Abstract
Attention-deficit/hyperactivity disorder may have substantial impact on family life, peer interactions, and quality of life. Stimulants are recommended as first-line pharmacotherapy for ADHD. OROS® MPH (Concerta®) is a long-acting preparation with duration of effect for up to 12 h. In this 8-week, prospective, open-label, non-interventional trial the impact of therapy with OROS® MPH on functioning in four different areas of life (school, recreation, family life, and peer interaction), severity of disease, and quality of life (QoL) as well as tolerability were investigated under daily routine care. 306 patients, aged 10.2 ± 2.3 years, were either transitioned to OROS® MPH from short-acting, immediate-release MPH (-IR) preparations (n = 231; 75%), or treatment was initiated with OROS® MPH in MPH-naïve patients (n = 75; 25%). In both groups, therapy with OROS® MPH was associated with significant improvements in daily functioning, severity of disease, and QoL. Adverse events (AE) were documented in 160 patients (52.3%). In 95 patients (31.0%) a causal relationship was assessed as at least possible. Four serious AEs were reported in 2 patients and rated as doubtfully related to study medication. Most frequent AEs (≥5% of patients) were insomnia, anorexia, ineffectiveness of medication, and headache. In 12.1% of patients AE led to discontinuation of study participation. Considering the limitations of this non-interventional study, the results refer to the importance of a therapy that covers not only school-time, but also takes other areas of life into account. Initiating treatment with long-acting preparations, such as OROS® MPH in MPH-naïve patients might be a feasible option.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Impact of ADHD on different areas of life and quality of life (QoL)
With a reported prevalence of 4 to 10%, attention-deficit/hyperactivity disorder (ADHD) is the most common neurobehavioural disorder in children and adolescents (American Academy of Pediatrics 2000; Barbaresi et al. 2002; Rappley 2005; Murphy and Barkley 1996; Faraone and Wilens 2003; Kessler et al. 2005). ADHD is recognized as a chronic condition with symptoms appearing in early childhood and an estimated persistence of about 50% into adulthood (Steinhausen 2003; Sobanski and Alm 2004; Murphy and Barkley 1996). Associations have been shown between the disorder and substantial impact upon academic achievements, and also upon important other aspects of the patients’ lives, e.g. peer and family interactions. There are indications for ADHD exerting continuous negative influence on educational and occupational achievements, and also on personality development, including self-esteem and interpersonal relationships, social functioning, driving ability, and quality of life (Hechtman et al. 1984; Gittelman et al. 1985; Mannuzza et al. 1993; Jerome et al. 2006; Escobar et al. 2008). In an 8-year prospective follow-up study, children with ADHD were at significantly higher risk of negative psychiatric, social, legal, academic, and family-functioning outcomes in adolescence than children without ADHD (Barkley et al. 1990). A recent quality of life study comparing children and adolescents with ADHD to a control group demonstrated ADHD patients having significant deficits in all psychosocial domains and more problems with emotional behavioural role-function, behaviour, mental health, and self-esteem (Klassen et al. 2004). In another study comparing male adolescents with ADHD to adolescents with no chronic condition and to adolescents with mobility impairments, adolescents with ADHD reported similar quality of life as adolescents in the mobility impairment group and lower quality of life than those with no chronic condition (Topolski et al. 2004). There is an association of ADHD with family disruption, marital functioning, parental exhaustion and stress, social isolation, increased alcohol consumption, and mental disorders, such as depression and substance-use disorders (Harpin 2005; Johnston and Mash 2001; Podolski and Nigg 2001; Pelham and Lang 1999; Minde et al. 2003). However, possible mechanisms underlying these associations are still unclear.
The relevance of extracurricular activities
Traditionally, academic or school activities have been highlighted as the most important, with concomitant focus on medication during these periods. However, this approach may underestimate the possible importance of non-academic and extra-curricular activities that may contribute to the patient’s personal development. These activities are usually pursued in the afternoon and early evening when the effects of short-acting medications might be fading, depending on medication intake regimes, possibly resulting in re-occurrence of symptoms. Usually in the afternoon and early evening many of the social and recreational activities take place, such as team sports, play, and other social interactions with the patients’ families and peers. Re-occurrence of symptoms during these times of the day may have an influence on family functioning.
Stimulant medication
Stimulant medication is an important cornerstone in the multimodal treatment of ADHD. Current guidelines recommend methylphenidate (MPH) as first line option in pharmacological treatment of ADHD (Brown et al. 2005; Banaschewski et al. 2006; Taylor et al. 2004; Stein and Perrin 2003). MPH markedly and rapidly reduces the overt clinical manifestations of ADHD. In addition, MPH positively influences the quality of social interactions and decreases aggressiveness (Taylor et al. 2004).
As for all patients with persistent disorders, adherence to medication is also challenging for patients with ADHD. Several factors have been identified to influence on adherence: tolerability plays an important role, but also the medication’s effects on social interactions, quality of life and the satisfaction with therapy perceived by patients, their parents and physicians, or stigmatization felt when having to take medication at school. If the degree of satisfaction with a therapeutic option is high, a positive impact on compliance can be expected. Good compliance is likely to enhance therapeutic outcome (Swanson 2003).
Due to its short half-life, immediate-release methylphenidate (MPH-IR) requires dosing 1–3 times a day, which might be inconvenient for the patient. Long-acting formulations have been developed that allow once-daily dosing. The possible advantages of long-acting drugs may be (i) a potential reduction of stigma at school, (ii) improved adherence, and (iii) possibly reduced risk of misuse. Current international guidelines for the management of ADHD, thus, state that, besides short-acting formulations, long-acting formulations should be available and used (Banaschewski et al. 2006). The smoother pharmacokinetic profile of long-acting agents may also provide a more consistent medication effect. A main countervailing argument is cost (Banaschewski et al. 2006). This may, however, be outweighed by a reduction in cost produced by compliance problems and resulting in insufficient effectiveness of medication (Swanson 2003).
Currently, treatment with MPH is usually initiated with immediate release formulations for dose-finding. Once therapy has been successfully initiated, patients may be transitioned to long-acting formulations. There is growing evidence that it may also be suitable to start therapy by using long-acting formulations initially without compromising safety and tolerability (Swanson et al. 2000). This would avoid the need for switching medication shortly after stimulant therapy has been successfully established in the patient.
OROS® MPH
OROS® MPH (Concerta®) is a long-acting formulation of MPH which uses Osmotic Release Oral System (OROS®) technology to produce an ascending MPH plasma profile with a duration of action of about 12 h (Modi et al. 2000). In three short-term, randomized, controlled studies in children, OROS® MPH has been shown to improve behavioural and attentional symptoms of ADHD through a 12-h period. Its efficacy has been shown to be comparable to that of MPH-IR dosed three times daily (Wolraich et al. 2001; Pelham et al. 2001; Swanson et al. 2004). In addition, long-term safety and effectiveness of OROS® MPH have been demonstrated in two open-label studies lasting 9 months and 24 months (Wilens et al. 2005; Wolraich 2003).
The effects of therapy with OROS® MPH on parents’ and physicians’ satisfaction as well as the effects on quality of life have been investigated in a prospective, open-label study over 3 weeks in Germany; 213 patients with ADHD previously treated with MPH-IR were switched to OROS® MPH 18, 36, or 54 mg. Primary criteria of effectiveness were the IOWA-Conners inattention/overactivity-subscale and a global assessment of efficacy. Secondary criteria of effectiveness included the IOWA-Conners oppositional/defiant-subscale, peer interaction rating, and investigators’ global assessment. Switching symptomatically stable patients from MPH-IR to OROS® MPH resulted in a significant improvement of ADHD-symptoms in the after-school time. At school, OROS® MPH showed to be at least as effective as MPH-IR. Tolerability was good with a trend for improved sleep and appetite. Caregivers and investigators did reflect a high degree of satisfaction with the medication (Heger et al. 2006). In an 8-week, open-label study, 147 patients were randomized to therapy either with MPH-IR tid or OROS® MPH once daily after a minimum 3-day wash-out phase. OROS® MPH showed statistically significant superiority to MPH-IR in remission rate, and severity of ADHD and ODD symptoms (Steele et al. 2006a, b).
The objectives of the present study were to assess tolerability of OROS® MPH therapy, as well as its possible effectiveness in children and adolescents aged 6 to 14 years under the conditions of paediatric daily routine treatment. Special attention was paid to social functioning in four important areas of life (school, recreation, family life and peer interaction), to the severity of disease and quality of life.
Methods
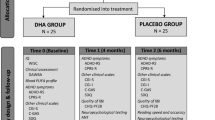
The design of this prospective, open-label, single-arm, non-interventional trial with OROS® MPH conducted in Germany (42603ATT0001/GER-CON-1) attempted to reflect everyday practice in paediatric care. The study was approved by the International Ethics Committee of the University of Freiburg (Germany). This study was conducted in accordance with the ethical principles that have their origin in the declaration of Helsinki, with the “recommendations for the planning, implementation, and evaluation of observational studies with medicinal products” of the Federal Institute for Drugs and Medical Devices (BfArM) dated 12th November 1998 and the “notice to marketing authorization holders—pharmacovigilance guidelines” issued by the European Agency for the Evaluation of Medicinal Products (EMEA). Clinical monitors performed on-site visits and checked patient record forms regarding completeness and plausibility. Selection criteria were: male and female patients (i) aged 6–14 years, (ii) with a diagnosis of attention deficit hyperactivity disorder according to ICD-10, (iii) in whom the initiation of therapy with OROS® MPH or a transition from short-acting MPH-IR to OROS® MPH was medically indicated. This indication was left at the sole discretion of the treating physician and was not defined in more detail or further questioned in the documentation file. The patients were allowed to be pre-treated with MPH-IR preparations once to thrice daily. No further information about the dosage or dosing regimen of this MPH pre-treatment was captured in the documentation file. Due to the nature of a non-interventional trial, diagnosis and treatment were also at the discretion of the treating physician. Neither standardized diagnostic procedures nor a pre-defined titration scheme were performed. No specification for the transition period from MPH-IR to OROS® MPH was made. A washout period was not required. It was recommended to follow the Summary of Product Characteristics (SmPC) and to keep dosage within the approved scope of 18–54 mg of OROS® MPH per day.
The duration of the observation was 8 weeks. Assessments were scheduled for day 0 (baseline, start of therapy with OROS® MPH, visit 1), week 1 (visit 2), week 2 (visit 3), and week 8 (or at the time of premature discontinuation, if applicable, visit 4/endpoint), respectively. No criteria for premature discontinuation were specified, and the decision to discontinue a patient from the study was the sole decision of the treating physician.
Criteria for evaluation
All criteria for evaluation should have been easy to use in the framework of paediatric daily routine care and should not require special rater training. Primary outcome measure was the change in functioning in four areas of life (school, recreational area, family life, and peer interaction). Criteria for effectiveness used non-validated, simplified scales, such as ratings of therapy effects on 4 areas of life (school, recreational area, family life, and peer interaction), all on a categorical scale from 1 = ‘very good’ to 5 = ‘very bad’ at all visits, ratings of changes in quality of life according to an interview with the parents, “How would you describe the influence of treatment on the family life compared to baseline?” on a categorical Likert scale from 1 = ‘much improved’ to 5 = ‘much worse’ at visits 2, 3, and 4, and global ratings of effectiveness and parents’ satisfaction, each on a categorical scale from 1 = ‘very good’ to 5 = ‘very bad’ at visit 4 and validated scales, such as the Clinical Global Impression, Severity and Change (CGI and CGI-C) scales at visits 1 and 4. The entries of CGI were coded as follows: 0 = ‘cannot be judged’; 1 = ‘no disease’; 2 = ‘borderline ill’; 3 = ‘mildly ill’; 4 = ‘moderately ill’; 5 = ‘markedly ill’; 6 = ‘severely ill’; 7 = ‘extremely severe ill’. The change in clinical global impression (CGI-C) was coded as follows: 0 = ‘cannot be judged’; 1 = ‘very much improved’; 2 = ‘much improved’; 3 = ‘minimally improved’; 4 = ‘unchanged’; 5 = ‘minimally worse’; 6 = ‘much worse’; 7 = ‘very much worse’.
Criteria for evaluation of tolerability were measuring of weight, BMI, and vital signs (blood pressure, pulse frequency), documentation of adverse events, ratings of quality of sleep and appetite on categorical Likert scales from 1 = ‘very good’ to 5 = ‘very bad’ at all visits, as well as the documentation of tics at visits 1 and 4. All ratings were performed by the treating physician who was asked to document the current symptomatology at the time of rating. Bases for this rating were the physician’s clinical observation and the caregivers’ report. The study design and data collection are outlined in Table 1.
Post-hoc analyses
To answer the question if initial therapy with OROS® MPH in MPH-naïve patients shows comparable results as the transition from MPH-IR, two subgroups (patients without previous MPH medications/MPH-naïve patients = initial treatment and patients with previous MPH medication = switch treatment) were examined separately in a post-hoc analysis. There was no further differentiation of the pre-treatment regimen possible. In a further post-hoc analysis, the response rate (defined as CGI-C ≤ 2, meaning at least ‘much improved’ at week 8) and the remission rate (defined as CGI ≤ 2, meaning not ill or borderline ill at week 8) were calculated. Another post-hoc analysis aimed at identification of explanatory variables for the changes in rating of different areas of life by means of regression analysis.
Statistical methods
Statistical analyses were based on the intention-to-treat (ITT) population. The last value after start of treatment was calculated according to the last observation carried forward (LOCF) method. Differences between baseline value and the last score in the efficacy variables were analysed with Wilcoxon’s test. All statistical tests were exploratory in nature. Two-sided p-values were reported; p-values contain no adjustment for multiple testing. Regression analysis was used post-hoc to investigate the effect of a set of explanatory variables on the changes in rating of different areas of life. For every area a separate model was analysed. The dependent variables were the differences in rating of functioning in the areas of school, recreation, family, and peers. Explanatory variables were group, gender, age, duration of disease, CGI at baseline, and the incidence of concomitant diseases. Evaluation was performed using the software package SAS 9.1.3.
Results
Demographics
As much as 313 CRFs from 79 centres were available. After exclusion of 7 patients in whom no relevant data about efficacy and safety were documented, the ITT-population comprised 306 patients (=safety set) from 76 study centres. Data from these 306 patients were analysed; 246 (80.4%) patients were male, and the mean age ± SD of the patients at baseline was 10.2 ± 2.3 years. There were no relevant differences between the switch treatment and the initial treatment groups (mean age ± SD in switch treatment group was 10.3 ± 2.3 and 9.7 ± 2.2 in initial treatment group; Table 2).
Diagnoses
The most frequent ICD-diagnoses were F90.0—‘Disturbance of activity and attention’ (72.5%) and F90.1—‘Hyperkinetic conduct disorder’ (34.3%). Mean duration ± SD of the disorder from diagnoses at baseline was 2.2 ± 2.0 years; 118 patients (38.6%) were represented with one to three concomitant disorders. Most frequent concomitant disorders were ‘Conduct Disorder’ in 25.5%, and ‘Conduct Disorder with Oppositional Defiant Disorder’ in 24.2% of patients. ‘Anxiety Disorders’ and ‘Obsessive–Compulsive Disorders’ were less frequent (5.6% and 1.3%, respectively [multiple answers could be stated] Table 2).
Prior and concomitant therapy
In 75 patients (24.5%) treatment was initiated with OROS® MPH (initial treatment group), whereas 231 patients (75.5%) were switched to OROS® MPH from MPH-IR preparations (switch treatment group). About half of the patients (49.7%) had only previous MPH medication; 25.8% of patients had previous as well as concomitant MPH medication; 19.0% had neither previous, nor concomitant MPH medication, and 5.6% of patients had only concomitant MPH medication. No further information on the pre- or concomitant MPH treatment regimen was available. At baseline, there were 100 patients (32.7%) with one or two additional non-pharmacological treatments (behavioural and ergotherapy or “others not otherwise specified” were documented) in the last 3 months; 283 patients (92.5%) had no changes in additional non-pharmacological treatment during the course of the study. As much as 15 patients (4.9%) had at least one more additional non-pharmacological treatment.
Duration of observation
Mean duration ± SD of observation was approximately 56 ± 16.8 days (range 6–114 days); 43 patients discontinued prematurely (14.1%). The patients could have multiple reasons for premature discontinuation; the most common reason was due to an adverse event (37 patients; 12.1%) and/or due to lack of efficacy (23 patients; 7.5%). Two patients were lost to follow-up, another two were discontinued due to lack of compliance and eight patients gave other reasons for premature discontinuation. Mean duration ± SD of treatment with OROS® MPH was approximately 55 ± 17.1 days (range 6–113 days).
Dosage of medication
The median starting dose of OROS® MPH as well as the median of the last documented dose was 36 mg/day. There was a small increase in the mean dosage ± SD from 29.5 ± 12.7 to 32.8 ± 13.2 mg/day at the end of documentation (whole sample); 227 patients (74.2%) had no changes in dosage during the study. In 22.9% of patients OROS® MPH dose was increased at least once during the study, whereas 6.2% of patients had one dose decrease. Dosage ranged from 18 to 72 mg/day in the whole sample and the switch treatment subgroup, and from 18 to 54 mg/day in the initial treatment subgroup. Patients in the switch treatment subgroup received higher doses at baseline and endpoint than patients in the initial treatment subgroup (31.6 ± 12.7 and 34.4 ± 13.5 mg/day vs. 22.8 ± 10.0 and 27.8 ± 10.8 mg/day, respectively).
Effectiveness results
Therapy effects on functioning in 4 areas of life (school, recreation, family and peer interaction)
At baseline, the situation at school was judged as ‘bad’ or ‘very bad’ in 39.9% of all patients. At the end of the study, the rate of patients with such judgments had diminished to 14.4%. At the same time, the rate of patients with judgments ‘good’ or ‘very good’ had increased from 28.4% to 61.8%. In total, more than half of the patients (56.2%) showed an improvement in their situation at school, 14.1% worsened, and 28.1% remained unchanged.
In 17.6% of all patients, the situation in the recreational area was judged as ‘bad’ or ‘very bad’ at baseline. At the end of the study, the rate of patients with such judgments had diminished to 7.5%. At the same time, the rate of patients with judgments ‘good’ or ‘very good’ had increased from 40.8% to 72.5%. More than half of the patients showed an improvement in the recreational area (50.7%), 13.7% worsened, and 35.3% remained unchanged.
In 28.8% of all patients, family life was judged as ‘bad’ or ‘very bad’ at baseline. At the end of the study, the rate of patients with such judgments had diminished to 11.8%. At the same time, the rate of patients with judgments ‘good’ or ‘very good’ had increased from 31.0% to 71.2%. More than half of the patients showed an improvement in the family area (58.8%), 13.1% worsened, and 28.1% remained unchanged.
Peer interaction was judged as ‘bad’ or ‘very bad’ in 23.9% of all patients at baseline. At the end of the study, the rate of patients with such judgments had diminished to 9.5%. At the same time, the rate of patients with judgments ‘good’ or ‘very good’ had increased from 42.2% to 65.4%. In total, 47.4% of patients showed an improvement in peer interactions, 17.3% worsened, and 35.3% remained unchanged.
Considering the distribution parameters after coding from 1 = ‘very good’ to 5 = ‘very bad’, significant improvements were found in all relevant areas of life in the whole sample as well as in both subgroups (initial treatment and switch treatment; all p < 0.0001), with numerically greater improvements in all areas in the initial treatment group (Table 3).
In the regression model for the main endpoints addressing effects on various life areas, the variables of CGI at baseline and, in some cases, group and duration of the disorder at baseline could be identified as significant influencing factors. The largest effects could be expected in patients with higher ratings in severity of disease, without previous MPH treatment and with longer duration of the disease.
CGI and CGI-C (severity of disease)
Most patients had ‘marked’ or ‘moderate’ disease at baseline (whole sample: 81.0%, initial treatment: 81.3%, and switch treatment: 81.0%). Actual severity of disease was slightly milder in patients of the switch treatment group, with a mean value ± SD in CGI at baseline of 4.4 ± 0.9 versus 4.7 ± 0.8 in the initial treatment group. In the whole sample, the rate of patients with ‘marked’, ‘severe’, or ‘extremely severe’ disease decreased from 51.0% at baseline to 20.3% at the end of the study. In the initial treatment group as well as in the switch treatment group most patients had ‘moderate’ disease at the end of the study (initial treatment: 32.0%, switch treatment: 28.6%) followed by ‘mild’ disease (initial treatment: 26.7%, switch treatment: 28.1%). Differences between CGI values at baseline and end of the study were statistically significant in both subgroups and in the whole sample (p < 0.0001; Fig. 1).
For the CGI Change (CGI-C), 81.0% of all patients showed an improvement in their severity of disease (including minimal improvement). At the end of the study, most patients had ‘much improved’ (43.8%) or ‘very much improved’ (23.5%); 13.7% of patients showed a worsening (‘minimally’, ‘much’, or ‘very much worse’), and 2.9% remained unchanged. Compared to the switch treatment group, more patients in the initial treatment group showed at least minimal improvement (79.7% vs. 85.3%) and less patients worsened (15.2% vs. 9.3%) (Fig. 2).
Response and remission
67.3% of patients showed a response (CGI-C ≤ 2, meaning at least ‘much improved’ at week 8). The response rate in the initial treatment group was higher than in the switch treatment group (74.7% vs. 64.9%). Remission rate (CGI ≤ 2 meaning not ill or borderline ill at week 8) was 20.9% (whole group). There was no difference in remission rates between the initial and the switch treatment group.
Quality of life (QoL)
Quality of life for the family at last value had at least ‘improved’ in 73.9% of all patients in the whole sample based on an interview with the parents. Quality of life was rated as ‘unchanged’ in 16.0%, as ‘worse’ in 8.5%, and as ‘much worse’ in 1.3% of all patients. In the switch treatment group 70.6% showed an improvement compared to 84.0% in the initial treatment group (Fig. 3).
Global rating of effectiveness
In this global rating, 29.1% of investigators rated therapeutic effectiveness as ‘very good’, 43.8% as ‘moderate’, 11.1% as ‘low’, and 13.7% as ‘unimproved/declined’. The remaining 2.3% provided no rating.
Parents’ satisfaction
Parents (51.0%) rated the effectiveness of therapy with OROS® MPH as ‘good’ and 20.9% as ‘very good’, 14.1% as ‘moderate’, 11.1% as ‘bad’, and 1.6% as ‘very bad’. In total, 69.3% of all parents were ‘very satisfied’ or ‘satisfied’ with the therapy.
Tolerability results
Tolerability was judged as ‘good’ or ‘very good’ by 85.0%, ‘moderate’ by 8.2%, ‘bad’ or ‘very bad’ by 5.6% of parents.
Adverse events
A total of 319 adverse events (AEs) were reported by 160 of 306 patients (52.3%). For 161 of 319 AEs (50.5%) in 95 patients (31.0%) a causal relationship between the administration of OROS® MPH and the event was assessed as at least possible by the investigator. Most frequent adverse events (≥5% of all patients) were insomnia (10.8%), anorexia (7.8%), ineffectiveness of medication (7.8%), and headache (5.6%). Adverse events with a frequency ≥2% and <5% of all patients were infections—mainly of the respiratory system—and related symptoms (such as fever), abdominal pain, involuntary muscle contractions, and weight decrease. Adverse events with at least possible causality were more common in patients of the initial treatment group (37.3%) than in the switch treatment group (29%), especially insomnia (14.7%) and anorexia (10.7%) occured more frequently. In 37 (12.1%) patients, AE led to discontinuation of study participation. The most frequent AE leading to premature discontinuation was lack of efficacy in 16 cases. No unexpected AE occurred. Four serious AEs (SAEs) were reported in 2 patients. These were ‘family stress’, short ‘loss of consciousness’, ‘tremor’, and ‘decreased activity’. Causal relationship between the SAEs and OROS® MPH was rated as ‘doubtful’ by the reporters in all four cases. All patients with SAEs recovered from the events.
Weight and BMI
Mean weight ± SD at baseline was 37.2 ± 12.9 kg (range 18.0–88.8 kg), and 37.0 ± 13.0 kg (range 18.6–88.0 kg) at endpoint. Mean weight change ± SD between baseline and endpoint accounted for −0.26 ± 1.4 kg (range −5.9 to 4.0; n = 285 evaluable). Mean decreases in weight were slightly larger in the initial treatment group (−0.69 ± 1.6 kg) compared to the switch treatment group (−0.12 ± 1.3 kg).
Mean BMI ± SD at enrolment was 17.8 ± 3.3 kg/m2 (range 12.5–33.4 kg/m2), and 17.5 ± 3.3 kg/m2 (range 12.7–32.3 kg/m2) at endpoint. Mean change in BMI ± SD was −0.3 ± 0.7 kg/m2 (range −4.1 to 1.8 kg/m2; n = 283 evaluable).
Vital signs
Mean systolic blood pressure ± SD was 106.9 ± 11.2 mmHg at baseline and 107.3 ± 11.0 mmHg at the end of the study. Mean change ± SD between visits 1 and 4 was 0.1 ± 10.8 mmHg. Mean diastolic blood pressure ± SD was 67.1 ± 9.2 mmHg at baseline and 68.1 ± 8.9 mmHg at the end of the study. Mean change ± SD between visits 1 and 4 was 0.7 ± 9.7 mmHg. Mean pulse rate ± SD was 80.6 ± 11.1/min at baseline and 82.1 ± 12.1/min at the end of the study. Mean change ± SD between visits 1 and 4 was 1.5 ± 12.6/min.
Appetite and sleep
79.4% of patients were at least ‘satisfied’ with their appetite at baseline; 41.8% showed no changes from baseline to last visit, 26.5% showed an improvement, and 31.7% a worsening in appetite. There were no statistically significant differences in quality of appetite between baseline and last value, but a tendency for decreasing appetite in the group without previous MPH (p = 0.06).
Most patients were at least ‘satisfied’ with their quality of sleep at baseline (80.7%); 38.2% of all patients had no changes from baseline to last value, followed by 34.0% with improvement, and 27.8 with a worsening in quality of sleep. There were no statistically significant differences in quality of sleep between baseline and last value, but a weak tendency for impaired quality of sleep in the initial treatment group (p = 0.12).
Tics
There were 25 patients with details to tics at visits 1 and/or 4. Most tics were present in patients with previous MPH medication. In most patients with preexisting tics, no change in tics occurred during the documentation period (n = 11). Eight patients showed positive changes and six patients showed negative changes. Tics emerging for the first time at visit 4 were found in five patients.
Discussion
Due to usually rigid inclusion and exclusion criteria, and closely described and monitored instructions for treatment and concomitant medication, controlled clinical trials do not necessarily reflect the conditions of daily routine care. Most patients with ADHD in Germany are either treated by child and adolescent psychiatrists or in paediatric private practices. It might, therefore, be important to document tolerability and effectiveness of a treatment under the conditions of this daily routine care by conducting non-interventional studies. One of the design requirements of this study was its practicability in paediatric routine care with simplified assessments feasible under these naturalistic conditions and without requiring special rater trainings. Therefore, predominantly uncomplex, categorical, non-validated Likert scales were chosen for assessment of treatment effects, easing study feasibility, but also limiting the interpretation of its results concerning their clinical relevance. Furthermore due to the nature of a non-interventional design, this study was an open-label study of short duration and with no further follow-up phase, with no control group and no active comparator as well. These limitations taken into account, data derived from non-interventional studies may serve as a valuable source of additional information (D’Agostino and D’Agostino 2007), especially concerning tolerability. Here, tolerability data were assessed in-depth by not only asking for documentation of adverse events, which may lead to underreporting (Segal et al. 2005), but also by prompting information on relevant safety issues, such as weight, vital signs, sleep, appetite, and tics.
In this prospective, open-label, single-arm, non-interventional study, data from 306 children and adolescents aged 10.2 ± 2.3 years with a diagnosis of ADHD could be analysed. The median duration of observation was 8 weeks. With a retention rate of 85.9%, the collected data may be considered as a valid basis for evaluation. Premature termination, in most cases, was due to adverse events or to lack of efficacy of medication. Treatment was initiated with OROS® MPH (subgroup initial treatment, MPH-naïve patients) in a fourth of the patients, whereas three-fourths of patients were switched to OROS® MPH from short-acting MPH-IR formulations (subgroup switch treatment). Demographic and disease characteristics of both subgroups were comparable.
It should be taken into consideration that, due to the non-interventional design, diagnosis and treatment decisions were made by the treating physician prior to documentation and during the course of the study, neither standardized diagnostic procedures nor a pre-defined titration scheme were performed. Some information was not captured in the documentation file not even retrospectively. This contained the information about how the ICD-10 diagnosis of ADHD or the diagnosis of comorbidities were made, why a treatment with OROS® MPH was initiated or why medication was transitioned and about any possible wash-out or switching phase of prior MPH treatment. Especially the lack of information concerning the dosage and dosing regimen of a prior MPH treatment could lead to biases and leaves the possibility that patients in the switch treatment group would have experienced the same benefit with a simple adjustment of dosage or dosing regimen, respectively. Therefore results should be interpreted with caution.
Regarding the importance of extracurricular activities, a main focus of evaluation of effectiveness was set on patients′ functioning in different areas of life, including family life, recreational activities, and peer interactions. Significant improvement was found in all four areas of life (including school), in the whole sample as well as in both subgroups. In the regression model to the different areas of life the largest improvements could be expected in patients without previous MPH medication and with higher severity and longer duration of disease.
CGI and CGI-C were used as generally accepted global measures of actual severity of psychopathology. Differences between CGI values at baseline and end of the study were statistically significant in both subgroups as well as in the whole sample. Considering the CGI Change (CGI-C) 81.0% of all patients showed at least minimal improvement. Following a definition by Steele et al. (2006a), response and remission in a post-hoc analysis of this trial accounted for 67.3% and 20.9% of patients, respectively. These response rates are in line with those given for MPH in literature (Rappley 2005). The remission rate seems to be lower than the results given for MPH in literature. This may be due to the relatively low doses given in this trial (mean 32.8 ± 13.2 mg/day). Based on the existing evidence Steele et al. (2006b) concluded that adequate doses are needed to achieve optimal outcomes and that remission rates increase with higher doses.
The positive effects concerning quality of life, possibly due to treatment, can be seen in line with results from another prospective, open-label study with 598 children and adolescents treated with OROS® MPH over a 12-week period, that showed significant improvement in quality of life from 17 ± 4 points to 20 ± 4 points on the ILK parent rating scale (p < 0.0001) and from 19 ± 4 points to 21 ± 4 points on the ILK child rating scale (p < 0.0001) (Wolff et al. 2008). Nevertheless profound research on quality of life in ADHD as a multidimensional construct is still sparse.
Satisfaction with therapy was very high. More than 69% of the parents were at least ‘satisfied’ with OROS® MPH, another 13.4% ‘moderately satisfied’. Only 16.0% were ‘dissatisfied’ or ‘very dissatisfied’. Satisfaction with medication is usually a result of favourable effectiveness, good tolerability, and a convenient therapeutic regimen.
In all analysed criteria of effectiveness, patients in the initial treatment group experienced slightly larger improvements than patients in the switch treatment group. Response rates of MPH naïve patients were higher as well. Mean CGI-Scores at baseline suggest that actual severity of disease was slightly milder in the group of patients already treated with MPH prior to this study. These findings might be interpreted in the way, that patients in the switch treatment group had already experienced a partial benefit of their previous MPH-treatment and gained (just) an incremental benefit through the transition to OROS® MPH. Another possible explanation may be that patients, who were switched to OROS® MPH from MPH-IR, were the more difficult patients with a history of unsatisfactory results under prior medication. Due to the lack of information concerning history of disease, prior treatment details and reasons for transition of medication the true cause for these slightly differential effects remain unclear.
Taking all limitations of this non-interventional study into account, therapy with OROS® MPH resulted in positive effects on some relevant areas of life for the described population possibly due to the long duration of action of the medication and also in a high degree of satisfaction with the medication in patients as well as their families. High satisfaction with therapy may likely influence compliance in a positive way. However, this study was not designed to prove this assumption. The described effectiveness results are therefore more of hypothesis generating value and further research is needed.
The most frequently reported adverse events seen in this study were insomnia, anorexia, and headache. MPH naïve patients experienced somewhat more AE, especially insomnia and anorexia, which probably also led to the slightly larger mean decreases in weight and tendencies to impaired quality of appetite and sleep, compared to patients in the switch treatment group. These findings are in accordance with the fact, that decreased appetite and sleep problems (and headache) are common adverse effects of MPH treatment and mainly occur early after the onset of treatment (Wolraich et al. 2007).
The average decrease in weight during this 8-week study was −0.26 kg. Other studies have also reported comparably small initial weight decreases (Heger et al. 2006; Lynch et al. 2003). There remains some conflicting evidence regarding weight and growth in children receiving methylphenidate and it is unclear whether final adult height is affected (NICE 2009). Therefore, weight and height should be regularly checked during stimulant therapy.
No clinically relevant changes in vital signs could be detected during the observation period, neither in the whole sample, nor in one of the subgroups. Research regarding the effect of MPH on blood pressure has indicated a small but clinically non-significant effect (average +5 mmHg) in short-term use with a slight increase in pulse rate (average +5 bpm) (NICE 2009). As long-term effects remain unclear, vital signs should be checked regularly during stimulant therapy.
The rate of patients with ‘involuntary muscle contractions’ as adverse event is lower than the rate of patients with documented tics and approximately as high as the rate of patients with documented worsening of tics during the documentation period. This supports the observation that stimulants can be used with care in patients with preexisting tics (Gadow et al. 2007).
Conclusion
In this prospective, open-label, non-interventional trial conducted in Germany, transition from MPH-IR as well as initiation of therapy with OROS® MPH in MPH-naïve patients aged 6–14 years with a diagnosis of ADHD were associated with significant improvements in daily functioning in several areas of life, severity of disease, and in quality of life. Recognizing the limitations inherent in the design of the study (non-interventional trial, no control group, no active comparator, some information on diagnosis and pre-treatment lacking, simplified assessments, non-validated scales, patient selection without rigid inclusion and exclusion criteria solely based on the discretion of the treating physician and post-hoc analyses based on within-group analyses), the results of this study in paediatric routine care may add additional findings for the good tolerability of an effective long-acting therapy with OROS® MPH. Furthermore, based on the results of this trial it could be stated that initial treatment with long-acting preparations might be an alternative effective and tolerable option. Long-acting MPH preparations for the treatment of ADHD might also be taken into consideration if a regimen with short-acting MPH preparation is not seen as optimal for the individual treatment. Overall, this non-interventional study supports similar findings from randomized, double-blind clinical trials and from other open-label studies. The improvements in functioning in different areas of life, severity of disease, and quality of life documented in this population after switching patients to OROS® MPH or after initiating treatment may point out the possible need for a therapy which covers not only school-time, but also the afternoon. Further controlled research on the influence of treatment on ADHD, concerning quality of life and impact on functioning and symptomatology throughout the whole day is needed. Besides using validated outcome measures, these investigations should be based on clear diagnostic procedures, a thorough documentation of disease characteristics, co-morbidities, and prior and concomitant therapies to identify criteria, e.g. ADHD subtypes, which allow a differential therapeutic approach.
References
American Academy of Pediatrics (2000) Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics 105:1158–1170
Banaschewski T, Coghill D, Santosh P et al (2006) Long-acting medications for the hyperkinetic disorders. A systematic review and European treatment guideline. Eur Child Adolesc Psychiatry 15:476–495
Barbaresi WJ, Katusic SK, Colligan RC et al (2002) How common is attention-deficit/hyperactivity disorder? Incidence in a population-based birth cohort in Rochester, Minn. Arch Pediatr Adolesc Med 156:217–224
Barkley RA, Fischer M, Edelbrock CS, Smallish L (1990) The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 29:546–557
Brown RT, Amler RW, Freeman WS et al (2005) Treatment of attention-deficit/hyperactivity disorder: overview of the evidence. Pediatrics 115:e749–e754
D’Agostino RB Jr, D’Agostino RB Sr (2007) Estimating treatment effects using observational data. JAMA 297:314–316
Escobar R, Hervas A, Soutullo C, Mardomingo M, Uruñuela A, Gilaberte I (2008) Attention deficit/hyperactivity disorder: burden of the disease according to subtypes in recently diagnosed children. Actas Esp Psiquiatr 36(5):285–294
Faraone SV, Wilens T (2003) Does stimulant treatment lead to substance use disorders? J Clin Psychiatry 11(Suppl 64):9–13
Gadow KD, Sverd J, Nolan EE, Sprafkin J, Schneider J (2007) Immediate-release methylphenidate for ADHD in children with comorbid chronic multiple tic disorder. J Am Acad Child Adolesc Psychiatry 46:840–848
Gittelman R, Mannuzza S, Shenker R et al (1985) Hyperactive boys almost grown-up. Arch Gen Psychiatry 42:937–947
Harpin VA (2005) The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child 90(Suppl 1):i2–i7
Hechtman L, Weiss G, Perlman T et al (1984) Young adult outcome of hyperactive children who received long-term stimulant treatment. Am Acad Child Adolesc Psychiatry 23:261–269
Heger S, Trott GE, Meusers M et al (2006) Switching from a short-acting to a long-acting methylphenidate preparation: a multicentre, open study in children with ADHD. Z Kinder-Jugendpsychiatr Psychother 34:257–265
Jerome L, Segal A, Habinski L (2006) What we know about ADHD and driving risk: a literature review, meta-analysis and critique. J Can Acad Child Adolesc Psychiatry 15(3):105–125
Johnston C, Mash EJ (2001) Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clin Child Fam Psychol Rev 4:183–207
Kessler RC, Adler L, Ames M et al (2005) The prevalence and effects of adult attention deficit/hyperactivity disorder on work performance in a nationally representative sample of workers. J Occup Environ Med 47:565–572
Klassen AF, Miller A, Fine S (2004) Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics 114:e541–e547
Lynch JM, Gu J, Meloni FJ (2003) OROS® MPH ADHD therapy: height and weight effects. Poster presented at the 50th anniversary meeting of the American Academy of Child and Adolescent Psychiatry, Miami, FL, 14–19 October 2003
Mannuzza S, Klein RG, Bessler A et al (1993) Adult outcome in hyperactive boys. Arch Gen Psychiatry 50:565–576
Minde K, Eakin L, Hechtman L et al (2003) The psychosocial functioning of children and spouses of adults with ADHD. J Child Psychol Psychiatry 44:637–646
Modi NB, Lindemulder B, Gupta SK (2000) Single- and multiple-dose pharmacokinetics of an oral once-a-day osmotic controlled-release OROS® (methylphenidate HCl) formulation. J Clin Pharmacol 40:379–389
Murphy KR, Barkley RA (1996) Adults with ADHD: comorbidity and adaptive functioning. Compr Psychiatry 37:393–401
National Institute for Health & Clinical Excellence (NICE) (2009) Diagnosis and management of ADHD in children, young people and adults. National Clinical Practice Guideline Number 72. http://www.nice.org.uk/nicemedia/pdf/ADHDFullGuideline.pdf
Pelham WE, Lang AR (1999) Can your children drive you to drink? Stress and parenting in adults interacting with children with ADHD. Alcohol Res Health 23:292–298
Pelham WE, Gnagy EM, Burrows-Maclean L et al (2001) Once-a-day concerta methylphenidate versus three-times-daily methylphenidate in laboratory and natural settings. Pediatrics 107:e105
Podolski CL, Nigg JT (2001) Parent stress and coping in relation to child ADHD severity and associated child disruptive behaviour problems. J Clin Child Psychol 30:503–513
Rappley MD (2005) Clinical practice. Attention deficit-hyperactivity disorder. N Engl J Med 352:165–173
Segal ES, Valette C, Oster L et al (2005) Risk management strategies in the postmarketing period: safety experience with the US and European bosentan surveillance programmes. Drug Saf 28:971–980
Sobanski E, Alm B (2004) Attention deficit hyperactivity disorder in adults. An overview. Nervenarzt 75:697–716
Steele M, Weiss M, Swanson J, Wang J, Prinzo R, Binder C (2006a) A randomized, controlled effectiveness trial of OROS-methylphenidate compared to usual care with immediate-release methylphenidate in ADHD. Can J Clin Pharmacol 13:e50–e62
Steele M, Jensen PS, Quinn DMP (2006b) Remission versus response as the goal of therapy in ADHD: a new standard for the field. Clin Ther 28(11):1892–1908
Stein MT, Perrin JM (2003) Diagnosis and treatment of ADHD in school-age children in primary care settings: a synopsis of the AAP Practice Guidelines. American Academy of Pediatrics. Pediatr Rev 24:92–98
Steinhausen HC (2003) Attention-deficit hyperactivity disorder in a life perspective. Acta Psych Scand 107:321–322
Swanson J (2003) Compliance with stimulants for attention-deficit/hyperactivity disorder: issues and approaches for improvement. CNS Drugs 17:117–131
Swanson J, Greenhill L, Pelham W et al (2000) Initiating Concerta® (OROS® methylphenidate HCl) qd in children with attention-deficit hyperactivity disorder. J Clin Res 3:59–76
Swanson JM, Wigal SB, Wigal T et al (2004) A comparison of once-daily extended-release methylphenidate formulations in children with attention-deficit/hyperactivity disorder in the laboratory school (the Comacs Study). Pediatrics 113:e206–e216
Taylor E, Doepfner M, Sergeant J et al (2004) European clinical guidelines for hyperkinetic disorder–first upgrade. Eur Child Adolesc Psychiatry 13(Suppl 1):17–30
Topolski TD, Edwards TC, Patrick DL, Varley P, Way ME, Buesching DP (2004) Quality of life of adolescent males with attention-deficit/hyperactivity disorder. J Atten Disord 7:163–173
Wilens T, McBurnett K, Stein M et al (2005) AD/HD treatment with once-daily OROS methylphenidate; final results from a long-term open-label study. J Am Acad Child Adolesc Psychiatry 44:1015–1023
Wolff C, Schauble B, Hargarter l, Mattejat F (2008) Changes in quality of life and daily functioning in patients with ADHD treated with extended release methylphenidate (OROS-MPH); Results from an open-label naturalistic study. Poster presented at 16th European congress of psychiatry, 5–9 April 2008, Nice, France
Wolraich M (2003) ADHD treatment with once-daily OROS® MPH: a long-term, open-label study of safety and tolerability. Poster presented at the Pediatric Academic Societies annual meeting, 3–6 May 2003, Seattle, WA
Wolraich ML, Greenhill LL, Pelham W et al (2001) Randomized controlled trial of OROS methylphenidate once a day in children with attention-deficit/hyperactivity disorder. Pediatrics 108:883–892
Wolraich ML, McGuinn L, Doffing M (2007) Treatment of attention deficit hyperactivity disorder in children and adolescents; safety considerations. Drug Saf 30(1):17–26
Acknowledgments
This study was supported by Janssen-Cilag GmbH, Germany. We thank the investigators and patients for participating in the study. We also acknowledge the statisticians of ClinAssess for their contribution to data management and analysis.
Conflict of interest statement
Martin Gerwe is employee of Janssen-Cilag, Manuela Bogdanow was the Leading Statistician from ClinAssess and Steffen Heger, as Medical Writer of this manuscript, delivers scientific consultancy services for Janssen-Cilag. The other authors were investigators in this study. Christopher Schaefer reports having received lecture and consulting fees from Janssen-Cilag. Kirsten Stollhoff, Hans-Juergen Kuehle and Ulrich Goertz report having received lecture fees from Janssen-Cilag. Jacek Mossakowski reports no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gerwe, M., Stollhoff, K., Mossakowski, J. et al. Tolerability and effects of OROS® MPH (Concerta®) on functioning, severity of disease and quality of life in children and adolescents with ADHD: results from a prospective, non-interventional trial. ADHD Atten Def Hyp Disord 1, 175–186 (2009). https://doi.org/10.1007/s12402-009-0010-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-009-0010-6