Abstract
Introduction
The efficacy and safety of rivaroxaban for the prevention of stroke and systemic embolism have been demonstrated in Asian and non-Asian patients with non-valvular atrial fibrillation (NVAF) in multiple studies. However, limited published data exist on its use specifically in treatment-naïve patients from the Asia region. Patients in South Korea and Taiwan can now receive rivaroxaban as first-line therapy, allowing for data generation in this patient group.
Methods
XaMINA was a prospective, real-world, multicenter, single-arm, observational cohort study of patients with NVAF in South Korea and Taiwan naïve to anticoagulation and initiating rivaroxaban. The primary outcome was major bleeding; secondary outcomes included all-cause mortality, symptomatic thromboembolic events, and treatment persistence.
Results
In total, 1094 patients were included and the follow-up was 1 year. The baseline mean CHADS2 score was 1.63 ± 0.98, mean CHA2DS2-VASc score was 2.92 ± 1.42, and mean HAS-BLED score was 1.00 ± 0.75. The primary outcome occurred in 20 (1.8%) patients [incidence rate 2.1 events per 100 patient-years (95% CI 1.35–3.25)]. Thromboembolic events occurred in 9 (0.8%) patients, of whom 5 (0.5%) had stroke, 3 (0.3%) myocardial infarction, and 1 (0.1%) a transient ischemic attack. There were no cases of non-central nervous system systemic embolism, and 735 (67.2%) patients persisted with rivaroxaban treatment for 1 year.
Conclusion
XaMINA demonstrated low incidence rates of major bleeding events and thromboembolic events in patients with NVAF newly initiating rivaroxaban in South Korea and Taiwan, consistent with previous real-world studies reconfirming the results of the ROCKET AF study.
Trial Registration
The trial was registered on ClinicalTrials.gov (identifier NCT03284762) on 15 September 2017.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The XaMINA study investigated the safety profile of rivaroxaban in treatment-naïve patients with non-valvular atrial fibrillation from South Korea and Taiwan |
The incidence rates of major bleeding and thromboembolic events in XaMINA were low and consistent with the data from previous real-world studies and phase III trials |
Introduction
The global prevalence of atrial fibrillation (AF) was estimated at 33 million in 2010, and this number is only expected to increase with time [1, 2]. In Asia alone it is expected that there will be 72 million patients with AF by the year 2050, which will be more than the number of cases in Europe and the USA combined [3].
AF is associated with a 2- to 3.5-fold increase in the risk of stroke compared with those without the condition [1]. Anticoagulant therapy is widely used in order to reduce the risk of stroke in patients with AF [4]. Randomized controlled trials of the direct oral anticoagulants (DOACs; rivaroxaban, dabigatran, apixaban, and edoxaban), including the ROCKET AF study of rivaroxaban [5,6,7,8], have resulted in their approval for the prevention of stroke and systemic embolism (SE) in patients with AF across multiple geographic regions, including South Korea and Taiwan [9, 10].
Subsequent observational studies, including several using data from the Korean and Taiwanese National Health Insurance databases, have shown that DOACs also demonstrate a consistent safety profile across the heterogeneous patient groups encountered in routine clinical practice [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Most of these studies were retrospective in nature. However, the XANTUS program of studies, which investigated the global real-world use of rivaroxaban for stroke prevention in patients with non-valvular AF (NVAF), collectively represents the largest prospective, observational study in this setting (n = 11,121) [27].
Asian patients with AF are at an increased risk of stroke, particularly hemorrhagic stroke, compared with White patients [28]. However, in Asian patients, antiplatelet agents have been favored over oral anticoagulants for stroke prevention, despite concerns regarding both their safety and effectiveness in this setting [28]. This is partly due to antiplatelet agents being considered a safer treatment option; higher incidence rates of bleeding have been associated with the use of vitamin K antagonists (VKAs) in Asian patients compared with non-Asian patients [3].
DOACs are at least as effective as VKAs, with a lower risk of particularly serious types of major bleeding in both Asian and non-Asian populations. The J-ROCKET AF study in Japanese patients [29], and a subanalysis of patients from South Korea and Taiwan in the phase III ROCKET AF study [30], demonstrated a consistent efficacy and safety profile with rivaroxaban versus VKA in an East Asian population. Further, the XANAP observational study [31], part of the international XANTUS program [32] (which also included XANTUS [11, 32] and XANTUS-EL [33]), demonstrated low incidence rates of major bleeding and stroke in patients with AF receiving rivaroxaban in clinical practice, as did the XAPASS study in Japanese patients [34]. These findings were consistent with those from the wider XANTUS program [11, 27]. Similar findings, for rivaroxaban and for the DOAC class in general, have been obtained from analyses of data from both the Korean and Taiwanese National Health Insurance databases [15,16,17,18,19,20,21,22,23,24,25,26]. Subanalyses of the primary trials of apixaban, dabigatran, and edoxaban have also all shown that they demonstrate similar efficacy and safety in Asian patients compared with overall patient populations [35] or non-Asian populations [36, 37]. Of particular note, the DOACs were associated with lower or comparable risks of intracranial hemorrhage, hemorrhagic stroke, and fatal bleeding versus VKA in both the overall study populations [5,6,7,8] and Asian subgroups [35,36,37].
In the XANAP study, 13.5% of patients from South Korea and 23.1% from Taiwan were treatment naïve. This is smaller than the 36.3% seen in the overall XANAP patient population [31] and the 31.8% in the pooled XANTUS program population [27]. For South Korea, this was likely the result of the reimbursement policy, which, at the time XANAP was conducted and until recently, only allowed for the reimbursement of rivaroxaban after failure of an alternative treatment [38]. However, it is not clear why such a low proportion of patients from Taiwan were treatment naïve. This was in contrast with both local treatment guidelines [39, 40] and the international European Society of Cardiology/European Heart Rhythm Association guidelines [41], which recommend the use of a DOAC in preference to a VKA for stroke prevention in patients with AF. Although eligible patients with NVAF in both South Korea and Taiwan are now able to receive rivaroxaban as first-line anticoagulation therapy for stroke prevention, there are limited real-world safety data in this treatment-naïve population.
The aim of the prospective, multicenter, observational, single-arm XaMINA (Xarelto on the prevention of stroke and non-central nervous system systemic embolism in treatment-naïve Asian patients with non-valvular atrial fibrillation) study was to investigate the safety profile of rivaroxaban for the prevention of stroke/non-central nervous system (CNS) SE in treatment-naïve patients with AF from Taiwan and South Korea in routine practice.
Methods
Study Design
XaMINA was a prospective, multicenter, observational, single-arm cohort study in patients with NVAF in South Korea and Taiwan who were naïve to anticoagulation treatment and who received rivaroxaban for the prevention of stroke or non-CNS SE. The study was registered at www.clinicaltrials.gov (NCT03284762) and was funded by Bayer AG.
Study Population
Patients were eligible for inclusion if they were aged ≥ 19 (South Korea) or ≥ 20 (Taiwan) years, had a diagnosis of NVAF, were naïve to anticoagulation treatment for the prevention of stroke/non-CNS SE, provided informed consent to participate, and were due to receive rivaroxaban for the prevention of stroke/non-CNS SE. The decision to initiate treatment with rivaroxaban was made as per the physician’s routine treatment practice. Patients were excluded if they had any contraindications to the use of rivaroxaban (according to the local label), or if they were participating in an investigational program with interventions outside of routine practice.
Eligible patients were screened consecutively and were documented in an anonymous log file independent of therapy. Patients were permitted to withdraw from the study at any point, with no requirement to provide a reason. Study centers in XaMINA were primary care practices, internal medicine specialist practices, or outpatient sites or clinics in South Korea and Taiwan. Data collection took place from September 2017 to September 2019 (Supplementary Material Fig. S1).
Medication and Follow-Up
Prescription decisions for rivaroxaban were solely at the discretion of the treating physician, without interference from the study sponsor. The dosage of rivaroxaban recommended in the label for the prevention of stroke/non-CNS SE differed between South Korea and Taiwan. In South Korea, the approved doses were rivaroxaban 20 mg once daily (od) for patients with creatinine clearance (CrCl) ≥ 50 ml/min and rivaroxaban 15 mg od for patients with CrCl 15–49 ml/min [9]. In Taiwan, the approved doses were rivaroxaban 15 mg or 20 mg od for patients with CrCl > 50 ml/min, and rivaroxaban 10 mg or 15 mg od for patients with CrCl 15–50 ml/min [10].
The planned follow-up period was 1 year, or until 30 days following the last dose of rivaroxaban if patients discontinued before 1 year. Patients were followed up according to routine medical practice and the frequencies of visits and procedures were performed under routine conditions. Investigators were asked to collect data at baseline and approximately every 3 months thereafter. Data were collected on patient demography, medical history, concomitant medication, current AF status, reasons for discontinuation (if applicable), and adverse events (AEs).
Study Outcomes
The primary outcome was major bleeding, defined using the International Society on Thrombosis and Haemostasis definition as fatal bleeding, a fall in hemoglobin of ≥ 2 g/dl, transfusion of ≥ 2 units of packed red blood cells or whole blood, or bleeding occurrence at a critical site (intracranial, intraspinal, intraocular, pericardial, intra-articular, intramuscular with compartment syndrome, or retroperitoneal). Major bleeding events were collected as treatment-emergent serious AEs (SAEs) or non-serious AEs. An event was considered a treatment-emergent AE (TEAE) if it started on or after the first dose of rivaroxaban, or up to 2 days following the last dose. Further details on the definitions used for AEs and SAEs can be found in the Supplementary Material Table S1.
Secondary outcomes were TEAEs and SAEs, all-cause mortality, non-major bleeding events, symptomatic thromboembolic events, and persistence with rivaroxaban treatment. Non-major bleeding events were collected as SAEs or non-serious AEs that did not fall into the category of major bleeding, while symptomatic thromboembolic events were collected as SAEs or non-serious AEs. Where feasible, study outcomes were also assessed in medically relevant subgroups.
All events were adjudicated by the central adjudication committee of five independent physicians. For an event to be considered as adjudicated, results from at least three physicians were required.
Management and Reporting of AEs
An AE was considered as any untoward medical occurrence that occurred following the administration of rivaroxaban, but which did not necessarily have a causal relationship with rivaroxaban treatment. An AE was considered to be serious (an SAE) if it resulted in death, was life-threatening, required inpatient hospitalization or prolonged existing hospitalization, resulted in persistent or significant disability or incapacity, was a congenital anomaly or birth defect, or was considered to be medically important. The outcomes of all reported AEs were followed up and documented during the course of the study, and up to 30 days after the last dose of rivaroxaban. Any reported SAE or pregnancy was forwarded immediately to the local pharmacovigilance contact responsible for SAE processing, and the outcome was followed up and documented. For any serious drug-related AE that occurred after the end of the study, standard procedures for spontaneous reporting were followed.
Statistical Analysis and Sample Size Calculation
XaMINA aimed to enroll a total of 1200 patients. This was based upon the assumption that the incidence proportion of major bleeding in treatment-naïve patients would be 1.9%, as observed in XANTUS AF [11]. In this case, a sample size of 1200 patients would allow for the estimation of the true incidence proportion of major bleeding by means of an exact 95% confidence interval (CI) with an entire width of 1.64 percentage points (Clopper–Pearson CI 1.22–2.86).
All analyses were exploratory and descriptive. Statistical analyses were performed on the safety population, which included all patients who had a diagnosis of NVAF, were treatment-naïve, took at least one dose of rivaroxaban, and had data collected for at least one post-baseline timepoint. Incidence proportions and incidence rates (events per 100 patient-years) with corresponding 95% CIs were calculated. Events were considered treatment emergent if they occurred on or after the day of the first dose of rivaroxaban, and up to 2 days following the final dose. Categorical variables were analyzed as absolute and relative frequencies, and continuous variables were analyzed with summary statistics, and described by absolute value and as change from baseline per analysis time point, if applicable. All therapies documented were coded using the World Health Organization Drug Dictionary. Medical history and AEs were coded using the latest version of the Medical Dictionary for Regulatory Activities.
Data Management and Administrative Organization
Where necessary, documented approval from an independent ethics committee or institutional review board at all participating centers was obtained prior to commencement of the study. Informed consent for the collection of their data for the purposes of the study was obtained in writing from all patients in advance, and strict confidentiality procedures were maintained with regard to patient data and identifiers. XaMINA was conducted within an approved indication in accordance with the guidelines and regulations of the European Medicines Agency (EMA), US Food and Drug Administration (FDA), and applicable local law(s) and regulations. The International Conference on Harmonisation Good Clinical Practice Guideline, and their Guideline on Good Pharmacovigilance Practice Modules VI and VIII, were also followed.
Results
Baseline Characteristics
A total of 1252 patients were screened at 38 study centers (28 in South Korea and 10 in Taiwan), and 1216 patients were enrolled in the study. Of the 36 patients who were screened but not enrolled, 32 (2.56%) did not meet the enrollment criteria for inclusion in XaMINA, and 4 (0.32%) decided not to take part in the study.
A total of 1094 (90.0%) patients were included in the safety analysis. The most common patient-level reason for non-inclusion in the safety analysis set was enrolled patients not being treatment naïve, which occurred for 35 (2.9%) patients. However, 80 (6.6%) patients were also not included as a result of the premature discontinuation of a study site (Fig. 1). All the recruited patients at this site were receiving rivaroxaban. There were 366 patients who discontinued the study prematurely. Full details on the reasons for the end of patient observation can be found in the Supplementary Material Table S2.
Patient disposition during the study. AF atrial fibrillation. aOne site withdrew early from the study without completing the close-out procedure. Patient data for this site were therefore not validated (83 patients screened; 80 patients enrolled). bOther dose includes initial rivaroxaban doses of 5 mg, 10 mg, or 30 mg
Similar proportions of patients received initial doses of rivaroxaban 15 mg od [488 (44.6%)] and rivaroxaban 20 mg od [489 (44.7%)]. Of those patients who received an initial dose of rivaroxaban other than 15 mg or 20 mg, the majority received 10 mg [113 (10.3%)].
There were 894 (81.7%) patients from 28 centers in South Korea in the safety analysis set and 200 (18.3%) from 10 centers in Taiwan (Table 1). The mean patient age was 70.1 ± 10.4 years, most patients were male [648 (59.2%)], and the mean body mass index was 25.2 ± 3.7. AF was paroxysmal in 418 (38.2%) patients, persistent in 240 (21.9%), long-standing persistent in 16 (1.5%), and permanent in 54 (4.9%). For the remaining 366 (33.5%) patients, it was their first diagnosis of AF. The mean CHADS2 [Congestive heart failure, Hypertension, Age ≥ 75 years, Diabetes mellitus, Stroke or transient ischemic attack (TIA; 2 points)] score was 1.6 ± 1.0, mean CHA2DS2-VASc [Congestive heart failure, Hypertension, Age ≥ 75 years (2 points), Diabetes mellitus, Stroke or TIA (2 points), Vascular disease, Age 65–74 years, Sex category (female)] score was 2.92 ± 1.42, and mean HAS-BLED (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio, Elderly, Drugs/alcohol concomitantly) score was 1.0 ± 0.8.
Notable comorbidities included hypertension (n = 798, 72.9%), diabetes mellitus (n = 293, 26.8%), congestive heart failure (n = 176, 16.1%), and prior stroke/CNS SE or TIA (n = 47, 4.3%).
CrCl ≥ 50 ml/min occurred in 693 (63.3%) patients and was < 50 ml/min in 152 (13.9%) patients. For the remaining 249 (22.8%) patients, CrCl data were missing. Of the 693 patients who had first available CrCl ≥ 50 ml/min, 277 (40.0%) received an initial dose of rivaroxaban 15 mg od, while 365 (52.7%) received rivaroxaban 20 mg od. Conversely, 84 (55.3%) of the 152 patients with an initial CrCl value < 50 ml/min received rivaroxaban 15 mg od, and 22 (14.5%) received rivaroxaban 20 mg od. It should be noted that the label-recommended dose of rivaroxaban based upon CrCl differed between South Korea and Taiwan. In South Korea, it was rivaroxaban 20 mg od for CrCl ≥ 50 ml/min and rivaroxaban 15 mg od for CrCl 15–49 ml/min [9]. In Taiwan, it was rivaroxaban 15 or 20 mg od for CrCl > 50 ml/min and rivaroxaban 10 mg or 15 mg od for CrCl 15–50 ml/min [10].
Primary Outcome
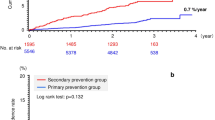
During the study, 22 major bleeding events occurred in 20 patients (1.8%), with an incidence rate of 2.10 events per 100 patient-years (95% CI 1.35–3.25), and events increased gradually over time (Fig. 2; Table 2). Most major bleeding events were associated with a fall in hemoglobin of ≥ 2 g/dl and the transfusion of ≥ 2 units of packed red blood cells, with each of these events occurring in 10 (0.9%) patients [1.05 per 100 patient-years (95% CI 0.56–1.95)]. A fatal bleeding event occurred in only 1 (0.1%) patient (0.10 per 100 patient-years; 95% CI 0.01–0.74), and critical site bleeding events occurred in 4 (0.4%) patients (0.42 per 100 patient-years; 95% CI 0.16–1.11).
The most common site of major bleeding was gastrointestinal [n = 10 (0.9%)], followed by CNS [n = 6 (0.5%)], pulmonary [n = 1 (0.1%)], and genitourinary [n = 1 (0.1%)]. There were also cases where the site of bleeding was missing [n = 1 (0.1%)] or unknown [n = 2 (0.2%)]. The major bleeding event occurred as the result of a procedure or surgery in 1 (0.1%) case.
Primary Outcome in Patient Subgroups
Major bleeding events in select patient subgroups are summarized in the Supplementary Material Table S3. Of note, the incidence rate of major bleeding events was higher in patients who received rivaroxaban 10 mg od (n = 8, 8.6 per 100 patient-years; 95% CI 4.3–17.3) than those who received rivaroxaban 15 mg od (n = 5, 1.2 per 100 patient-years; 95% CI 0.5–2.9) or rivaroxaban 20 mg od (n = 6, 1.4 per 100 patient-years; 95% CI 0.6–3.0). There was also a slightly higher incidence of events in female patients (n = 10, 2.6 per 100 patient-years; 95% CI 1.4–4.8) compared with male patients (n = 10, 1.8 per 100 patient-years; 95% CI 1.0–3.3). Incidence rates of major bleeding events increased with higher CHADS2, CHA2DS2-VASc, and HAS-BLED scores.
Secondary Outcomes
Non-major bleeding events occurred in 102 patients [9.3%, 11.4 per 100 patient-years (95% CI 9.37–13.81); Table 2]. There were 9 [0.8%, 0.94 per 100 patient-years (95% CI 0.49–1.81)] patients who had a symptomatic thromboembolic event. Of these, 5 (0.5%) had a stroke, 3 (0.3%) experienced myocardial infarction, and 1 (0.1%) had a TIA. There were no cases of non-CNS SE.
There were eight treatment-emergent deaths [0.73%, 0.84 per 100 patient-years (95% CI 0.42–1.67); Table 2]. Four of these were due to infectious disease, two were unexplained, one was due to myocardial infarction, and one was the result of ischemic stroke. In addition, there were five deaths that were not considered to be treatment emergent. Following adjudication, it was determined that one death was caused by intracranial bleeding, one was due to cancer, and one was the result of infectious disease. There was also one death that was initially unexplained but later confirmed as respiratory failure, and one for which the cause was classified as ‘other’. Symptomatic thromboembolic events and treatment-emergent deaths both accumulated throughout the study, with no appreciable peaks in incidence at any timepoint (Fig. 2).
TEAEs occurred in 502 (45.9%) patients, with 85 (7.8%) of these considered to be related to rivaroxaban treatment. Further details on the TEAEs that occurred in XaMINA can be found in the Supplementary Material Table S4. SAEs occurred in 150 (13.7%) patients, and 18 (1.7%) of these were determined to be related to rivaroxaban treatment.
The mean duration of rivaroxaban treatment in XaMINA was 301.4 ± 123.6 days. A total of 735 (67.2%) patients in the safety analysis population persisted with rivaroxaban for the full 12-month observation period, with 359 (32.8%) patients discontinuing during the same period.
There were 84 patients (7.7%) who changed their dose of rivaroxaban during the study; 74 (6.8%) of these changed their dose once, while 10 (0.9%) changed their dose either two or three times. There were 24 (2.2%) patients who increased their dose once, but there were no further dose increases in any of these patients. Conversely, 66 (6.0%) patients decreased their dose once, and an additional 2 (0.2%) decreased their dose either two or three times. Treatment interruption occurred 120 times throughout the observation period, with 108 (9.9%) patients interrupting therapy at least once. The main reasons for a change in rivaroxaban dose or a treatment interruption were AEs (n = 44, 4.0%) and ‘other’ (n = 44, 4.0%). Other reasons were invasive procedures/surgeries (n = 18, 1.6%), subject choice (n = 17, 1.6%), supply issues due to health system (n = 5, 0.5%), insufficient therapeutic effect (n = 2, 0.2%), and dentistry (n = 4, 0.4%).
Secondary Outcomes in Patient Subgroups
Secondary outcomes that occurred in selected patient subgroups are detailed in the Supplementary Material Table S5. Incidence rates of non-major bleeding were similar in patients receiving different doses of rivaroxaban and higher in patients with normal CrCl than in those with renal impairment, but this should be interpreted with caution because of the small number of patients with non-major bleeding and renal impairment. There were too few symptomatic thromboembolic events to determine if the incidence rates increased according to CHADS2 and CHA2DS2-VASc scores.
TEAEs occurred more frequently in patients receiving rivaroxaban 10 mg od than either rivaroxaban 15 mg od or rivaroxaban 20 mg od. However, similar proportions of AEs were considered to be drug related across all rivaroxaban doses. A similar trend was seen for SAEs, although these were more often considered drug related in patients who received the rivaroxaban 10 mg od dose.
Discussion
XaMINA is the first prospective real-world study of treatment-naïve patients with NVAF from South Korea and Taiwan receiving rivaroxaban for the prevention of stroke/SE. The results of XaMINA indicate that rivaroxaban had a reassuringly low incidence of bleeding events in this population.
The findings of this study complement the results of the previously published XANTUS [11], XANAP [31], and XAPASS [34] real-world studies, which explored the safety of rivaroxaban in global, East Asian, and Japanese populations, respectively. Only a proportion of patients in these previous studies were treatment naïve. The findings from XaMINA also complement clinical trial results from the ROCKET AF [5, 30, 42] and J-ROCKET AF [29] studies, which investigated the efficacy and safety of rivaroxaban for the prevention of stroke/SE in patients with AF in global and Japanese populations, respectively.
Baseline characteristics in XaMINA were generally consistent with those from the East Asian and Japanese populations studied in XANAP and XAPASS, respectively [31, 34], and also with the non-Asian population studied in XANTUS (Table 3) [11]. An expected, but notable, exception to this is the proportion of patients in each study who had a prior stroke, non-CNS SE, or TIA, which was much lower in XaMINA (4.3%) than in XANAP (32.8%) [31], XAPASS (23.4%) [34], or XANTUS (19.0%) [11]. This difference is also reflected in the baseline CHADS2 and CHA2DS2-VASc scores seen in each study (Table 3) [11, 31, 34]. These differences are likely related to the fact that patients in XaMINA were treatment naïve, because those patients who have already had a prior thromboembolic event would be more likely to be receiving anticoagulant treatment. In addition, there was a relatively high proportion of patients in XaMINA for whom it was their first diagnosis of AF (33.5% compared with 22.2% in XANAP, none reported in XAPASS, and 18.5% in XANTUS). This means there may have been less time for an event to occur in XaMINA than in the other studies.
XaMINA showed a similar incidence of major bleeding to previous studies, with incidence rates of 2.1 per 100 patient-years in XANTUS [11], 1.5 per 100 patient-years in XANAP [31], and 1.8 per 100 patient-years in XAPASS [34]. However, there were very few fatal bleeding events in all the studies, with incidence rates of 0.1 per 100 patient-years in XaMINA, and 0.2 per 100 patient-years in XANAP, XANTUS, and XAPASS [11, 31, 34]. Major bleeding events in critical organs occurred less frequently in XaMINA (0.4 per 100 patient-years) than in XANAP and XAPASS (0.8 per 100 patient-years in each case) [31, 34] or XANTUS (0.7 per 100 patient-years) [11], while those associated with a fall in hemoglobin of ≥ 2/dl or a requirement for transfusion of ≥ 2 g/dl of packed red blood or whole blood were slightly higher in XaMINA when compared with XANAP [31] and XAPASS [34] (although similar to XANTUS [11]) (Table 3). The reasons for these differences in bleeding rates are unknown, and it is challenging to ascertain whether such small differences in incidence rates are significant or have an underlying cause. These findings are consistent with analyses of the Korean and Taiwanese National Health Insurance databases, which also showed that rivaroxaban is associated with low incidence rates of major bleeding in these populations [16, 17, 20].
It is also of note that incidence rates of major bleeding in XaMINA, XANAP, XANTUS, and XAPASS were lower than those seen in the ROCKET AF trial (3.6 per 100 patient-years) [5], the East Asian subanalysis of ROCKET AF (3.4 per 100 patient-years) [30], and the J-ROCKET AF clinical trial (3.0 per 100 patient-years) [29]. This likely reflects the fact that patients included in ROCKET AF had higher baseline HAS-BLED scores than in the real-world studies (Table 3).
Although major bleeding occurred in too few patients for a formal comparison, it is notable that the incidence rate of major bleeding events in XaMINA was higher in patients who received rivaroxaban 10 mg od (8.6 per 100 patient-years) than in those who received rivaroxaban 15 mg od (1.2 per 100 patient-years) or 20 mg od (1.4 per 100 patient-years). A similar trend towards higher incidence rates of bleeding associated with lower doses of DOAC was also seen in XANAP, XAPASS, and XANTUS [11, 31, 34], and in analyses of data from the Dresden NOAC Registry for rivaroxaban, dabigatran, and apixaban [43,44,45]. This finding from XaMINA lends further support to a previously proposed explanation that physicians might tend to prescribe lower doses of DOACs to patients with a higher risk of bleeding, resulting in an association between these lower doses and higher incidence rates of bleeding events [43,44,45]. Unfortunately, patients receiving lower than recommended doses of DOACs may have inadequate protection against stroke, while remaining at risk of bleeding as a result of their clinical characteristics [46,47,48]. This scenario may have been the case in XaMINA.
The incidence rates of bleeding events, treatment-emergent symptomatic thromboembolic events, and AEs in XaMINA were either lower or comparable with those seen in the XANAP, XAPASS, and XANTUS studies [11, 31, 34]. While the incidence rates of major bleeding events were broadly consistent between XaMINA, XAPASS, and XANTUS, they were somewhat lower in XANAP (Table 3) [11, 31, 34]. Incidence rates of non-major bleeding events in XaMINA were consistent with those reported in the other studies [5, 11, 29,30,31, 34].
The incidence rate of thromboembolism in XaMINA was lower than that seen in XANAP, XAPASS, and XANTUS, as were rates of stroke and SE (Table 3) [11, 31, 34]. Again, this may reflect the lower baseline CHADS2 and CHA2DS2-VASc scores seen in XaMINA compared with the other studies, and the fact that, as previously mentioned, more patients in XaMINA were treatment naïve, had not had a prior stroke, and were presenting with their first diagnosis of AF. However, this lower rate of thromboembolism is still of interest given the higher stroke risk previously reported in Asian versus non-Asian patients. Similarly, at 0.8 per 100 patient-years, the mortality rate in XaMINA was lower than that seen in other real-world studies (rates were 2.0, 1.9, and 2.5 per 100 patient-years in XANAP, XANTUS, and XAPASS, respectively [11, 31, 34]). Notably, the majority of these deaths in XaMINA were the result of infectious diseases or unknown causes, with only two due to thromboembolic events.
AEs occurred in 46% of patients in XaMINA, and SAEs occurred in 14%, which is comparable with both XANAP and XANTUS (Table 3) [11, 31]. Only a small proportion of these events were related to rivaroxaban treatment. One-year treatment persistence in XaMINA was similar to that in XANAP and XAPASS [31, 34], but slightly lower than in XANTUS [11]. The most frequent reason for a change or interruption in treatment was due to AEs, accounting for 4% of treatment interruptions. A similar trend was also seen with the mean treatment durations, which were comparable across the Asian XaMINA, XANAP, and XAPASS studies [31, 34], but longer in the global XANTUS study (Table 3) [11]. This may indicate that measures to encourage further follow-up might be warranted in Asian countries.
Although no other prospective studies assessing the efficacy and safety of DOACs in anticoagulation-naïve Asian patients have been published to date, several retrospective studies have been published based on the Korean National Health Insurance database [15, 20, 49, 50]. The results from XaMINA broadly align with findings from these studies. The incidence rate per 100 patient-years for major bleeding events varied between 2.07 and 2.79 for patients receiving rivaroxaban, 1.67 and 2.05 for patients receiving dabigatran, 1.62 and 1.85 for patients receiving apixaban, and 1.65 and 2.45 for patients receiving edoxaban [20, 49, 50].
Data on CrCl were missing for 22.8% of patients in XaMINA, meaning that it was not always possible to determine whether patients received rivaroxaban doses based upon their renal function, as per the local label. Even in patients with known CrCl, further analyses would be required to determine if patients received local label-recommended doses according to renal function, because the label-recommended doses of rivaroxaban differed between South Korea [9] and Taiwan [10]. A large proportion of patients also had missing CrCl data in XANAP (48.5%) and XANTUS (34.4%) [11, 31]. In XANTUS, as in XaMINA, event rates in patients with missing CrCl data were very low [11, 27, 31]. Therefore, it was suggested that physicians might not have considered renal function testing necessary in these patients, or that renal function was assessed without being documented [11, 31]. This may have also been the case in XaMINA.
Limitations and Strengths
Limitations
XaMINA had a single-arm, open-label study design, which may have introduced bias as a result of patient and physician knowledge of treatment. This single-arm design was used because comparison with a VKA would not have reflected clinical practice, and comparison to another DOAC would have introduced alternative bias. Additionally, due to the non-interventional nature of the study, interference with patient management was not allowed, which may have resulted in missing data. For example, the fact that a large number of patients did not have a CrCl value recorded limits the interpretation of findings based upon subgroup analysis of renal function. Patient follow-up was based upon routine care, meaning that follow-up time may have differed among physicians. The planned sample size was 1200 patients and, although 1216 patients were enrolled, the number of patients valid for determination of safety outcomes was 1094; although fewer than anticipated, this number remained adequate to achieve the aim of the study.
Strengths
As a prospective, non-interventional study, the results of XaMINA reflect the use of rivaroxaban in treatment-naïve patients in a real-world, clinical setting. Steps were also taken to limit the potential for bias as much as possible. To reduce selection bias, physicians were asked to document consecutive patients who received rivaroxaban, and eligible patients were enrolled consecutively. Data verification was also performed in at least 5% of study centers to reduce reporting bias.
Conclusions
Results from the real-world XaMINA study of patients with NVAF from Taiwan and South Korea who were naïve to anticoagulation, and initiated on rivaroxaban for the prevention of stroke/SE, showed that rivaroxaban was associated with low incidence rates of the primary outcome of major bleeding events. Similar results were seen for secondary outcomes, including thromboembolic events and mortality, and treatment persistence was similar to that seen in previous studies. These findings were consistent with the similar real-world XANAP, XAPASS, and XANTUS studies, which studied similar outcomes across a variety of global populations.
References
Andrew NE, Thrift AG, Cadilhac DA. The prevalence, impact and economic implications of atrial fibrillation in stroke: what progress has been made? Neuroepidemiology. 2013;40:227–39. https://doi.org/10.1159/000343667.
Pistoia F, Sacco S, Tiseo C, et al. The epidemiology of atrial fibrillation and stroke. Cardiol Clin. 2016;34:255–68. https://doi.org/10.1016/j.ccl.2015.12.002.
Chiang CE, Wang KL, Lin SJ. Asian strategy for stroke prevention in atrial fibrillation. Europace. 2015;17 Suppl 2:ii31–9. https://doi.org/10.1093/europace/euv231.
Zirlik A, Bode C. Vitamin K antagonists: relative strengths and weaknesses vs. direct oral anticoagulants for stroke prevention in patients with atrial fibrillation. J Thromb Thrombolysis. 2017;43:365–79. https://doi.org/10.1007/s11239-016-1446-0.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91. https://doi.org/10.1056/NEJMoa1009638.
Granger CB, Alexander JH, McMurray JJV, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92. https://doi.org/10.1056/NEJMoa1107039.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51. https://doi.org/10.1056/NEJMoa0905561.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104. https://doi.org/10.1056/NEJMoa1310907.
Bayer HealthCare Manufacturing Srl. Xarelto® (rivaroxaban) SOUTH KOREA - Summary of Product Characteristics. 2020. https://nedrug.mfds.go.kr/pbp/CCBBB01/getItemDetail?itemSeq=200902650. Accessed 18 May 2021.
Bayer AG. Xarelto® (rivaroxaban) TAIWAN - Summary of Product Characteristics. 2019. https://info.fda.gov.tw/MLMS/H0001D3.aspx?LicId=02025648. Accessed 18 May 2021.
Camm AJ, Amarenco P, Haas S, et al. XANTUS: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation. Eur Heart J. 2016;37:1145–53. https://doi.org/10.1093/eurheartj/ehv466.
Lauffenburger JC, Farley JF, Gehi AK, et al. Effectiveness and safety of dabigatran and warfarin in real-world US patients with non-valvular atrial fibrillation: a retrospective cohort study. J Am Heart Assoc. 2015;4:e001798.
Proietti M, Romanazzi I, Romiti GF, et al. Real-world use of apixaban for stroke prevention in atrial fibrillation: a systematic review and meta-analysis. Stroke. 2018;49:98–106. https://doi.org/10.1161/STROKEAHA.117.018395.
Lee HF, See LC, Li PR, et al. Non-vitamin K antagonist oral anticoagulants and warfarin in atrial fibrillation patients with concomitant peripheral artery disease. Eur Heart J Cardiovasc Pharmacotherap. 2021;7:50–8. https://doi.org/10.1093/ehjcvp/pvz072.
Cha MJ, Choi EK, Han KD, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2017;48:3040–8. https://doi.org/10.1161/STROKEAHA.117.018773.
Chan YH, Lee HF, See LC, et al. Effectiveness and safety of four direct oral anticoagulants in Asian patients with nonvalvular atrial fibrillation. Chest. 2019;156:529–43. https://doi.org/10.1016/j.chest.2019.04.108.
Chan YH, See LC, Tu HT, et al. Efficacy and safety of apixaban, dabigatran, rivaroxaban, and warfarin in Asians with nonvalvular atrial fibrillation. J Am Heart Assoc. 2018;7: e008150. https://doi.org/10.1161/JAHA.117.008150.
Lee SR, Choi EK, Han KD, et al. Edoxaban in Asian patients with atrial fibrillation: effectiveness and safety. J Am Coll Cardiol. 2018;72:838–53. https://doi.org/10.1016/j.jacc.2018.05.066.
Lee SR, Choi EK, Han KD, et al. Optimal rivaroxaban dose in Asian patients with atrial fibrillation and normal or mildly impaired renal function. Stroke. 2019;50:1140–8. https://doi.org/10.1161/STROKEAHA.118.024210.
Lee SR, Choi EK, Kwon S, et al. Effectiveness and safety of contemporary oral anticoagulants among Asians with nonvalvular atrial fibrillation. Stroke. 2019;50:2245–9. https://doi.org/10.1161/STROKEAHA.119.025536.
Lee SR, Choi EK, Kwon S, et al. Oral anticoagulation in Asian patients with atrial fibrillation and a history of intracranial hemorrhage. Stroke. 2020;51:416–23. https://doi.org/10.1161/STROKEAHA.119.028030.
Lin YC, Chien SC, Hsieh YC, et al. Effectiveness and safety of standard- and low-dose rivaroxaban in Asians with atrial fibrillation. J Am Coll Cardiol. 2018;72:477–85. https://doi.org/10.1016/j.jacc.2018.04.084.
Park J, Lee SR, Choi EK, et al. Effectiveness and safety of direct oral anticoagulant for secondary prevention in Asians with atrial fibrillation. J Clin Med. 2019;8:2228. https://doi.org/10.3390/jcm8122228.
Tsai CT, Liao JN, Chiang CE, et al. Association of ischemic stroke, major bleeding, and other adverse events with warfarin use vs non-vitamin K antagonist oral anticoagulant use in patients with atrial fibrillation with a history of intracranial hemorrhage. JAMA Netw Open. 2020;3: e206424. https://doi.org/10.1001/jamanetworkopen.2020.6424.
Lee HF, Chan YH, Tu HT, et al. The effectiveness and safety of low-dose rivaroxaban in Asians with non-valvular atrial fibrillation. Int J Cardiol. 2018;261:78–83. https://doi.org/10.1016/j.ijcard.2018.03.063.
Chan YH, Kuo CT, Yeh YH, et al. Thromboembolic, bleeding, and mortality risks of rivaroxaban and dabigatran in Asians with nonvalvular atrial fibrillation. J Am Coll Cardiol. 2016;68:1389–401. https://doi.org/10.1016/j.jacc.2016.06.062.
Kirchhof P, Radaideh G, Kim YH, et al. Global prospective safety analysis of rivaroxaban. J Am Coll Cardiol. 2018;72:141–53. https://doi.org/10.1016/j.jacc.2018.04.058.
Sabir I, Khavandi K, Brownrigg J, et al. Oral anticoagulants for Asian patients with atrial fibrillation. Nat Rev Cardiol. 2014;11:290–303.
Hori M, Matsumoto M, Tanahashi N, et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study. Circ J. 2012;76:2104–11.
Wong KS, Hu DY, Oomman A, et al. Rivaroxaban for stroke prevention in East Asian patients from the ROCKET AF trial. Stroke. 2014;45:1739–47.
Kim YH, Shim J, Tsai CT, et al. XANAP: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation in Asia. J Arrhythm. 2018;34:418–27. https://doi.org/10.1002/joa3.12073.
Camm AJ, Amarenco P, Haas S, et al. XANTUS: rationale and design of a noninterventional study of rivaroxaban for the prevention of stroke in patients with atrial fibrillation. Vasc Health Risk Manag. 2014;10:425–34. https://doi.org/10.2147/VHRM.S63298.
Martinez CAA, Lanas F, Radaideh G, et al. XANTUS-EL: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation in Eastern Europe, Middle East, Africa and Latin America. Egypt Heart J. 2018;70:307–13. https://doi.org/10.1016/j.ehj.2018.09.002.
Ikeda T, Ogawa S, Kitazono T, et al. Real-world outcomes of the Xarelto post-authorization safety & effectiveness study in Japanese patients with atrial fibrillation (XAPASS). J Cardiol. 2019;74:60–6. https://doi.org/10.1016/j.jjcc.2019.01.001.
Hori M, Connolly SJ, Ezekowitz MD, et al. Efficacy and safety of dabigatran vs. warfarin in patients with atrial fibrillation – sub-analysis in Japanese population in RE-LY trial. Circ J. 2011;75:800–5.
Goto S, Zhu J, Liu L, et al. Efficacy and safety of apixaban compared with warfarin for stroke prevention in patients with atrial fibrillation from East Asia: a subanalysis of the Apixaban for Reduction in Stroke and Other Thromboembolic Events in atrial fibrillation (ARISTOTLE) trial. Am Heart J. 2014;168:303–9.
Yamashita T, Koretsune Y, Yang Y, et al. Edoxaban versus warfarin in East Asian patients with atrial fibrillation - an ENGAGE AF-TIMI 48 subanalysis. Circ J. 2016;80:860–9. https://doi.org/10.1253/circj.CJ-15-1082.
Lee SR, Choi EK, Han KD, et al. Non-vitamin K antagonist oral anticoagulants in Asian patients with supranormal renal function. Stroke. 2019;50:1480–9. https://doi.org/10.1161/STROKEAHA.118.024264.
Joung B, Lee JM, Lee KH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018;48:1033–80. https://doi.org/10.4070/kcj.2018.0339.
Chiang CE, Wu TJ, Ueng KC, et al. 2016 Guidelines of the Taiwan Heart Rhythm Society and the Taiwan Society of Cardiology for the management of atrial fibrillation. J Formos Med Assoc. 2016;115:893–952. https://doi.org/10.1016/j.jfma.2016.10.005.
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962.
ROCKET AF Study Investigators. Rivaroxaban - once-daily, oral, direct Factor Xa inhibition - compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am Heart J. 2010;159:340–7.
Hecker J, Marten S, Keller L, et al. Effectiveness and safety of rivaroxaban therapy in daily-care patients with atrial fibrillation. Results from the Dresden NOAC Registry. Thromb Haemost. 2016;115:939–49.
Helmert S, Marten S, Mizera H, et al. Effectiveness and safety of apixaban therapy in daily-care patients with atrial fibrillation: results from the Dresden NOAC Registry. J Thromb Thrombolysis. 2017;44:169–78. https://doi.org/10.1007/s11239-017-1519-8.
Beyer-Westendorf J, Ebertz F, Förster K, et al. Effectiveness and safety of dabigatran therapy in daily-care patients with atrial fibrillation. Results from the Dresden NOAC Registry. Thromb Haemost. 2015;113:1247–57.
Yu HT, Yang PS, Jang E, et al. Label adherence of direct oral anticoagulants dosing and clinical outcomes in patients with atrial fibrillation. J Am Heart Assoc. 2020;9: e014177. https://doi.org/10.1161/JAHA.119.014177.
Lee KN, Choi JI, Boo KY, et al. Effectiveness and safety of off-label dosing of non-vitamin K antagonist anticoagulant for atrial fibrillation in Asian patients. Sci Rep. 2020;10:1801. https://doi.org/10.1038/s41598-020-58665-5.
Steinberg BA, Shrader P, Thomas L, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II registry. J Am Coll Cardiol. 2016;68:2597–604. https://doi.org/10.1016/j.jacc.2016.09.966.
Cho MS, Yun JE, Park JJ, et al. Outcomes After Use of Standard- and Low-Dose Non-Vitamin K Oral Anticoagulants in Asian Patients With Atrial Fibrillation. Stroke. 2018: doi:https://doi.org/10.1161/strokeaha.118.023093:Strokeaha118023093. https://doi.org/10.1161/strokeaha.118.023093.
Lee SR, Choi EK, Han KD, et al. Comparison of Once-Daily Administration of Edoxaban and Rivaroxaban in Asian Patients with Atrial Fibrillation. Sci Rep. 2019;9:6690. https://doi.org/10.1038/s41598-019-43224-4.
Acknowledgements
We would like to express our thanks to all participants of the study.
Funding
This study was funded by Bayer AG. The Rapid Service Fee was funded by Bayer AG.
Medical Writing and Editorial Assistance
The authors would like to acknowledge Tom Rowles from Chameleon Medical Communications, who provided medical writing services with funding from Bayer AG.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors have contributed to design, analysis, interpretation of data, drafting and reviewing the manuscript and have read and approved the final draft for submission.
Disclosures
All authors were investigators for XaMINA and were paid for their participation. Eue-Keun Choi has also received research grants from Bayer, Bristol Myers Squibb/Pfizer, Biosense Webster, Chong Kun Dang, Daiichi-Sankyo, Dreamtech Co., Ltd, Medtronic, Samjinpharm, Sanofi-Aventis, Seers Technology, Skylabs, and Yuhan. Lili Wang is an employee of Bayer. Ping-Yen Liu, Tae-Soek Kim, Jen-Yuan Kuo, Jung Myung Lee, Young Keun On, Hyung-Wook Park, Sang-Weon Park, Dong-Gu Shin, Hsueh-Wei Yen, and Moon-Hyoung Lee have no further conflicts of interest to disclose.
Compliance with Ethics Guidelines
The study was carried out within an approved indication in accordance with guidelines and regulations of EMA, FDA, and applicable local laws and regulations. In all countries where reference to an independent ethics committee or institutional review board is required, documented approvals from appropriate groups were obtained. Informed consent was obtained from every patient in writing before the documentation of any data.
Data Availability
Study results will be disclosed in a publicly available database within the standard timelines.
Author information
Authors and Affiliations
Consortia
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, PY., Choi, EK., Kim, TS. et al. XaMINA: A Real-World, Prospective, Observational Study of Treatment-Naïve Patients Treated with Rivaroxaban for Stroke Prevention in Atrial Fibrillation in Asia. Adv Ther 39, 3316–3333 (2022). https://doi.org/10.1007/s12325-022-02102-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02102-8