Abstract
Most studies on socially assistive robots (SARs) in elder care are conducted in care homes and recruit participants with some degree of cognitive impairment. The ethical dimension in these studies thus requires careful attention, suggesting that the researchers involved should be offered specific research ethics training. To meet this need in CARESSES—an international multidisciplinary project that aims to design and evaluate the first culturally competent SAR for the care of older adults—a research ethics training module for the project researchers was developed. The training module is largely based on case-based learning (CBL), a widely recognized approach to learning and instruction that is regarded as highly effective across multiple disciplines. In this paper, we argue that research ethics training should be offered to robotics investigators involved in research on SARs in elder care, and we provide an overview of the ethical issues involved in conducting research with SARs and older adults in care homes. Finally, we show how CBL can be used for research ethics training in this context.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Ageing populations and shrinking caregiver numbers are one of the main societal challenges worldwide today [1]. The convergence between this challenge and advances in robotic technology has determined an increased interest in the possibility of using socially assistive robots (SARs), i.e. robots designed to give assistance to human users through non-contact interaction [2], to support the delivery of safe and efficient care to older persons [3]. Indeed, a recent scoping review designed to establish the clinical usefulness of SARs in elderly care found that 33 studies have been conducted to date focusing on the use of SARs with older persons, involving 1574 participants and 11 different types of robots. Most of those studies enrolled participants with declining cognitive and mental abilities living in care homes [4].
Human subjects research involving vulnerable individuals such as persons living in long-term care facilities requires careful attention to its ethical dimension, as it is likely that investigators will encounter a broad array of ethical challenges [5, 6]. These challenges will often be associated with issues of informed consent, confidentiality and participant rights [6].
Research ethics training can help researchers conduct experiments with human subjects in an ethically appropriate manner, as well as improve their ethical sensitivityFootnote 1 and their practical skills in ethical reasoning and deliberation. We therefore developed a research ethics training module (RETM) for the researchers participating in CARESSES (Culture-Aware Robots and Environmental Sensor Systems for Elderly Support), an internationalFootnote 2 multidisciplinary project that aimed to design the first culturally competent SAR for the care of older persons [7]. CARESSES’ innovative approach is expected to translate into socially assistive care robots that are sensitive to the culture-specific needs and preferences of older clients, while offering them a safe, reliable and intuitive system, specifically designed to support active and healthy ageing and reduce caregiver burden [8].
CARESSES included an experimental phase in which the SAR, a Pepper robot [9] running an innovative custom-built software developed by the project, was trialed in care homes with residents belonging to different cultures. Informal caregivers were also recruited to establish whether the SAR could relieve caregiver burden. The CARESSES study protocol was designed by health psychologists with the contribution of the roboticists who developed the CARESSES software, and of an internal ethics advisor. Both the psychologists and the roboticists conducted the trials and came into direct contact with the research participants during the experiments [10].
The RETM developed for the CARESSES researchers is largely based on case-based learning (CBL), an approach to learning and instruction that relies on scenarios to illustrate teaching points and issues [11]. CBL is acknowledged to have positive effects on learners’ decision-making and deductive and inductive reasoning skills [10, 11]. Because it has clear benefits for individuals grappling with complex situations, CBL is widely used in ethics education [12, 13]. The core of the CARESSES RETM are thus three ethical cases that were developed for this project and exemplify situations that could realistically emerge during the project experiments.
This paper’s purpose is threefold: first, to emphasize the importance of providing instruction in research ethics and human subjects protection to robotics researchers involved in human subjects research, and specifically in research on SARs in elder care; second, to present the main ethical issues involved in conducting research in care homes and research with older adults and SARs; third, to show how case-based learning can be used for research ethics training in this context.
The article is organized as follows: Sect. 2 clarifies the need for training in research ethics and human subjects protections for investigators involved in research with human subjects; Sect. 3 provides an overview of the main ethical issues in research with older participants; Sect. 4 specifically addresses ethical concerns that emerge when conducting research with SARs in long-term care facilities; Sect. 5 provides background knowledge on case-based learning and case design; Sect. 6 outlines the ethics training approach designed for the CARESSES project along with the ethics cases developed; furthermore, it summarizes the feedback CARESSES researchers provided on the RETM and its perceived impact. We close with conclusions in Sect. 7.
2 The Need for Research Ethics Training
Research ethics is often defined as the ethics of planning, conduct and reporting of research [14]. It aims at protecting human research participants, ensuring that research is carried out in ways that are beneficial to individuals, groups, communities or society as a whole, and at examining specific research activities and projects for their ethical soundness.
According to the Declaration of Helsinki, the recognized cornerstone of research ethics, investigators who conduct research with human subjects are responsible for the protection of participants’ rights, safety, and welfare [15]. In many countries these protections are ensured through independent review of research projects by Research Ethics Committees (REC) or Independent Research Boards (IRB), consisting of both professionals and lay people. In addition, in some countries, and depending on the type of research funding organization, the protection of human research participants is enhanced by investigator training in the principles and regulations pertaining to the ethical conduct of human subjects research [16, 17].
There are at least three good reasons why training in human subject protections and ethical research conduct is often a requirement for investigators involved in human subject research. First, it enables researchers to understand the fundamental principles of research ethics, so they can then design, plan and conduct research in ways that position the protection of participants’ rights, safety and welfare at its core [14]. Second, RECs and IRBs will be more confident in approving a research application if they have evidence that the researchers involved have completed some form of research ethics training and possess at least a basic understanding of those fundamental principles [17, 18]. The third reason is more complex. One of the key aims of education in research ethics is to provide researchers with the knowledge and tools that will help them engage with the ethical issues and tensions they may encounter during research activities. As iterated by Sedenberg and colleagues [19], those ethical tensions often stem from the need to balance the risks and benefits intrinsic to research activities with regard to individual participants, while at the same time considering their societal impacts. Indeed, many of the principles and values that research ethics strives to safeguard specifically address the fact that tradeoffs may sometimes be necessary to increase generalizable knowledge and eventually benefit society as a whole. Thus, within research activities some risk to participants (in terms of, for instance, discovery of unexpected health-related findings, minor discomfort during experiments, etc.) may be acceptable in order to enable scientific discovery. Providing researchers with an understanding of the fundamentals of research ethics and an ethical framework to determine acceptable risk/benefits tradeoffs can enable them to balance ethical tensions in ways that protect participants, preserve ethical principles and values, and allow research activities [19].
3 Ethical Issues in Research with Older Persons Living in Care Homes
Conducting research in care homes can involve a number of specific challenges regarding research ethics and the protection of human participants [20]. We provide here a brief overview of some of the main challenges discussed in the literature.
The first source of ethical concern, as emphasized by Ramos et al., is associated with the values and goals of a research project itself, when the benefits it is expected to generate for policy-makers, organizations, professional care-givers, families or other stake-holders (such as increased safety through the implementation of technology-based solutions) are not consistent with the preferences or needs of research participants. When this occurs, outcomes that may be viewed positively by the research can produce unintended or negative consequences for those participants and/or the population they represent [21].
Selection criteria and the procedures followed to recruit older participants or retain them in studies may also be of concern; for instance, the selection process may involve a risk of psychological harm to those who are found not to qualify or to no longer qualify for participation (e.g. owing to deteriorated cognitive abilities).
As Mody and colleagues point out [22], questions of reciprocity must be taken into account and the benefit to burden ratio maximized (e.g. is the research project expected to enhance the quality of care for the research participants?). Furthermore, a balance must be struck between accommodating the needs of the facility and preserving the integrity of the study protocol [22].
Some of the major ethical issues related with research involving older participants, particularly when it comes to care home residents, revolve around informed consent [5]. Protecting participants and respecting their right to self-determination and to exercise personal choice requires that researchers seek their informed consent to participate in a research study. Thus, candidate research subjects must be given the opportunity to learn what is expected of their participation and what will happen to them and to the data that is collected during the study. Prior to deciding whether they want to participate, they should also be given a clear description of risks and benefits related to the study and learn about their right to withdraw at any time and without penalty. The decline in cognitive abilities that often occurs with aging, however, is known to negatively impact on understanding and retention of informed consent information. At the same time, if at all possible, older persons and not surrogate decision-makers should give consent; this may require using targeted strategies or formats, such as easy-to-read text, the use of graphic illustrations and revisiting consent, which can help remind participants of key aspects of the research enterprise [23].
Protecting the welfare of older research participants also requires that special attention be paid to maintaining role boundaries: although trust and empathy should characterize the research relationship, emotional bonds should be avoided to preserve participants and researchers from psychological harm [24]. This will also prevent a personal relationship from influencing research outcomes. Furthermore, clearly differentiating between research and care roles whenever possible allows investigators and care staff to demarcate and make clear the extent of their responsibilities towards the care home residents who are recruited to studies [25].
Elder abuse is a known problem in long-term care facilities [26], and handling suspected cases of abuse can be ethically fraught [27]. Researchers need to make themselves aware of any institutional rules and local or national laws requiring mandatory reporting. In cases where mandatory reporting is not required, researchers may be concerned about potential ethical violations when reporting such incidents and should establish procedures for actively handling suspected cases of abuse [28].
Finally, questions may emerge involving ageism, that is negative attitudes based on age, including negative feelings, age-based stereotypes and discrimination. As ageism is more likely to impact research design and conduct when researchers are unfamiliar with older populations, providing training and opportunities for discussion is often a helpful approach to prepare researchers to work with older adults and reduce ageist attitudes [29].
4 Ethical Issues in Research on SARs in Elder Care
The future of SARs in the care of older persons has been the focus of a great deal of regulatory and ethical reflection [30,31,32], much of which has centered on concerns relating to a loss of human contact, diminished autonomy and privacy, loss of dignity [33, 34], and to negative impacts on professional caregiving and standards of care [35]. Ethical concerns that arise within research settings, when SARs are trialed with older persons, do not seem to have garnered as much attention despite, predictably, much of this research being conducted in care home facilities with vulnerable individuals and interaction with novel technologies possibly raising specific concerns [15, 19, 26, 36]. We discuss some of these issues below, with a focus on potential risks to participants associated with interactions with SARs during experimental trials.
4.1 Safety
Older individuals may experience difficulties with mobility, vision and coordination, which may be hazardous depending on the SAR’s stability, color, size, shape, movement or sound. Therefore, all the SAR’s safety vulnerabilities should be identified and procedures to address them developed [37]. Video and audio surveillance of interactions between research participants and the SAR, with the participants’ consent, can be useful to monitor participants throughout experiments, so researchers can step in if necessary to protect participants’ safety and well-being, and participants can easily call for help.
4.2 Attachment
SARs are generally characterized by some degree of human-like appearance, qualities or behaviors. These features may have impacts with ethical ramifications [38]. For instance, research participants who become psychologically attached to the SAR may experience disappointment if they have to share it with others [37]. Developing psychological and emotional bonds with the SAR can also have harmful effects on participants at the end of the project when they have to part with it. Accordingly, protocols must be specified in advance to address any consequent needs on the part of participants.
4.3 Privacy
SARs’ programmed reactions towards the behavior and movement of research participants may affect participants’ sense of privacy in that they may feel that they are not alone (which can also be positive) or that they are being watched. If participants can control privacy levels, such problems can easily be overcome [37]. Monitoring research participants for safety purposes or recording their interactions with the SAR for research purposes can both be perceived as invasions of privacy and require specific consent from participants. Researchers should also have guidelines on how to respect participant privacy even if participants do not specifically request it.
4.4 Data Management and Protection
The processing of any personal data collected during the research project (including any footage from safety monitoring) requires freely given, specific informed consent from research participants.
Data processing must employ appropriate technical and organizational measures to comply with national laws and regulations. In the US, for instance, this may be the Health Insurance Portability and Accountability Act (HIPAA), a set of standards created to secure protected health information [39]. In the EU, it will mean complying with the General Data Protection Regulation 2016/679 (GDPR), and particularly with the data subject rights identified in the GDPR such as the right to be informed, the right of access and the right to erasure [40]. Data collected from the study participants, including data from video- and audio-monitoring, must also comply with the principle of data minimization, meaning that the collection of personal information should be limited to what is directly relevant and necessary to protect participants and accomplish the specific goals of the study [40].
4.5 Participant Autonomy and Proportionality
In experiments with research subjects, SARs can be used to carry out certain tasks on participants’ behalf or to provide support that enables them to complete the task on their own. Whether this will promote older users’ autonomy and independence will depend on whether the SAR’s interventions are restricted to what is required and useful for a selected population or individual. Providing more assistance than is actually required may result in the premature loss of capacities in older adults, generating dependency on the SAR [27, 29].
4.6 Dignity
Individuals may feel more or less at ease interacting with SARs, and interactions with the SAR may suit some research participants more than others. It could even be problematic if people find interactions with the SAR useful or enjoy them but feel ridiculous using it [37]. The SAR may also remind them of the human contact that is not available to them. Some may be confused by the SAR, or have difficulty understanding how it works, what to do to make it work or what triggers its actions, which could lead to self-blame and lowered self-efficacy. It must be clear to participants that they can withdraw from the study at any time if they so wish.
4.7 Psychological Harm
Older research participants may experience anxiety, depression, embarrassment, or acute stress reactions due to utilization of the SAR, to the fact that they are participating in the experiment, or due to other unrelated reasons. It can also be presumed that older adults may experience technology anxiety and frustration due to not remembering or understanding how to use the robot [41]. Researchers must therefore be prepared to identify and minimize these risks and ensure that the benefits of the study outweigh them. If at some point during the study the research team becomes concerned about psychological distress emerging in a participant, either through observation or by being informed by the participant or others, the researchers must take steps to help minimize this risk by, for instance, following a distress protocol [42]. In some situations, the appropriate course of action will be to withdraw the participant from the study.
4.8 Managing Unexpected Health-Related Findings
Interacting with the SAR is a novel, unusual activity that may uncover health-related issues in research participants that would not emerge otherwise [36]. Protocols for managing such issues need to be developed ensuring that researchers can balance their obligation to protect confidential health-related information about participants, with their ancillary obligation to protect participants’ welfare. One way to do this is for researchers to sensitively raise the possibility of unexpected health-related findings during the informed consent process and ask participants for permission to discuss anything of potential health importance that they should observe during the experiments (e.g., a pronounced tremor, a peculiar gait, a significant change in behavior) with the participants’ carers or other care home staff, as appropriate [36].
4.9 Stigma and Self-stigma
Stigma can be defined as a social process whereby an older adult experiences exclusion or rejection owing to negative social judgement associated with a feature related to a health problem or a health condition. In studies with SARs and older adults, researchers cannot rule out the possibility that relying on a robot for assistance, entertainment, and, to some extent, companionship, may result in negative judgements about research participants by other care home residents, for instance, or by research participants about themselves, or by their family members [43]. Approaching all participants with discretion, ensuring confidentiality, and treating their experiences and contributions equally and with full respect can help avoid stigmatization and self-stigma, as can increasing knowledge and understanding of how and why older adults might be stigmatized (and why they might self-stigmatize).
5 Case-Based Learning in Ethics Training
Situations involving the ethical issues described above are often complex, dynamic and multi-faceted. They may present competing goals and values, so that resolutions may be far from clear and not univocal [44]. A helpful way to make sense of similar situations is case-based reasoning, in which reflection on experiences is used to help solve new problems [45]. Individuals can acquire experiential knowledge to apply to similar future problems relatively quickly through CBL, a widely used instructional method that enables them to adapt and respond to new situations [46]. CBL involves analyzing problems presented in study cases, drawing analogies, building inferences and forming decisions in ambiguous contexts that mirror real-world scenarios [47, 48]. Compared with traditional lecture-based approaches, CBL is considered to be a more effective instructional method in improving critical thinking and decision-making skills [10]. Additionally, CBL is often reported to be more enjoyable than traditional lectures, which may improve learner engagement [47, 49].
CBL is well-suited for ethics training because cases can be designed to replicate the layered, ambiguous nature of ethically fraught situations [49, 50], providing trainees with practice navigating them [46] but also with opportunities to discuss abstract ethical principles [51]. In addition, CBL may be especially beneficial with researchers who have little or no experience handling ethical problems, because cases allow for the development and practice of skills without having to actually experience those circumstances [52] .
Even in their simplest form, “good” cases should be characterized by having a specific setting, a logical sequence of events, and defined characters [46]. Several authors have discussed other features of case content in view of improving learning and the acquisition of decision-making skills [11, 53]. In their attempt to identify best strategies for case construction, Kim et al. reviewed 100 studies on case-based teaching and learning [47]. Based on their evaluation of the literature, they concluded that effective cases should be relevant, realistic, engaging, challenging, and instructional. Along with these core elements, Kim and colleagues suggested a number of strategies for successfully integrating these five elements into cases, among which: developing a case in a realistic and relevant setting, enriching it by providing sufficient information about the characters and ethical problems and dilemmas at hand, and increasing difficulty by adding or concealing certain information [47].
Cases should also prompt trainees to reach a decision, encouraging them to work through the controversial situation as if it were a first-hand experience [54]. Finally, cases must provide enough information about key aspects to elicit critical thinking, but should not be so long that they become tedious or boring [54].
6 Research Ethics Training in the Caresses Project
6.1 Training Design
The purpose of the CARESSES Research Ethics Training Module was threefold:
-
to provide the robotics researchers involved in the trials with a basic understanding of the main ethical concepts and principles that underpin the CARESSES study protocol [36];
-
to improve their awareness of ethical issues that may arise during the experiments with a SAR and older adults in a long-term care setting;
-
to improve their ability to identify those ethical issues and understand the consequences of decisions made to solve or manage them.
Although these goals go in the direction of improving researchers’ ethical decision-making skills, it was explained to trainees they would not be asked to make any ethical decision independently during the experiments. Instead, to ensure protection of research participants, they would be required to discuss any issue with their Team Leader and the CARESSES Internal Ethics Board, comprised of the internal ethics advisor and the two psychology leads of the project.
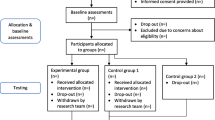
Based on the literature summarized in Sect. 5 above, CBL was chosen as the most suitable approach to achieve these goals. The RETM (Fig. 1) was developed by the CARESSES internal ethics advisor and jointly administered by the ethics advisor and the other members of the project’s Internal Ethics Board. The RETM was computer-based and delivered remotely. It included multiple steps and employed a variety of activities, which has been suggested to improve participant engagement with the content and ultimately facilitate knowledge and skill acquisition [55]. In addition, it structured opportunities for active trainee participation [56].
The training materials consisted of:
-
(a)
the “Ethical Considerations” section of the CARESSES Study Protocol: this document is part of the Ethics Deliverable of the CARESSES project, which is available for download from the project website (http://caressesrobot.org/ethics/D10.1_updated.pdf). It relies on previous work [36] to provide an ethical framework for the study and covers the topics described in Sects. 3 and 4 above; it also explains how those ethical issues and concerns, such as questions of dignity, autonomy, safety, privacy and data management and protection, may arise within the CARESSES experiments, and describes appropriate ways of handling them.
-
(b)
three study cases built around relevant ethical issues (see Tables 1, 2, 3) including informed consent, confidentiality, role boundaries and protection of research participants from harm; the cases describe ethically challenging situations that could emerge during the CARESSES trials.
Table 1 The case of Mr. Chaterjee (sub-tables A and B were not shared with trainees.) Table 2 The case of Mrs. Smith (sub-tables A and B were not shared with trainees.) Table 3 The case of Mrs. Yamada (sub-tables A and B were not shared with trainees.)
In accordance with the recommendations in the literature, the effort was made to ensure that the cases would be realistic and descriptive [47]. Cases were also kept brief, avoiding irrelevant material [44]. Additionally, we attempted to infuse them with emotion [45], omitted certain information to emphasize the importance of gathering all the relevant facts, avoided pointing to clear-cut, obvious solutions, and included elements of ambiguity [47]. Overall, designing the instructional content so that it was specifically customized for the research project was expected to result in greater benefits to trainees, compared with standard off-the-shelf training programs [11].
6.2 Training Delivery
Ten trainees (two robotics researchers in Italy, two in France, two in Sweden and four in Japan) participated in the training. All were male and 8/10 were early stage career researchers. None had previously received any training in research ethics. In the first part of the training process, they were asked to familiarize themselves with the “Ethical Considerations” document. None of the trainees were native speakers of English but all were proficient English readers. Having read the document and having had the opportunity to ask questions about it, they completed a 22-item online multiple-choice quiz (http://caressesrobot.org/ethics/training_questionnaire.pdf). The purpose of the quiz was to enable trainees to demonstrate that they had studied and understood the document, and not to assess their level of knowledge. Trainees were then asked to read and reflect upon the ethics cases independently before discussing them with each other and the Internal Ethics Board during a series of dedicated videoconferences. The discussion included a guided case analysis that was structured around questions relevant to the scenarios described. Trainees were encouraged to analyze the cases and apply relevant knowledge to “solve” the ethical problems, simulating the ethical decision-making process. Specifically, they were asked variations on the following questions, which are based on the Markkula Center Framework for Ethical Decision-Making [57]:
-
What is/are the ethical issue/s illustrated in this case?
-
What are the facts? Is any important information not available in the case description?
-
Who are the stakeholders?
-
Which is the course of action that best fits with the recommendations and requirements set out in the “Ethical Considerations” section of the CARESSES study protocol?
-
How can that course of action be implemented in practice?
-
Could the ethical issue/s presented in the case be prevented? If so, how?
6.3 Knowledge, Feedback and Perceived Impact
Seven out of ten trainees obtained a perfect 22/22 score on the online quiz, one made one mistake, one made two and one made three. These results show that they had studied and understood the material. Furthermore, during the RETM videoconferences all trainees were able to identify the main ethical considerations in the ethics cases discussed and to describe ways of handling those cases that followed the guidance provided in the “Ethical considerations” document.
One week after completing the training module, the trainees were asked to respond to an anonymous feedback survey which used a 5-point Likert scale (Fig. 2), and 9/10 agreed. The instrument had been previously piloted with a convenience sample of robotics fellows to test for content and clarity. Responses to the survey items showed that satisfaction was high (Median = 5; Mean = 4.69; SD = 0.457). Trainees reported that the training had been helpful (3/9) or very helpful (6/9) to achieve learning objectives (Median = 5; Mean = 4.33; SD = 0.5, and 9/9 expressed agreement or strong agreement with the suggestion that similar training should be offered in other projects involving SARs and vulnerable individuals (Median = 5; Mean = 4.67; SD = 0.5).
In their answers to the open-ended questions contained in the survey, 8/9 trainees stated that the ethics cases had been the most useful part of the RETM. One trainee commented that the cases had given him the chance to “really think about situations that I would not have considered otherwise”; according to another, the case discussions “greatly facilitated moving from abstract concepts to practical situations”. When asked about their views on how the training module could be improved, 6/9 trainees stated that increasing the number of cases would be helpful; 3/9 suggested spending more time on discussing individual cases, one of whom also suggested that short vignettes could be usefully included in the “Ethical Considerations” document to illustrate the ethical issues discussed therein.
Eight weeks after completing the training, the trainees were invited to another survey. The specific goal of this instrument was to assess the perceived impact of the ethics training. The instrument used a 5-point Likert scale and was piloted as done for the feedback survey. The first section was designed as a retrospective pre-post survey. This type of tool is useful to explore the knowledge or attitude that participants in a training program had toward a subject before that program, experience, treatment or intervention, and after [58].
There is evidence that when using the traditional pretest–posttest, students asked to rate their knowledge or performance at the beginning of a course tend to overestimate their abilities as they are not able to appreciate the complexity of the content taught [59]. Once they have acquired some knowledge of the topic, students are better able to reflect on how much their knowledge or skills have changed, and their ratings of initial performance levels tend to be lower. In other words, exposure to course content changes student’s ability to benchmark their own performance. This well-known effect has been defined the “response shift bias” [60]. In addition, although recall bias and memory lapses are inherent limitations of the retrospective pre-post design, in this study we attempted to minimize their effects by administering the survey after a relatively short period of time (8 weeks).
Eight out of ten trainees agreed to complete this survey. In the first section of the instrument (Fig. 3), they reported positive or very positive perceptions in terms of how successful the training had been in achieving each of its learning objectives (improving levels of awareness, basic understanding and ability to identify ethical issues). A paired t test of differences between pre and post-training measures was conducted and rendered the following: Pair 1: t (7) = − 9.029, p = < .001, d = 3.38; Pair 2: t (7) = − 6.148, p = < .001, d = 2.84; Pair 3 t (7) = − 14.346, d = 4.23, p = < .001, thus showing very significant results with very high levels of effectiveness. In the second section of the instrument (Fig. 4), questions focusing on how useful familiarizing with the Ethical Considerations document and discussing the ethical cases had been in helping trainees achieve those goals revealed that both were perceived as helpful or very helpful (Median = 5; Mean = 4.73, SD = 0.446).
7 Conclusions
A large number of studies reporting on research ethics training efforts in the sciences have been conducted in the past 20 years [56]. This interest likely mirrors the growing consensus that research ethics training may result in sizable benefits to participants and be crucial to their protection [18]. Yet, wide variation is known to exist across programs in terms of effectiveness [18]. Developed as a project-tailored educational intervention and delivered remotely, the CARESSES RETM was successful in ensuring that trainees were well familiar with the ethical guidance provided in the CARESSES study protocol. Trainees were then able to use that guidance to identify the ethical issues illustrated in the case studies and propose appropriate ways of handling them. In light of the statistical analyses conducted, our findings on the trainees’ perception of how effective the training was, are encouraging. We are nonetheless aware that the small sample and the potential social desirability bias are limitations of the study, and that the results of statistical analyses presented should therefore be treated with caution.
We now plan to conduct semi-structured qualitative interviews with the trainees. By exploring their experience of the ethical facets of the CARESSES trials, we hope to gain a more in-depth understanding of the impact of our RETM.
Overall, we believe this paper shows that research ethics training is an important component in projects involving experiments with SARs and human participants, especially in the case of vulnerable research subjects such as older individuals residing in care homes. We are aware that the use of specific cases may seem to reduce the scope of applicability of our approach and provide too specific a frame for the ethical questions that may emerge. However, the literature on case-based training suggests that relevant, customized cases like those described here are more effective than off-the-shelf solutions in providing instructional benefits to trainees. Certainly, developing such project-specific cases requires close collaboration between ethics experts and roboticists, something that is indeed advocated by proponents of Responsible Research and Innovation [61].
We conclude that, with suitable modifications and appropriate contextualization, the training approach we designed could be usefully adapted for other human–robot interaction projects involving human subjects, to help ensure that the values and principles of research ethics are upheld, and the protection of human subjects is placed at the fore.
Notes
Ethical sensitivity refers to the ability to identify an ethical issue and understand the consequences of decisions made to solve or manage that issue.
The project involves researchers from Italy, the UK, France, Sweden and Japan, caressesrobot.org.
References
United Nations, Department of Economic and Social Affairs PD (2019) World Population Prospects 2019
Feil-Seifer D, Mataric MJ (2005) Defining socially assistive robotics. In: Proceedings of the 2005 IEEE 9th international conference on rehabilitation robotics Chicago, IL, USA
Lehmann H, Syrdal D, Dautenhahn K et al (2013) What should a robot do for you ? Evaluating the needs of the elderly in the UK. In: ACHI 2013—the sixth international conference on advances in computer–human interactions, pp 83–88
Abdi J, Al-Hindawi A, Ng T, Vizcaychipi MP (2018) Scoping review on the use of socially assistive robot technology in elderly care. BMJ Open. https://doi.org/10.1136/bmjopen-2017-018815
Lingler J, Jablonski R, Bourbonniere M, Kolanowski A (2009) Informed consent to research in long-term care settings. Res Gerontol Nurs 2:153–161. https://doi.org/10.3928/19404921-20090428-03
Maas ML, Kelley LS, Park M, Specht JP (2002) Issues in conducting research in nursing homes. West J Nurs Res 24:373–389. https://doi.org/10.1177/01945902024004006
Bruno B, Chong NY, Kamide H et al (2017) Paving the way for culturally competent robots : a position paper. In: 2017 26th IEEE international symposium on robot and human interactive communication (RO-MAN) Lisbon, Portugal
Bruno B, Chong NY, Kamide H et al (2019) The CARESSES EU-Japan project: making assistive robots culturally competent. Lect Not Electr Eng 540:151–169. https://doi.org/10.1007/978-3-030-04672-9_10
Pandey AK, Gelin R (2018) A mass-produced sociable humanoid robot: pepper: the first machine of its kind. IEEE Robot Autom Mag 25:40–48. https://doi.org/10.1109/MRA.2018.2833157
Papadopoulos C, Hill T, Battistuzzi L et al (2020) The CARESSES study protocol: testing and evaluating culturally competent socially assistive robots among older adults residing in long term care homes through a controlled experimental trial. Arch Public Heal. https://doi.org/10.1186/s13690-020-00409-y
Bagdasarov Z, Thiel CE, Johnson JF et al (2013) Case-based ethics instruction: the influence of contextual and individual factors in case content on ethical decision-making. Sci Eng Ethics 19:1305–1322. https://doi.org/10.1007/s11948-012-9414-3
Falkenberg L, Woiceshyn J (2008) Enhancing business ethics: using cases to reach moral reasoning. J Bus Ethics 79:213–217. https://doi.org/10.1007/s10551-007-9381-9
Kolodner JL (1997) Educational implications of analogy: a view from case-based reasoning. Am Psychol 52:57
Kalichman M (2009) Evidence-based research ethics. Am J Bioeth 9:85–87. https://doi.org/10.1080/15265160902923457
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc 310:2191–4. https://doi.org/10.1001/jama.2013.281053
European Commission (2010) European textbook on ethics in research
College SN Required Education in Protecting Human Research Participants. https://www.snc.edu/irb/humansubjects.html
Kalichman M (2014) Rescuing responsible conduct of research (RCR) education. Acc Res 21:68–83. https://doi.org/10.1080/08989621.2013.822271
Sedenberg E, Chuang J, Mulligan D (2016) Designing commercial therapeutic robots for privacy preserving systems and ethical research practices within the home. Int J Soc Robot 8:575–587. https://doi.org/10.1007/s12369-016-0362-y
Lam HR, Chow S, Taylor K et al (2018) Challenges of conducting research in long-term care facilities: a systematic review. BMC Geriatr 18:242. https://doi.org/10.1186/s12877-018-0934-9
Ramos L, van den Hoven E (2015) Balancing ethics in research with older adults and persons with dementia. Paper presented at the OzCHI 2015 workshop on ethical encounters: HCI research in sensitive and complex settings, pp 1–3
Mody L, Miller DK, McGloin JM et al (2008) Recruitment and retention of older adults in aging research. J Am Geriatr Soc 56:2340–2348. https://doi.org/10.1111/j.1532-5415.2008.02015.x.Recruitment
Begun AL, Otto-Salaj LL, Berger L (2018) Participant recruitment and retention in intervention and evaluation research. Oxford University Press, New York
Glesne C (1989) Rapport and friendship in ethnographic research. Int J Qual Stud Educ 2:45–54. https://doi.org/10.1080/0951839890020105
Berkman BE, Chandros Hull S, Eckstein L (2014) The unintended implications of blurring the line between research and clinical care in a genomic age. Person Med 11:285–295
McGuire J (2009) Ethical considerations when working with older adults in psychology. Int J Aviat Psychol 19:112–128. https://doi.org/10.1080/10508420902772702
Bonnie RJ, Wallace RB (2003) Elder mistreatment abuse, neglect and exploitation in an aging America. The National Academies Press, Washington
Resnik DB, Randall D (2018) Reporting suspected abuse or neglect in research involving children. J Med Ethics. https://doi.org/10.1136/medethics-2017-104452
Ragan A, Bowen A (2001) Improving attitudes regarding the elderly population: the effects of information and reinforcement for change. Gerontologist 41:511–515
van Wynsberghe A (2013) Designing robots for care: care centered value-sensitive design. Sci Eng Ethics 19:407–433. https://doi.org/10.1007/s11948-011-9343-6
van Wynsberghe A (2016) Healthcare robots: ethics, design and implementation, 1st edn. Routledge, London
Fosch-Villaronga E (2019) Robots, healthcare, and the law: regulating automation in personal care, 1st edn. Routledge, London
Sharkey A, Sharkey N (2012) Granny and the robots: ethical issues in robot care for the elderly. Ethics Inf Technol 14:27–40. https://doi.org/10.1007/s10676-010-9234-6
Sharkey AJ (2015) Robots and human dignity: a consideration of the effects of robot care on the dignity of older people. Ethics Inf Technol 14:27–40. https://doi.org/10.1007/s10676-014-9338-5
Vallor S (2011) Carebots and caregivers: sustaining the ethical ideal of care in the twenty-first century. Philos Technol 24:251–268. https://doi.org/10.1007/s13347-011-0015-x
Battistuzzi L, Sgorbissa A, Papadopoulos C et al (2018) Embedding ethics in the design of culturally competent socially assistive robots. In: IEEE international conference on intelligent robots and systems
Alzheimer Europe (2010) The ethical issues linked to the use of assistive technology in dementia care—ethical issues in practice—ethics—Alzheimer Europe. In: Alzheimer Eur. http://www.alzheimer-europe.org/Ethics/Ethical-issues-in-practice/2010-The-ethical-issues-linked-to-the-use-of-assistive-technology-in-dementia-care. Accessed 19 Feb 2019
Turkle S (2007) Authenticity in the age of digital companions. Interact Stud 8:501–517
Annas GJ (2003) HIPAA regulations—a new era of medical-record privacy? N Engl J Med. https://doi.org/10.1056/nejmlim035027
EU General Data Protection Regulation (GDPR) Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data
Alvseike H, Brønnick K (2012) Feasibility of the iPad as a hub for smart house technology in the elderly; effects of cognition, self-efficacy, and technology experience. J Multidiscip Healthc 5:299–306. https://doi.org/10.2147/JMDH.S35344
Draucker CB, Martsolf DS, Poole C (2009) Developing distress protocols for research on sensitive topics. Arch Psychiatr Nurs 23:343–350
Fraser SA, Kenyon V, Lagacé M et al (2016) Stereotypes associated with age-related conditions and assistive device use in Canadian media. Gerontologist 56:1023–1032. https://doi.org/10.1093/geront/gnv094
Werhane PH (2002) Moral imagination and systems thinking. J Bus Ethics 38:33–42
Kolodner JL (2014) Case-based reasoning. Morgan Kaufmann, Burlington
Kolodner J, Owensby J, Guzdial M (2004) Case-based learning aids. In: Jonassen D (ed) Handbook of research for educational communications and technology, 2nd edn. Lawrence Erlbaum Associates, Mahwah, pp 829–861
Kim S, Phillips WR, Pinsky L et al (2006) A conceptual framework for developing teaching cases: a review and synthesis of the literature across disciplines. Med Educ 40:867–876. https://doi.org/10.1111/j.1365-2929.2006.02544.x
Johnson JF, Bagdasarov Z, Connelly S et al (2012) Case-based ethics education: the impact of cause complexity and outcome favorability on ethicality. J Empir Res Hum Res Ethics 7:63–77. https://doi.org/10.1525/jer.2012.7.3.63
Menzel DC (2009) Teaching and learning ethical reasoning with cases. Public Integr 11:239–250. https://doi.org/10.2753/pin1099-9922110303
Harkrider LN, MacDougall AE, Bagdasarov Z et al (2013) Structuring case-based ethics training: how comparing cases and structured prompts influence training effectiveness. Ethics Behav 23:179–198. https://doi.org/10.1080/10508422.2012.728470
Plinio AJ, Young JM, McCormick Lavery L (2010) The state of ethics in our society: a clear call for action. Int J Discl Gov 7:172–197
Atkinson TN (2008) Using creative writing techniques to enhance the case study method in research integrity and ethics courses. J Acad Ethics 6:33–50
Currie G (2008) Moving towards reflexive use of teaching cases. Int J Manag Educ 7:41–50. https://doi.org/10.3794/ijme.71.205
Herreid CF (1998) Sorting potatoes for Miss Bonner. J Coll Sci Teach 27:236–239
Watts LL, Medeiros KE, Mulhearn TJ et al (2017) Are ethics training programs improving? A meta-analytic review of past and present ethics instruction in the sciences. Ethics Behav 27:351–384. https://doi.org/10.1080/10508422.2016.1182025
Antes A, Murphy S, Waples E et al (2009) meta-analysis of ethics instruction effectiveness in the sciences. Ethics Behav 19:379–402
Velasquez M, Moberg D, Meyer MJ, Shanks T, McLean MR, DeCosse D, André C, Hanson KO (2009) A framework for thinking ethically. Markkula Center for Applied Ethics at Santa Clara University. http://www.scu.edu/ethics/practicing/decision/framework.html
Nimon K (2014) Explaining differences between retrospective and traditional pretest self-assessments: competing theories and empirical evidence. Int J Res Method Educ 37:256–269
Geldhof GJ, Warner DA, Finders JK et al (2018) Revisiting the utility of retrospective pre-post designs: the need for mixed-method pilot data. Eval Program Plann 70:83–89
Schiekirka S, Anders S, Raupach T (2014) Assessment of two different types of bias affecting the results of outcome-based evaluation in undergraduate medical education. BMC Med Educ 14:149
Carsten B, Coeckelbergh M (2016) Ethics of healthcare robotics: towards responsible research and innovation ethics of healthcare robotics: towards responsible research and innovation. Rob Auton Syst 86:152–161. https://doi.org/10.1016/j.robot.2016.08.018
Acknowledgements
This work was supported by the European Commission Horizon2020 Research and Innovation Program under Grant Agreement n. 737858 (CARESSES).
Funding
This work was supported by the European Commission Horizon2020 Research and Innovation Program under Grant Agreement n. 737858 (CARESSES).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Standards
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee of the Department of Informatics, Bioengineering, Robotics and Systems Engineering at the University of Genoa, Italy, and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Battistuzzi, L., Papadopoulos, C., Hill, T. et al. Socially Assistive Robots, Older Adults and Research Ethics: The Case for Case-Based Ethics Training. Int J of Soc Robotics 13, 647–659 (2021). https://doi.org/10.1007/s12369-020-00652-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12369-020-00652-x