Abstract
Although maternal smoking during pregnancy has been shown to be associated with an increased risk of offspring attention-deficit/hyperactivity disorder (ADHD) in Western countries, there is no empirical evidence in non-Caucasian. Purpose of the present study is to examine the relationship between maternal smoking during pregnancy and offspring ADHD in Japanese population. A case–control study design was adopted. A total of 90 pairs of children with ADHD and mothers as well as 270 corresponding control pairs were recruited throughout the study period. A psychiatrist interviewed all the mothers of children with ADHD and control children and elicited information regarding their lifestyles during pregnancy, including active and passive smoking or drinking habits, as well as psychosocial and perinatal factors. Diagnosis of ADHD was made by each physician in charge according to DSM-IV diagnostic criteria. Logistic regression analysis was used to calculate odds ratios (OR) and 95% confidence intervals (CI) with adjustments for other possible confounding factors. Maternal active smoking during pregnancy was associated with an approximately twofold increased risk of offspring ADHD, even after adjusting for socioeconomic and perinatal confounding factors (OR 1.8 95% CI 0.9–3.6). However, the association was obviously attenuated when factors regarding parental psychopathological vulnerability were controlled (OR 1.3 95% CI 0.6–2.9). On the other hand, maternal passive smoking during pregnancy failed to show any material association with ADHD. These results suggested that a significant part of the association between maternal smoking during pregnancy, and ADHD might be explained by genetic factors including parental psychopathological vulnerability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is characterized by inattentiveness and/or impulsiveness and hyperactivity, factors which are inappropriate to a patient’s age or developmental stage. Although the mechanism leading to the onset of the disease is still unclear, this condition seriously hinders children’s social or learning capabilities.
Previous studies in Western countries, especially the USA, regarding the epidemiological aspects of ADHD, such as prevalence, male/female ratio, and etiology have been conducted. This is not the case in Japan in part because operational diagnostic criteria such as DSM-IV, which is indispensable for diagnosing ADHD, have been widely used for a longer period in Western countries than in other regions. However, many of these epidemiological issues still remain unclear mainly due to the changes in diagnostic criteria even in the West.
While epidemiological evidence regarding the etiology of ADHD is also insufficient, several factors have been noted as possible risk factors for ADHD. The risk of developing ADHD is strongly influenced by both genetic and environmental factors (Coghill et al. 2008). Candidate gene association studies to identify genetic markers of ADHD have been reported, and a variety of gene variants, including polymorphisms of dopamine-related genes such as DRD4 or DAT (DiMaio et al. 2003; Brookes et al. 2008) were shown to be associated with the risk of ADHD. At the same time, the emerging literature has also implicated a number of environmental risk factors, including pre- or perinatal complications such as maternal smoking or drinking during pregnancy as well as psychosocial vulnerabilities (Linnet et al. 2003). In particular, prenatal exposure to nicotine is probably causing direct teratogenic effects (Paz et al. 2007), and evidence has been accumulated which identified maternal smoking during pregnancy as a possible risk factor of offspring ADHD (Milberger et al. 1996, 1998; Thapar et al. 2003; Schmitz et al. 2006).
In addition, the findings on such genetic and environmental risk factors are consistent with the hypothesis that ADHD is a complex disorder influenced by the interaction of multiple etiologic factors (Coghill et al. 2008; Banerjee et al. 2007).
From this point of view, the prior studies regarding environmental risk factors of ADHD lacked two critical elements. First, as mentioned earlier, since almost all previous epidemiological studies regarding ADHD have been conducted in Western countries, the corresponding problems of ADHD in non-Western ethnic or cultural subgroups have been less thoroughly investigated. For instance, Polanczyk et al. (2007) reported a significantly lower pooled ADHD prevalence estimate in African and Middle-East studies than in North American ones, and referred to a role of cultural factors in the etiology of ADHD. Replication of the adverse effects of maternal smoking during pregnancy on ADHD demonstrated by recent epidemiological studies should also be ascertained in various non-Caucasian ethnical populations.
Second, as suggested by Linnet et al. (2003), much of the previous research regarding maternal smoking during pregnancy did not take account of other confounding factors, such as genetic and dietary factors, maternal mental stress during pregnancy, and socioeconomic problems. Especially, parental psychopathology, such as ADHD, depression or anxiety should be rigorously controlled when studying the relationship between maternal smoking during pregnancy and ADHD (Langley et al. 2005).
In Japan, ADHD was selected by the Ministry of Science and Culture as a target disease deserving of special support starting in 2007, together with learning disorders and high-functioning autism, with the social goal of increasing interest in ADHD (Tsuge 2007). On the other hand, while only the concept of the disorder has become popular in the clinical or educational disciplines, the basic epidemiological evidence remains seriously deficient. However, such epidemiological concepts should enlist the efforts of all relevant institutions, such as welfare, education, judicature, and medicine in addressing ADHD in children.
To realize the above-mentioned goal, we evaluated the relationship between maternal smoking during pregnancy and offspring ADHD using a case–control design. To the best of our knowledge, this is the first epidemiological study to deal with that topic in Japan.
Methods
Cases and controls
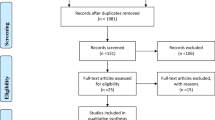
Eligible cases were comprised of pairs of outpatients aged 6–15 years who, along with their mothers, received periodic medical treatment for ADHD, from March 2006 to December 2008 at seven hospitals in the Kinki area of Japan. While five hospitals were continuously monitored throughout the study period, one hospital was followed for the initial 12 months, and another for the last 16 months of the study period.
In each hospital, experienced psychiatrists or pediatricians diagnosed ADHD according to the diagnostic criteria of DSM-IV, with full consideration of both parents’ and teachers’ evaluations. Except for two institutions where physicians in charge directly investigated (n = 16), after a brief introduction by the physicians in charge of the patients with ADHD, the first author (K.Y) met their mothers, and explained the study contents in detail. All the participant mothers then gave written informed consent. There were 110 candidate patients with ADHD during the study period. Six mothers could not be contacted, and 12 others refused to participate. Two mothers were excluded due to a history of schizophrenia, which might have negated the reliability of the interview. Thus, a total of 90 pairs of patients with ADHD and their mothers remained for the analysis.
Controls were comprised of pairs of patients aged 6–15 years and their mothers who had undergone a check-up for mild physical disorders at three core hospitals in the region between September 2005 and November 2008. The eligible controls were originally restricted to children aged 6–12 years but were extended to those aged 6–15 in June 2006. We excluded patients with a history of congenital diseases, malignant tumors, neurological or mental disorders, as well as those who were strongly suspected of these disorders along with any patients whose daily activities were restricted by their physicians beforehand. Control pairs were also recruited from among female workers at the collaborating hospitals and others affiliated with the central research institution. The job categories of the former included nurses, licensed cooks, clerks, and charwomen. The latter were comprised of women such as residents or temporary employees of the institution. If these mothers (except those of clinic patients) had several children aged 6–15 years, information was mainly elicited about the eldest child. If there was still enough time for the interview, inquiries were also made about their younger children.
As with the interviews of mothers of ADHD cases, the first author (K.Y) met the mothers of the control children after a brief introduction by the physicians in charge, and written consent was obtained. The interviews were conducted when it was most convenient for the interviewer. Except for two mothers who refused to participate in the study, all the others agreed to be interviewed. Subjects who were suspected by the interviewer to have ADHD (total score of 17 or more by the rating scale described) were excluded (n = 20). This left a total of 270 pairs of mothers and their children who were eligible to be enrolled in the study.
Interview survey
A questionnaire was used to ascertain demographic characteristics as well as maternal lifestyle factors during pregnancy, such as parental educational background, family annual income, family structure, medical history of parental mental disorders (schizophrenia, depression, alcohol dependence, personality disorder), maternal mental stress, active smoking, passive smoking, and drinking habits during pregnancy, maternal tendency for ADHD, and the severity of the children’s ADHD. Information regarding children’s dietary habits related to foods rich in iron was also obtained. Maternal mental stress during pregnancy was assessed by one simple question ‘To what extent were you bothered by psychological problems during pregnancy?’, which was a modified version of the question developed by Fukuhara and Suzukamo (2004).
A maternal childhood history of ADHD symptoms was assessed using the Wender Utah Rating Scale (WURS). The items on the WURS include indications of mood and learning problems in addition to classic ADHD symptoms. The 25 items in this scale were translated with confirmation by a back-translated procedure (Satake et al. 2004). Five degree points ranging from 0 to 4 were assigned to answers from ‘not applicable’ to ‘always applicable’.
Iron deficiency has been suggested as a possible contributing cause of ADHD (Konofal et al. 2004, 2008). Children’s intake of those foods with a high iron content was evaluated by the following procedure. We chose 12 kinds of common foods rich in iron, based on data from the list of ingredients, fifth edition with a digest version (Kagawa 2003). Frequencies of the intakes of such foods by the children during one recent year were ascertained by the questionnaire, and the iron intake volume (shown as mg per month) was calculated for each child.
The severity of the children’s ADHD symptoms was evaluated by the ADHD Rating Scale IV, Japanese version (RS-IV-J). Points 3, 2, 1, and 0 corresponded to the answers ‘very often,’ ‘often,’ ‘sometimes,’ and ‘hardly ever,’ respectively. It was reported that a range of 14–16 points assessed by parents indicated the borderline zone of ADHD (Yamasaki 2003). Consequently, those control children scored as 17 or more by RS-IV-J were suspected of having ADHD and were therefore excluded from the analyses.
Statistical analyses
Differences in socioeconomic, lifestyle, perinatal, and genetic or clinical factors between cases and controls were statistically tested by χ2 test, unpaired t-test, or analysis of covariance. Logistic regression analysis was used to obtain odds ratios (OR) and 95% confidence intervals (CI) with adjustments for children’s gender and other potential variables. OR and 95% CI were used to examine the association of maternal smoking during pregnancy with children’s ADHD.
In the logistic regression analysis, independent variables were indicator variables representing the categories of children’s gender, family income, parental history of mental disorders, maternal smoking, drinking, and mental stress during pregnancy, maternal tendency of ADHD, birth weight, pregnancy-induced hypertension, and children’s iron intake. The multivariate regression models were composed of the following three expressions; sex-adjusted model, multi-adjusted model except for genetic factors, and fully adjusted model. Families with annual incomes of 4,000,000 Japanese yen (approximately 40,000 US dollars) or less were relegated to the low earning group. A parental history of mental disorders was defined as present if at least one of the parents had a history of depression, alcoholic dependence, and personality disorder, or a father with a history of schizophrenia.
As for smoking habits during pregnancy, mothers were asked whether they were lifetime non-smokers, former smokers, or pregnant smokers. The mothers were regarded as smokers if they had smoked everyday for more than 1 month. Those who had stopped smoking when they became aware of their pregnancy were regarded as pregnant smokers. The regression model, which distinguished those who stopped smoking upon recognition of their pregnancy from those who continued smoking after such recognition, was also used. The total number of cigarettes smoked during pregnancy was calculated for pregnant smokers, and dichotomized at a mean value (1,750 cigarettes). Non-smoking mothers who shared space with smokers in a family or workplace during their pregnancy were classified as passive smokers.
Regarding alcohol use, the mothers reported whether they were lifelong non-drinkers, former drinkers, or pregnant drinkers. Maternal mental stress during pregnancy was divided into the following three levels: very low, low or middle, and high or very high. A maternal tendency for ADHD was included in the regression model as a continuous variable. Birth weight was divided into two categories, with less than 2,500 g regarded as a low birth weight. Children with iron intake of less than 200 mg/month were categorized into the low-intake group.
P values (two-sided) less than 0.05 were considered statistically significant. All computations were performed using the SAS software package version 9.1.3 (SAS Institute, Inc., Cary, NC, USA).
Reliability assessments of relevant measures
Reproducibility by the test–retest method in each scale was assessed using mailed sub-samples of 73 control mothers over an interval of 3–6 months (73/111, response rate; 66%). For categorical variables such as smoking or drinking during pregnancy, simple κ coefficients and their 95% CI were calculated, whereas intraclass correlation coefficients were calculated for continuous variables such as scores assessed by WURS or RS-IV-J. The main results were as follows; simple κ coefficients (95% CI) were 0.85 (0.72–0.99) for active smoking, 0.70 (0.52–0.88) for passive smoking, 0.64 (0.43–0.85) for drinking, 0.61 (0.42–0.78) for mental stress, and 0.40 (0.18–0.62) for gestational weeks from the time when pregnancy had been recognized as a categorical variable (less than 8 weeks or not). Intraclass correlation coefficients were 0.79 for WURS score, 0.65 for RS-IV-J score, 0.96 for birth weight, 0.16 for gestational weeks from when pregnancy had been recognized as a continuous variable, and 0.51 for children’s iron intake.
The internal consistency of WURS and RS-IV-J items was also evaluated using Cronbach’s α coefficients in the control mothers. The α coefficients of WURS and RS-IV-J items were 0.89 and 0.78, respectively.
Ethical considerations
The questionnaires used in the present survey were completed under anonymous conditions so that the participating subjects could not be identified. All the participant mothers gave written informed consent for participating in the study after a detailed explanation including items such as study objective, voluntary participation, and principal investigator’s contact address. The overall protocol of the present survey was approved by the Research Ethics Committee of Wakayama Medical University, as well as by that of each collaborating institution as the occasion demanded.
Results
Table 1 shows the distributions of familial, psychosocial, perinatal, and children’s dietary factors between cases and controls. There were no statistically significant differences in mean ages (SD) of the case and control children as well as those of the mothers. Ninety-one percent of the case children were males, whereas the male proportion in the controls was 47%. Sex-adjusted scores of RS-IV-J were statistically significantly higher in cases than in controls. The mean gestation period since pregnancy had been recognized in the entire sample was 8.0 weeks (SD 2.6). A total of 50% of the case children had been administered periodical medication of methylphenidate during the final 6 months. Proportions of the first-born children did not differ between cases and controls. Proportion of smoking mothers during pregnancy in controls was 17.4%, which was similar to that of twenties women in Japan reported by the national survey (Office for Life-Style Related Disease Control General Affairs Division Health Service Bureau 2007).
As for socioeconomic factors, case children showed a higher proportion of absent real fathers than the controls, whereas parental educational background and family income showed no material differences between the two groups. The proportions of maternal mental stress during pregnancy and a parental history of mental disorders were statistically significantly higher in cases than in controls, a maternal tendency for ADHD was also stronger in cases. Interestingly, children’s iron intake was significantly lower in cases than in controls.
The association between maternal active smoking during pregnancy and ADHD was presented according to the three regression models in Table 2. Maternal smoking during pregnancy tended to be associated with an approximately twofold increased risk of ADHD in sex-adjusted and multi-adjusted models, except for factors related to parental psychopathology. However, these harmful effects were evidently attenuated once those factors were included in the regression model.
Table 3 shows the association between maternal active smoking during pregnancy and ADHD, with pregnant smokers divided into two categories. Those who quit smoking upon recognition of pregnancy showed a similar risk of their children having ADHD as those who continued smoking even after recognition of their pregnancy. Both groups showed a two or two and a half-fold increased risk of ADHD, but again, the risks were diminished when parental psychopathological factors were accounted for in the regression model.
The dose–effect relationships between maternal smoking during pregnancy and ADHD were also evaluated. The same pattern of results was obtained in this analysis. Although the dose–effect relationships were observed in the former two models, they disappeared in the third model, which included the factors of parental psychopathological vulnerability (data not shown).
The relation of maternal passive smoking during pregnancy to ADHD was shown in Table 4, in which no material association with ADHD was detected in any of the three models.
Discussion
Maternal active smoking during pregnancy was associated with an approximately twofold increased risk of ADHD. Such a risk was also observed even in mothers who had quit smoking upon recognition of their pregnancy. However, the association was apparently attenuated when parental psychopathological factors were taken into account. On the other hand, maternal passive smoking during pregnancy failed to show any material associations with offspring ADHD. The proportion of children with a susceptibility to ADHD (20/290, 6.9%) was slightly higher than the worldwide-pooled prevalence (5.3%, Polanczyk et al. 2007), which might be due to using only one informant (mothers) for ADHD. To the best of our knowledge, this is the first epidemiological study to investigate the relationship between maternal smoking during pregnancy and ADHD in a Japanese population.
Ruling out the autism spectrum of pervasive developmental disorders (PDD) is one of the important steps in any epidemiological studies of ADHD. However, this diagnostic procedure often demands high clinical skills of physicians. Compared with the large attribution of genetic factors noted in the etiology of PDD (Moura et al. 2008), several environmental factors have been thought to play an important role in causing ADHD (Linnet et al. 2003; Banerjee et al. 2007; Lehn et al. 2007). Although PDD was ruled out as completely as possible during the clinical settings in the present survey, application of the exclusion criteria still might differ according to the opinion of each physician, especially for PDD not otherwise specified (PDDNOS). On the other hand, there has been some criticism of these exclusion criteria from various clinical viewpoints (Barkley 2006; Gillberg 2006), and the diagnoses of these two disorders could change mutually through the developmental process of the children. In addition, genetic and environmental risk factors regarding developmental disorders are difficult to clearly distinguish. For instance, although maternal mental stress during pregnancy is an environmental factor usually regarded as an external stressor, it can also be identified as a genetic factor since mothers with a genetic predisposition to psychological vulnerability might perceive greater mental stress during their pregnancies than those without it. In any event, there is no doubt that a wide variety of factors are involved in the pathogenesis by means of which clinical ADHD symptoms were formed.
As mentioned in the introduction, maternal smoking during pregnancy has been shown to be a possible environmental risk factor for ADHD in several epidemiological studies. However, since those studies were mainly conducted in United States, the issue of reproducibility in non-Western ethnic populations has yet to be addressed. The present results, which have suggested an approximately twofold increased risk of ADHD from maternal smoking, were consistent with those of a meta-analysis of Western epidemiological studies conducted by Langley et al. (2005). Furthermore, we found that smoking in the early period of pregnancy was shown to increase the risk of ADHD even if the mother had quit upon the recognition of her pregnancy, a finding that was also consistent with a previous study (Knopik et al. 2005). On the other hand, the risks were not significantly increased when adjusting for the other confounding factors, especially parental psychopathological factors. Previous studies that measured parental psychopathology have included the effects of existing maternal depression, perceived mental stress during pregnancy, and other parental psychopathologies, but with mixed results regarding the relationship between maternal smoking during pregnancy and offspring ADHD or behavioral problems (Knopik et al. 2005; Maughan et al. 2004; Rodriguez and Gunilla 2005; Mick et al. 2002). Taken together, these results suggest that the relationship between maternal smoking and ADHD may be explained by the possibly confounding effects of parental psychopathological vulnerability, they also provide supportive evidence that the majority of ADHD cases may be attributable to heritability (Banerjee et al. 2007; Biederman 2005).
The present study included several methodological limitations mainly due to a sampling bias caused by using hospital-referred subjects. First, both the children with ADHD and control children in the present study were outpatients referred to hospitals. In general, because mothers who visit a hospital periodically seeking help with their children’s ADHD symptoms tend to have a high regard for health promotion, they are less likely to smoke, especially during pregnancy. Thus, the observed association between maternal smoking and ADHD may be underestimated. Second, smoking mothers may tend to have more severe psychosocial problems than non-smokers, such as divorce or the burden of rearing the children alone due to paternal abandonment. They are also considered to be less likely to consult a doctor for their children’s ADHD, resulting in an underestimation of the adverse effects of maternal smoking on ADHD. In this connection, it has been reported that patients with mental disorders have higher rates of smoking than the general population (Leonard et al. 2001; Williams and Ziedonis 2004; Salin-Pascual et al. 2003; Kollins et al. 2005). If the mothers of children with ADHD suffer such disorders, the observed increasing crude ORs of maternal smoking may have been due to maternal mental disorders including ADHD. This is plausible given that the significant association between maternal smoking during pregnancy, and ADHD was diminished when parental psychopathology was taken into account.
Third, the interviewer who assessed the maternal smoking habits during pregnancy was not blind to the clinical outcome as well as the objectives and hypotheses of the study. However, it should be reinforced that there were no differences between case and control in other variables (drinking during pregnancy or birth weight) that could also be associated with ADHD. Thus, it seems unlikely that the interviewer have only been biased regarding the variables of mental stress or smoking during pregnancy.
Another critical limitation of the present study is the inaccuracy of many mothers in recalling the time when they noted their pregnancy. Although the results of reproducibility reached acceptable levels for maternal smoking habits during pregnancy, they were extremely unsatisfactory regarding the gestation weeks when pregnancy had first been recognized. Since the total cigarette consumption during pregnancy was calculated based on the time when the mothers became aware of their pregnancy, the resulting calculations were lacking in sufficient reliability. The fact is that we could not reliably ascertain the dose–response relationship between maternal active smoking and ADHD, and this might be related to the negative findings on the connection between maternal passive smoking during pregnancy and ADHD. The measure of passive smoking might be too broad to detect precise associations. This failure to detect dose–response relationships is mainly due to a methodological limitation, i.e., maternity health-record documentation was not available in the current interview settings.
Recently, ADHD has been considered to result from a complex interplay between genetic and environmental factors including maternal smoking (gene–environment interaction) (Knopik 2009) as well as common diseases such as cancer or cardiovascular disease. A few studies have been conducted that examined the gene–environment interaction on ADHD at the molecular level, but with mixed results (Neuman et al. 2007; Brookes et al. 2006; Becker et al. 2008; Altink et al. 2009). Although these studies mainly evaluated environmental factors such as maternal smoking or drinking during pregnancy, our current findings suggested that a large part of the association between such maternal lifestyle during pregnancy and ADHD might be explained by genetic vulnerability. Further research focused on various gene–environment interactions on ADHD as well as mechanisms underlying the onset of the disease should be conducted to enhance our understanding of the etiology of ADHD which involves a variety of environmental and genetic factors.
In conclusion, our study brought to light some suggestions of a relationship between ADHD and maternal active smoking during pregnancy, but the current sample size may prevent any conclusive inference. Future studies involving larger control and case populations, precisely and uniformly defined clinical classification of ADHD and better exposure histories will undoubtedly lead to a more thorough understanding of the role of maternal active smoking in ADHD development.
References
Altink ME, Slaats-Willemse DI, Rommelse NN, Buschgens CJ, Fliers EA, Arias-Vásquez A, Xu X, Franke B, Sergeant JA, Faraone SV, Buitelaar JK (2009) Effects of maternal and paternal smoking on attentional control in children with and without ADHD. Eur Child Adolesc Psychiatry 18:465–475
Banerjee TD, Middleton F, Faraone SV (2007) Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr 96:1269–1274
Barkley RA (2006) Comorbid disorders, social and family adjustment, and subtype. In: Barkley RA (ed) Attention-deficit hyperactivity disorder, 3rd edn. The Guilford Press, New York, pp 184–218
Becker K, El-Faddagh M, Schmidt MH, Esser G, Laucht M (2008) Interaction of dopamine transporter genotype with prenatal smoke exposure on ADHD symptoms. J Pediatr 152:263–269
Biederman J (2005) Attention-deficit/hyperactivity disorder: a selective overview. Biol Psychiatry 57:1215–1220
Brookes KJ, Mill J, Guindalini C et al (2006) A common haplotype of the dopamine transporter gene associated with attention-deficit/hyperactivity disorder and interacting with maternal use of alcohol during pregnancy. Arch Gen Psychiatry 63:74–81
Brookes KJ, Xu X, Anney R et al (2008) Association of ADHD with genetic variants in the 5′-region of the dopamine transporter gene: evidence for allelic heterogeneity. Am J Med Genet B Neuropsychiatr Genet 147B:1519–1523
Coghill D, Rohde LA, Banaschewski T (2008) Attention-deficit/hyperactivity disorder. In: Banaschewski T, Rohde LA (eds) Biological child psychiatry. Recent trends and developments. Advances in biological psychiatry. Karger Press, Basel, pp 1–20
DiMaio S, Grizenko N, Joober R (2003) Dopamine genes and attention-deficit hyperactivity disorder: a review. J Psychiatry Neurosci 28:27–38
Fukuhara S, Suzukamo Y (2004) Manual of the SF-8 Japanese version. Institute for Health Outcomes & Process Evaluation Research, Kyoto (in Japanese)
Gillberg C (2006) Autism spectrum disorders. In: Gillberg C, Harrington R, Steinhausen HC (eds) A clinician’s handbook of child and adolescent psychiatry. Cambridge University Press, Cambridge, pp 447–488
Kagawa Y (2003) List of ingredients, digest version, 5th edn. Kagawa education institute of nutrition, Tokyo (in Japanese)
Knopik VS (2009) Maternal smoking during pregnancy and child outcomes: real or spurious effect? Dev Neuropsychol 34:1–36
Knopik VS, Sparrow EP, Madden PAF et al (2005) Contributions of parental alcoholism, prenatal substance exposure, and genetic transmission to child ADHD risk: a female twin study. Psychol Med 35:625–635
Kollins SH, McClernon FJ, Fuemmeler BF (2005) Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of adults. Arch Gen Psychiatry 62:1142–1147
Konofal E, Lecendreux M, Arnulf I, Mouren MC (2004) Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 158:1113–1115
Konofal E, Lecendreux M, Deron J et al (2008) Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatr Neurol 38:20–26
Langley K, Rice F, Van Den Bree MBM, Thapar A (2005) Maternal smoking during pregnancy as an environmental risk factor for attention deficit hyperactivity disorder behavior. Minerva Pediatr 57:359–371
Lehn H, Derks EM, Hudziak JJ, Heutink P, van Beijsterveldt TC, Boomsma DI (2007) Attention problems and attention-deficit/hyperactivity disorder in discordant and concordant monozygotic twins: evidence of environmental mediators. J Am Acad Child Adolesc Psychiatry 46:83–91
Leonard S, Adler LE, Benhammou K et al (2001) Smoking and mental illness. Pharmacol Biochem Behav 70:561–570
Linnet KM, Dalsgaard S, Obel C et al (2003) Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: review of the current evidence. Am J Psychiatry 160:1028–1040
Maughan B, Taylor A, Caspi A, Moffitt TE (2004) Prenatal smoking and early childhood conduct problems: testing genetic and environmental explanations of the association. Arch Gen Psychiatry 61:836–843
Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S (2002) Case–control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. J Am Acad Child Adolesc Psychiatry 41:378–385
Milberger S, Biederman J, Faraone SV, Chen L, Jones J (1996) Is Maternal smoking during pregnancy a risk factor for attention deficit hyperactivity disorder in children? Am J Psychiatry 153:1138–1142
Milberger S, Biederman J, Faraone SV, Jones J (1998) Further evidence of an association between maternal smoking during pregnancy and attention deficit hyperactivity disorder: findings from a high-risk sample of siblings. J Clin Child Psychol 27:352–358
Moura PJ, Lombroso PJ, Mercadante MT (2008) Autism. In: Banaschewski T, Rohde LA (eds) Biological child psychiatry. Recent trends and developments. Advances in biological psychiatry. Karger Press, Basel, pp 21–38
Neuman RJ, Lobos E, Reich W, Henderson CA, Sun LW, Todd RD (2007) Prenatal smoking exposure and dopaminergic genotypes interact to cause a severe ADHD subtype. Biol Psychiatry 61:1320–1328
Office for Life-Style Related Disease Control General Affairs Division Health Service Bureau, Ministry of Health, Labor and Welfare, Japan (2007) Smoking status. In: The National Health and Nutrition Survey in Japan, 2005. Ministry of Health, Labor and Welfare, Japan, Tokyo, pp 60 (in Japanese)
Paz R, Barsness B, Martenson T, Tanner D, Allan AM (2007) Behavioral teratogenicity induced by nonforced maternal nicotine consumption. Neuropsychopharmacol 32:693–699
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-regression analyses. Am J Psychiatry 164:942–948
Rodriguez A, Gunilla B (2005) Are maternal smoking and stress during pregnancy related to ADHD symptoms in children? J Child Psychol Psychiat 46:246–254
Salin-Pascual RJ, Alcocer-Castillejos NV, Alejo-Galarza G (2003) Nicotine dependence and psychiatric disorders. Revista de investigación clínica 55:677–693 (in Spanish)
Satake H, Yamashita H, Yoshida K (2004) The family psychosocial characteristics of children with attention-deficit hyperactivity disorder with or without oppositional or conduct problems in Japan. Child Psychiatry Human Dev 34:219–235
Schmitz M, Denardin D, Silva TL, Pianca T, Hutz MH, Faraone S, Rohde LA (2006) Smoking during pregnancy and attention-deficit/hyperactivity disorder, predominantly inattentive type: a case–control study. J Am Acad Child Adolesc Psychiatry 45:1338–1345
Thapar A, Fowler T, Rice F, Scourfield J, van den Bree M, Thomas H, Harold G, Hay D (2003) Maternal smoking during pregnancy and attention deficit hyperactivity disorder symptoms in offspring. Am J Psychiatry 160:1985–1989
Tsuge M (2007) Special support education for students with Asperger’s syndrome. Nippon Rinsho 65:551–555 (in Japanese)
Williams JM, Ziedonis D (2004) Addressing tobacco among individuals with a mental illness or an addiction. Addict Behav 29:1067–1083
Yamasaki K (2003) ADHD-RS-IV Japanese versions. In: Kanbayashi Y, Saito K, Kita M (eds) Japanese guideline for the diagnosis and treatment of attention deficit hyperactivity disorder (ADHD). Jiho Press, Tokyo, pp 48–53 (in Japanese)
Acknowledgments
This work was financially supported by a research grant from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (Grant No. 18590609) and from the Smoking Research Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the Wakayama ADHD Study Group are listed in the Appendix.
Appendix: Members of the Wakayama ADHD Study Group (in each affiliation)
Appendix: Members of the Wakayama ADHD Study Group (in each affiliation)
Nobuyuki Miyai, Kazuhisa Miyashita, Kouichi Yoshimasu † (Department of Hygiene, School of Medicine, Wakayama Medical University), Chikako Kiyohara (Department of Preventive Medicine, Graduate School of Medical Sciences, Kyushu University), Mina Booka, Asumi Higa, Genkichi Izumi, Takaomi Minami, Masakazu Miyawaki, Yuko Tsuda, Yoshinobu Tsuno, Tetsu Yoshimasu (Department of Pediatrics, Social Insrance Kinan Hospital), Shoichi Shibuta, Yuko Shima, Hiroyuki Suzuki, Takashi Takeuchi, Hiroko Togawa, Norishige Yoshikawa (Department of Pediatrics, School of Medicine, Wakayama Medical University), Shogo Kihira (Department of Pediatrics, Arita City Hospital), Eiko Honaga, Hiroshi Sato, Koji Toyonaga, Hinako Yamaguchi (Department of Neuropsychiatry, Osaka City General Hospital), Aki Kohno, Daisuke Nakanishi, Hiromichi Nakashima, Hisami Nishida, Kazuyuki Ohtsuki, Akira Yamamoto, Tomoko Yoshioka (Mie Prefectural Asunaro Hospital for Child and Adolescent Psychiatry), Harumi Kose, Kazuhiro Shinosaki (Department of Neuropsychiatry, School of Medicine, Wakayama Medical University), Hiroshi Yamashita (Department of Neuropsychiatry, Graduate School of Medical Sciences, Kyushu University), Junzo Iida (School of Nursing, Nara Medical University), Yoshiro Ono (Wakayama Prefecture Children and Disabled Persons’ Guidance Center), Toshihiko Yanagawa (School of Health and Nursing Sciences, Wakayama Medical University), Toshiko Juri (Department of Pediatrics, Kainan City Hospital), and Akira Miyamoto (Wakayama Prefectural Nanki Welfare Center).
† Principal investigator.
Rights and permissions
About this article
Cite this article
Yoshimasu, K., Kiyohara, C., Minami, T. et al. Maternal smoking during pregnancy and offspring attention-deficit/hyperactivity disorder: a case–control study in Japan. ADHD Atten Def Hyp Disord 1, 223–231 (2009). https://doi.org/10.1007/s12402-009-0015-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-009-0015-1