Abstract
Background
Numerous studies proved that all pedicle screw constructs produce the best outcome in the surgical treatment of patients with scoliosis. However, the optimal amount and distribution of screws has not yet been defined. In recent studies on idiopathic scoliosis, the correlation between curve correction and implant density has been discussed with diversifying results.
Purpose
The aim of this study was to detect a possible correlation of sagittal and coronal curve correction in dependence of metal load and flexibility index.
Materials and methods
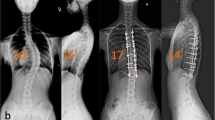
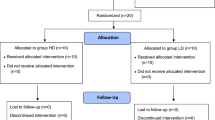
Twenty-six patients were included in this study with surgical correction by one surgeon between January 2014 and December 2017. Clinical data and radiographic images (preoperative, postoperative and one-year follow-up) were retrospectively analyzed and metal load, flexibility index, correction rate and correction index were consequently calculated. The Pearson correlation analysis was used for metal load—correction index and metal load—correction rate, correction of kyphosis—metal load and correction of lordosis—metal load. According to the mean metal load of 88%, patients were divided into two subgroups—a low-density group of 12 patients and a high-density group of 14 patients. Clinical and radiographic features were examined by an independent two-sided t-test.
Results
Eight patients were male, 18 patients female. Ten suffered from neuromuscular and 16 from idiopathic scoliosis. Mean age was 17.1 years. Correction rate directly postoperative was 70.43%, at the follow-up 67.90%. Mean correction index directly postoperative was 3.40 and at the follow-up 3.23. Pearson correlation of metal load—correction index directly postoperative was − 0.188 and one year postoperative − 0.189. The correlation between metal load—correction rate immediately after the surgery was 0.324 and at the follow-up 0.285. Correlation for correction of kyphosis—metal load postoperative was − 0.120 and one year later − 0.178. Pearson coefficient of lordosis—metal load directly after the surgical intervention was − 0.214 and at the follow-up − 0.220. Dependency of flexibility index and correction rate showed a positive trend (Pearson flexibility—correction rate direct 0.616; flexibility index—correction rate follow-up 0.516). A statistically significant difference between the high- and the low-density group was detected in the correction rate directly postoperative (p = 0.047).
Conclusion
With an implant density over 70%, satisfactory surgical treatment can be achieved in idiopathic and neuromuscular scoliosis. No statistical significance between the high-density (88–100%) and the low-density (73–87%) group could be verified in curve correction, ICU stay and complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The trend for the surgical treatment of patients with scoliosis changed from hook and wire constructions to all pedicle screw constructs over the last years.
The advantages of pedicle screws have been proven by multiple studies. The clinical and radiographic outcomes of pedicle screw constructs achieved better results than the correction by a hook/wire system since a better correction within a shorter fusion length can be obtained. Additionally, the previous anterior release for more flexibility can be averted in many cases. However, the disadvantages of pedicle screws are high financial costs, long duration of the surgery and the risk of neurological and vascular injuries [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18].
The dependency of a better correction on a higher pedicle screw density has been discussed in recent studies with diversifying results. Furthermore, the main part of the literature covers the treatment of idiopathic scoliosis. Therefore, the aim of this study was to include idiopathic and neuromuscular scoliosis and detect a possible correlation of curve correction in dependence of metal load and flexibility index. In addition, the correlation between sagittal curve correction and metal density as well as flexibility index and correction rate was investigated [1,2,3,4,5,6,7, 9,10,11,12,13,14,15,16,17,18].
Materials and methods
A total of 62 surgical scoliosis treatments in one institution between January 2014 and December 2017 were retrospectively analyzed. Every operation was performed by the same senior surgeon. Each patient had to perform a preoperative magnetic resonance imaging of the whole spine to exclude malformations of the medulla, e.g., a tethered cord. Before the surgery, standardized posterior-anterior, lateral and left- and right-bending radiographs were carried out. Postoperative imaging control (posterior-anterior and lateral whole spine) was performed one week and one year after the surgery. The Cobb-angle measurement for each radiographic image was performed by two examiners in order to minimize the measurement error. After applying the exclusion criteria, which are listed below, a total of 26 patients could be included in this study.
Exclusion criteria:
-
Congenital scoliosis
-
Previous spine surgery
-
Anterior spinal correction
-
Missing follow-up radiographs
-
Osteotomies (Smith-Peterson osteotomy, pedicle subtraction osteotomy, vertebral column resection)
The statistical analysis was performed for all 26 patients, and the calculated parameters were defined as follows:
-
Metal load (%): Number of implants per vertebra in the fusion segment/ (Number of included vertebra in the fusion segment × 2) [2, 3, 7, 9, 10, 12, 16]
-
Flexibility index (%): (Cobb-angle PA—Cobb bending on convex site) *100/Cobb-angle PA [2, 3, 5, 6, 9, 12]
-
Correction rate (%): (Cobb-angle PA preop—Cobb-angle PA postop) *100/Cobb-angle PA preop [2, 3, 6, 9, 12]
By calculating the correction index, the dependency of the flexibility on the correction rate was excluded. Sagittal correction was calculated for kyphosis (T5–T12) and lordosis (L1–L5). These measurements and calculations were performed individually for every curve in the scoliotic deformity directly postoperative and at the one-year follow-up. Additionally, the patients were divided into a high-density and a low-density group according to the mean metal load (88%) and consequently compared.
Surgical technique
All patients were operated by the same senior surgeon at a single institution with the same technique with neuromonitoring (SEP and MEP). Every patient was placed in a prone position under general anesthesia. Posterior midline incision was followed by a subperiosteal dissection of the muscles. Pedicle screws were placed in anatomic position under intraoperative imaging control. The amount of screws per vertebra was dependent on the anatomical conditions of the pedicle. The correction was performed by cantilever technique, derotation, translation, concave distraction and convex compression. Allograft bone was implanted after decortication for better posterolateral fusion.
Statistical analysis
All data are presented as mean ± standard deviation. Pearson correlation analysis (Lund, Sweden) was performed for the relationship between metal load and correction index, and metal load and correction rate. Correlation of the sagittal correction and implant density, flexibility index and curve correction directly after the surgery and at the follow-up was also depicted by Pearson coefficient. This calculation was also performed for the dependency of flexibility index and metal load. Sixteen patients had a double curve, 10 patients had only one structural curve. Double-curved scoliosis’ were divided into two curves and measured individually. The patients were divided into two groups according to the mean metal load. The features of these groups were investigated by an independent, two-sided t test. A p value < 0.05 was considered statistically significant.
Results
In summary, 26 patients, with a mean age of 17.1 ± 3.26 years, were included in this study. Eight patients were male and 18 female, 10 patients had a neuromuscular and 16 an idiopathic scoliosis. Mean flexibility index was 34.7 ± 20.19%. The correction rate directly postoperative was 70.43 ± 13.79%. At the follow-up one year later, the correction rate was 67.90 ± 13.96%. The mean correction index was 3.40 ± 4.81 directly postoperative and 3.23 ± 4.47 at the follow-up.
The Pearson correlation of metal load and correction index direct postoperatively measured − 0.188 (Fig. 1) and one year postoperative − 0.189 (Fig. 2).
The correlation between metal load and correction rate was 0.324 directly after the surgery (Fig. 3) and 0.285 at the follow-up (Fig. 4). The mean metal load was 88 ± 8%. Divided by the metal load, there was a low-density group (LD < 88%) and a high-density group (HD ≥ 88%).
Mean kyphosis was 39.93 ± 22.29° preoperatively, 30.68 ± 14.02° directly postoperative and 32.41 ± 15.31° at the one-year follow-up. The common angle of lordosis before the surgical correction was 42.28 ± 17.05°. Directly after the surgery, the mean lordosis was 41.73 ± 9.19° and one year later 39.50 ± 9.18°.
The average correction of the kyphosis directly postoperative was 8.65 ± 16.25° and 7.36 ± 18.42° at the follow-up.
Lordosis was corrected by a mean 1.00 ± 12.89° after the surgical intervention and 3.46 ± 13.60° one year later.
Pearson correlation for correction of kyphosis and metal load directly after the surgery was − 0.120 and − 0.178 at the follow-up. The correlation for lordosis and implant density immediately postoperative was − 0.213 and one year later − 0.220.
The Pearson correlation of flexibility index and correction rate directly after the surgery was 0.616 and 0.516 at the follow-up. Pearson coefficient for flexibility index and metal load was 0.238.
Low-density group
This group included 12 patients with a mean age of 17.3 ± 3.09 years. The ratio male:female was 3:9, seven patients had an idiopathic and five a neuromuscular scoliosis. The mean Cobb-angle of the preoperative posterior-anterior radiograph was 62.6 ± 16.89°, of the convex bending radiograph 43.83 ± 19.11° and the mean flexibility index was 29.76 ± 19.11%. The average metal load was 81 ± 3.85% with 13.58 ± 2.36 instrumentation levels and 22.17 ± 4.63 pedicle screws. The mean operation time was 365.08 ± 48.69 min with a mean blood loss of 1162.86 ± 849.82 ml. Postoperative patients averagely had to stay 3.58 ± 3.85 days in the ICU and 0.33 ± 0.47 patients had a complication. In total numbers, four patients developed a complication. Three suffered from postoperative pneumonia and one patient had a urinary tract infection. Data for blood loss were only available for seven patients in this subgroup.
Directly postoperative, the mean Cobb-angle was 22.5 ± 12.95° with a correction rate of 65.82 ± 14.65% and a correction index of 4.42 ± 6.51. At the one-year follow-up, the average Cobb-angle was 23.11 ± 13.49°, the correction rate was 64.93 ± 15.43% and correction index 4.26 ± 6.063.
Before the surgery, the mean kyphosis was 42.40 ± 25.88°. After the correction, the mean Cobb-angle amounted 31.98 ± 14.39° immediately after the surgery and 30.77 ± 15.74° one year later. In average, kyphosis was corrected 8.55 ± 19.24° right after the surgery and 9.80 ± 18.26° at the one-year follow-up.
Average lordosis preoperatively was 45.28 ± 16.52°. The correction in the low-density group was directly postoperative 45.26 ± 5.70° and at the follow-up 43.20 ± 7.13°. The amount of the lordosis adjustment immediately after the intervention depicted 0.40 ± 12.56° and one year after 2.51 ± 11.66°.
High-density group
The total number of patients in this group was 14; nine had an idiopathic and five a neuromuscular scoliosis. The ratio of male:female was 5:9, and the mean age was 16.9 ± 3.39. Preoperatively, the mean Cobb-angle was 66.3 ± 18.14°, the angle of the convex bending 45.93 ± 18.74° and the flexibility index was 40.13 ± 19.49%. The average instrumentation levels were 12.22 ± 3.09, with an average number of pedicle screws of 22.93 ± 5.89 and a mean metal load of 94 ± 5.08%. The mean operation time in minutes was 359 ± 90.21, the blood loss 670.83 ± 422.52 ml, the average ICU stay 4.21 ± 3.05 days and 0.29 ± 0.45 patients showed adverse events. Of the four complications detected in patients, three were due to pneumonia. One patient suffered from a haematothorax. In the CT scan, no screw misplacement was detected. The CT angiography showed no injury of a vessel, and the central venous catheter was in the right place. The patient did not need a thoracic drainage and no further intervention had to be performed. The amount of the perioperative blood loss in the high-density group was documented for twelve of the fourteen patients.
Immediately after the surgery, the mean Cobb-angle was 17.33 ± 10.82°, the correction rate was 75.04 ± 11.11% and the correction index 2.38 ± 1.28. One year after the surgery, the mean Cobb-angle was 20.28 ± 13.89°, the correction rate was 70.87 ± 11.59% and correction index was 2.20 ± 0.99.
The mean Cobb-angle of kyphosis preoperatively amounted 37.68 ± 18.11°, directly after the procedure 29.56 ± 13.61° and at the time of the follow-up 34.19 ± 14.61°. The correction depicted immediately postoperative 8.73 ± 12.90° and one year after the intervention 4.69 ± 12.22°.
Middle value for lordosis of the high-density group before the surgery was 39.53 ± 17.06°, right after the correction 38.47 ± 10.50° and at the follow-up 35.47 ± 9.47°. The average Cobb-angle of lordosis changed directly postoperative with an amount to 1.56 ± 13.16° right after the intervention and 4.51 ± 15.38° one year after.
Comparison between low- and high-density group
The only statistically significant difference between the high- and the low-density group was found in the correction rate directly postoperative (p = 0.047). At the one-year follow-up, no significant variance could be detected (p = 0.21).
There was no statistical significance in age (p = 0.76), preoperative Cobb-angle (p = 0.54), convex bending (p = 0.63), Flexibility index (p = 0.13), operation time (p = 0.84), blood loss (p = 0.22), length of ICU stay (p = 0.63) or complication rate (p = 0.80).
The postoperative Cobb-angle and correction index showed no significant distinction directly after the surgery or at the follow-up (Cobb-angle directly postoperative p = 0.22, at the follow-up p = 0.55; correction index directly postoperative p = 0.22, at the follow-up p = 0.18).
No statistically significance was detected between the high- and low-density group in kyphosis before the surgery (p = 0.64), directly postoperatively (p = 0.68) and at the one-year follow-up (p = 0.61).
Preoperative lordosis showed no statistical significance between the two groups of implant density (p = 0.44). Right after the intervention, the p value was 0.07 and one year later the t-test resulted in a p value of 0.05.
Discussion
There has been a variety of publications on pedicle screw constructs in the treatment of idiopathic scoliosis and the effect of implant density on curve correction [1,2,3,4,5,6,7,8,9,10,11,12, 14,15,16,17,18].
In the database search, only one article about the outcome of surgical treatment of thoracic scoliosis due to neurofibromatosis Type 1 could be found [13].
The results of all these studies are similar, regardless the type of scoliosis.
Therefore, the aim was to include all different types of idiopathic and neuromuscular scoliosis in order to examine the dependency of metal load on curve correction exclusive of the flexibility of the curve.
Similar to Quan and Gibson [6], we found no high correlation of the flexibility of the curve and implant density (0.248).
Li et al. [3] statet no statistically significance for dependency of curve flexibility and metal load. Altough more patients with flexible spine were distributed in the low-density group. Li et al. interpreted this finding by stating that surgeons tend to use less fixation points in more flexible scoliosis [3].
Pearson coefficient for flexibility index and correction rate immediately postoperative was 0.616 and at the follow-up one year later 0.516. This could be interpreted as a positive correlation like Quan and Gibson [6] depicted in their study. Mac-Thiong et al. [9] and Li et al. [3] in contrary found no dependency of curve flexibility with curve correction rate.
To eliminate the flexibility factor on the surgical correction, the correction index (correction ratio / flexibility index) was calculated for every curve by itself. When determining the Pearson correlation between the metal load and the correction index, slightly negative results were observed directly postoperative (− 0.188) and at the one-year follow-up (-0.189), indicating no correlation between these two parameters.
Metal load and correction rate showed a Pearson correlation of 0.324 directly after the surgery and 0.285 at the follow-up. This slightly positive trend could prove coherence among these parameters.
Pearson coefficient for sagittal correction and implant density showed neither directly postoperative nor at the follow-up a dependency (kyphosis—metal load directly postop − 0.120; kyphosis—metal load follow-up − 0.178; lordosis—metal load directly postop − 0.214; lordosis—metal load follow-up − 0.220).
The only statistical significance between low- and high-density group was detected in the directly postoperative correction rate (p = 0.047). At the follow-up one year later, no statistical significance was proven (p = 0.21). The flexibility index directly after the surgery and at follow-up was not significant for correction index.
It can be presumed that the better correction could be by virtue of the flexibility of the curve. There was no statistical significance of correction of kyphosis and lordosis in dependency of the density of the implants (kyphosis preop p = 0.64; kyphosis postop p = 0.68; kyphosis follow-up p = 0.61; lordosis preop p = 0.44; lordosis postop p = 0.07; lordosis follow-up p = 0.05).
When compared to the existing literature, this result is similar to the study outcome by Chen et al. [2]. In comparison with the one-year follow-up in our study, Clements et al. [10] were able to show a statistically significant correlation between implant density and curve correction two years after the surgery. Furthermore, Li et al. [13] also demonstrated a statistically significant better correction rate (p = 0.048) for the high-density group (> 1.35). The flexibility index was not calculated, but the difference between high- and low-density was statistically significant for correction loss at the last follow-up (two years postoperative). Quan et al. [6] proved a statistically significant correlation of curve flexibility with correction rate of the main thoracic curve (p = 0.05) but not for the absolute correction (p = 0.57).
On the contrary, Sariyilmaz et al. [12] (mean follow-up 41.21–44.61 months) stated no effect of high or low implant density on correction rate.
The mean metal load in our study was 88% with 1.76 pedicle screws per vertebra. Clements et al. [10] had a mean load of 60% and Sariyilmaz et al. [12] of 80%. The range of instrumentation per level in other studies was 0.6 [3], 0.77 [2], 0.8–1.69 [7], 1.31 [11], 1.32 [15], 1.35 [13], 1.6 [6], 1.61 [1], 1.2–1.7 [5] and 1.66 [16]. The lowest value of metal load in our study was 73%. This could be a reason for the low correlation between implant per vertebra with the correction rate and correction index.
Min et al. [8] stated that an implant density higher than 50% achieves satisfactory results and Mac-Thiong et al. [9] reported good corrections with implant density higher than 70%. Quan et al. [6] advised higher density for scoliosis curves with Cobb over 70°. None of our cases had a metal load under 70% because of the recommendations of present literature.
Surgeons should consider increasing forces on bone screw interface by overconstrained constructs with similar intervertebral forces [4, 5, 15]. High density is important in the apex of the curve for better EnBloc derotation, but in non-apical regions the metal load could be reduced [5, 10, 15].
With a curve flexibility higher than 50% and a Cobb smaller than 55°, there is no correlation between correction and density according to Le Naéaux et al. [16]. This was confirmed by Chen et al. [2] who stated an implant density of 50% is sufficient for a curve with a flexibility higher than 40%.
Li et al. [3] claimed no correction loss by reducing the implant density by more than 34%. We had high implant density in flexible and non-flexible curves with satisfactory results therefore we cannot suggest a smaller metal load than 73%.
Shen et al. [1], and Hwang et al. [17] stated a shorter operation time, less blood loss and lower implant costs by reducing implant density. In the present study, there was no significant difference in blood loss, ICU stay, operation time or complications. Pneumonia was the main cause for complications in patients (Table 1).
Initially our goal was to achieve a high metal density in every patient. Therefore, we tried to place a screw in every pedicle, even if the pedicle was very small and deformed. Sometimes we had to use several attempts for the correct placement, especially in the apex of a curve with a high Cobb-angle and a great rotation component.
If it was not possible to insert the screw in the correct way, we chose not to instrument it. An additional reason to remove a pedicle screw was too narrow space between the heads of each individual screw.
This could be the reason for the extended operation time 365.08 ± 48.69 (vs 359 ± 90.21) and the higher blood loss 1162.86 ± 849.82 (vs 670.83 ± 422.52) in the low-density group.
Barucha et al. [11] only had a significant difference in costs for low-density instrumentation but not in blood loss, length of stay, operation time, sagittal correction complications and SRS-22 outcome. Li et al. [13] also had no significant difference in blood loss, operation time and sagittal correction.
Sanders et al. [7, 14] proved a higher patient satisfaction after surgical correction of scoliosis (p = 0.047) but had no significant difference in SRS-22 outcomes in dependency of high- and low-density instrumentation.
Better sagittal correction through a higher implant density was stated by Le Navéaux et al. [15], Clements et al. [10] and Larson et al. [7]. On the contrary, Wang et al. [4] showed no statistically significant dependency of sagittal correction on higher implant density.
Quan et al. [6] reported a dependency of the sagittal on the coronal correction. We were not able to prove a significant dependency of the sagittal correction to the amount of the implant density.
The small number of cases and short follow-up period are some of the limitations of our study. For a more statistically significant statement about the restoration of the thoracic kyphosis due to surgical correction, the calculation should be performed individually for idiopathic and neuromuscular scoliosis. Due to our limited number of cases, the computation was invalid. Furthermore, implant costs were not surveyed. It was a common goal to achieve a high density in curve correction in scoliosis surgery [7]. For further studies, we intend to plan a metal density scarce higher than 70% on the base of X-rays before the surgery. This should result in a shorter surgery time and less blood loss.
The statistical analyzation of the amount of the perioperative blood loss of our study is furthermore only documented for nineteen patients. In future research, we aim to have a larger cohort and also intend to compare the blood loss in dependence of the application of tranexamic acid.
Conclusion
This study examined the radiological and clinical outcome in patients with idiopathic and neuromuscular scoliosis. With and without taking the flexibility of the curve into account, no correlation between curve correction and high or low implant density was detected. Every case had an implant density of over 70% with satisfactory postoperative curve correction. The only statistical significance was examined in the curve correction rate directly postoperative (p = 0.047) with high-density instrumentation, which could be due to the flexibility of the curve.
No statistically significant difference between high-density (88–100%) and low-density (73–87%) instrumentation was detected in the coronal curve correction index directly postoperative and at the follow-up, sagittal correction immediately and one year after the surgery, complications or the length of ICU stay. Therefore, an implant density of over 70% can be suggested as adequate operative treatment for idiopathic and neuromuscular scoliosis.
References
Shen M, Jiang H, Luo M, Wang W, Li N, Wang L, Xia L (2017) (2017) Comparison of low density and high density pedicle screw instrumentation in Lenke 1 adolescent idiopathic scoliosis. BMC Musculoskelet Disord 18:336. https://doi.org/10.1186/s12891-017-1695-x
Chen J, Yang C, Ran B, Wang Y, Wang C, Zhu X, Bai Y, Li M (2013) Correction of Lenke 5 adolescent idiopathic scoliosis using pedicle screw instrumentation. Spine 38(15):E946–E951. https://doi.org/10.1097/BRS.0b013e318297bfd4
Li Y, Yang C, Zhu X, Li M (2018) Analysis of correlation between regional implant density and the correction rate in treatment of Lenke 1A and 1B adolescent idiopathic scoliosis with pedicle screws. Medicine 97(2):e9488. https://doi.org/10.1097/MD.0000000000009488
Wang X, Aubin C-E, Robitaille I, Labelle H (2012) Biomechanical comparison of alternative densities of pedicle screws for the treatment of adolescent idiopathic scoliosis. Eur Spine J 21:1082–1090. https://doi.org/10.1007/s00586-011-2089-7
Delikaris A, Wang X, Boyer L, Larson AN, Ledonio CGT, Aubin C-E (2018) Implant density at the apex is more important than overall implant density for 3D correction in thoracic adolescent idiopathic scoliosis using rod derotation and en bloc vertebral derotation technique. Spine 43(11):E639–E647. https://doi.org/10.1097/BRS.0000000000002465
Quan GMY, Gibson MJ (2010) Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation. Spine 35(5):562–567
Larson AN, Aubin C-E, Polly DW, Ledonio CGT, Lonner BS, Shah SA, Richards BS, Erickson MA, Emans JB, Weinstein SL (2013) Are more screws better? a systematic review of anchor density and curve correction in adolescent idiopathic scoliosis. Spine Deform 1:237–247. https://doi.org/10.1016/j.jspd.2013.05.009
Min K, Sdzuy C, Farshad M (2013) Posterior correction of thoracic adolescent idiopathic scoliosis with pedicle screw instrumentation: results of 48 patients with minimal 10-year follow-up. Eur Spine J 22:345–354. https://doi.org/10.1007/s00586-012-2533-3
Mac-Thiong J-M, Ibrahim S, Parent S, Labelle H (2017) Defining the number and type of fixation anchors for optimal main curve correction in posterior surgery for adolescent idiopathic scoliosis. Spine J 17:663–670. https://doi.org/10.1016/j.spinee.2016.11.012
Clements DH, Betz RR, Newton PO, Rohmiller M, Marks MC, Bastrom T (2009) Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine 34(20):2147–2150
Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD (2013) Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J 13:375–381. https://doi.org/10.1016/j.spinee.2012.05.029
Sariyilmaz K, Ozkunt O, Karademir G, Gemalmaz HC, Dikici F, Domanic U (2018) Does pedicle screw density matter in Lenke type 5 adolescent idiopathic scoliosis? Medicine 97(2):e9581. https://doi.org/10.1097/MD.0000000000009581
Li Y, Yuan X, Sha S, Liu Z, Zhu W, Qiu Y, Wang B, Yu Y, Zhu Z (2017) Effect of higher implant density on curve correction in dystrophic thoracic scoliosis secondary to neurofibromatosis Type 1. J Neurosurg Pediatr 20:371–377. https://doi.org/10.3171/2017.4.PEDS171
Sanders JO, Diab M, Richards SB, Lenke LG, Johnston CE, Emans JB, Sucato DJ, Erickson MA, Bridwell KH, McCarthy RE, Sarwark JF, Dormans JP (2011) Spinal Deformity Study Group; (2011) Fixation points within the main thoracic curve. Spine 36(21):E1402–E1406. https://doi.org/10.1097/BRS.0b013e31822815ff
Le Navéaux F, Larson AN, Labelle H, Wang X, Aubin C-E (2016) How does implant distribution affect 3D correction and bone screw forced in thoracic adolescent idiopathic scoliosis spinal instrumentation. Clin Biomech 39:25–31. https://doi.org/10.1016/j.clinbiomech.2016.09.002
Le Navéaux F, Aubin CE, Larson AN, Polly DW, Baghdadi YMK, Labelle H (2015) Implant distribution in surgically instrumented Lenke 1 adolescent idiopathic scoliosis. Spine 40(7):462–468. https://doi.org/10.1097/BRS.0000000000000793
Hwang CH, Lee C-K, Chang B-S, Kim M-S, Yeom JS, Choi J-M (2011) Minimum 5 year follow-up results of skipped pedicle screw fixation for flexible idiopathic scoliosis. J Neurosurg Spine 15:146–150. https://doi.org/10.3171/2011.4.SPINE10321
Suk SI, Lee S-M, Chung E-R, Kim J-H, Kim S-S (2005) Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 30(14):1602–1609
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wolfram, J.M., Kristen, V.A., Cip, J. et al. Influence of implant density and flexibility index on curve correction after scoliosis surgery. Musculoskelet Surg 106, 317–323 (2022). https://doi.org/10.1007/s12306-021-00707-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-021-00707-w