Abstract
The overexpression of mutant p53 stimulates serum p53 antibody production in patients with colorectal carcinoma even in superficial tumors. Although the short-term perioperative monitoring of serum p53 antibody titers is reported to be useful in predicting tumor recurrence and patient survival in colorectal carcinoma, the clinical utility of the long-term monitoring of serum p53 antibody titers in patients with colorectal cancer remains unknown. Here, we report the 3-year monitoring of serum p53 antibody titers in a 60-year-old man with rectal cancer, clinical stage IV (T2N2M1b, lung and liver metastases), who was treated with chemotherapy and surgery. Screening tests for CEA (29.4 ng/ml), CA19-9 (41.1 U/ml), and serum p53 antibody (2170 U/ml) were positive before treatment. After chemotherapy with mFOLFOX6 + bevacizumab (B-mab), CEA and CA19-9 decreased to the normal range. However, serum p53 antibody titer remained positive (283 U/ml). After low anterior resection, the serum p53 antibody titer still remained positive (63.4 U/ml). Serum p53 antibody titer significantly changed and was associated with treatment response and tumor recurrence. In the last 6 months of the patient’s life, serum p53 antibody titer gradually decreased, which possibly reflects the modification of the patient’s immune response to p53 antigens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serum CEA and CA19-9 in rectal cancer patients are useful for establishing diagnosis, estimating prognosis, monitoring treatment, and detecting tumor recurrence [1]. The overexpression of mutant p53 stimulates the production of serum p53 IgG antibodies (s-p53-Abs) in patients with colorectal carcinoma [2–5], even when the tumors are superficial [6]. We previously reported that a highly sero-positive patient had a poor survival outcome in esophageal carcinoma [7]. The short-term perioperative monitoring of s-p53-Ab titers is considered to be useful in predicting tumor recurrence and patient survival in colorectal carcinoma [6, 8, 9]. These reports support the clinicopathological significance of s-p53-Ab titers in surgically treated patients with colorectal carcinoma. However, the clinical utility of long-term monitoring of s-p53-Ab titer for patients with colorectal carcinoma treated with chemotherapy combined with surgery remains unknown. Here we demonstrate fluctuations in s-p53-Ab titers for more than 3 years in a patient with rectal cancer and demonstrate its utility in understanding the patient’s tumor load during chemotherapy and surgery. Furthermore, we observed a paradoxical trend in the s-p53-Ab titers during the last several months of patient’s life; this report discusses this interesting phenomenon.
Case report
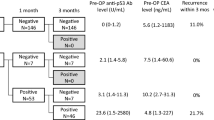
A 60-year-old man was diagnosed with a type 2 rectal cancer with liver and lung metastases (Fig. 1a, b). Biopsy revealed a moderately differentiated adenocarcinoma with p53 overexpression (Fig. 1c). S-p53-Ab titers were assessed using enzyme-linked immunosorbent assay (ELISA; MESACUP anti-p53 Test; Medical and Biological Laboratories Co. Ltd., Nagoya, Japan) [1]. Serum tumor markers revealed that CEA (29.4 ng/ml), CA19-9 (41.1 U/ml), and s-p53-Ab (2170 U/ml) were all positive before treatment. Because of the very advanced tumor stage for surgery, systemic chemotherapy was applied as the first treatment. Eleven courses of mFOLFOX6 + bevacizumab were administered as first-line chemotherapy. This resulted in shrinkage of the primary tumor. Although all serum markers gradually decreased, s-p53-Ab remained elevated at more than 250 U/ml (Fig. 2). The CEA and CA19-9 levels soon decreased to within normal range, whereas the elevated s-p53-Ab titer was the only positive marker for monitoring treatment response. Low anterior resection and partial hepatectomy were performed 7 months after treatment initiation. Thereafter, 27 courses of FOLFIRI + bevacizumab or cetuximab were administered. Although s-p53-Ab remained elevated at more than 30 U/ml, CA19-9 and CEA stayed within the normal range, (Fig. 2).
Right lung metastatic lesions significantly grew 21 months after treatment initiation (Fig. 3a); therefore, partial lobectomy was performed. Although serum markers transiently decreased after lung resection, rapid increases were observed at the moment of metastatic lesion recurrence (Fig. 3b). Even after radiation and chemotherapy, multiple metastatic lesions rapidly developed (Fig. 3c), and the patient died 38 months after the initiation of first chemotherapy treatment. Following the second regrowth, although CEA and CA19-9 levels began to increase, the s-p53-Ab titer gradually decreased during the last phase of the patient’s life.
This study was approved by the institutional review boards of Toho University School of Medicine (#22-112). Written informed consents were obtained from the patient.
Discussion
Only a few patients with colorectal carcinoma exhibit s-p53-Ab titers greater than 100 U/ml and very rarely do cases exhibit s-p53-Ab titers greater than 1000 U/ml. Typically, patients with more advanced tumors exhibit such high titers. Moreover, because serum titer is significantly associated with tumor load, the trend of s-p53-Ab titer may reflect treatment response. Because there is a significant association between s-p53-Ab and mutations in TP53, tumors which precipitate extremely high s-p53-Ab titers may be more resistant to chemotherapy and/or radiotherapy [10]. In the present case, the rapid decrease in s-p53-Ab titer, even though it remained above the cutoff value, may indicate a good response to first-line chemotherapy (mFOLFOX6 + B-mab). In this case, residual adenocarcinoma cells and treatment responses were clearly detected through the monitoring of s-p53-Abs. Because the specificity of this marker is greater than 95% [2], we believe that s-p53-Abs may be useful for detecting residual cancer cells and predicting tumor recurrence. In our previous study, we observed patients with esophageal carcinoma whose s-p53-Ab titers did not decrease after treatment, and who showed significantly poorer survival than those with decreased s-p53-Ab titers [11]. In the present case, the s-p53-Ab titer was consistently positive, even after the negative conversion of CA19-9. Therefore, s-p53-Ab could reflect the response to residual lung metastases.
Patients with more advanced stage tumors frequently have very high p53 antibody titers [8]. The present case suggests that p53 antibody concentrations gradually decrease; therefore, patients with extremely high antibody titers will tend to have detectable antibody concentrations for a long period. In the present case, the rapid reduction in s-p53-Ab titers after surgery may be associated with the near complete clearance of cancer cells. Patients with extremely high s-p53-Ab titers are more likely to have tumors that are resistant to chemotherapy and/or radiation therapy [12]. However, in this case, chemotherapy seemed to be effective after it was initially implemented. In addition, changes in s-p53-Ab titers precisely reflected the treatment response. As ELISA is quick and easy in detecting p53 alteration in cancer cells, the perioperative monitoring of s-p53-Ab titers may prove to be useful for identifying the presence of residual cancer cells and predicting long-term surgical outcomes. Although further studies are required to gain a more precise understanding of the clinical implications of s-p53-Ab titers in rectal adenocarcinoma, this case shows that the monitoring of s-p53-Ab titers during chemotherapy and/or surgery may be a useful tool for the management of residual cancer cells. The changes in CEA and CA19-9 levels could be explained by the associated changes in the primary tumor load. The reason why s-p53-Ab titer remained elevated during the entire treatment course was probably because of its significant association with residual cancer cells.
After the first tumor regrowth, the CEA and CA19-9 titer began to increase. In contrast, the s-p53-Ab titer gradually decreased, even after the second regrowth. Such a paradoxical decrease during the last several months of life might reflect a modification of the immune response to p53 antigen and was not reflective of the treatment response but was due to a generalized deterioration of the patient’s immune response [13]. This paradoxical changing of serum titers should be investigated in further studies in the future. Therefore, combination tests of s-p53-Ab with CEA and CA19-9 might be important in diagnosing the appropriate time point for intensive treatment to switch to palliative care.
In conclusion, this case report follows the perioperative and long-term trends of s-p53-Ab titers in a patient with rectal adenocarcinoma treated with chemotherapy, followed by surgery. This is the first case report to show the results of the long-term monitoring of s-p53-Ab titers for more than 3 years, after the initiation of combination treatments for a patient with rectal adenocarcinoma.
References
Shimada H, Noie T, Ohashi M, Oba K, Takahashi Y. Clinical significance of serum tumor markers for gastric cancer: a systematic review of literature by task force of Japanese Gastric Cancer Association. Gastric Cancer. 2014;17:26–33.
Shimada H, Ochiai T, Nomura F, Japan p53 Antibody Research Group. Titration of serum p53 antibodies in 1,085 patients with various types of malignant tumors: a multi-institutional analysis by the Japan p53 Antibody Research Group. Cancer. 2003;97:682–9.
Zhang J, Xu Z, Yu L, Chen M, Li K, et al. Assessment of the potential diagnostic value of serum p53 antibody for cancer: a meta-analysis. PLoS One. 2014;9:e99255. doi:10.1371/journal.pone.0099255.
Yamaguchi T, Takii Y, Maruyama S. Usefulness of serum p53 antibody measurement in colorectal cancer: an examination of 1384 primary colorectal cancer patients. Surg Today. 2014;44:1529–35.
Ochiai H, Ohishi T, Osumi K, Tokuyama J, Urakami H, Seki S, et al. Reevaluation of serum p53 antibody as a tumor marker in colorectal cancer patients. Surg Today. 2012;42:164–8.
Takeda A, Shimada H, Nakajima K, et al. Serum p53 antibody as a useful marker for monitoring of treatment of superficial colorectal adenocarcinoma after endoscopic resection. Int J Clin Oncol. 2001;6:45–9.
Shimada H, Nabeya Y, Okazumi S, Matsubara H, Funami Y, Shiratori T, et al. Prognostic significance of serum p53 antibody in patients with esophageal squamous cell carcinoma. Surgery. 2000;132:41–7.
Tang R, Yeh CY, Wang JY, et al. Serum p53 antibody as tumor marker for follow-up of colorectal cancer after curative resection. Ann Surg Oncol. 2009;16:2516–23.
Kawahara H, Watanabe K, Enomoto H, et al. Normalization of serum p53 antibody levels in patients after curative resection for colorectal cancer. Anticancer Res. 2013;33:2221–5.
Shimada H, Okazumi S, Takeda A, Nabeya Y, Matsubara H, Funami Y, et al. Presence of serum p53 antibodies is associated with decreased in vitro chemosensitivity in patients with esophageal cancer. Surg Today. 2001;31:591–6.
Shimada H, Shiratori T, Takeda A, Matsushita K, Okazumi S, Akutsu Y, et al. Perioperative changes of serum p53 antibody titer is a predictor for survival in patients with esophageal squamous cell carcinoma. World J Surg. 2009;33:272–7.
Lechpammer M, Lukac J, Lechpammer S, Kovacević D, Loda M, Kusić Z. Humoral immune response to p53 correlates with clinical course in colorectal cancer patients during adjuvant chemotherapy. Int J Colorectal Dis. 2004;19:114–20.
Shimada H, Nagata M, Nabeya Y, et al. Paradoxical changing of serum p53 antibody titers during chemotherapy for a stage IV esophageal squamous cell carcinoma. Int Canc Conf J. 2014;44:1957–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
Hideaki Shimada received research Grant from Medical and Biological Laboratories, co. ltd. The other co-authors declare that they have no conflict of interest.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments.
Informed Consent:
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Suzuki, T., Shimada, H., Ushigome, M. et al. Three-year monitoring of serum p53 antibody during chemotherapy and surgery for stage IV rectal cancer. Clin J Gastroenterol 9, 55–58 (2016). https://doi.org/10.1007/s12328-016-0633-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-016-0633-z