Abstract
Parkinson’s disease (PD) is one of the most common neurodegenerative disorders in the world. Previous studies have focused on the basal ganglia and cerebral cortices. To date, the cerebellum has not been systematically investigated in patients with PD. In the current study, 45 probable PD patients and 40 age- and gender-matched healthy controls underwent structural magnetic resonance imaging, and we used support vector machines combining with voxel-based morphometry to explore the cerebellar structural changes in the probable PD patients relative to healthy controls. The results revealed that the gray matter alterations were primarily located within the cerebellar Crus I, implying a possible important role of this region in PD. Furthermore, the gray matter alterations in the cerebellum could differentiate the probable PD patients from healthy controls with accuracies of more than 95 % (p < 0.001, permutation test) via cross-validation, suggesting the potential of analyzing the cerebellum in the clinical diagnosis of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a common progressive neurodegenerative disease, Parkinson’s disease (PD) is characterized by motor dysfunction, such as resting tremors, rigidity, and slowness of movements [1]. This disease affects millions of people worldwide and reduces their living quality and happiness. Thus far, the pathophysiology of the disease remains unclear.
Previous studies have demonstrated structural and functional alterations within the basal ganglia in PD patients relative to healthy controls [2, 3]. As a multisystem disease, PD is also observed with structural and functional abnormalities in cerebral cortex [4, 5]. Melzer et al. reported decreased perfusion in the posterior parieto-occipital cortex, precuneus and cuneus, and middle frontal gyri [6]. Additionally, Yu et al. demonstrated that the putamen, supplementary motor area (SMA), and pre-SMA are hypoactive in PD patients [7]. These previous studies have improved our understanding of the pathophysiology of PD, providing evidence that highlights the important roles of the cerebrum, especially the basal ganglia, in this disease.
The cerebellum plays a pivotal role in motor function [8], so structural or functional alterations of the cerebellum are likely to occur in PD patients. Zhang et al. observed disrupted white matter in the cerebellum of PD patients using DTI [9]. Several other studies found abnormal cerebellar activity or connectivity in PD patients using task-related functional MRI [10–12]. Structural abnormalities might contribute to the functional abnormalities observed in PD patients. Several previous studies have involved cerebellar gray matter abnormalities in PD patients more or less [13, 14]. In addition to motor function, the cerebellar Crus I plays roles in high-order functions as well [14, 15], while cognitive, emotional, and executive deficits are very common in the late stage of PD [1, 16, 17]. It is likely that the cerebellum plays a role in Parkinson’s disease include pathological and compensatory effects [18]. However, the gray matter structure of the cerebellum has not been systematically investigated in PD patients.
In this study, we used a multivariate pattern analysis (MVPA) approach which combined support vector machines (SVMs) with voxel-based morphometry (VBM) to explore cerebellar gray matter alterations in 45 probable PD patients relative to 40 matched healthy controls. Our aims were to identify cerebellar morphological abnormalities in the probable PD patients and to test the potential of these changes in the diagnosis of PD.
Materials and Methods
Subjects
We collected 45 probable PD patients and 40 age- and gender-matched healthy subjects (Table 1). The participants were all right-handed Chinese natives. All patients were diagnosed based on the UK Parkinson’s Disease Society Brain Bank Clinical Diagnostic Criteria. We excluded patients whose PD were induced by medications, metabolic diseases, encephalitis, and other neurodegenerative disease. Patients had at least two of the following signs: resting tremor, rigidity, and slowness of movements, at least one of which was bradykinesia (slowness). Patients were assessed with the Unified Parkinson’s Disease Rating Scale (UPDRS) while off their medications more than 12 h. For the PD patients, the disease duration was defined from the time of symptom onset. All subjects were assessed with the mini-mental state exam (MMSE). The clinical data of the probable PD patients are shown in Table 1. Two-tailed two-sample t tests and Pearson chi-square tests were used to compare the demographic data between the patients and healthy controls. Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Xuanwu Hospital’s Medical Research Ethical Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Image Acquisition
Data acquisition was performed on a 3-T scanner (Trio system; Siemens Magnetom scanner, Erlangen, Germany). We acquired the structural images with a T1-weighted 3-D magnetization-prepared rapid acquisition gradient echo (MPRAGE) sequence protocol [repetition time (TR) = 2000 ms, echo time (TE) = 2.19 ms, inversion time (TI) = 900 ms, flip angle = 9°, image matrix = 224 × 256, 176 slices, 1-mm isotropic voxel].
Image Preprocessing
The Diffeomorphic Anatomical Registration Exponentiated Lie Algebra (DARTEL) registration method [19] was used to process the images with SPM8 (Wellcome Department of Imaging Neuroscience, University College London, UK; http://www.fil.ion.ucl.ac.uk/spm). At first, the new segment procedure was performed to segment the structural MRI images into six partitions, including gray matter, white matter, cerebrospinal fluid, and three other background partitions based on a modified mixed model cluster analysis technique. Then, a template was generated from the entire image dataset using the DARTEL procedure, and the resulting images were spatially normalized into the standard Montreal Neurological Institute (MNI) space using an affine spatial normalization. Finally, the gray matter images were spatially normalized to the relative template (1.5-mm isotropic voxel) and smoothed with a 4-mm full width at half maximum isotropic Gaussian kernel. To eliminate possible edge effects, a mask covering voxels with gray matter densities above 0.2 was generated and then applied to all the gray matter images. The mask of the cerebellum was generated with the free software WFU_PickAtlas (version 3.0.4, http://www.ansir.wfubmc.edu) [20]. Then the gray matter voxels within the cerebellar mask were extracted for further analyses. To exclude the potential confounding effects of a generalized atrophy of the whole brain, the voxel-wise gray matter densities were corrected by regressing out global gray matter densities. The flowchart of data preprocessing can be seen in Fig. 1.
Pattern Classification
Before conducting the training and classification, feature selection could be necessary. The method of recursive feature elimination (RFE) [21] was introduced to identify the optimal feature number by maximizing prediction accuracy. The procedure of feature selection was performed on the training dataset; then the linear SVMs (http://www.kyb.tuebingen.mpg.de/bs/people/spider/index.html) were used to solve the classifications. The penalty parameter was equal to 1 (default setting) throughout the study. Cross-validation strategies were used to estimate the generalization ability of our classifiers. In this study, we used leave-one-out (LOOCV), fivefold, .632-fold (i.e., (1-1/e) [22], and twofold cross-validation strategies (100 times randomly partition for the latter three strategies). The flowchart of classification analysis can be seen in Fig. 1. In addition, permutation tests were employed to evaluate the performance of classifiers [23]. The class labels of the training data were randomly permuted first. Cross-validation was then performed on the permuted training set, and the permutation was repeated 10,000 times. The p value was the probability of observing a classification prediction rate no less than the actual classification accuracy.
Most Discriminative Gray Matter Regions
The N significantly different gray matter voxels identified by two-tailed two-sample t tests were selected during each cross-validation iteration, in which N was the feature number. Most discriminative features were defined as the features that appeared in all iterations of cross-validation [23], which were selected to reconstruct the anatomical regions with cluster sizes of no less than 100 voxels.
Clinical Correlation Analysis
An exploratory partial correlation analysis was performed to assess the correlations between gray matter densities of the cerebellar regions with group differences and clinical variables, i.e., the UPDRS score. Age was included as a confounding covariate. Two-sample two-tailed levels of significance were set at p < 0.05 and were uncorrected for multiple comparisons in the correlation analysis [24].
Results
Classification Results
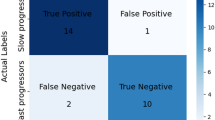
In the .632-fold strategy, the optimal feature number of 7600 was determined by using RFE method. Based on these selected features, the PD patients and controls could be classified with accuracies of 95.6 ± 3.3 % (97.6 ± 4.3 % for patients, 93.8 ± 6.1 % for controls, p < 0.001, Table 2). In addition, using LOOCV, fivefold, and twofold strategies, we obtained accuracies of 97.8 % (p < 0.0001), 96.9 ± 1.2 % (p < 0.001), and 97.2 ± 2.1 % (p < 0.001), respectively (Table 2), suggesting that the classification results were not sensitive to the cross-validation strategies.
Morphologic Changes in the Cerebellum
The cerebellar regions with high discriminative power were identified, mainly including the right medial Crus I, left Crus I, Vermis III, Vermis VIII, and right lateral Crus I (Table 3 and Fig. 2). The gray matter densities within the right medial Crus I, left Crus I, and Vermis III were decreased in the PD patients (p < 0.0001, uncorrected), while the gray matter densities within the Vermis VIII and right lateral Crus I were increased (p < 0.0001, uncorrected). The two-tailed two-sample t tests revealed no significant difference in the total brain gray matter, cerebellar gray matter, or cerebellar white matter between the two groups (p = 0.82, 0.21, and 0.45, respectively). None of the aforementioned regions was significantly correlated with the UPDRS scores, regardless of whether the age effects were removed or not.
Abnormal cerebellar gray matter regions in patients with Parkinson’s disease (a–e). Gray matter densities (GMD, corrected by regressing out global gray matter density) were significantly different (p < 0.0001, uncorrected) in each abnormal region (a–e) between the patient and control groups (f). The color intensity reflects the t statistic value between the patients and healthy controls, and the warm and cool colors indicate gray matter density increase and decrease, respectively
Discussion
In the current study, an MVPA approach was employed to differentiate PD patients from healthy controls based on structural MRI scans, resulting in accuracies of more than 95 % (p < 0.001) via different cross-validation strategies. The cerebellar gray matter changes are mainly distributed in the right medial Crus I, left Crus I, Vermis III, Vermis VIII, and right lateral Crus I.
In a previous study, Cherubini and colleagues employed SVM to discriminate tremor-dominant PD patients from essential tremor patients [25], indicating the discriminative power of the cerebellum in PD. In another study by Cherubini and colleagues, Parkinson’s disease and progressive supranuclear palsy (PSP) could be discriminated by structural MRI scans, including the structural alterations in the cerebellum [26], further suggesting the potential of the cerebellum in the classification of PD. The current study, in which we used the cerebellar gray matter density to differentiate the probable PD patients from healthy controls at the individual level, could complement the previous studies separating subtypes of Parkinsonism. The current results together with the previous findings suggest that the cerebellar structural alterations may have the potential in the diagnosis of Parkinsonism and its subtypes. A longitudinal study on a much larger sample including patients with different forms of Parkinsonism and healthy controls to ascertain the classification accuracy is warranted.
In the present study, the most discriminative gray matter voxels were mainly located in the cerebellar Crus I. Yu et al. observed hyperactivation of the cerebellar Crus I in PD patients [7]. Helmich et al. demonstrated a clear spatial segregation of lateral cerebellar Crus I with task-related activity in PD [27]. Wu et al. demonstrated more effective connectivity between bilateral cerebellum and left primary motor cortex while performing self-initiated movements in PD [10]. In addition to motor function, the cerebellar Crus I plays roles in high-order functions as well [14, 15]. Most areas of the Crus I observed here were assigned as default and control network components according to a priori functional network parcellation of the whole brain [28]. The default network is associated with emotional process, self-referential, and self-projection [29], and the control network is involved in working memory and cognitive control function [30]. Our recently study demonstrates that the neurobiological basis of head motion is associated with the functional connectivity within the default network [31]. The structural cerebellar abnormalities in the default network were reported in the PD patients with dementia in a recent study [32]. PD patients always suffer from the symptoms of depressed mood, and head and neck tremor [33], which may be associated with the abnormal activity and connectivity within the cerebellar part of the default network [10]. Cognitive and executive deficits are very common in PD; the gray matter alterations in the left medial and right cerebellar Crus I may be related to such deficits that are optionally present in PD [1, 16]. For the right lateral cerebellar Crus I, in addition to a possibility of pathophysiological change, it is also possible that the increased gray matter is a compensation for basal ganglia dysfunction to maintain motor and non-motor function at a near normal level [18].
The cerebellar Vermis III and VIII exhibited high discriminative power in the current study as well. The functional abnormalities have been demonstrated within the cerebellar vermis in patients with PD [34, 35]. The cerebellar vermis is connected with the limbic areas and has been proposed to be involved in emotion and motivation modulation [36]. Emotional deficit is common in the late stage of PD. Incidentally, in a late stage of data collection, we assessed depression in half sample of the current patient cohort (N = 22) and observed that seven patients have mild to moderate depression. As such, the gray matter alterations in the vermis together with default network part of the cerebellar Crus I may be related to emotional deficits in PD [24, 37]. For the increased gray matter in Vermis III, we would not exclude a possibility of compensatory effect for that the motivational processes are sometime relatively intact in PD [18].
Though the current study mainly focused on the cerebellum in PD, it is not against a critical role of basal ganglia in the pathophysiology of PD [2, 3]. In the past, the basal ganglia are the major clinical and research targets in PD. The univariate statistical analyses revealed that the gray matter of basal ganglia was significantly different between the probable PD patients and healthy controls in our cohort. Exactly, 52 % of the voxels with significant gray matter alterations in the probable PD patients were located in the basal ganglia (32 % in the cerebellum and 16 % in other brain areas). Using the gray matter density measures within the basal ganglia, the probable PD patients could be differentiated from the healthy controls with an accuracy of 100 % via cross-validation. The previous investigations demonstrated anatomical reciprocal connections between the basal ganglia and cerebellum [38], which may provide an anatomical basis to explain the role of the cerebellum in PD. The cerebellum receives a disynaptic projection from the subthalamic nucleus [38], and the subthalamic nucleus was described as the “driving force of the basal ganglia” [39]. The previous studies revealed different connectivity patterns between the cerebellum, basal ganglia, and supplementary motor area in early PD patients and controls during predictive motor timing [12], implying that the impaired striato-cerebellar connection may be a reflection of abnormal signals from the basal ganglia to influence cerebellar function [38]. The previous studies have provided evidence that the cerebellum may be involved in the gait disturbances and genesis of dyskinesia and that resting tremor may result from a pathological interaction between the basal ganglia and cerebello-thalamo-cortical circuit [18]. The gray matter alterations within the cerebellum observed in the current study might contribute to the functional anomaly or compensation in PD patients, providing structural imaging evidence to support possible pathological or compensatory roles of cerebellum in PD. However, the current results are very limited; further investigations are warranted to clarify pathological alterations in the cerebellum, and how cerebellar pathological and compensatory effects evolve as the PD progresses.
The current study still has some limitations. First, most PD patients are currently diagnosed based on the UK Parkinson’s Disease Society Brain Bank Clinical Diagnostic Criteria, and clinicians diagnose the disease incorrectly in approximately 25 % of patients [40]. Though all patients were evaluated by an experienced clinician (T.W.) in movement disorders and he attempted to conduct pathological confirmation, it is possible that, in some patients, the clinical diagnosis may have been in error. However, it remains unknown how many of the patients included here might suffer from an undiagnosed condition such as PSP or other forms of Parkinsonism. As such, the current study at least implies that the cerebellar gray matter abnormalities could differentiate between probable PD patients and controls, though the classification did not seem to be specific to idiopathic PD alone. Second, most patients had a symptom of mild tremor, which may confound the current results. Third, the medication effect on the patients was not considered in the current study. It is noted that the medication by neuropsychiatric patients during illness have potential effect on brain functions [41] and structures [37]. The potential effect of long-term medication on gray matter in PD should be examined carefully and should be considered in the future. Fourth, the cognitive, emotional, and executive deficits were not completely assessed in the patients. It is essential to collect these data in future studies. Finally, due to inter-subject brain differences and scanner variability, it is important to confirm the results with a larger sample size and multicenter imaging data.
Conclusion
The current study demonstrated that the gray matter alterations in the cerebellum could differentiate probable PD patients from healthy controls with accuracies of more than 95 % at the individual level and that the most gray matter alterations were located within the cerebellar Crus I, suggesting the a possible important role of the cerebellar Crus I in PD and the potential of the cerebellar structural changes in the diagnosis of PD.
References
Dirnberger G, Jahanshahi M. Executive dysfunction in Parkinson’s disease: a review. J Neurophysiol. 2013;7(2):193–224.
Shine JM, Matar E, Ward PB, Bolitho SJ, Gilat M, Pearson M, et al. Exploring the cortical and subcortical functional magnetic resonance imaging changes associated with freezing in Parkinson’s disease. Brain. 2013;136:1204–15.
Sterling NW, Du G, Lewis MM, Dimaio C, Kong L, Eslinger PJ, et al. Striatal shape in Parkinson’ s disease. Neurobiol Aging. 2013;34:2510–6.
Obeso JA, Rodriguez-Oroz MC, Goetz CG, Marin C, Kordower JH, Rodriguez M, et al. Missing pieces in the Parkinson’s disease puzzle. Nat Med. 2010;16:653–61.
Pyatigorskaya N, Gallea C, Garcia-Lorenzo D, Vidailhet M, Lehericy S. A review of the use of magnetic resonance imaging in Parkinson’s disease. Therapeut Adv Neurol Disord. 2014;7(4):12–26.
Melzer TR, Watts R, MacAskill MR, Pearson JF, Rueger S, Pitcher TL, et al. Arterial spin labelling reveals an abnormal cerebral perfusion pattern in Parkinson’s disease. Brain. 2011;134:845–55.
Yu H, Sternad D, Corcos DM, Vaillancourt DE. Role of hyperactive cerebellum and motor cortex in Parkinson’s disease. NeuroImage. 2007;35:222–33.
Middleton FA, Strick PL. The cerebellum: an overview. Trends Cogn Sci. 1998;2(9):305–6.
Zhang K, Yu C, Zhang Y, Wu X, Zhu C, Chan P, et al. Voxel-based analysis of diffusion tensor indices in the brain in patients with Parkinson’s disease. Eur J Radiol. 2011;77:269–73.
Wu T, Wang L, Hallett M, Chen Y, Li K, Chan P. Effective connectivity of brain networks during self-initiated movement in Parkinson’s disease. NeuroImage. 2011;55:204–15.
Husárová I, Lungu OV, Mareček R, Mikl M, Gescheidt T, Krupa P, et al. Functional imaging of the cerebellum and basal ganglia during predictive motor timing in early Parkinson’s disease. J Neuroimaging. 2014;24(1):45–53.
Husárová I, Mikl M, Lungu OV, Mareček R, Vaníček J, Bareš M. Similar circuits but different connectivity patterns between the cerebellum, basal ganglia, and supplementary motor area in early Parkinson’s disease patients and controls during predictive motor timing. J Neuroimaging. 2013;23(4):452–62.
Joana B. Pereira CJ, Maria J. Martı’, Blanca Ramirez-Ruiz, David Bartre’s-Faz, Eduard Tolosa. Structural brain correlates of verbal fluency in Parkinson’s disease. NeuroReport. 2009;20(8):741-4.
Bar M. Visual objects in context. Nat Rev Neurosci. 2004;5(8):617–29.
Habas C, Kamdar N, Nguyen D, Prater K, Beckmann CF, Menon V, et al. Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci. 2009;29(26):8586–94.
Chaudhuri KR, Healy DG, Schapira AHV. Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol. 2006;5:235–45.
Baumann O, Mattingley JB. Functional topography of primary emotion processing in the human cerebellum. NeuroImage. 2012;61(4):805–11.
Wu T, Hallett M. The cerebellum in Parkinson’s disease. Brain. 2013;136:696–709.
Ashburner J. A fast diffeomorphic image registration algorithm. NeuroImage. 2007;38:95–113.
Maldjian JA, Laurienti PJ, Burdette JB, Kraft RA. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. NeuroImage. 2003;19:1233–9.
Craddock RC, Holtzheimer PE, Hu XP, Mayberg HS. Disease state prediction from resting state functional connectivity. Magn Reson Med. 2009;62:1619–28.
Efron B, Tibshirani R. [Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy]: rejoinder. Statist Sci. 1986;1(1):77.
Zeng L-L, Shen H, Liu L, Wang L, Li B, Fang P, et al. Identifying major depression using whole-brain functional connectivity: a multivariate pattern analysis. Brain. 2012;135:1498–507.
Zeng L-L, Liu L, Liu Y, Shen H, Li Y, Hu D. Antidepressant treatment normalizes white matter volume in patients with major depression. PLoS One. 2012;7(8):e44248.
Cherubini A, Nistico R, Novellino F, Salsone M, Nigro S, Donzuso G, et al. Magnetic resonance support vector machine discriminates essential tremor with rest tremor from tremor-dominant Parkinson disease. Mov Disord. 2014;29(9):1216–9.
Cherubini A, Morelli M, Rita N, Salsone M, Arabia G, Vasta R, et al. Magnetic resonance support vector machine discriminates between Parkinson Disease and progressive supranuclear palsy. Mov Disord. 2014;29(2):266–9.
Helmich RC, Bloem BR, Toni I. Motor imagery evokes increased somatosensory activity in Parkinson’s disease patients with tremor. Hum Brain Mapp. 2012;33:1763–79.
Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BTT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106(5):2322–45.
Gusnard DA, Akbudak E, Shulman GL, Raichle ME. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc Natl Acad Sci U S A. 2001;98(7):4259–64.
Vincent JL, Kahn I, Snyder AZ, Raichle ME, Buckner RL. Evidence for a frontoparietal control system revealed by intrinsic functional connectivity. J Neurophysiol. 2008;100:3328–42.
Zeng L-L, Wang D, Fox MD, Sabuncu M, Hu D, Ge M, et al. Neurobiological basis of head motion in brain imaging. Proc Natl Acad Sci U S A. 2014;111(16):6058–62.
Rektorova I, Biundo R, Marecek R, Weis L, Aarsland D, Antonini A. Grey matter changes in cognitively impaired Parkinson’s disease patients. PLoS One. 2014;9(1):e85595.
Yarnall A, Archibald N, Burn D. Parkinson’s disease. Mov Disord. 2012;40(10):529–35.
Ekman U, Eriksson J, Forsgren L, Mo SJ, Riklund K, Nyberg L. Functional brain activity and presynaptic dopamine uptake in patients with Parkinson’s disease and mild cognitive impairment: a cross-sectional study. Lancet Neurol. 2012;11:679–87.
Ko JH, Mure H, Tang CC, Ma Y, Dhawan V, Spetsieris P, et al. Parkinson’s disease: increased motor network activity in the absence of movement. J Neurosci. 2013;33(10):4540–9.
Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex. 2010;46:831–44.
Zeng L-L, Shen H, Liu L, Fang P, Liu Y, Hu D. State-dependent and trait-related gray matter changes in nonrefractory depression. NeuroReport. 2015;26:57–65.
Bostan AC, Dum RP, Strick PL. The basal ganglia communicate with the cerebellum. Proc Natl Acad Sci U S A. 2010;107(18):8452–6.
Kitai ST, Kita H. The basal ganglia II—structure and function: current concepts. New York: Plenum; 1987.
Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson’s disease. Lancet Neurol. 2006;5:75–86.
Aarts E, Nusselein AAM, Smittenaar P, Helmich RC, Bloem BR, Cools R. Greater striatal responses to medication in Parkinson’s disease are associated with better task-switching but worse reward performance. Neuropsychologia. 2014;62:390–7.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Xuanwu Hospital’s Medical Research Ethical Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
This study was funded by the National Science Foundation of China (61503397, 61420106001, 61375111, and 61375034) and National High-tech Program of China (2012AA011601).
Rights and permissions
About this article
Cite this article
Zeng, LL., Xie, L., Shen, H. et al. Differentiating Patients with Parkinson’s Disease from Normal Controls Using Gray Matter in the Cerebellum. Cerebellum 16, 151–157 (2017). https://doi.org/10.1007/s12311-016-0781-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-016-0781-1