Abstract
Social cognitive dysfunction, including deficits in facial emotion recognition and theory of mind, is a core feature of schizophrenia and more strongly predicts functional outcome than neurocognition alone. Although traditionally considered to play an important role in motor coordination, the cerebellum has been suggested to play a role in emotion processing and theory of mind, and also shows structural and functional abnormalities in schizophrenia. The aim of this systematic review was to investigate the specific role of the cerebellum in emotion and theory of mind deficits in schizophrenia using previously published functional neuroimaging studies. PubMed and PsycINFO were used to search for all functional neuroimaging studies reporting altered cerebellum activity in schizophrenia patients during emotion processing or theory of mind tasks, published until December 2014. Overall, 14 functional neuroimaging studies were retrieved. Most emotion studies reported lower cerebellum activity in schizophrenia patients relative to healthy controls. In contrast, the theory of mind studies reported mixed findings. Altered activity was observed across several posterior cerebellar regions involved in emotion and cognition. Weaker cerebellum activity in schizophrenia patients relative to healthy controls during emotion processing may contribute to blunted affect and reduced ability to recognise emotion in others. This research could be expanded by examining the relationship between cerebellum function, symptomatology and behaviour, and examining cerebellum functional connectivity in patients during emotion and theory of mind tasks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Social cognition consists of processes that enable people to perceive and process information about themselves and other people [1]. These processes underpin social skills used every day, such as recognising emotions from people’s faces or understanding what other people are thinking. These skills are essential in daily life, for example understanding that another person is upset or that certain types of behaviour may be seen as inappropriate.
Impairments in social cognition are a core feature of schizophrenia [2] and are stronger predictors of functional outcomes in employment, relationships and independent living than neurocognition alone [3]. Similarly, efforts to ameliorate social cognitive deficits are likely to significantly improve patient quality of life and social functioning. Thus, social cognition has emerged as a potential target for developing new treatments, both pharmacological and cognitive, aimed at improving clinical outcomes.
Given that many pharmaceutical companies have reduced investment in drug development for psychiatric disorders due to their perceived complexity [4], elucidating the biological mechanisms underlying specific aspects of schizophrenia-related disability is a core priority for the field (e.g. as reflected in the NIMH Research Domain Criteria initiative, RdoC; [5]). Social cognition, described as ‘systems for social processes’, is one of the six domains that have been selected as a potentially tractable avenue of progress towards the goals of identifying (a) specific treatment targets (e.g. molecular pathways), (b) translational models to test the effects of particular therapies and (c) biomarkers for more accurate diagnosis.
In understanding the neural mechanisms of social cognition, functional neuroimaging has a key role in identifying specific brain regions and networks disrupted in schizophrenia patients during social information processing. Combining imaging data with genetic and/or environmental data can, additionally, help elucidate molecular and social risk factors affecting the brain [6, 7]. One brain region that has been reported in a number of schizophrenia studies to be activated during social cognitive performance is the cerebellum, a brain region more traditionally associated with aspects of motor function. This review discusses the possible contribution of the cerebellum to social cognition in schizophrenia, examining whether this brain region may play a role in the abnormal processing of two components of social information—emotion recognition and theory of mind—characteristic of the disorder [8].
Facial Emotion
Facial emotion recognition is important for correctly inferring the emotional state of another person, an important type of non-verbal communication. In schizophrenia, meta-analysis of neuropsychological studies suggests that patients show large deficits in facial emotion recognition, deficits that are associated with differences in functional outcomes such as community functioning [2, 9]. Facial emotion recognition deficits are thought to arise due to impaired emotion processing, which also behaviourally manifests as flattened affect, a core feature of the disorder [10, 11]. Although patients report normal ratings of experience of emotion, they show reduced emotional expression and reduced emotion perception in response to emotional stimuli, including during social interactions [12]. This could contribute to a decreased ability to recognise certain facial expressions and understand how others are feeling.
Theory of Mind
Theory of mind (also known as mentalising) is the cognitive ability required to attribute mental states to oneself and to other people [1, 13]. Unlike facial emotion recognition, theory of mind also involves processing of spatial and contextual information rather than perception of direct emotional signals alone [14]. Although adult reasoning about the mental states of others can be complex and likely draws on other cognitive processes such as attention and language, theory of mind is nonetheless thought to develop from simpler, automatic cognitive processes such as the detection of goals and agency in moving shapes that are observed in infants as young as six and a half months old [15]. Meta-analysis of neuropsychological studies suggests that schizophrenia patients generally show significant deficits in theory of mind, and impaired mentalising is a stronger predictor of functional outcome than other social cognitive measures [3].
Other Cognitive Deficits Associated with Schizophrenia
Patients with schizophrenia consistently present with a wide variety of perceptual and cognitive impairments, including general cognitive decline, memory deficits and deficits in working memory and attention control often referred to more general as ‘executive’ deficits. Collectively, these deficits significantly predict functional outcome over and above the so-called positive and negative clinical symptoms [16–18]. Of these ‘executive’ functions, working memory (which allows people to maintain, store and manipulate information over short periods; [19]), appears to be particularly correlated with decline in both general cognitive ability and difficulties with other specific cognitive abilities, including reasoning, problem-solving and learning [20–24].
The Role of the Cerebellum in Emotion and Theory of Mind
A prevailing view for many years held that the exclusive role of the cerebellum was to collect information from multiple cortical areas and feed this information to the primary motor cortex to coordinate movement [25, 26]. However, anatomical, neurological and neuroimaging studies have challenged this idea.
For example, cerebellar damage from trauma, tumours, infection or stroke has been associated with cognitive and emotional deficits in addition to motor problems [27, 28]. Clinically defined as Schmahmann’s syndrome (and also known as cerebellar cognitive affective syndrome (CCAS)), these deficits include impaired working memory, reasoning and planning, flattened affect and inappropriate behaviour [29, 30]. These deficits are consistent with both social-emotional deficits observed in schizophrenia and with cognitive deficits observed outside of the social-emotional area (e.g. deficits in executive function).
Schmahmann’s syndrome is more frequently associated with lesions to the posterior lobe of the cerebellum (including lobules VI to IX, Crus I and Crus II, and the midline vermis), suggesting a particularly important role for posterior regions in executive function, social cognition and emotion [30, 31]. These clinical findings are supported by functional neuroimaging studies which report cerebellar activation in different but overlapping regions associated with sensory, cognitive and emotion processing. For example, activation likelihood estimation (ALE) meta-analysis of 53 functional magnetic resonance imaging (fMRI) studies by Stoodley and Schmahmann [32] reported activation in lobules VI–VIII and Crus I associated with working memory, other executive functions and emotion processing. In contrast, sensory processing was also associated with activation in lobule V. More recently, ALE meta-analysis of over 350 fMRI studies by Van Overwalle and colleagues [8] suggests that posterior cerebellar regions are active during theory of mind (including lobules VI and VII). Van Overwalle et al. [33] later examined these findings in light of functional connectivity analysis of the cerebellum by Buckner et al. [38], revealing that the cerebellum regions involved in mentalising overlap with regions correlating with default mode activity.
Finally, Riedel et al. [34] performed two meta-analyses examining (a) co-activation of the cerebellum with cortical regions, and (b) association of cerebellar activation with cognitive/emotional processes, using published neuroimaging data from the BrainMap database. Supporting previous findings, activation across lobules VII–VIII, Crus I and Crus II was associated both with co-activation in the prefrontal cortex and with executive processing. However, activation across lobules I–IV was associated with emotion processing, suggesting that activation in anterior regions may play a role in emotion also.
Further highlighting a role for the cerebellum in social cognition, individuals with cerebellar stroke show reduced amygdala and medial prefrontal activity during emotion processing [35], and resting-state fMRI reveals that neural activity in other cortical regions important for social cognition and emotion correlate with activity in lobules VI and VII, suggesting communication between these regions during rest [36–38]. In particular, Buckner et al. [38] reported that a substantial portion of the cerebellum, including Crus I and Crus II, shows correlations with the default mode network, which plays a critical role in theory of mind.
In patients with schizophrenia, functional neuroimaging studies have reported reduced cerebellar activity during memory processing [39, 40], including working memory [41], and finger-tapping [42], suggesting this structure might contribute to working memory and executive deficits observed in the disorder. During rest, lower cerebellar metabolism [43] and weaker functional connectivity between the cerebellum and prefrontal cortex have also been observed [44]. Functional connectivity can be described as the temporal correlation of neural activity between two or more separate brain areas and is thought to indicate communication between different parts of the brain [45].
Post-mortem studies of schizophrenia patients report 8.3 % decreased size of inhibitory Purkinje cells in the cerebellar vermis [46], while structural imaging studies report reduced white matter integrity of tracts connecting the cerebellum to cortical regions [47, 48], and reduced volume of the cerebellum relative to healthy controls, which also predicts negative psychosocial outcomes [49].
Given the evidence that (a) emotion processing and theory of mind are affected in schizophrenia, (b) the cerebellum shows increased activity during emotion and theory of mind tasks, and (c) cerebellum activity and structure is altered in schizophrenia, we sought to systematically review all previously published functional imaging studies that report altered cerebellum activity in schizophrenia during emotion processing or theory of mind tasks in order to examine the possible contribution of this structure towards emotion and/or theory of mind deficits in the disorder.
Materials and Methods
Using Pubmed and PsycINFO, we searched for all functional neuroimaging studies reporting altered cerebellum activity in schizophrenia patients during emotion or theory of mind tasks. Studies published until December 2014 were searched for with the following search term: ‘(schizophrenia OR schiz*) AND cerebellum AND (emotion OR theory of mind) AND (functional magnetic resonance imaging OR positron emission tomography OR single photon emission computed tomography OR electroencephalography OR magnetoencephalography OR fMRI OR PET OR SPECT OR EEG OR MEG) NOT Review’. This resulted in 22 studies being identified in total. Seven studies were excluded as they were part of the Molecular Imaging and Contrast Agent Database (an online database containing information about molecular imaging and contrast agents), three studies were excluded as they used structural imaging and/or transcranial magnetic stimulation and thus did not directly examine cerebellar activity during emotion or theory of mind, and one study was excluded as it did not examine patients with schizophrenia. Thus, 11 original studies matched the study criteria. This literature search was supplemented with a review of the references from each of the papers identified. This additional search retrieved a further three studies matching the criteria. In total, 14 studies meeting search criteria were retrieved.
In each study identified, altered cerebellar activity was observed in a whole-brain analysis (i.e. no a priori cerebellum regions of interest were reported). Seven of the 14 studies reported Positive and Negative Syndrome Scale scores (PANSS) [50–56], four studies reported Scale for the Assessment of Positive Symptoms (SAPS) and Scale for the Assessment of Negative Symptoms (SANS) scores [57–60], one study reported Brief Psychiatric Rating Scale (BPRS) and SANS scores [61], one study reported BPRS scores only [62], and one study did not report symptom severity [63].
Similarly, ten studies reported antipsychotic dosages, either reported as chlorpromazine equivalent in mg per day [57, 50–53] or reported by listing dosage in mg of each antipsychotic separately [54, 61, 55, 62, 56]. Three studies reported that all patients were either drug naïve or medication free for the three weeks prior to scanning [58–60] and one study did not report presence or absence of medication [63].
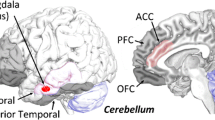
In Tables 1 and 2, we present for each study clusters showing significant differences in cerebellum activity when groups of interest were compared (e.g. patients versus controls, male patients versus female patients). In some studies, no significant effects were reported between groups, or groups were not compared directly; in these studies, we list any cerebellum findings reported in one group only. For each of these clusters, Montreal Neurological Institute (MNI) coordinates of significant maxima were entered into the Anatomy toolbox in SPM 8 [64–66], and anatomical regions (with associated probability estimates) were identified using the AllAreas_v18_MPM atlas, which contains the Probabilistic Atlas of the Human Cerebellum developed by Diedrichsen and colleagues [67]. Where coordinates were initially presented in Talairach space, these were converted to MNI space using GingerALE 2.1 software (‘Talairach to MNI (SPM)’ transform) [68, 69] and rounded to the nearest whole number. MNI coordinates of significant maxima for (a) emotion studies and (b) theory of mind studies were then plotted on a standard brain template in SPM 8 to show the distribution of these maxima across left and right hemispheres (Fig. 1).
Next, we used the ALE method in GingerALE to perform a meta-analysis, combining coordinates from (a) each of the emotion studies and (b) each of the theory of mind studies, in order to examine whether any clusters showed consistent differences between patients and controls [68–71]. We only included studies that directly compared patients and controls and reported a clusters showing altered cerebellum activation between groups (seven emotion studies and two theory of mind studies).
Results
Emotion Processing Studies
Six studies reported decreased cerebellum activity in schizophrenia patients relative to healthy controls during emotion processing tasks, one study reported increased activity in patients relative to healthy controls, and one study reported no statistically significant differences between patients and controls (though task-dependent activity was observed in controls only and not patients) (see Table 1; Fig. 1a). These results were based on either blood-oxygenated level-dependent (BOLD) signal (fMRI) or cerebral blood flow (CBF; positron emission tomography, PET).
Interpretations of these results are limited by the heterogeneity of the patient samples used, including samples with varying levels of symptom severity and medication dosage. Studies also presented different types of stimuli to examine emotion processing, including videos of facial emotion [57], pictures of facial emotion [53], images from the International Affective Picture System [59, 62, 61, 51, 63] and pleasant/unpleasant olfactory stimuli [60].
In addition, three studies reported effects of gender [54, 52] and negative symptoms [55, 52] within a group of schizophrenia patients. These studies reported increasing cerebellum activity during sad film viewing correlated with negative symptoms in males but not in females [52], increasing cerebellar activity in males relative to females during processing of negative images [54], and a pattern of increased cerebellar activity during sad film viewing observed in patients with blunted affect but not in patients without [55]. Cerebellum clusters showing altered activity in patient groups in these studies were observed across both cerebellar hemispheres in these studies, with several clusters observed in the posterior cerebellum.
Theory of Mind Studies
One study reported increased cerebellum activity in schizophrenia patients relative to healthy controls during theory of mind, one study reporting decreased activity, and one study reported no significant differences in cerebellum activity when the groups were compared (though task-dependent activity was observed in patients only and not controls) [56, 58, 50] (Table 2; Fig. 1b). These studies also presented different types of stimuli to examine theory of mind processing, including videos of moving shapes [50], visual presentation of verbal stories [58] and static cartoon strips [56], but each of these tasks required participants to mentlalise about momentary actions and beliefs rather than enduring personality traits or more abstract trait inferences [1]. Cerebellar clusters showing altered activity in patients were reported in regions including bilateral lobule VI and right Crus II.
ALE Meta-analysis
ALE meta-analysis of the seven emotion studies revealed one cluster in the left culmen that showed significant overlap between two of the studies [59, 60] (Fig. 2a; p < 0.01, false discovery rate (FDR) corrected and volume >200 mm3). ALE meta-analysis of the two theory of mind studies revealed one cluster in the left vermis that showed significant overlap between the studies [50, 58] (Fig. 2b; p < 0.01, FDR corrected and volume >200 mm3).
ALE activation maps for clusters showing significant overlap between a two emotion studies and b two theory of mind studies (p < 0.01, FDR corrected and volume >200 mm3), rendered on the ‘ch256’ brain template using MRIcroGL (http://www.mccauslandcenter.sc.edu/mricrogl/)
Discussion
This review described neuroimaging studies that reported altered function of the cerebellum in patients with schizophrenia during emotion processing and theory of mind. Consistent with reports of lower cerebellum activity in schizophrenia in both resting-state studies and studies of other cognitive functions [41, 43], patients generally showed lower cerebellar activity relative to healthy controls during emotion processing. In addition, three studies reported effects of gender and/or symptom severity on cerebellar function in patients during emotion processing. Association between cerebellar activity and theory of mind were more equivocal by comparison. In presenting this evidence for the cerebellum’s role in aberrant emotional processing in schizophrenia, this review highlights a broader role for the cerebellum in schizophrenia pathophysiology than simply in cognitive dysfunction [72].
Weaker engagement of the cerebellum during emotion processing may contribute to the blunted affect and difficulties recognising emotion in others associated with schizophrenia [10, 11]. Consistent with this hypothesis, both established and experimental treatments for schizophrenia have been suggested to exert some of their effects through a mechanism of altered cerebellum activity. Surguladze et al. [53] reported increased cerebellum activity in patients treated with risperidone compared to patients treated with conventional antipsychotics during facial emotion recognition. In an attempt to treat affective symptoms more specifically, Demirtas-Tatlidede et al. [73] used MRI-guided transcranial magnetic stimulation (TMS) to increase vermal activity in schizophrenia patients, and this was associated with improvements in mood and negative symptoms. To confirm the hypothesised contribution of the cerebellum to altered emotion recognition in schiozphrenia, it will be important for future MRI studies of emotion in schizophrenia to include the cerebellum in addition to corticolimbic regions typically associated with affective symptoms, particularly regarding choice of regions of interest and regions for inclusion in functional connectivity analyses.
Two of the studies in our review reported that male patients with schizophrenia displayed altered cerebellum activity compared to female patients during emotion processing. Mendrek et al. [54] observed right vermis activity in males relative to females when viewing negative images and later [52] observed that left vermis activity in males was correlated with negative symptoms, but this pattern was not observed in females. In healthy volunteers, gender differences in vermis activity during emotion processing have also been widely reported, albeit in what appears to be the opposite direction. In a meta-analysis of 88 functional neuroimaging studies [74], female volunteers displayed increased right vermis activity relative to males. While the schizophrenia studies reported here appear to be in the opposite direction, any conclusions about patient-specific effects remain speculative due to the small number of studies that have directly examined gender. Future studies including both patients with schizophrenia and healthy volunteers will no doubt shed further light on this question by further examining gender × diagnosis interactions.
Cerebellar effects on emotion processing in schizophrenia were not confined to either hemisphere. Patients with schizophrenia displayed altered activity in both cerebellar hemispheres in the emotion studies, consistent with previous research reporting bilateral cerebellar activation during emotion processing [32, 75]. Clusters in the vermis [52, 54, 60], left Crus I [57] and right lobule VI [54] are also consistent with previous clinical and neuroimaging data implicating these regions in emotion processing [31, 32]. However, ALE meta-analysis of coordinates from the seven emotion studies directly comparing patients and controls revealed a cluster showing overlap only between two of the studies [59, 60]. This suggests that results from the emotions studies are variable across studies, possibly owing to the variety of emotion processing tasks employed (although the two studies identified in the meta-analysis used different emotion processing tasks, suggesting that similar patterns might be observed despite the use of different tasks).
Thus, although this review suggests that the cerebellum is affected in schizophrenia during emotion processing, the variability of the results and experiments used and the lack of significant clusters observed across the studies in the meta-analysis do not allow us to infer how specifically the cerebellum might be affected. Further neuroimaging studies of emotion processing in schizophrenia will no doubt help to clarify this point, using more similar tasks and examining patients with similar levels of symptom severity and medication.
It should be noted that some of the cerebellar clusters reported were, based on the Anatomy Toolbox used in this review, adjacent to the cerebellum, e.g. [54, 63, 59]. This was likely due to individual differences in cerebellar morphology and differences in MRI pre-processing methodologies that may affect localisation of cerebellum coordinates [32]. Whatever the reason, confirming whether these clusters are cerebellar or rather adjacent to the cerebellum will likely be clarified as data from further studies accumulate. In addition, one cluster appeared to be localised outside the cerebellum and adjacent regions [51].
Results from ALE meta-analysis by Van Overwalle et al. [8, 33] and functional connectivity analysis by Buckner et al. [38] suggest the cerebellum plays an important role in theory of mind, with areas such as Crus I consistently activated during abstract mentalising tasks, and showing functional connectivity with the default network. However, differences in cerebellum activity during theory of mind in schizophrenia revealed by this study were equivocal both in the specific region activated and in the direction of activation. Specifically, relative to controls, patients showed decreased right posterior cerebellum activity during a verbal theory of mind task [58] but increased left posterior cerebellum activity during a theory of mind task that emphasised spatial processing [50]. ALE meta-analysis of the theory of mind studies revealed only one cluster in the left vermis showing significant overlap between these studies. However, the paucity of studies showing any cerebellar effects on theory of mind, and the differences in verbal versus spatial tasks used, makes interpretation of these inconsistencies hazardous. Also, each theory of mind task required participants to engage in momentary mental state inferences rather than abstract trait inferences. Thus, given that the cerebellum plays a particularly important role in abstract mentalising [8, 33], it will be a priority for future studies to examine whether cerebellum activity is altered in schizophrenia patients specifically during this type of theory of mind.
In terms of limitations, this review only examined studies that reported altered function of the cerebellum. Using the same search term and excluding ‘cerebellum’ yielded 480 studies, suggesting that there is likely to be a large body of functional neuroimaging literature on emotion and theory of mind in schizophrenia in which altered cerebellum activity was either not examined or not reported. Also, due to the under-publication of negative findings, other neuroimaging studies of emotion and theory of mind in schizophrenia may not have been retrieved. As a result, the studies examined in this review may misrepresent the role of the cerebellum in emotion and theory of mind in schizophrenia. However, these results could be extended by more systematic investigation of the cerebellum in schizophrenia as more studies, including negative findings, are published.
A second limitation is that, for those studies that did report cerebellar effects, these effects were not the primary focus of these studies and were likely to represent an incidental finding. Arising from this, the relationship between cerebellum activity and either symptom severity or task accuracy was not considered in most studies. Future studies could address this issue by examining effects of cerebellum activity in schizophrenia on behaviour and symptomatology, similar to the approach taken by Mendrek et al. [52].
Future imaging studies could also advance our knowledge of the cerebellum’s role in schizophrenia by examining functional connectivity between this region and other brain regions during emotion/theory of mind tasks. Abnormal functional connectivity has been proposed as a key etiological factor in schizophrenia [76], and is observed in patients relative to healthy controls across different imaging modalities [77–80], and during emotion processing [81]. Abnormal functional connectivity between the cerebellum and brain regions important in emotion processing and theory of mind (e.g. the medial prefrontal cortex (mPFC)) has already been observed in schizophrenia patients relative to healthy controls [44].
Conclusion
In conclusion, we reviewed the evidence from all functional neuroimaging studies reporting abnormal cerebellum function in schizophrenia patients during emotion processing and theory of mind tasks. During performance of emotion recognition tasks, patients showed lower cerebellum activity during emotion processing relative to healthy controls, consistent with resting-state studies and studies of neuropsychological function. Associations between cerebellar function and theory of mind were more equivocal. Future studies can add to what is known about the cerebellum in schizophrenia by (a) examining the effects of abnormal cerebellum function on clinical symptom severity and behaviour, and (b) establishing whether functional connectivity between the cerebellum and corticolimbic regions is altered in patients relative to controls during emotion and theory of mind tasks. Doing so may help further elucidate the contributions of this structure to emotional and cognitive deficits in schizophrenia.
References
Van Overwalle F. Social cognition and the brain: a meta‐analysis. Hum Brain Mapp. 2009;30(3):829–58.
Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32 suppl 1:S44–63.
Fett A-KJ, Viechtbauer W, Dominguez M-d-G, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011;35(3):573–88.
Brady LS, Insel TR. Translating discoveries into medicine: psychiatric drug development in 2011. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2012;37(1):281–3.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatr. 2010;167(7):748–51.
Walter H, Schnell K, Erk S, Arnold C, Kirsch P, Esslinger C, et al. Effects of a genome-wide supported psychosis risk variant on neural activation during a theory-of-mind task. Mol Psychiatry. 2011;16(4):462–70.
Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, et al. Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatry. 2012;71(4):286–93.
Van Overwalle F, Baetens K, Mariën P, Vandekerckhove M. Social cognition and the cerebellum: a meta-analysis of over 350 fMRI studies. Neuroimage. 2014;86:554–72.
Kohler CG, Walker JB, Martin EA, Healey KM, Moberg PJ. Facial emotion perception in schizophrenia: a meta-analytic review. Schizophr Bull. 2010;36(5):1009–19.
Aleman A, Kahn RS. Strange feelings: do amygdala abnormalities dysregulate the emotional brain in schizophrenia? Prog Neurobiol. 2005;77(5):283–98.
Gur R, Nimgaonkar V, Almasy L, Calkins M, Ragland J, Pogue-Geile M, et al. Neurocognitive endophenotypes in a multiplex multigenerational family study of schizophrenia. Am J Psychiatr. 2007;164(5):813–9.
Aghevli MA, Blanchard JJ, Horan WP. The expression and experience of emotion in schizophrenia: a study of social interactions. Psychiatry Res. 2003;119(3):261–70.
Goldman AI, Margolis E, Samuels R, Stich S. Theory of mind. Oxford handbook of philosophy and cognitive science. Oxford: Oxford University Press; 2012:402-24.
Schnell K, Bluschke S, Konradt B, Walter H. Functional relations of empathy and mentalizing: an fMRI study on the neural basis of cognitive empathy. Neuroimage. 2011;54(2):1743–54.
Csibra G. Goal attribution to inanimate agents by 6.5-month-old infants. Cognition. 2008;107(2):705–17.
Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72(1):29–39.
McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164(12):1791–802.
Lewandowski KE, Cohen BM, Keshavan MS, Öngür D. Relationship of neurocognitive deficits to diagnosis and symptoms across affective and non-affective psychoses. Schizophr Res. 2011;133(1):212–7.
Baddeley A. Working memory. Science. 1992;255(5044):556–9.
Süß H-M, Oberauer K, Wittmann WW, Wilhelm O, Schulze R. Working-memory capacity explains reasoning ability—and a little bit more. Intelligence. 2002;30(3):261–88.
Baddeley A. Working memory and language: an overview. J Commun Disord. 2003;36(3):189–208.
Colom R, Rebollo I, Palacios A, Juan-Espinosa M, Kyllonen PC. Working memory is (almost) perfectly predicted by g. Intelligence. 2004;32(3):277–96.
Bühner M, Kröner S, Ziegler M. Working memory, visual-spatial-intelligence and their relationship to problem-solving. Intelligence. 2008;36(6):672–80.
Colom R, Abad FJ, Quiroga MÁ, Shih PC, Flores-Mendoza C. Working memory and intelligence are highly related constructs, but why? Intelligence. 2008;36(6):584–606.
Thach WT, Goodkin H, Keating J. The cerebellum and the adaptive coordination of movement. Annu Rev Neurosci. 1992;15(1):403–42.
Bostan AC, Dum RP, Strick PL. Cerebellar networks with the cerebral cortex and basal ganglia. Trends Cogn Sci. 2013;17(5):241–54.
Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16(3):367–78.
Baillieux H, De Smet HJ, Dobbeleir A, Paquier PF, De Deyn PP, Mariën P. Cognitive and affective disturbances following focal cerebellar damage in adults: a neuropsychological and SPECT study. Cortex. 2010;46(7):869–79.
Manto M, Mariën P. Schmahmann’s syndrome—identification of the third cornerstone of clinical ataxiology. Cerebellum Ataxias. 2015;2(2):1–5.
Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121(4):561–79.
Tavano A, Grasso R, Gagliardi C, Triulzi F, Bresolin N, Fabbro F, et al. Disorders of cognitive and affective development in cerebellar malformations. Brain. 2007;130(10):2646–60.
Stoodley CJ, Schmahmann JD. Functional topography in the human cerebellum: a meta-analysis of neuroimaging studies. Neuroimage. 2009;44(2):489–501.
Van Overwalle, F, Baetens, K, Mariën, P, Vandekerckhove, M. Cerebellar areas dedicated to Social Cognition? A comparison of meta-analytic and connectivity results. Soc Neurosci 2015; 10(4):337-44.
Riedel MC, Ray KL, Dick AS, Sutherland MT, Hernandez Z, Fox PM, et al. Meta-analytic connectivity and behavioral parcellation of the human cerebellum. Neuroimage. 2015;117:327–42.
Turner BM, Paradiso S, Marvel CL, Pierson R, Boles Ponto LL, Hichwa RD, et al. The cerebellum and emotional experience. Neuropsychologia. 2007;45(6):1331–41.
Krienen FM, Buckner RL. Segregated fronto-cerebellar circuits revealed by intrinsic functional connectivity. Cereb Cortex. 2009;19(10):2485–97.
O'Reilly JX, Beckmann CF, Tomassini V, Ramnani N, Johansen-Berg H. Distinct and overlapping functional zones in the cerebellum defined by resting state functional connectivity. Cereb Cortex. 2010;20(4):953–65.
Buckner R, Krienen F, Castellanos A, Diaz JC, Yeo BT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:2322–45.
Andreasen NC, O'Leary DS, Cizadlo T, Arndt S, Rezai K, Ponto L, et al. Schizophrenia and cognitive dysmetria: a positron-emission tomography study of dysfunctional prefrontal-thalamic-cerebellar circuitry. Proc Natl Acad Sci. 1996;93(18):9985–90.
Crespo‐Facorro B, Wiser AK, Andreasen NC, O'Leary DS, Watkins GL, Boles Ponto LL, et al. Neural basis of novel and well‐learned recognition memory in schizophrenia: a positron emission tomography study. Hum Brain Mapp. 2001;12(4):219–31.
Walter H, Vasic N, Höse A, Spitzer M, Wolf RC. Working memory dysfunction in schizophrenia compared to healthy controls and patients with depression: evidence from event-related fMRI. Neuroimage. 2007;35(4):1551–61.
Müller JL, Röder C, Schuierer G, Klein HE. Subcortical overactivation in untreated schizophrenic patients: a functional magnetic resonance image finger‐tapping study. Psychiatry Clin Neurosci. 2002;56(1):77–84.
Volkow ND, Levy A, Brodie JD, Wolf AP, Cancro R, Van Gelder P, et al. Low cerebellar metabolism in medicated patients with chronic schizophrenia. Am J Psychiatry. 1992;149:686–8.
Liu H, Fan G, Xu K, Wang F. Changes in cerebellar functional connectivity and anatomical connectivity in schizophrenia: a combined resting‐state functional MRI and diffusion tensor imaging study. J Magn Reson Imaging. 2011;34(6):1430–8.
Friston KJ, Frith CD. Schizophrenia: a disconnection syndrome? Clin Neurosci. 1995;3(2):89–97.
Tran KD, Smutzer GS, Doty RL, Arnold SE. Reduced Purkinje cell size in the cerebellar vermis of elderly patients with schizophrenia. Am J Psychiatr. 1998;155(9):1288–90.
Okugawa G, Nobuhara K, Sugimoto T, Kinoshita T. Diffusion tensor imaging study of the middle cerebellar peduncles in patients with schizophrenia. Cerebellum. 2005;4(2):123–7.
Kyriakopoulos M, Vyas NS, Barker GJ, Chitnis XA, Frangou S. A diffusion tensor imaging study of white matter in early-onset schizophrenia. Biol Psychiatry. 2008;63(5):519–23.
Wassink TH, Andreasen NC, Nopoulos P, Flaum M. Cerebellar morphology as a predictor of symptom and psychosocial outcome in schizophrenia. Biol Psychiatry. 1999;45(1):41–8.
Pedersen A, Koelkebeck K, Brandt M, Wee M, Kueppers KA, Kugel H, et al. Theory of mind in patients with schizophrenia: is mentalizing delayed? Schizophr Res. 2012;137(1):224–9.
Lakis N, Jiménez JA, Mancini-Marïe A, Stip E, Lavoie ME, Mendrek A. Neural correlates of emotional recognition memory in schizophrenia: effects of valence and arousal. Psychiatry Res Neuroimaging. 2011;194(3):245–56.
Mendrek A, Jiménez J, Mancini-Marïe A, Fahim C, Stip E. Correlations between sadness-induced cerebral activations and schizophrenia symptoms: an fMRI study of sex differences. Eur Psychiatry. 2011;26(5):320–6.
Surguladze SA, Chu EM, Marshall N, Evans A, Anilkumar AP, Timehin C, et al. Emotion processing in schizophrenia: fMRI study of patients treated with risperidone long-acting injections or conventional depot medication. J Psychopharmacol. 2011;25(6):722–33.
Mendrek A, Mancini-Marië A, Fahim C, Stip E. Sex differences in the cerebral function associated with processing of aversive stimuli by schizophrenia patients. Aust N Z J Psychiatry. 2007;41(2):136–41.
Stip E, Fahim C, Liddle P, Mancini-Marïe A, Mensour B, Bentaleb LA, et al. Neural correlates of sad feelings in schizophrenia with and without blunted affect. Can J Psychiatr. 2005;50:909–17.
Brunet E, Sarfati Y, Hardy-Baylé M-C, Decety J. Abnormalities of brain function during a nonverbal theory of mind task in schizophrenia. Neuropsychologia. 2003;41(12):1574–82.
Mothersill O, Morris DW, Kelly S, Rose EJ, Bokde A, Reilly R, et al. Altered medial prefrontal activity during dynamic face processing in schizophrenia spectrum patients. Schizophr Res. 2014;157(1-3):225–30.
Andreasen NC, Calage CA, O'Leary DS. Theory of mind and schizophrenia: a positron emission tomography study of medication-free patients. Schizophr Bull. 2008;34(4):708–19.
Paradiso S, Andreasen NC, Crespo-Facorro B, O’Leary DS, Watkins GL, Ponto LLB, et al. Emotions in unmedicated patients with schizophrenia during evaluation with positron emission tomography. Am J Psychiatr. 2003;160(10):1775–83.
Crespo-Facorro B, Paradiso S, Andreasen NC, O'Leary DS, Watkins GL, Ponto LL, et al. Neural mechanisms of anhedonia in schizophrenia: a PET study of response to unpleasant and pleasant odors. JAMA. 2001;286(4):427–35.
Taylor SF, Phan KL, Britton JC, Liberzon I. Neural response to emotional salience in schizophrenia. Neuropsychopharmacol Off Publ Am College Neuropsychopharmacol. 2005;30(5):984–95.
Takahashi H, Koeda M, Oda K, Matsuda T, Matsushima E, Matsuura M, et al. An fMRI study of differential neural response to affective pictures in schizophrenia. Neuroimage. 2004;22(3):1247–54.
Fahim C, Stip E, Mancini-Marı̈e A, Beauregard M. Genes and memory: the neuroanatomical correlates of emotional memory in monozygotic twin discordant for schizophrenia. Brain Cogn. 2004;55(2):250–3.
Eickhoff SB, Stephan KE, Mohlberg H, Grefkes C, Fink GR, Amunts K, et al. A new SPM toolbox for combining probabilistic cytoarchitectonic maps and functional imaging data. Neuroimage. 2005;25(4):1325–35.
Eickhoff SB, Heim S, Zilles K, Amunts K. Testing anatomically specified hypotheses in functional imaging using cytoarchitectonic maps. Neuroimage. 2006;32(2):570–82.
Eickhoff SB, Paus T, Caspers S, Grosbras M-H, Evans AC, Zilles K, et al. Assignment of functional activations to probabilistic cytoarchitectonic areas revisited. Neuroimage. 2007;36(3):511–21.
Diedrichsen J, Balsters JH, Flavell J, Cussans E, Ramnani N. A probabilistic MR atlas of the human cerebellum. Neuroimage. 2009;46(1):39–46.
Eickhoff SB, Laird AR, Grefkes C, Wang LE, Zilles K, Fox PT. Coordinate‐based activation likelihood estimation meta‐analysis of neuroimaging data: a random‐effects approach based on empirical estimates of spatial uncertainty. Hum Brain Mapp. 2009;30(9):2907–26.
Turkeltaub PE, Eickhoff SB, Laird AR, Fox M, Wiener M, Fox P. Minimizing within‐experiment and within‐group effects in activation likelihood estimation meta‐analyses. Hum Brain Mapp. 2012;33(1):1–13.
Eickhoff SB, Bzdok D, Laird AR, Kurth F, Fox PT. Activation likelihood estimation revisited. Neuroimage. 2012;59(3):2349–61.
Laird AR, Fox M, Price CJ, Glahn DC, Uecker AM, Lancaster JL, et al. ALE meta‐analysis: controlling the false discovery rate and performing statistical contrasts. Hum Brain Mapp. 2005;25(1):155–64.
Andreasen NC, Pierson R. The role of the cerebellum in schizophrenia. Biol Psychiatry. 2008;64(2):81–8.
Demirtas-Tatlidede A, Freitas C, Cromer JR, Safar L, Ongur D, Stone WS, et al. Safety and proof of principle study of cerebellar vermal theta burst stimulation in refractory schizophrenia. Schizophr Res. 2010;124(1):91–100.
Stevens JS, Hamann S. Sex differences in brain activation to emotional stimuli: a meta-analysis of neuroimaging studies. Neuropsychologia. 2012;50(7):1578–93.
Singer T, Seymour B, O'Doherty J, Kaube H, Dolan RJ, Frith CD. Empathy for pain involves the affective but not sensory components of pain. Science. 2004;303(5661):1157–62.
Stephan KE, Friston KJ, Frith CD. Dysconnection in schizophrenia: from abnormal synaptic plasticity to failures of self-monitoring. Schizophr Bull. 2009;35(3):509–27.
Meyer-Lindenberg A, Poline JB, Kohn PD, Holt JL, Egan MF, Weinberger DR, et al. Evidence for abnormal cortical functional connectivity during working memory in schizophrenia. Am J Psychiatry. 2001;158(11):1809–17.
Meyer-Lindenberg AS, Olsen RK, Kohn PD, Brown T, Egan MF, Weinberger DR, et al. Regionally specific disturbance of dorsolateral prefrontal-hippocampal functional connectivity in schizophrenia. Arch Gen Psychiatry. 2005;62(4):379–86.
Lawrie SM, Buechel C, Whalley HC, Frith CD, Friston KJ, Johnstone EC. Reduced frontotemporal functional connectivity in schizophrenia associated with auditory hallucinations. Biol Psychiatry. 2002;51(12):1008–11.
Breakspear M, Terry JR, Friston KJ, Harris AW, Williams LM, Brown K, et al. A disturbance of nonlinear interdependence in scalp EEG of subjects with first episode schizophrenia. Neuroimage. 2003;20(1):466–78.
Das P, Kemp AH, Flynn G, Harris AW, Liddell BJ, Whitford TJ, et al. Functional disconnections in the direct and indirect amygdala pathways for fear processing in schizophrenia. Schizophr Res. 2007;90(1):284–94.
Acknowledgments
This work was supported by a Science Foundation Ireland Research Investigator project awarded to GD (SFI: 12.IP.1359).
Conflict of Interest
All authors have declared that there are no conflicts of interest in relation to the subject of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mothersill, O., Knee-Zaska, C. & Donohoe, G. Emotion and Theory of Mind in Schizophrenia—Investigating the Role of the Cerebellum. Cerebellum 15, 357–368 (2016). https://doi.org/10.1007/s12311-015-0696-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-015-0696-2