Abstract
Relative frequency of hereditary ataxias remains unknown in many regions of Latin America. We described the relative frequency in spinocerebellar ataxias (SCA) due to (CAG)n and to (ATTCT)n expansions, as well as Friedreich ataxia (FRDA), among cases series of ataxic individuals from Peru. Among ataxic index cases from 104 families (38 of them with and 66 without autosomal dominant pattern of inheritance), we identified 22 SCA10, 8 SCA2, 3 SCA6, 2 SCA3, 2 SCA7, 1 SCA1, and 9 FRDA cases (or families). SCA10 was by far the most frequent one. Findings in SCA10 and FRDA families were of note. Affected genitors were not detected in 7 out of 22 SCA10 nuclear families; then overall maximal penetrance of SCA10 was estimated as 85%; in multiplex families, penetrance was 94%. Two out of nine FRDA cases carried only one allele with a GAA expansion. SCA10 was the most frequent hereditary ataxia in Peru. Our data suggested that ATTCT expansions at ATXN10 might not be fully penetrant and/or instability between generations might frequently cross the limits between non-penetrant and penetrant lengths. A unique distribution of inherited ataxias in Peru requires specific screening panels, considering SCA10 as first line of local diagnosis guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hereditary ataxias (HA) are clinically and genetically heterogeneous diseases characterized by gait and limb ataxia, dysarthria, oculomotor impairment and other highly variable signs. Age of onset varies from early childhood to late adulthood [1, 2]. All are rare disorders with frequencies varying according to their geographical origin [3].
Among autosomal dominant ataxias (AD), spinocerebellar ataxias (SCAs) are the most common inherited disorders. At least 42 genetic loci have been linked to a given SCA [2]. The most frequent SCAs are caused by unstable CAG repeat expansions coding for polyglutamine (polyQ) tracts. This is the case of SCA1, SCA2, SCA3(also known as Machado-Joseph disease, SCA3/MJD), SCA6, SCA7, SCA17, and dentatorubro-pallidoluysian atrophy (DRPLA) [4]. SCA10, a relatively common HA among Latin Americans, is caused by an expansion of hundreds of ATTCT repeats in intron 9 of the ATXN10 gene [5]. The remaining SCAs are caused by either point mutations or intronic expansions.
Most autosomal recessive ataxias (AR) are clinically heterogeneous with overlapping features, complicating their diagnostic; except for Friedreich Ataxia (FRDA), the most known of these disorders. FRDA is caused by biallelic pathogenic variants in the FXN gene. The most common mutation is the expansion of an intronic GAA repeat, found in homozygosis in 90–94% of cases, and in compound heterozygosis-usually combined with a point mutation- in the remaining individuals [6, 7]. Sex-linked forms of ataxia are rare, and the tremor-ataxia syndrome (FXTAS) described in male carriers of premutated alleles at the fragile-X locus [8] might be suspected through an X linked pattern relating ataxic individuals to mentally disable male relatives.
The relative frequency of several HA has been reported in many populations [9]. In Latin America, the distribution of HA differs across regions. There is a large and well-described SCA3/MJD population in Brazil with higher frequencies reported in Southern states mainly associated to Azorean founder effect [10]. SCA2 has been reported as the most frequent ataxia in Cuba, where a founder effect was described at the Holguin Province [11]. SCA2 has been also reported as the most frequent SCA in Mexican families [12]. SCA10 has been described as the second most common inherited ataxia in Mexico and some states of Brazil, after SCA2 and SCA3/MJD, respectively [12, 13]. A nationwide study in Venezuela found SCA7 as the most frequent SCA closely followed by SCA3/MJD [14].
These studies prompted a guideline for their diagnosis [15]. However, the adequacy of this guideline in Latin American countries will depend on the population-specific frequencies of HA, which remain largely unknown.
In order to contribute to the growth of knowledge in this field, we aimed to describe the relative frequency of SCA1, SCA2, SCA3/MJD, SCA6, SCA7, SCA10, SCA12, SCA17, DRPLA, and FRDA cases among a case series of ataxic individuals followed at the Instituto Nacional de Ciencias Neurologicas (INCN), the only specialized center providing molecular diagnosis for inherited ataxias in Peru.
Methods
Patients
From August 2012 to August 2016, ataxic individuals followed up at the INCN, Lima, Peru, were invited to participate in this study. Exclusion criteria for secondary ataxias and phenocopies were (a) the presence of any abnormality that explain occurrence of ataxia or related neurological symptoms on the following exams at recruitment: basic blood biochemistry; thorax X-ray; abdominal ultrasound; mammary ultrasound and mammography, in women; thyroid-stimulating hormone, lymphocyte and thrombocyte count, hemoglobin, erythrocyte median corpuscular volume, sedimentation rate, vitamin B12, Vitamin E, VDRL (venereal disease research laboratory), antibodies (anti-HIV, Human Immunodeficiency Virus), qualitative urine test, anti-Yo and anti-Hu antibodies; (b) suggestive MRI for a vascular, autoimmune, or infectious process in central nervous system; (c) the presence of the Met30 mutation at the transthyretin gene to rule out transthyretin polyneuropathy; or (d) the presence of a CAG repeat expansion at HTT gene, in patients with associated cognitive impairment.
Informed consent was obtained from each participant. This study was approved by the Institutional Ethics Committees (EC) from the INCN, Lima, Peru, and Hospital de Clínicas de Porto Alegre, Brazil, registered at Plataforma Brasil as 20620613.2.3001.5479.
After consent, a structured interview was performed. Clinical and demographic data such as place of birth, gender, age, age at onset, age at sample collection, disease duration, and family history were obtained and were double-checked in clinical records from the ataxia registry at the INCN. Age at onset was defined when the patient or a close relative noticed the first symptom of the disease (usually but not always gait unbalance). When possible, extended pedigrees were drawn using free online pedigree tool (https://www.progenygenetics.com/). Presence or absence of several neurological findings, as well as clinical and family history, was collected through an online digital form, as described elsewhere [10]. Data were included into an electronic database, in a standardized format.
Blood sample was collected, and then DNA was isolated from leukocytes at the Neurogenetics Lab in Lima using standard procedures [16]. A DNA aliquot was shipped to the laboratories at Hospital de Clínicas de Porto Alegre, where the molecular analyses were performed.
Procedures
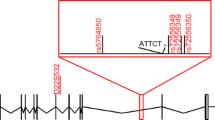
Fluorescence-based assay (Quant-iT – Invitrogen) was used for DNA quantitation. Evaluation of the (CAG)n tract was performed by PCR amplification with gene-specific fluorescently labeled primers. After amplification, an aliquot of PCR products was mixed with formamide (HiDi™ formamide, Applied Biosystems) and GeneScan™ 500 LIZ (Applied Biosystems), and capillary electrophoresis was performed in an ABI3130xl Genetic Analyzer (Applied Biosystems). Amplicon lengths at ATXN1, ATXN2, ATXN3, CACNA1A, ATXN7, PPP2R2B, TBP, and ATN1 genes were estimated using GeneMapper 3.2 software (Applied Biosystems). Expanded allele in the ATXN10 gene was detected by the repeat primed-PCR (RP-PCR) methodology as previously described [17]. Length of the expanded repeats at ATXN10 was not determined. Amplicons following PCR reaction were also mixed with formamide (HiDi™ Formamide, Applied Biosystems) and GeneScan™ 500 LIZ (Applied Biosystems), and capillary electrophoresis was performed in the ABI 3130xl Genetic Analyzer (Applied Biosystems). Amplification pattern of normal alleles was compared to that of expanded alleles after analysis with the GeneMapper® software v 3.2 (Applied Biosystems). Positive and negative controls were also included in each analysis to control run variability. GAA repeats within the FRDA1 gene were genotyped by PCR; qualitative expanded allele determination (threshold over 200 GAA repeats) was confirmed by RP-PCR.
Figure 1 summarizes the recruitment criteria and the diagnostic workout for two groups of ataxic subjects included in the study, as follows:
Patients and families with a recurrence pattern characteristic of an autosomal dominant inheritance were called AD cases. They were studied for expansions at ATXN1(SCA1), ATXN2(SCA2), ATXN3(SCA3/MJD), CACNA1A(SCA6), ATXN7(SCA7), ATXN10(SCA10), PPP2R2B(SCA12), TBP(SCA17), and ATN1(DRPLA) genes.
Patients without a recurrence pattern characteristic of an autosomal dominant inheritance were called “without an AD pedigree” (WADP) cases. The WADP group included isolated cases (without any family history) and individuals with recurrence only in their sibship. WADP individuals were firstly studied for the presence of GAA expansions at FXN gene, the gene associated with FRDA. If repeats within the normal range were found, then samples were included in the protocol of AD cases, as described above.
Data Analyses
Patient characteristics are given as mean ± SD and range. Age at onset and age at examination showed a normal distribution on Kolmogorov-Smirnov test: comparisons between diagnostic categories were performed through ANOVA test. Statistical significance threshold was set at 0.05. All statistical tests were performed in PASW 18.
Penetrance was considered the value equal to the ratio: symptomatic heterozygotes/all heterozygotes. Among SCA10 families, penetrance was estimated based on the occurrence of ataxia or dysarthria. Individuals with isolated seizures, if present, would be excluded from the penetrance estimation analysis. Asymptomatic individuals related to symptomatic subjects in a given family, and older than 45 years of age, were considered “asymptomatic obligate heterozygotes.” Since we did not have genotype data from majority of their relatives, we did not perform survival analyses to estimate penetrance. We called our estimation as “maximal family penetrance” when estimations studied only SCA10 families with recurrence cases (AD or recurrence in sibship). After that, we called “overall maximal penetrance” when estimations studied all SCA10 families, including isolated SCA10 cases. In this scenario, we consider that at least one parent plus one grandparent of an isolated case were obligate carriers. Grandparents were included in order to standardize families as presenting information from an average of three generations.
Results
About 115 individuals from 104 families were included, being 46 (38 families) AD and 69 (66 families) WADP cases. Results per AD and WADP groups as well as overall results are summarized in Table 1.
Among the 38 AD families, there were 1 family with SCA1, 6 with SCA2, 2 with SCA3/MJD, 2 with SCA6, 2 with SCA7, 15 with SCA10, and 10 families without a molecular diagnosis. Among the 66 WADP families, there were 2 families segregating SCA2, 1 SCA6, 7 SCA10, 9 FRDA (7 families with a definitive diagnosis and 2 with a possible diagnosis), and 47 families without a molecular diagnosis.
Therefore, a substantial amount of SCAs were molecularly confirmed in WADP individuals (or families). Overall, there were 48 SCA families (38 of them with a molecular diagnosis): 22 SCA10 families (46%), 8 SCA2 (17%), 3 SCA6 (6%), 2 SCA3 (4%), 2 SCA7 (4%), 1 SCA1 (2%), and 10 SCA families with a clear-cut family history but without molecular diagnosis (21%).
If WADP families whose investigation revealed a molecular diagnosis of SCA were removed, then the remaining 56 families can be identified as families with ataxic disorders other than SCAs (Fig. 1). Among them, there were nine FRDA families (14%), while up to 47 other families remained without a molecular diagnosis (86%).
Ataxic Families with a Molecular Diagnosis
General characteristics of SCA subjects are summarized in Tables 1 and 2. Although the limited number of cases prevents accurate comparisons, age at onset in SCA10 carriers seems to be older than in SCA2, SCA3/MJD, and SCA7 patients. Recruitment bias with predominance of severely affected cases among families cannot be ruled out, at least in SCA2 and SCA7, which compared to larger series have earlier age at onset and larger expanded CAG repeat lengths [11, 14]. Molecular diagnosis was very late in all forms, as can be seen by their ages at examination.
The most common hereditary ataxia was SCA10, represented by 22 index cases (i.e., families). About 14 index cases were AD and 8 were WADP. Among the eight index cases without an autosomal dominant pattern of inheritance, four had ataxic sibs. The age at onset of SCA10 patients with and without family history was not substantially different (Table 1). Most SCA10 individuals did not present seizures; subjects with isolated seizures were not detected in these families. The 22 SCA10 pedigrees were then extended in order to estimate the penetrance rate among these families (Supplemental File). About 82 carriers were identified within the 22 families: 70 were symptomatic (27 were genotyped) and 12 were asymptomatic individuals who were obligate heterozygotes like parents or grandparents (one each) of isolated cases. Overall maximal penetrance was equal to 70/82 or 85%. In the 18 families with recurrent symptomatic subjects (multiplex families), there were 66 symptomatic and 4 obligate carriers. Their penetrance (maximal family penetrance) was equal to 66/70 or 94%.
GAA expansions at FXN gene were found in homozygosis in seven families, where a definitive diagnosis of FRDA was obtained. General features of the ataxic subjects with confirmed FRDA are described in Table 1. Only one affected case was identified in each family. Consanguinity was not reported in any of the seven FRDA families. Six of them showed the classical phenotype combining ataxia, absent reflexes, and Babinski sign. Two other subjects from independent families carried a GAA expansion identified in only one allele, and therefore they remain as possible FRDA cases. Despite older age at onset (24 and 50), both cases experienced classical phenotype, with progressive ataxia, axonal polyneuropathy, and generalized areflexia with positive Babinski; thus both cases were considered as carrying a non-identified mutation in the other allele.
Discussion
In this study, we sought to describe the relative frequency of the most common hereditary ataxias in Peru. SCA10 was the most common ataxia, accounting for 21% of all ataxia families, followed by SCA2 (7.6%) and FRDA (9%). The most common ataxia worldwide, SCA3/MJD, was relatively rare, with only two families (2%) identified.
SCA10 revealed to be the most frequent SCA among ataxic families from Peru. Geographic distribution of SCA10 families by origin of the ancient affected family member (Fig. 2) shows that most of SCA10 families are located within region of influence of Amerindian Quechua language, harboring Peruvian populations with high Amerindian ancestry component [18, 19]. Until recently, SCA10 was only found in North, Central, and South American regions [12, 20,21,22]. More recently, one Chinese Han [23] and one Japanese family [24] were described. These data suggested an early Amerindian origin of the ATXN10 expansion and a North-South spreading with the settlers, through the ice-free corridor in the Pacific coast, 10 to 30,000 years ago. The SCA10 mutation may have a unique ancestral origin that either occurred before the divergence of Proto-Amerindians from ancestral Asians or that back-migrated to East Asia through the Bering Strait. Haplotype studies support this unique-origin hypothesis [23,24,25]. Peruvian population concentrates a large proportion of Amerindian ancestry, with geographical locations where this component represents more than 80% of estimated ancestry [18]. Therefore, finding SCA10 as the frequent ataxia in Peru is consistent with the theory of an Amerindian origin of this mutation.
Incomplete penetrance of SCA10 and late age of onset, as well as its milder presentation and slower progression compared to other SCAs, may have contributed to the ATXN10 expansion survival [5]. Formerly, we have shown that the Scale for Assessment and Rating of Ataxia (SARA) [26] and the Neurological Examination Score for SCAs-NESSCA [27] progressions were slower in SCA10 compared to other SCAs [5]. These factors might have contributed to ATXN10 expansions survival over around 400 to 800 generations (10 to 20,000 years) in populations of the New World.
Incomplete penetrance has been repeatedly reported in SCA10 [28,29,30,31]. For a number of reasons, penetrance estimation of late-onset disorders is a hard task. The best penetrance estimation approach requires genotyping entire 2–3 generation families and follows them over life span to identify all non-penetrant subjects. Since this approach was not applicable to our study, we estimated the maximal penetrance using available information gathered from pedigrees. Although Kaplan-Meyer survival estimates may reduce the confusion between non-penetrance and variable expressivity (very-late-onset cases), it does not avoid the fact that cohort-based data sets frequently contain an overrepresentation of patients (i.e., carriers of the gene variant of interest affected with the associated disease) and an underrepresentation of disease-free carriers. Moreover, family-based studies may not find families without recurrence [32]. Turning this scenario even more complicated, among the 22 SCA10 index cases, only 5 other genotypes were obtained within their relatives, all of them symptomatic subjects; majority of the available information was based on phenotypes, obtained by the family-based study (Supplemental File). Since our results most probably underwent to upward biases (i.e., overestimations), we decided to present just exploratory penetrance estimations and to call them as “maximal penetrance” rates. Taking these limitations into account, the present pedigrees show that the maximal penetrance was between 85 and 94% in SCA10. We should highlight the fact that these estimates ignored the possibility that some of asymptomatic sibs could be mutation carriers. Despite these limitations, these numbers emphasize the fact that SCA10 mutation is sometimes non-penetrant. Although we do not have a hypothesis to explain non-penetrance in SCA10, we suggest that studies genotyping all brotherhood, in a double-blind way, should be performed in the near future in order to clarify this phenomenon.
Other interesting result from our ataxic case series suggests that point mutations at FXN might be more frequent in Peru than in other populations. Only seven of the nine index cases segregating FRDA phenotype presented GAA expansions in homozygosis. The other two ataxic subjects (or 23% of the FRDA families) were probably compound heterozygotes for GAA expansion and a point mutation. These numbers are different than the usual homozygous GAA expansions seen in 96% of FRDA carriers around the world [33, 34]. However, our FRDA numbers are still small and might reflect an undetected recruitment bias favoring these cases among Peruvians.
The diagnostic process of inherited ataxias can be complex [15] and should be ideally guided by epidemiological data for each population. On the other hand, carriers of dominant forms sometimes have a negative family history; thus, isolated (or sporadic) cases should be investigated for both recessive and dominant disorders. Following that guideline, we identified 11 (17%) different SCAs among 66 families without an autosomal dominant pedigree (WADP): 8 SCA10, 2 SCA2, and 1 SCA6 were detected. About 4 of these SCA10 families actually showed recurrence between sibs (mimicking a recessive pattern), reducing the overall number of sporadic ataxic cases under study to 62. In fact, 7 SCA subjects (4 other SCA10, 2 SCA2, and 1 SCA6) out of these 62 (11%) were indeed AD forms presented as isolated cases. Similar rates of expanded SCA repeats, varying from zero to 13%, have been found among sporadic ataxic cases in Spain [35], Brazil [36], Japan [37], Mexico [12], China [38], and Greece [39]. Lack of knowledge about family history, as well as non-penetrance and instabilities of large repeats giving rise to “de novo” cases, might explain this phenomenon. The last mechanism has been reported in SCA6 [40] and in SCA2 [41].
There are some limitations of our study that must be considered for further studies. Since we did not offer pre-symptomatic diagnosis for inherited ataxias in Peru, we could not explore frequency of asymptomatic carriers. Due to the diagnostic approach, collecting samples for several months and sending them abroad (through Rede Neurogenetica), we were not able to estimate annual incidence rate of cases.
In conclusion, the unique distribution of inherited ataxias in Peru supports the development of specific panels addressed to the investigation of HA. SCA10 screening should be placed as first line of evaluations. Secondly, sporadic cases must be studied as deeply for AD forms as familial cases, especially in relation to the incomplete penetrance related to SCA10. Thirdly, our results suggest that point mutations at FXN might be more prevalent in Peru than elsewhere; whether or not FXN sequencing should be incorporated in future panels for this population remains to be established. The results of this study lay the groundwork for diagnosis guidelines of HA in Peru.
Change history
15 January 2020
The original version of this article unfortunately contained some mistakes in Table 2. The additional row (just above SCA2) with the following information “SCA1, 1(1), 1, 50, 74, 24, 46 and 0/1” should be inserted.
References
Jayadev S, Bird TD. Hereditary ataxias: overview. Genet Med. 2013;15:673–83.
Bird TD. Hereditary ataxia overview. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, et al., editors. GeneReviews®. Seattle: University of Washington, Seattle; 1993. [cited 2019 Mar 7]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1138/.
Sequeiros J, Martins S, Silveira I. Epidemiology and population genetics of degenerative ataxias. Handb Clin Neurol. 2012;103:227–51.
Durr A. Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol. 2010;9:885–94.
Gheno TC, Furtado GV, JAM S, Donis KC, AMV F, Emmel VE, et al. Spinocerebellar ataxia type 10: common haplotype and disease progression rate in Peru and Brazil. Eur J Neurol. 2017;24:892–e36.
Campuzano V, Montermini L, Moltò MD, Pianese L, Cossée M, Cavalcanti F, et al. Friedreich’s ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–7.
Bidichandani SI, Delatycki MB. Friedreich Ataxia. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, et al., editors. GeneReviews®. Seattle: University of Washington, Seattle; 1993. [cited 2019 Mar 7]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1281/.
Hagerman P. Fragile X-associated tremor/ataxia syndrome (FXTAS): pathology and mechanisms. Acta Neuropathol. 2013;126:1–19.
Ruano L, Melo C, Silva MC, Coutinho P. The global epidemiology of hereditary ataxia and spastic paraplegia: a systematic review of prevalence studies. Neuroepidemiology. 2014;42:174–83.
de Castilhos RM, Furtado GV, Gheno TC, Schaeffer P, Russo A, Barsottini O, et al. Spinocerebellar ataxias in Brazil – frequencies and modulating effects of related genes. Cerebellum. 2014;13:17–28.
Molecular epidemiology of spinocerebellar ataxias in Cuba: insights into SCA2 founder effect in Holguin. - PubMed - NCBI [Internet]. [cited 2019 Nov 30]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19429075.
Alonso E, Martínez-Ruano L, De Biase I, Mader C, Ochoa A, Yescas P, et al. Distinct distribution of autosomal dominant spinocerebellar ataxia in the Mexican population. Mov Disord. 2007;22:1050–3.
Teive HAG, Munhoz RP, Arruda WO, Raskin S, Werneck LC, Ashizawa T. Spinocerebellar ataxia type 10 – a review. Parkinsonism Relat Disord. 2011;17:655–61.
Paradisi I, Ikonomu V, Arias S. Spinocerebellar ataxias in Venezuela: genetic epidemiology and their most likely ethnic descent. J Hum Genet. 2016;61:215–22.
van de Warrenburg BPC, van Gaalen J, Boesch S, Burgunder J-M, Dürr A, Giunti P, et al. EFNS/ENS consensus on the diagnosis and management of chronic ataxias in adulthood. Eur J Neurol. 2014;21:552–62.
Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215.
Cagnoli C, Michielotto C, Matsuura T, Ashizawa T, Margolis RL, Holmes SE, et al. Detection of large pathogenic expansions in FRDA1, SCA10, and SCA12 genes using a simple fluorescent repeat-primed PCR assay. J Mol Diagn. 2004;6:96–100.
Harris DN, Song W, Shetty AC, Levano KS, Cáceres O, Padilla C, et al. Evolutionary genomic dynamics of Peruvians before, during, and after the Inca empire. Proc Natl Acad Sci U S A. 2018;115:E6526–35.
Instituto Nacional de Desarrollo de Pueblos Andinos, Amazónicos y Afroperuanos (INDEPA). Ethnolinguistic map of Peru. Rev Peru Med Exp Salud Publica. 2010;27:288–91.
Cintra VP, Lourenço CM, Marques SE, de Oliveira LM, Tumas V, Marques W. Mutational screening of 320 Brazilian patients with autosomal dominant spinocerebellar ataxia. J Neurol Sci. 2014;347:375–9.
Teive HAG, Munhoz RP, Raskin S, Arruda WO, de Paola L, Werneck LC, et al. Spinocerebellar ataxia type 10: frequency of epilepsy in a large sample of Brazilian patients. Mov Disord. 2010;25:2875–8.
Cornejo-Olivas M, Cornejo-Herrera I, Lindo-Samanamud S, Castilhos R, Saraiva-Pereira ML, Jardim L, et al. Spinocerebellar Ataxia Type 10 or SCA10 in Peruvian Population. First Report of Three Families (IN6–1.007). Neurology [Internet]. 2013 [cited 2019 Mar 7];80:IN6–1.007-IN6–1.007. Available from: https://n.neurology.org/content/80/7_Supplement/IN6-1.007.
Wang K, McFarland KN, Liu J, Zeng D, Landrian I, Xia G, et al. Spinocerebellar ataxia type 10 in Chinese Han. Neurol Genet. 2015;1:e26.
Naito H, Takahashi T, Kamada M, Morino H, Yoshino H, Hattori N, et al. First report of a Japanese family with spinocerebellar ataxia type 10: the second report from Asia after a report from China. PLoS One. 2017;12:e0177955.
Bampi GB, Bisso-Machado R, Hünemeier T, Gheno TC, Furtado GV, Veliz-Otani D, et al. Haplotype study in SCA10 families provides further evidence for a common ancestral origin of the mutation. NeuroMolecular Med. 2017;19:501–9.
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–20.
Kieling C, Rieder CRM, Silva ACF, JAM S, Cecchin CR, Monte TL, et al. A neurological examination score for the assessment of spinocerebellar ataxia 3 (SCA3). Eur J Neurol. 2008;15:371–6.
Matsuura T, Fang P, Pearson CE, Jayakar P, Ashizawa T, Roa BB, et al. Interruptions in the expanded ATTCT repeat of spinocerebellar ataxia type 10: repeat purity as a disease modifier? Am J Hum Genet. 2006;78:125–9.
Alonso I, Jardim LB, Artigalas O, Saraiva-Pereira ML, Matsuura T, Ashizawa T, et al. Reduced penetrance of intermediate size alleles in spinocerebellar ataxia type 10. Neurology. 2006;66:1602–4.
Gatto EM, Gao R, White MC, Uribe Roca MC, Etcheverry JL, Persi G, et al. Ethnic origin and extrapyramidal signs in an Argentinean spinocerebellar ataxia type 10 family. Neurology. 2007;69:216–8.
Schüle B, McFarland KN, Lee K, Tsai Y-C, Nguyen K-D, Sun C, et al. Parkinson’s disease associated with pure ATXN10 repeat expansion. NPJ Parkinsons Dis. 2017;3:27.
Jonker MA, Rijken JA, Hes FJ, Putter H, Hensen EF. Estimating the penetrance of pathogenic gene variants in families with missing pedigree information. Stat Methods Med Res. 2018;962280218791338.
Galea CA, Huq A, Lockhart PJ, Tai G, Corben LA, Yiu EM, et al. Compound heterozygous FXN mutations and clinical outcome in Friedreich ataxia. Ann Neurol. 2016;79:485–95.
Fussiger H, Saraiva-Pereira ML, Leistner-Segal S, Jardim LB. Friedreich Ataxia: diagnostic yield and minimal frequency in South Brazil. Cerebellum. 2019;18:147–51.
Pujana MA, Corral J, Gratacòs M, Combarros O, Berciano J, Genís D, et al. Spinocerebellar ataxias in Spanish patients: genetic analysis of familial and sporadic cases. The Ataxia Study Group. Hum Genet. 1999;104:516–22.
Jardim LB, Silveira I, Pereira ML, Ferro A, Alonso I, do Céu Moreira M, et al. A survey of spinocerebellar ataxia in South Brazil – 66 new cases with Machado-Joseph disease, SCA7, SCA8, or unidentified disease-causing mutations. J Neurol. 2001;248:870–6.
Maruyama H, Izumi Y, Morino H, Oda M, Toji H, Nakamura S, et al. Difference in disease-free survival curve and regional distribution according to subtype of spinocerebellar ataxia: a study of 1,286 Japanese patients. Am J Med Genet. 2002;114:578–83.
Wang J, Shen L, Lei L, Xu Q, Zhou J, Liu Y, et al. Spinocerebellar ataxias in mainland China: an updated genetic analysis among a large cohort of familial and sporadic cases. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2011;36:482–9.
Koutsis G, Pemble S, Sweeney MG, Paudel R, Wood NW, Panas M, et al. Analysis of spinocerebellar ataxias due to expanded triplet repeats in Greek patients with cerebellar ataxia. J Neurol Sci. 2012;318:178–80.
Shimazaki H, Takiyama Y, Sakoe K, Amaike M, Nagaki H, Namekawa M, et al. Meiotic instability of the CAG repeats in the SCA6/CACNA1A gene in two Japanese SCA6 families. J Neurol Sci. 2001;185:101–7.
Laffita-Mesa JM, Rodríguez Pupo JM, Moreno Sera R, Vázquez Mojena Y, Kourí V, Laguna-Salvia L, et al. De novo mutations in ataxin-2 gene and ALS risk. PLoS One. 2013;8:e70560.
Acknowledgments
Authors would like to thank patients and families affected from inherited ataxias that kindly contributed to research on ataxias in Peruvian population. We would also thank Diego Veliz-Otani for critical review of the manuscript. We are grateful to RIBERMOV “Red Iberoamericana Multidisciplinar para el Estudio de los Trastornos de Movimiento” for providing the initial environment for collaborative research studies, as this one, among Latin Americans.
Funding
EPM, GVF, GBB, SLS, MLSP, and LBJ were supported by the National Council for Research and Development (CNPq), Brazil. LBJ received grants from Fundo de Incentivo à Pesquisa do Hospital de Clínicas de Porto Alegre (FIPE 2006-0384) and Pesquisa para o SUS/Fundo de Apoio à Pesquisa do Rio Grande do Sul, Brazil (PPSUS-FAPERGS, PROCESS 07-00832), for performing the laboratory procedures. MCO, MIM, VM, and PM are partially supported by research funds provided by Instituto Nacional de Ciencias Neurológicas.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The additional row (just above SCA2) with the following information “SCA1, 1(1), 1, 50, 74, 24, 46 and 0/1” were inserted.
Electronic supplementary material
ESM 1
(DOCX 1544 kb)
Rights and permissions
About this article
Cite this article
Cornejo-Olivas, M., Inca-Martinez, M., Castilhos, R.M. et al. Genetic Analysis of Hereditary Ataxias in Peru Identifies SCA10 Families with Incomplete Penetrance. Cerebellum 19, 208–215 (2020). https://doi.org/10.1007/s12311-019-01098-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-019-01098-2