Abstract
Purpose
Today, in rotator cuff tear repair, the transosseous sutures are considered superior from a biological and biomechanical point of view. Our purpose is to present the early clinical and biomechanical data of a new arthroscopic rotator cuff tear transosseous repair system: the Sharc-FT®.
Materials and methods
A total of 34 patients with rotator cuff tear affecting supraspinatus and infraspinatus, 1 to 3 cm wide, were treated and evaluated from 2010 to 2013. The average age was 63.2 years. Mean follow-up was 18.6 months. All patients were assessed through Constant score in the preoperative step and at 3-, 6-, and 12-month follow-up, performing an MRI 6 months after surgery.
Results
The patients have shown a mean preoperative Constant score of 24.5 pt that constantly increases after surgery, until a mean value of 86.9 at 12 months. Regarding complications two cases of adhesive capsulitis were recorded.
Conclusions
This device permits to obtain transosseous sutures with cortical fixation; to greatly reduce the problems of lack of bone resistance; to decrease motion at tendon–footprint interface improving fatigue resistance; to make the stress–load distribution homogeneous at the footprint, thus optimizing biological healing. A later evaluation will be necessary, especially for the incidence of retears.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past 40 years, rotator cuff tear repair techniques have undergone a remarkable evolution, permitting a gradually improved tendon to bone fixation. In 1944, McLaughlin [1] was the first to describe a transosseous rotator cuff tear repair that has represented the gold standard of the types of repair of these lesions, open or mini-open.
The advent of the arthroscopy technique has revolutionized the approach to this kind of surgery; in the last years, we have attended to the appearance of many devices of fixation: screwed or beaten anchors, made of materials like titanium, peek or reabsorbable ones. The repair techniques also evolved from single row to double row [2–5], until the development of transosseous-equivalent configurations like the suture bridge technique, to obtain a better tendon compression to the footprint interface optimizing contact area and pressure, as well as pullout strength and less interface motion [6, 7].
These surgical repair techniques have become of common use in arthroscopic approach, but the rate of pull out with poor bone stock is still high [8], as well as the rate of failure at tendon level, so the problem of rotator cuff retears is still not completely solved [9]. To improve outcomes after repair, healing biology at the footprint interface must be advanced.
The transosseous repair fixation system represents today the most reliable surgical technique from the biological and mechanical point of view, even if it still needs to be improved.
The purpose of our analysis is to present the early clinical and biomechanical data of a new arthroscopic rotator cuff tear transosseous repair system: the Sharc-FT®.
Methods
From September 2010 to January 2013, 67 patients (31 male–36 female) were treated with an average age of 63.2 years (range 41–75) and a rotator cuff tear that affected supraspinatus and infraspinatus tendons, 1 to 3 cm wide, by MRI evaluation.
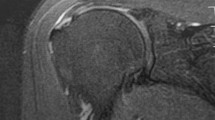
All patients were assessed with the constant score (0–100 points) in the preoperative phase and at 3-, 6-, 12-months follow-up. Six months after surgery, patients underwent a MRI for healing evaluation. We have completely evaluated 34 patients with a mean follow-up of 18.6 months (range 12.4–22.3).
The operative technique consisted of one Sharc-FT® device with its relative three sutures. A couple of the adopted configurations are sketched in the picture below reported (Fig. 1).
To minimize variability, all patients were treated by the same two surgeon (P. B., E. R. D.).
After surgery, the upper limb was immobilized in a 20° abduction sling for 30 days, passive physiotherapy was started after 10 days, while active physiotherapy after 3 weeks.
Surgical technique
The Sharc-FT® was developed in collaboration with NCS-LAB of Carpi (Modena, Italy) (Fig. 2).
This device is characterized by its placement, in a region with a good bone quality, located about 15–20 mm distally to the great tuberosity; management of two to four inner sutures to achieve a medial row in the footprint that can be developed also within lateral sutures in traction or compression configuration, so the possibility to perform a wide and personalized range of repairs with internal and external sutures; and its shape, created to maximize the resistance to pull out effect and to prevent suture–bone interaction. Its in vivo use was preceded by laboratory biomechanical tests in repaired rotator cuff tear created on young fresh frozen bovine humeri. To simulate the tears an artificial 35 × 10 mm defect of thickness was performed at the supraspinatus tendon insertion after removing other tendons. This tendon lesion was repaired to its physiological footprint using four simple half stitched polyethylene sutures tied with the same force and the Sharc-FT® suture platform.
Two tests were developed: the loading cyclic test and failure test by a multi-actuator Italsigma IT08-074. In both, the device has shown good results in comparison with the data measured with other repair techniques using anchors with different suture configurations.
The Sharc-FT® application needs specific surgical instrumentations that allow guided and repeatable procedure saving operative time: the special compass (Fig. 3) permits easy passage of the shuttle transosseous sutures and the implant carrier assures a beating insertion of the Sharc-FT®, overcoming the traditional difficulties related to the transosseous arthroscopic suture repair procedures.
Patients were positioned in lateral decubitus with the operated upper limb in traction, under general anesthesia.
After tendon preparation for suture, the surgeon proceeded with the footprint preparation creating a heavy surface decortication with an extension of several millimeters with a bonecutter. Then the Sharc-FT® system instrumentations could be applied: first, the proximal 3 mm Ø hole on the footprint was made; and second, the guide compass could be assembled and set to perform the distal lateral 3 mm Ø hole 3 cm from the greater tuberosity edge. The shuttle wire could then be passed through the transosseous tunnel with the compass, so it could drag the suture wires connected to the front part of the Sharc-FT® up to obtain the back surface of the device in contact with the cortical bone (Fig. 4).
To conclude the rotator cuff tear was sutured.
Results
The 34 operated and completely evaluated patients with a mean follow-up of 18.6 months (range 12.4–22.3) showed a mean constant score before surgery of 24.5 pt (min 16.4–max 68.1). Three months after surgery, the mean value was 63.1 pt (min 43.6–max 82.0); at 6 months 83.2 pt (min 47.0–max 89.5); finally, at 12 months 86.9 pt (min 47.5–max 90.4) (Table 1).
At 6 months, all patients had undergone an MRI for rotator cuff and surgical repair evaluation: there was no device mobilization nor rotator cuff retear.
There were no other outstanding complications, except for two cases of adhesive capsulitis treated with prolonged rehabilitation.
Discussion
The rotator cuff tear represents one of the most frequent musculoskeletal lesions. In spite of numerous technological innovations, retears are still complications with extremely variable rate (Galatz et al. JBJS 2004) [10].
The first transosseous repair technique was developed by McLaughlin in 1944 [1]; since then, technological improvements, in particular with the coming of arthroscopy, have produced a very high possibility of repairing these lesions [11–13].
In rotator cuff tear repair procedures, anchors are the most commonly used devices, which can be screwed or beaten, of various kinds of materials, with 2 or 3 sutures, and permit several repair configurations (single row, double rows, suture bridge having multiple sutures configurations).
However, possible failure induced the development of other types of sutures over the years, until the production of anchors that can allow a transosseous-equivalent repair technique [14]. The problems related to the migration and pullout of these devices, especially in patients with a poor bone stock, still represent the principle complications nowadays.
Today, the transosseous suture is considered superior in rotator cuff tear repair from a biological and biomechanical point of view [12, 13, 15]. In fact, it allows reduction of the tendon–bone gap formation, taking into consideration that a displacement of 3 mm is considered a repair failure [16]; it increases blood contribution through the tunnel, maximizing the healing potential; it enhances the contact area between footprint and the repaired tendon; it reduces stress at the repaired tendon–bone interface; and it avoids the presence of hardware on the footprint.
A recognized concern is represented by the cortical cut that can occasionally, when poor bone stock is present, modify the tunnel geometry leading to an unwanted early gap formation between tendon and footprint.
The development of an arthroscopic transosseous suture system has undergone some basic biomechanical evaluations. In the estimation of maximum load to failure, no differences between repair with anchors or with the transosseous system can be shown [17, 18]. Tocci et al’s study [19] on fatigue resistance demonstrated, in high stress load, a bigger gap between tendon and bone in the repair with anchors, while in low stress load, no differences between the two systems were shown.
In anchor repair, the failure occurs at tendon level, whereas in the transosseous one in the tunnel [20, 21]. The footprint coverage has appeared greater in the transosseous technique [22–24], such as the bone–tendon interface stability [22]. The stress load is distributed much more in the bone tunnel of the transosseous repair, whereas in anchor repair, the stress load is charged to tendon and device insertion points, increasing the retear rate [25]. In addition, the pressure is homogenously delivered in transosseous sutures unlike the anchor repair, where elevated values recorded in tendon–bone interface have increased the risk of ischemic damage to tendon tissue [24].
From these biomechanical assumptions, a transosseous suture system was developed which allows conjugation of the validity of this type of repair technique with the advantages of arthroscopy: the Sharc-FT®. This device permits to obtain arthroscopic transosseous sutures with cortical fixation; to create a traction-compression lateral suture inside the footprint prepared purposely; to greatly reduce the problems of poor bone resistance; to decrease motion at tendon–footprint interface improving fatigue resistance; finally, to make the stress–load distribution at the footprint homogeneous, optimizing biological healing.
Our initial clinical experience has obtained encouraging results. In our study, we have taken into consideration the same type of rotator cuff tear affecting supraspinatus and infraspinatus, 1 to 3 cm wide: 6 months after the surgical operation, MRI examination highlighted a very good biological tendon healing without retears. Constant score values were satisfactory, except in one case, probably due to an error of surgical indication.
We did not have complications in short and long term, except for two cases of adhesive capsulitis; we noted an initial increase in surgical time compared with the anchor technique due to the learning curve in the compass use.
Nevertheless, this study shows some limitations: it is retrospective, the follow-up is still very short and the system needs to be tested in much wider rotator cuff tears.
A later evaluation will be necessary, especially for the incidence of retears.
Conclusions
The improvement of suture technique in rotator cuff tears has permitted a considerable increase in the possibility of a successful treatment of this pathology; nevertheless, the complication of relapses remains. From the point of view of technological evolution, a new system of arthroscopic transosseous suture has been created. This first clinical experience confirms the efficacy of this system which could have a very interesting evolutionary application.
These early clinical results are consistent with the relevant cyclic and static (ultimate tensile load) results measured in a biomechanical test set up [26] confirming that the measured mechanical primary stability could be, as reported in several previous papers, at the basis of the good clinical outcome.
References
McLaughlin HL (1944) Lesions of the musculotendinous cuff of the shoulder. The exposure and treatment of tears with retraction. Clin Orthop Relat Res 304:3–9
Charousset C, Grimberg J, Duranthon LD et al (2007) Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair?: a prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med 35(8):1247–1253
Park JY, Lhee SH, Choi JH et al (2008) Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med 36(7):1310–1316
Burks RT, Crim J, Brown N et al (2009) A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med 37(4):674–682
Dines JS, Bedi A, ElAttrache NS et al (2010) Single-row versus Double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg 18:83–93
Park MC, Elattrache NS, Ahmad CS et al (2006) Transosseous-equivalent rotator cuff repair technique. Arthroscopy 22(12):e1361–e1365
Park MC, Tibone JE, Elattrache NS et al (2007) Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg 16(4):469–476, 17321158
Kannus P, Leppala J, Lehto M et al (1995) A rotator cuff rupture produces permanent osteoporosis in the affected extremity, but not in those with whom shoulder function has returned to normal. J Bone Miner Res 10(8):1263–1271
Benson EC, MacDermid JC, Drosdowech DS et al (2010) The incidence of early metallic suture anchor pullout after arthroscopic rotator cuff repair. Arthroscopy 26(3):310–315
Galatz LM, Ball CM, Teefey SA et al (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-A(2):219–224
Burkhart S, Lo IK (2006) Arthroscopic rotator cuff repair. J Am Acad Orthop Surg 14(6):333–346
Chiaracane G, Aglietti P, De Biase P et al (2001) Lesioni della cuffia dei rotatori. Analisi dei risultati dopo trattamento chirurgico. GIOT 27:13–19
Kim KC, Rhee KJ, Shin HD et al (2008) Arthroscopic transosseous rotator cuff repair. Orthopaedics 31(4):327–330
Frank JB, ElAttrache NS, Dines JS et al (2008) Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med 36(8):1496–1503
Kang L, Henn RF, Tashjian RZ et al (2007) Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy 23(6):573–582
Porcellini G, Campi F, Paladini P et al (2008) Il trattamento artroscopico della cuffia dei rotatori. Lo Scalpello 22(1):36–41
Craft DV, Moseley JB, Cawley PW et al (1996) Fixation strength of rotator cuff repair swith suture anchors and the transosseous suture technique. J Shoulder Elbow Surg 5(1):32–40
Burkhead WZ Jr, Skedros JG, O’Rourke PJ et al (2007) A novel double-row rotator cuff repair exceeds strengths of conventional repairs. Clin Orthop Relat Res 461:106–113
Tocci SL, Tashjian RZ, Leventhal E et al (2008) Biomechanical comparison of single-row arthroscopic rotator cuff repair technique versus transosseous repair technique. J Shoulder Elbow Surg 17(5):808–814
Burkhart SS, Johnson TC, Wirth MA et al (1997) Cyclic loading of transosseous rotator cuff repairs: tension overload as a possible cause of failure. Arthroscopy 13(2):172–176
Goradia VK, Mullen DJ, Boucher HR et al (2001) Cyclic loading of rotator cuff repairs: a comparison of bioabsorbable tacks with metal suture anchors and transosseous sutures. Arthroscopy 17:360–364
Ahmad CS, Stewart AM, Izquierdo R et al (2005) Tendon bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med 33(11):1667–1671
Apreleva M, Ozbaydar M, Fitzgibbons PG et al (2002) Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy 18(5):519–526
Tuoheti Y, Itoi E, Yamamoto M et al (2005) Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med 33(12):1869–1874
Sano H, Yamashita T, Wakabayashi I et al (2007) Stress distribution in the supraspinatus tendon after tendon repair: suture anchors versus transosseous suture fixation. Am J Sports Med 35(4):542–546
Mahar A, Tamborlane J, Oka R et al (2007) Single-row suture anchor repair of the rotator cuff is biomechanically equivalent to double-row repair in a bovine model. Arthrosc: J Arthrosc Relat Surg 23(12):1265–1270
Conflict of interest
We certify that there is no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baudi, P., Rasia Dani, E., Campochiaro, G. et al. The rotator cuff tear repair with a new arthroscopic transosseous system: the Sharc-FT® . Musculoskelet Surg 97 (Suppl 1), 57–61 (2013). https://doi.org/10.1007/s12306-013-0254-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-013-0254-3