily when switched to the sustained release MPH formulation (Equasym XL®). We assume that the reduction in dosing frequency by the switch to Medikinet® retard resulted in increased adherence since for this group forgetting doses and reluctance to take medication at school were given as most common reasons for the medication switch. Further, other studies have also shown an association between insufficient medication adherence and ≥3 daily doses of MPH-IR (Gau et al. 2008). The improvement of adherence of our sample was considerably less than the improved adherence in 57 % of patients after switch to Medikinet® retard reported by Döpfner et al. (2011b). This may be due to the higher percentage of 41 % of patients that were treated previously with multiple daily doses of MPH-IR in the study by Döpfner et al. (2011b) compared to the 29.9 % of patients in our study and also to the younger age of the patients in the study by Döpfner et al. (2011b), who investigated school children with a mean age of 10.7 ± 2.5 years. This suggests that patients’ parents took care of medication administration in the study by Döpfner et al. (2011b), whereas the adolescent patients investigated by our study may have been more responsible by themselves for medication administration. Our findings are in accordance with recent studies indicating that adolescence is a critical period for treatment discontinuation and reduction in treatment adherence when treating chronic disorders such as ADHD (Turgay et al. 2012).
None of the side effects that occurred during this NIS while administering Medikinet® retard were unexpected compared to RCTs, even though we also included patients that received additional medication for internal or other mental disorders. However, this finding may be biased as most patients with additional medication, that were switched to Medikinet® retard, were previously treated with a combination of another MPH formulation and additional medication, which they tolerated well.
When interpretating the findings of our study, some limitations have to be considered. Because of the open study design and the assessment of symptom severity, effectiveness and adherence by the treating physician, a rater bias cannot be ruled out. The evaluation of adherence was not realized by objective measures, for example pill count, medication event monitoring caps or pharmacy refill records and not defined by distinct cut-offs, e.g. medication possession rates, but relied on the subjective judgement of the clinicians, which may have resulted in an overestimation of adherence (Sajatovica et al. 2010). Adverse events were assessed by spontaneous reports but not by the use of structured measures possibly resulting in underreporting. Most patients that were included in the study had an indication for a medication switch. Thus, the study does not allow for conclusions about general effectiveness or superiority of Medikinet® retard compared to alternative medications. RCTs have to be conducted for this. Nevertheless, our study shows that adolescent patients with ADHD and insufficient symptom reduction and/or adherence under previous medication can profit from switching to Medikinet® retard in clinical practice and that Medikinet® retard is well-tolerated under clinical routine conditions.
References
American Psychiatric Association (2000) Attention-deficit and disruptive behavior disorders. Attention-deficit/hyperactivity disorder. Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Arlington, pp 85–103
Banaschewski T, Coghill D, Santosh P et al (2006) Long-acting medications for the hyperkinetic disorders: a systematic review and European treatment guideline. Eur Child Adolesc Psychiatry 5:476–495
Döpfner M, Banaschewski T, Schmidt J et al (2003) Langzeitwirksames Methylphenidat bei Kindern mit Aufmerksamkeitsdefizit-Hyperaktivitätsstörungen—Eine multizentrische Studie. Nervenheilkunde 22:85–92
Döpfner M, Gerber WD, Banaschewski T et al (2004) Comparative efficacy of once-a-day extended-release methylphenidate, two-times-daily immediate-release methylphenidate, and placebo in a laboratory school setting. Eur Child Adolesc Psychiatry 13:I/93–I/101
Döpfner M, Lehmkuhl G, Steinhausen HC (2006) KIDS 1: Aufmerksamkeitsdefizit- und Hyperaktivitätsstörung. Hogrefe-Verlag, Göttingen
Döpfner M, Ose C, Fischer R, Ammer R, Scherag A (2011a) Comparison of the efficacy of two different modified release methylphenidate preparations for children and adolescents with attention-deficit/hyperactivity disorder in a natural setting: comparison of the efficacy of Medikinet® Retard and Concerta®—a randomized, controlled, double-blind multicenter clinical crossover trial. J Child Adolesc Psychopharmacol 21(5):445–454
Döpfner M, Breuer D, Ose C, Fischer R (2011b) Methylphenidat mit modifizierter Freisetzung in der Routineversorgung. Monatsschr Kinderheilkd. doi:10.1007/s00112-011-2413-7
Döpfner M, Görtz-Dorten A, Breuer D, Rothenberger A (2011c) An observational study of once-daily modified-release methylphenidate in ADHD: effectiveness on symptoms and impairment, and safety. Eur Child Adolesc Psychiatry 20(Suppl 2):S243–S255
Faraone SV, Spencer T, Aleardi M, Biederman J (2004) Meta-analysis of the efficacy of methylphenidate for treating adult attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 24(1):24–29
Gau SSF, Shin-Jwa C, Chou WJ et al (2008) National Survey of adherence, efficacy, and side effects of methylphenidate in children with attention-deficit/hyperactivity disorder in Taiwan. J Clin Psychiatry 69(1):131–138
Heger S, Trott GE, Meusers M, Schulz E, Rothenberger A, Rettig K, Medori R, Schreiner A, Remschmidt H, for the German C-2000-045 study group (2006) Umstellung von einem unretardierten auf ein retardiertes Methylphenidatpräparat: Eine multizentrische, offene Studie an Kindern mit ADHS. Z Kinder Jugendpsychiatr Psychotherapie 34:257–265
Lopez FA (2006) ADHD: new pharmacological treatments on the horizon. J Dev Behav Pediatr 27(5):410–416
Polanczyk G, de Lima MS, Horta BL et al (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948
Prince JB (2006) Pharmacotherapy of attention-deficit hyperactivity disorder in children and adolescents: update on new stimulant preparations, atomoxetine, and novel treatments. Child Adolesc Psychiatr Clin N Am 15:13–50
Remschmidt H, Hoare P, Ettrich C, Rothenberger A, Santosh P, Schmidt M, Spender Q, Tamhne R, Thompson M, Tinline C, Trott GE, Medori R (2005) Symptom control in children and adolescents with attention-deficit/hyperactivity disorder on switching from immediate-release MPH to OROS MPH results of a 3-week open-label study. Eur Child Adolesc Psychiatry 14:297–304
Retz W, Rösler M, Ose C et al (2010) Multiscale assessment of treatment efficacy in adults with ADHD: a randomized placebo-controlled, multi-centre study with extended-release methylphenidate. World J Biol Psychiatry 14:1–12
Rösler M, Fischer R, Ammer R et al (2009) A randomised, placebo-controlled, 24-week, study of low-dose extended-release methylphenidate in adults with attention-deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci 259:120–129
Rothenberger A, Döpfner M (2011) Editorial: Observational studies in ADHD: the effects of switching to modified-release methylphenidate preparations on clinical outcomes and adherence. Eur Child Adolesc Psychiatry 20(Suppl 2):S235–S242
Rothenberger A, Becker A, Breuer D, Döpfner M (2011) An observational study of once-daily modified-release methylphenidate in ADHD: quality of life, satisfaction with treatment and adherence. Eur Child Adolesc Psychiatry 20(Suppl 2):S257–S265
Sajatovica M, Velliganb DI, Weidenc PJ, Valensteind MA, Ogedegbee G (2010) Measurement of psychiatric treatment adherence. J Psychosom Res 69:591–599
Sinzig JK, Döpfner M, Plück J, German Methylphenidate Study Group (2004) Lassen sich hyperkinetische Auffälligkeiten am Nachmittag durch eine Morgengabe von Methylphenidat Retard vermindern? Z Kinder Jugendpsychiatr Psychotherapie 32:225–234
Sinzig J, Döpfner M, Lehmkuhl G, German Methylphenidate Study Group (2007) Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 17:421–432
Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, Barkley R, for the ADHD Transition Phase Working Group (2012) Lifespan persistence of ADHD: The life transition model and its application. J Clin Psychiatry 73(2):192–197
von Elm E, Altman DG, Egger M et al (2008) Strengthening the reporting of observational studies in epidemiology (STROBE-) statement. leitlinien für das berichten von Beobachtungsstudien. Der Internist 6:688–693
Weltgesundheitsorganisation (WHO) (1991) Internationale Klassifikation psychischer Störungen: ICD-10. 1. Aufl. Hans Huber-Verlag, Göttingen
Acknowledgments
The study was funded by Medice.
Conflict of interest
Esther Sobanski has received consulting income and research support from Eli Lilly, Medice, Novartis and Shire and research support from the German Research Foundation, German Ministry of Education and Research. She receives royalties from books by Medizinisch Wissenschaftliche Verlagsgesellschaft and Dansk Psychologisk Forlag. Manfred Döpfner received consulting income and research support from Lilly, Medice, Shire and Vifor and research support from the German Research Foundation, German Ministry of Education and Research. He receives royalties from books and psychological tests published by Hogrefe, Beltz and Huber. Claudia Ose has received an unrestricted educational grant for statistical and administrative support from Medice. Roland Fischer is the medical director of Medice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sobanski, E., Döpfner, M., Ose, C. et al. A non-interventional study of extended-release methylphenidate in the routine treatment of adolescents with ADHD: effectiveness, safety and adherence to treatment. ADHD Atten Def Hyp Disord 5, 387–395 (2013). https://doi.org/10.1007/s12402-013-0113-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-013-0113-y