Abstract
Objectives
To assess the diagnostic performance of stress cardiac magnetic resonance (stress CMR) vs stress single-photon emission computed tomography (SPECT) in patients presenting to the emergency department (ED) with chest pain.
Background
SPECT imaging is the most utilized outpatient procedure in the United States. The diagnostic accuracy of SPECT can be limited by soft tissue attenuation and low spatial resolution. Stress CMR has much higher spatial resolution and without the susceptibility to soft tissue attenuation.
Methods
Eighty-seven patients without a history of CAD presenting to the ED with chest pain were prospectively enrolled. Patients underwent both stress CMR and stress SPECT imaging within 12 hours of presentation. Both the stress imaging tests were interpreted immediately for clinical purposes and coronary angiography was performed if either was abnormal. Patients were considered to have significant CAD if identified by angiography (≥50%) or if a cardiac event (cardiac death, myocardial infarction or revascularization) occurred during follow-up (mean 2.6 ± 1.1 years).
Results
Thirty-seven patients were referred for coronary angiography; 29 due to a positive stress test and eight patients for persistent chest pain despite two negative stress tests. There were 22 patients who had significant CAD (≥50%). The remaining patients were followed for 2.6 ± 1.1 years. At the conclusion of the follow-up period, there were four clinical events. The sensitivity, specificity, and diagnostic accuracy of CMR are 85%, 93%, and 89%, respectively. The sensitivity, specificity, and diagnostic accuracy of stress SPECT are 84%, 91%, and 88%, respectively.
Conclusion
Stress CMR has similar diagnostic accuracy as stress SPECT in diagnosis of CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is the leading cause of mortality in the United States, accounting for one of every five deaths in 2005.1 Stress testing has become the primary tool in the diagnosis of CAD; with single-photon emission computed tomography (SPECT) being the prominent imaging modality used today. In the United States alone, 7 million people undergo myocardial perfusion imaging with SPECT every year.2
SPECT imaging, however, has limitations including long scan times and radiation exposure. In addition, it has poor spatial resolution and is prone to attenuation artifacts, which can limit the diagnostic accuracy. Although, in a meta-analysis of the contemporary studies performed between 1990 and 1997, the sensitivity and specificity of SPECT imaging were 87% and 64%, respectively; there have been studies that have reported sensitivity and specificity as low as 65% and 53%.3-5
Stress cardiac magnetic resonance (stress CMR) is a relatively new imaging modality with much higher spatial resolution and a shorter examination time than SPECT and is not prone to soft tissue artifacts. In previous studies, the sensitivity and specificity of stress CMR has been shown to be 93% and 90%, respectively.6,7 However, there are scant data validating these results in a head-to-head comparison of both stress tests performed on the same patient population in the Emergency Department (ED) setting.
We hypothesized that a comprehensive stress CMR study, including evaluation of ventricular wall motion and function, viability, and adenosine stress/rest perfusion will compare favorably to stress SPECT, in the evaluation of patients with intermediate risk for CAD.
Methods
Population
We prospectively recruited patients presenting to the ED with acute chest discomfort deemed to have an intermediate risk of CAD. Intermediate risk was defined as (a) one or more CAD risk factors in a male >40 years old or female >50 years old, or (b) two or more risk factors in a male >30 years old or female >40 years old.8 Risk factors included hypertension, hyperlipidemia, diabetes mellitus, current smoker, or family history of myocardial infarction (MI) prior to age 55. Patients with intermediate risk were chosen to eliminate those with very low probability of CAD in whom stress testing would not be needed to discharge directly from the ED, and also to increase the prevalence of CAD in the study population as the prevalence in all patients presenting to the ED with chest pain has been reported to be as low as 5%.9 Patients at highest risk for CAD, in whom stress testing would be inappropriate, such as those with elevated cardiac enzymes or electrocardiographic ST-segment changes consistent with on-going infarction or ischemia, were excluded. To reduce “spectrum” bias 10 and to provide the best estimates of sensitivity and specificity, we also excluded patients with known CAD, including those with prior MI or revascularization procedures. Other exclusion criteria were aortic stenosis with a mean gradient ≥40 mmHg, second-degree or higher atrioventricular block, pregnancy, hemodynamic or clinical instability, non-cardiac medical problems that could lead to hospital admission, and standard contraindications to CMR.
Written informed consent was obtained in all patients. The study was approved by the institutional review board for research ethics. Support for this study was obtained from a National Institute of Health grant. There were no other sources of funding. The authors are solely responsible for the design and conduct of this study, and also for all study analyses, the drafting and editing of the paper, and its final contents.
Study Protocol and Patient Follow-up
Consecutive patients were recruited on weekdays from 7 AM to 3 PM and when the CMR and SPECT scanner had a capacity for examinations within approximately 3 hours. All patients underwent a comprehensive evaluation including serial cardiac enzymes, serum lipid panel, high-sensitivity C-reactive protein (hsCRP), and serial electrocardiograms. After a second negative troponin level (typically 4 hours after the initial blood draw), patients underwent stress CMR and stress SPECT in random order on the same day. The time between stress imaging tests was no more than 5 hours in all patients. All underwent stress testing within 12 hours of their presentation to the ED. If patients consumed caffeine within 16 hours of the stress test, vasodilator stress tests were switched to dobutamine. Stress imaging studies were clinically interpreted immediately after completion without knowledge of the other stress study result. If either stress study was interpreted as abnormal, the patient was admitted for invasive coronary angiography. If both studies were interpreted as normal, the patient was discharged home and then followed for clinical events (see Figure 1 for patient flow). Clinical follow-up information was obtained via1 telephone interview with the patient, or, if deceased, with family members,2 contact with the patient’s physician, and3 hospital records.
To examine the independent value of stress imaging over the available clinical information, both stress imaging studies were interpreted (independently) a second time, months later, blinded to patient name and all associated clinical information.
Truth Standard for Significant CAD
The truth standard for the presence of significant CAD was pre-specified and was a composite endpoint based on the results of invasive coronary angiography if performed, and the finding of adverse cardiac events during clinical follow-up, if angiography was not performed (Figure 1). An adverse cardiac event was defined as cardiac death, non-fatal MI, or revascularization, and the definition of MI was based on the recent multi-society consensus definition.11 Hospital records were reviewed to confirm this endpoint. Cardiac death was defined as death in the hospital for any cardiac condition or sudden death, defined as death within 24 hours of chest pain or death during sleep.
All x-ray coronary angiograms were analyzed masked to patient identity, clinical information, and stress imaging results. Significant CAD on coronary angiography was defined as >50% luminal narrowing, assessed by percentage of diameter narrowing, relative to adjacent “normal” luminal diameter of at least one major epicardial artery, by visual assessment.
Stress CMR
Acquisition
The stress CMR examination has been described previously.12,13 It consisted of 4 components that were performed in the following order: (a) cine imaging at rest for assessment of left ventricular (LV) function, (b) adenosine gadolinium first-pass imaging for assessment of stress perfusion, (c) repeated first-pass imaging without adenosine 15 minutes later for assessment of rest perfusion, and (d) delayed enhancement imaging for assessment of MI.
CMR was performed on a 1.5-Tesla Siemens scanner using phased-array receiver coils. Details of the individual components are as follows. Cine images were acquired in multiple short-axis (every 10 mm throughout the entire LV) and 3 long-axis views using a steady-state free precession sequence (slice thickness, 6 mm; interslice gap, 4 mm; repetition time (TR), 3.0 ms; echo time (TE), 1.5 ms; temporal resolution, 35-40 ms; flip angle, 60°; in-plane resolution, ~1.7 × 1.4 mm). Following cine imaging, the patient table was partially moved outside the scanner to allow direct patient observation and full access. Adenosine (140 µg·kg−1·min−1) was infused under continuous ECG and blood pressure monitoring for approximately 3 minutes. At 2.5 minutes into the infusion, the patient was re-positioned in the magnet and underwent first-pass perfusion imaging during an infusion of 0.075 mmol·kg−1 gadolinium contrast (Gadoversetamide, [Mallinckrodt, St Louis, MO]) followed by a 50 cc saline flush, both at 4 ml·s−1. Typically 4 short-axis slices (matched to cine locations excluding most basal and apical slices) were obtained per heartbeat using a saturation-recovery, gradient-echo sequence as described previously (TE: 1.1 ms, delay time: 90-110 ms, temporal resolution: 110-125 ms, voxel size: 3.0 × 1.8 × 8 mm, acceleration factor of 2).12,13 Patients were asked to breath-hold during the left ventricular perfusion phase as visualized in real time on the user interface display. Rest perfusion imaging was performed using the same sequence settings and the same dose of contrast 15 minutes later. Finally, delayed enhancement imaging was initiated 5 minutes following rest perfusion imaging using a segmented inversion recovery sequence (slice thickness, 6 mm; interslice gap, 4 mm; TR, 9.5 ms; TE, 3.8 ms; flip angle, 25°; in-plane resolution 1.8 × 1.4 mm) in the identical image planes to cine imaging.14
Analysis
For the immediate clinical interpretation, scans were interpreted by a single reader. For the blinded interpretation, scans were read qualitatively by consensus of 2 experienced readers; a pre-designated third reader was consulted in cases of interpretive discordance. The specific algorithm described by Klem et al12 was used to define an abnormal stress CMR study. In brief, evidence of a stress perfusion defect or delayed enhancement was considered abnormal, unless there were matched stresses and rest perfusion defects without evidence of delayed enhancement. The latter was considered to represent artifactual perfusion defects. The criterion for a perfusion defect was a persistent delay in first-pass myocardial enhancement in more than three consecutive images. Cine findings were considered when perfusion results were equivocal. For the blinded interpretation, CMR scans were placed in random order with identity markers removed.
SPECT Tl-201 and Tc-99m Imaging
Initially, resting myocardial SPECT images were acquired, while the patient was in a supine position with shoulders flexed to 180°, using a GE Millennium MyoSIGHT rotating gamma camera (General Electric Company, Milwaukee, WI). Resting images were performed after receiving thallium (201Tl) (predetermined using a weight-based algorithm) for patients weighing less than 300 lbs using the following parameters: 201Tl dosing up to 4mcI; imaging time: 18 minutes; 36 views/30 seconds per view; matrix 64 × 64; circular; Collimator: LEHR. Patients weighing greater than 300 lbs underwent resting images with technetium (Tc-99m), but followed the same parameters with the exception of a dosing rate of 12-15 mcI. Stress imaging for patients less than 300 lbs was performed with Tc-99m and used the following parameters: Tc-99 m dosing range 24-35mcI; imaging time: 15 minutes; 36 views/25 seconds per view; matrix 64 × 64; circular; 16 frames/RR interval. Again, the same parameters were used for patients weighing over 300 lbs, only the dosing ranged from 35 to 40 mcI.
Treadmill Exercise Testing
All treadmill tests were conducted using either the Bruce or Modified Bruce protocols (GE Medical Systems CASE Stress System Version 5 with Series 2000 Marquette Treadmill, General Electric Company, Milwaukee, WI). End points of exercise were predetermined according to absolute and relative indications for terminating exercise testing.15 One minute prior to peak exercise, patients received Tc-99m (weight-based) and were imaged 15 to 20 minutes post exercise. All 12 leads of the standard ECG were monitored and used for analysis. ST measurements were assessed visually 80 ms post J-point during exercise or recovery with the PR segments used as the baseline. The criteria for determining a positive exercise ST-segment response were as follows: ≥1.0 mm horizontal or downsloping depression 80 ms post J-point in at least three consecutive beats.
Statistical Analysis
Continuous data are reported as mean ± standard deviation (SD). Two sample t-tests were used to assess differences in continuous variables and Fisher’s Exact tests were used to assess differences in discrete variables. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of CMR stress perfusion and stress SPECT for the detection of CAD were compared using McNemar’s Chi square tests. All statistical tests were two-tailed; P < .05 was regarded as significant.
Results
Baseline Characteristics
A total of 87 patients were prospectively enrolled, and all completed both the stress tests. Two patients were deemed to have non-interpretable SPECT image quality, and were excluded. The remaining 85 patients were included in the analysis, and had a mean age of 56 ± 7 years and 59 (69%) were male. Over half of the patients had hypertension or dyslipidemia, just under a quarter of the patients were diabetic, and a third had a family history of premature CAD (Table 1).
Twenty-six patients had significant CAD, 22 patients with significant stenosis on coronary angiography, and four patients had a clinical event on follow-up (1 MI, and three revascularizations).
On comparing patients with and without CAD, the patients with CAD were significantly older (59 ± 7 vs 54 ± 7) and had a higher prevalence of diabetes (32% vs 17%). There was no significant difference with regard to gender, history of hypertension, dyslipidemia, family history of premature CAD, or smoking (Table 1).
Evaluation for CAD
Twenty-nine out of 85 patients were found to have either a positive stress CMR and/or positive stress SPECT; all patients with the positive stress test were referred for coronary angiography. Another eight patients with both the stress tests being normal were referred for coronary angiography after discussion with their physician because of recurrent chest pain within 6 weeks of recruitment, and all of them were negative for significant CAD. The remaining 48 patients with both stress tests being normal were followed for a mean of 2.6 ± 1.1 years (Figure 1). Forty-two patients did not have any cardiac event throughout the follow-up period. Two patients were lost to clinical follow-up; however, both were alive according to the National Death Index. One patient died of metastatic prostate cancer. One patient had a MI and three patients underwent a coronary revascularization procedure.
Stress SPECT Results
Stress SPECT imaging was completed in all of the 87 enrolled patients; in two patients, image quality was deemed non-interpretable and they were excluded from analysis. Fifty-four patients had exercise SPECT and 33 patients had persantine SPECT. Twenty-two patients (26%) had a positive SPECT study. Sixteen out of the 22 patients with a positive SPECT were found to have had significant CAD on coronary angiography (Figures 2, 3, and 4).
Of the 63 patients who had negative stress SPECT, one patient was found to have CAD on coronary angiography (referred because of positive stress CMR) and two patients had an adverse cardiac event on follow-up (total three patients with false negative test), leading to a sensitivity, specificity, PPV, NPP, and diagnostic accuracy of 84%, 91%, 72%, 95%, and 88%, respectively. In the patients who underwent exercise SPECT, the target heart rate was achieved in 82%. The patients who did not achieve the 75% of the target heart rate were changed to pharmacologic stress.
Stress CMR Results
CMR stress testing was completed in all of the eighty-seven enrolled patients. Of the eighty-five patients used in the study analysis, 21 (25%) had a positive stress CMR and 64 had negative stress CMR for CAD on blinded analysis.
Of the 21 patients with positive stress CMR, 17 patients were found to have CAD with coronary angiography. Out of the 64 patients with a negative stress CMR, three patients had an adverse cardiac event at the end of the follow‐up period (3 false negative a negative studies), leading to sensitivity, specificity, PPV, NPV, and diagnostic accuracy of 85%, 93%, 81%, 95%, and 89%, respectively.
We found no significant difference in sensitivity, specificity, or diagnostic accuracy of both stress CMR and stress SPECT for detection of CAD, (Table 2). In assessing the concordance between the two studies, the correlation coefficient between the 2 test by Fisher’s Exact test was r = 0.79, P < .001.
Discussion
In patients with suspected coronary heart disease, SPECT is the most widely used test for the assessment of myocardial ischemia, but its diagnostic accuracy is reported to be variable and it exposes patients to ionizing radiation. Stress CMR has emerged as a potential modality for the diagnosis and risk stratification of patients with documented or suspected CAD. Our study demonstrates that a comprehensive CMR protocol incorporating adenosine stress perfusion imaging is not only safe and accurate but also has similar diagnostic performance to stress SPECT with similar sensitivity, specificity, and diagnostic accuracy without the hazards of radiation exposure. The sensitivity (85%) and specificity (93%) of stress CMR were obtained in a patient population that had an intermediate pretest probability of having significant CAD. This is an important concept since it reflects the actual benefit of stress test application in clinical practice. We excluded patients with both high and low pretest probability of having CAD in order to reduce pretest referral bias, which can inappropriately affect the sensitivity and specificity of the test. In addition, we excluded patients with prior myocardial infarction or known history of CAD as this could artificially increase the sensitivity of the tests.
Our study highlights several important points: First it is done in patients presented to the ED with chest pain that required further evaluation by stress testing. This may pave the way for stress CMR to be considered as a good rule-out test in patients presenting with possible acute coronary syndrome as it is safe and quick with high diagnostic performance. Second, we interpreted both stress CMR and stress SPECT qualitatively by visual assessment. This is an important aspect for stress CMR to become part of the routine clinical practice. Finally, we demonstrated very good agreement between stress SPECT and stress CMR in the same patient population.
In this study, patients underwent coronary angiography when either stress CMR or stress SPECT on immediate clinical interpretation was abnormal. We chose this study design to allow patients with normal stress imaging results (on one modality) to undergo angiography, and thereby reduce post-test “verification” bias.16 Nonetheless, patients who had normal results on both the stress tests did not undergo coronary angiography. Thus, we also required systematic patient follow-up to track clinical events and additional cardiac workup, if any, for recurrent chest pain. We surmised that our definition of a “true negative,” which required both the initial stress interpretations to be negative and also follow-up to be negative, would lead to a very low rate in which patients with significant CAD would be missed.
Comparison with Other Studies
The sensitivity and specificity of stress CMR, in our study, were comparable to other published data with sensitivities ranging from 83% to 88% and specificity ranging from 85% to 89%.15,17,18 In prior studies, stress CMR did very well compared to stress SPECT in diagnosing CAD. Ishida et al19 compared stress CMR perfusion and SPECT in 69 patients who also underwent catheter-based x-ray angiography and found a significantly greater area under the receiver-operating characteristic curve for CMR perfusion imaging compared with that in SPECT. Sakuma et al20 found superior but not statistically significant diagnostic accuracy for perfusion imaging compared with that in SPECT in 40 patients. More recently these results were confirmed on two large-scale prospective trials: the (MR-IMPACT) and the CE-MARC trials. The MR-Impact trial examined the diagnostic performance of perfusion-CMR vs SPECT in 214 patients and the authors reported that perfusion-CMR is superior to SPECT in the entire study population21 The CE-MARC trial is the largest, prospective stress CMR trial to date that enrolled 752 patients and the investigators reported that stress CMR has higher diagnostic accuracy compared to SPECT in diagnosing CAD.22 Moreover, the recently published MR-IMPACT II trial which was designed to assess the superiority of stress CMR compared to stress SPECT in diagnosing CAD showed that stress CMR has superior sensitivity, while stress SPECT has superior specificity in 533 patients.23 The favorable capabilities of stress CMR perfusion imaging are likely due to superior spatial resolution compared with that in SPECT allowing for the distinction between subendocardial and transmural defects, which is important because subendocardial perfusion defects can indicate ischemia at an early stage. Some of the previous studies, however, employed quantitative assessment of stress CMR perfusion, which entails laborious, time-consuming post-processing. In our study, we used visual evaluation to reflect the real clinical practice and to fit the requirement for a rapid diagnostic test with high diagnostic accuracy to evaluate ED patients.
This study and prior studies used cardiac catheterization as a gold standard. In three studies that compared stress CMR to positron emission tomography (PET) and SPECT, there was higher agreement between stress perfusion-CMR and either PET or SPECT, than between stress CMR and cardiac catheterization, suggesting that cardiac catheterization may not be the best gold standard in the evaluation of ischemia.12,18,24 Future studies, including MR-INFORM)25 and (CE-MARC-2),26 will expand the evidence base for CMR compared with fractional flow reserve and importantly both are multicenter and multivendor trials.
Advantages and Disadvantages of CMR vs SPECT
Stress CMR is becoming a well-validated stress perfusion imaging modality that has a higher spatial resolution than SPECT; however, the prognostic data in the cardiac CMR literature, although growing, are not as robust as SPECT. Practical advantages of stress CMR include a relatively short examination time as compared to stress SPECT (most studies were completed within 45 minutes), no ionizing radiation, and good safety and tolerability (no adverse events in this study), particularly with the abbreviated infusion time of adenosine (3 minutes maximum). In addition, the ability to obtain high-resolution pictures in patients with a large body habitus and the ability to visualize the aorta to rule out dissection are two important advantages of stress CMR. Finally, stress CMR has the ability to detect myocardial infarction long after serologic markers return to normal. Practical disadvantages of stress CMR include the small bore resulting in limitation of body habitus and claustrophobia. Other disadvantages are an inability to perform the test at the bedside as well as perfusion imaging artifacts. Probably the most important disadvantage to stress CMR is the inability to assess functional capacity.
Practical disadvantages of stress SPECT include moderate temporal resolution, limited spatial resolution; longer scan time, lack of anatomical landmarks, and radiation exposure.27 In a study of patient exposure to low-dose ionizing radiation, myocardial perfusion imaging had the highest average effective dose (15.6 millisieverts) and the highest percentage (22.1%) of all effective doses to the entire patient population from all major radiologic procedures.28
Limitations
There are a few limitations of this study, including the relatively low prevalence of disease. Although we specifically identified intermediate risk patients, there were still only 29 patients found to have significant CAD. Secondly, cardiac catheterization as a gold standard has its problems. There may be a subgroup of patients that have endothelial dysfunction, or syndrome X, with a normal epicardial disease by coronary angiography. The use of 50% stenosis as a cut off for CAD could be considered too low and performing fractional flow reserve might have improved the accuracy of the gold standard. Another potential limitation is that the stress laboratory protocol is to use dual isotope which some consider inferior to single isotope. In addition, analysis was performed on the patient level and not on the coronary artery level which could lead to a patient having a positive anterior wall ischemia but on coronary catheterization having right coronary artery stenosis and this patient would be considered a true positive study. Finally, the study is subjected to the common verification bias where a patient with positive stress test went for cardiac catheterization, while patients with negative test were just followed up for cardiac events. We found it inappropriate to refer patients for coronary angiography when they have 2 negative stress tests and attempted to address this by following these patients for clinical events over 2½ years. Although this is not an ideal gold standard, we feel it adequate as patients who have 2 negative stress tests that both have a sensitivity of approximately 85-90% and have no clinical events on 2½ year follow-up are unlikely to have significant CAD.
New knowledge gained
We are reporting similarly high diagnostic accuracy for Stress CMR and Stress SPECT in patients presenting to the ED with chest pain and intermediate pretest probability.
Conclusion
Stress CMR has comparable diagnostic performance to stress SPECT in patients at intermediate risk for CAD presenting to the ED with chest pain.
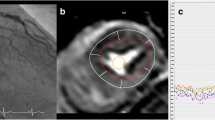
An example of a patient with abnormal stress CMR showing subendocardial inferolateral perfusion defect. Invasive angiography showed critical stenosis of a large obtuse marginal branch. Stress nuclear imaging of the same patient showed no perfusion abnormalities.
Abbreviations
- CAD:
-
Coronary artery disease
- CE-MARC:
-
Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease: a prospective trial
- ECG:
-
Electrocardiogram
- ED:
-
Emergency department
- hsCRP:
-
High-sensitivity C-reactive protein
- LV:
-
Left ventricular
- MI:
-
Myocardial infarction
- MR-IMPACT:
-
Comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicenter, multivendor, randomized trial
- MR-IMPACT II:
-
Magnetic resonance imaging for myocardial perfusion assessment in coronary artery disease trial: perfusion-cardiac magnetic resonance vs single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicenter, multivendor trial
- NPV:
-
Negative predictive value
- PET:
-
Positron emission tomography
- PPV:
-
Positive predictive value
- SPECT:
-
Single-photon emission computed tomography
- Stress CMR:
-
Stress cardiac magnetic resonance
- TE:
-
Echo time
- TR:
-
Repetition time
References
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics—2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:e21-181.
Wackers FJ. Diabetes and coronary artery disease: The role of stress myocardial perfusion imaging. Cleve Clin J Med 2005;72:9-33.
Fleischmann KE, Hunink MG, Kuntz KM, Douglas PS. Exercise echocardiography or exercise SPECT imaging? A meta-analysis of diagnostic test performance. J Nucl Cardiol 2002;9:133-4.
Miller TD, Hodge DO, Christian TF, Milavetz JJ, Bailey KR, Gibbons RJ. Effects of adjustment for referral bias on the sensitivity and specificity of single photon emission computed tomography for the diagnosis of coronary artery disease Am J Med. 2002;112:290-7.
Stewart RE, Schwaiger M, Molina E, Popma J, Gacioch GM, Kalus M, et al. Comparison of rubidium-82 positron emission tomography and thallium-201 SPECT imaging for detection of coronary artery disease. Am J Cardiol 1991;67:1303-10.
Giang TH, Nanz D, Coulden R, Friedrich M, Graves M, Al-Saadi N, et al. Detection of coronary artery disease by magnetic resonance myocardial perfusion imaging with various contrast medium doses: First European multi-centre experience. Eur Heart J 2004;25:1657-65.
Nagel E, Klein C, Paetsch I, Hettwer S, Schnackenburg B, Wegscheider K, et al. Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation 2003;108:432-7.
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 2007;50:e1-157.
Saddichha S, Saxena MK. Is every chest pain a cardiac event?: An audit of patients with chest pain presenting to emergency services in India. Intern Emerg Med 2009;4:235-9.
Ransohoff DF, Feinstein AR. Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med 1978;299:926-30.
Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, et al. Universal definition of myocardial infarction. Circulation 2007;116:2634-53.
Klem I, Heitner JF, Shah DJ, Sketch MH Jr, Behar V, Weinsaft J, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol 2006;47:1630-8.
Klem I, Greulich S, Heitner JF, Kim H, Vogelsberg H, Kispert EM, et al. Value of cardiovascular magnetic resonance stress perfusion testing for the detection of coronary artery disease in women. JACC Cardiovasc Imaging 2008;1:436-45.
Kim RJ, Shah DJ, Judd RM. How we perform delayed enhancement imaging. J Cardiovasc Magn Reson 2003;5:505-14.
Medicine ACoS. ACSM’s guidelines for exercise testing and prescription. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. p. 106.
Hachamovitch R, Di Carli MF. Methods and limitations of assessing new noninvasive tests: Part I: Anatomy-based validation of noninvasive testing. Circulation 2008;117:2684-90.
Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined—A consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959-69.
Lauerma K, Virtanen KS, Sipila LM, Hekali P, Aronen HJ. Multislice MRI in assessment of myocardial perfusion in patients with single-vessel proximal left anterior descending coronary artery disease before and after revascularization. Circulation 1997;96:2859-67.
Ishida N, Sakuma H, Motoyasu M, Okinaka T, Isaka N, Nakano T, et al. Noninfarcted myocardium: Correlation between dynamic first-pass contrast-enhanced myocardial MR imaging and quantitative coronary angiography. Radiology 2003;229:209-16.
Sakuma H, Suzawa N, Ichikawa Y, Makino K, Hirano T, Kitagawa K, et al. Diagnostic accuracy of stress first-pass contrast-enhanced myocardial perfusion MRI compared with stress myocardial perfusion scintigraphy. AJR Am J Roentgenol 2005;185:95-102.
Schwitter J, Wacker CM, van Rossum AC, Lombardi M, Al-Saadi N, Ahlstrom H, et al. MR-IMPACT: Comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J 2008;29:480-9.
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): A prospective trial. Lancet 2012;379:453-60.
Schwitter J, Wacker CM, Wilke N, Al-Saadi N, Sauer E, Huettle K, et al. MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: Perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 2013;34:775-81.
Matheijssen NA, Louwerenburg HW, van Rugge FP, Arens RP, Kauer B, de Roos A, et al. Comparison of ultrafast dipyridamole magnetic resonance imaging with dipyridamole SestaMIBI SPECT for detection of perfusion abnormalities in patients with one-vessel coronary artery disease: assessment by quantitative model fitting. Magn Reson Med 1996;35:221-8.
Hussain ST, Paul M, Plein S, McCann GP, Shah AM, Marber MS, et al. Design and rationale of the MR-INFORM study: Stress perfusion cardiovascular magnetic resonance imaging to guide the management of patients with stable coronary artery disease. J Cardiovasc Magn Reson 2012;14:65.
Ripley DP, Brown JM, Simon Walker PB, Sculpher M, McCann GP, Berry C, et al. Rational and design of the Clinical Evaluation of Magnetic Resonance Imaging in Coronary heart disease 2 trial (CE‐MARC 2): a prospective, multicenter, randomized trial of diagnostic strategies in suspected coronary heart disease. Am Heart J 2015;169:17-24.e1.
Ibrahim DY, DiFilippo FP, Steed JE, Cerqueira MD. Optimal SPECT processing and display: Making bad studies look good to get the right answer. J Nucl Cardiol 2006;13:855-66.
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, et al. Exposure to Low-Dose Ionizing Radiation from Medical Imaging Procedures. N Engl J Med 2009;361:849.
Conflicts of interest
There were no conflicts of interest or outside funding for this project.
Disclosure
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-015-0225-1
Funding
This study did not receive any funding from any sources.
Rights and permissions
About this article
Cite this article
Ahmad, I.G., Abdulla, R.K., Klem, I. et al. Comparison of stress cardiovascular magnetic resonance imaging (CMR) with stress nuclear perfusion for the diagnosis of coronary artery disease. J. Nucl. Cardiol. 23, 287–297 (2016). https://doi.org/10.1007/s12350-015-0242-0
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0242-0