Abstract
Lack of cardiometabolic profile data based on severity of opiate dependence for opiate abusers. The study aimed to evaluate the effect severity of opiate abuse on the cardiometabolic profile of male opiate abusers without co-morbidities. The study included 30 healthy controls (HCs), 90 prospective chronic opiate (opium and heroin) abusers, with and without co-dependence of smoking and tobacco-chewing. The subjects were categorized based on severity of opiate dependence questionnaire (SODQ) and metabolic syndrome (MS) based on NCEP ATP-III criteria and fasting blood samples analyzed for sugar, insulin, insulin resistance (IR), lipid profile, Hs-CRP and total antioxidant capacity (TAC). There was higher prevalence of MS in opiate abusers as compared to HCs. Majority of the patients fell in grade 2 and 3 of severity. There was significant difference across groups for WHR (p < 0.001), SBP (p < 0.03), FBS (p < 0.001), insulin (p < 0.02), IR (p < 0.03) and TAC (p < 0.01). Multiple regression analysis of SODQ grades 2 and 3 independently predicted TAC by Hs-CRP (p = 0.032 and 0.042). There was a significant correlation of TAC with serum insulin, IR and Hs-CRP in SODQ grade 2 and serum insulin and Hs-CRP in SODQ grade 3. Chronic opiate abuse is not benign and predisposes abusers to cardiometabolic risk with increasing severity of dependence, owing to oxidative stress and chronic low-grade inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Habitual use of opium has been documented in Indians since nineteenth century, but little attention has been paid to the chronic opiate abuse which is rampant now in many parts of the country. Opiate abuse is an important cause of premature mortality and morbidity among adults. Besides its socio-economic effects, its triggering role on disabling disorders such as cardiovascular disorders also has been suggested [1]. There is a traditional belief of opiate use having protective effects against cardiovascular disease (CVDs) and diabetes mellitus (DM). However, the reports of higher risk of coronary artery disease (CAD) among opium abusers as compared to the non-opium users suggests the opposite [2]. The data on traditional risk factor for cardiovascular risk-serum lipid profile is inconsistent in opium abusers. Some clinical studies have shown that opium might be associated with alterations in the levels of total cholesterol, triglycerides, LDLc and HDLc, [3,4,5] whereas others have shown no significant difference in these parameters between individuals who are addicted and those who are not addicted to opium [6]. But standardized mortality ratios for CAD have been higher in opioid addicts as compared to general population. Although opioids have the protective effects on heart and play an important treatment role during ischemic event, the chronic usage of opioid may complicate influence of opioids, particularly when the consumption ways are different like inhalation [7]. Further, it have been shown that exogenous opioids tend to suppress the immune system and this negative modulation of immune cells depends on the opioid, its dose and the route of administration, possibly leading to low grade inflammation [8].
The effect of chronic abuse of heroin has been shown to cause oxidative stress in animal models, as well as in human studies [9]. Thus chronic opiate abuse may increase the hallmarks of cardiometabolic risk factors like dyslipidemia, inflammation and oxidative stress. However, there is a lack of data on the cardiometabolic profile of chronic opiate abusers form India, and a gap in the knowledge about the effect severity of opiate dependence on cardiometabolic profile. In the present study we aim to study the effect of chronic opiate abuse on the markers of cardio-metabolic syndrome based on the severity of opiate abuse. Prevalence of cardiometabolic syndrome/metabolic syndrome was evaluated using NCEP ATP-III criteria [10].
Methods
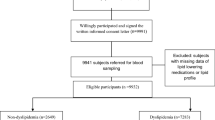
In this hospital based, cross-sectional study 90 chronic opiate abusers (with or without associated smoking and non-smoking tobacco abuse) and 30 age matched controls were included. The study participants were categorized into four groups (I—healthy controls; II—pure opiate abusers; II—opiate and tobacco chewers; III—opiate and smokers). The opiate abusers were recruited prospectively from the de-addiction clinic of a tertiary care center in western India for a duration of 1 year i.e. from March 2015 to March 2016. The control group was recruited from the attendants of the substance abuse patients, who were having no complains of organic or functional diseases and who were not on any medication at the time of evaluation. The family history of the control subjects was taken and those with family history of cardiovascular disorders were excluded. An informed consent of the study protocol as approved by the institutional ethics committee was taken by all the participants prior to inclusion in the study.
Experimental
Inclusion Criteria
The study group from substance abuse were dependent on opiates (including pure opium, opium husk, and heroin) and or smoking and non-smoking tobacco. The study did not take into account the exact amount of opiate consumed, but a minimum of 100 mg/day consumption was a criteria for selection of the subjects.
Exclusion Criteria
Exclusion criteria for the substance abuse persons were—age > 50 years, multiple substance abuse, diagnosed diabetics, hypertensive, CAD, patients taking rifampicin, ranitidine, nifedipene, levothyroxine to avoid cross reaction with urinary opiates analysis. The opiate abusers should have fulfilled the criteria of 100 mg/day opiate consumption for a minimum of 1 year abuse and dependence as per ICD 10 classification 1992 [11]. All opiate dependent patients should not have abstained for more than 24 h and the urine samples were analyzed for screening urinary opiate levels and those negative were excluded.
Anthropometric measurements of individuals wearing light clothing and no shoes were carried out. Weight was measured to the nearest 0.1 kg, and height was measured to the nearest 1 cm. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Waist circumference (cm) was measured at the level of the iliac crest at the end of normal expiration. Waist circumference was measured to the nearest 0.5 cm. The subjects were screened for components of MS using modified ATP III criteria. Blood pressure was measured at rest in supine position three times and a mean was recorded. Biochemical analysis of fasting serum samples was performed on Beckman and Coulter AU 480 using the chemistry kits of Randox. The biochemical parameters analysed included fasting blood sugar (FBS; hexokinase method), lipid profile, serum insulin (chemileuminiscence assay). IR in the participants was evaluated according to the homeostasis model assessment-insulin resistance (HOMA-IR) protocol [12]. Severity of opiate dependence was evaluated based on SODQ [13].
The study data was analyzed using SPSS 21 (Chicago, USA) software. The categorical data was expressed as mean and standard deviation. The difference between the groups was analyzed using one way analysis of variance (ANOVA), frequencies were used to determine the components of MS in different groups. Multiple linear regression was used to study the effect of independent variables on cardiometabolic risk factors.
Results
Most of the study participants were in the grade 3 of severity of opiate dependence and a large chunk of these belonged to the farming community, skilled workers (carpenters, goldsmiths, barbers, etc.) semi-skilled workers (masonry workers, labourers, etc.; Fig. 1). The prevalence of MS by the NCEP ATP III criteria was highest in opiate + smoke free tobacco users (43.3%), followed by opiate + smoking tobacco (33.33%), then pure opiate abusers (26.7%) and least in HCs (16.7%). One way ANOVA showed a significant difference across groups for BMI, WHR, TCH, TG, Hs-CRP and TAC (Table 1). Further multiple linear regression analysis conducted for pure opium abusers with opium dependency as dependent variable, showed dependency years were predicted independently by SBP, insulin, IR and advancing age (Tables 2) and Pearson’s correlation analysis showed dependency to be significantly associated with HsCRP (Table 3). A multiple linear regression in SODQ grades 2 and 3 showed that TAC was independently predicted by Hs-CRP (p = 0.032; p = 0.042) respectively (Tables 4, 5). Pearson’s correlation analysis showed a significant association of TAC with serum insulin, IR and Hs-CRP in SODQ grade 2 and serum insulin and Hs-CRP in SODQ grade 3 (Tables 6, 7).
Discussion
The present study is the first of its kind in male, chronic opiate abusers with no associated co-morbidity. We observed that the cardio-metabolic profile of these subjects deteriorates with increasing severity of dependence due to increased oxidative stress and low grade chronic inflammation. The one way ANOVA showed significant difference between the groups (p = 0.001) and group II subjects had higher BMI and WHR as compared to the controls and opiate with co-dependence of tobacco (smoke and smokeless; Table 1). This probably is due to higher preferences for sweet and fatty foods as reported by Davis et al. [14] due to genotypic differences in the regulation of mu opioid receptors. Evidence from preclinical animal studies suggest that direct action of mu agonists at the nucleus accumbens shell, hypothalamus, and paraventricular nucleus is associated with development of sweet preference. Similarly, clinical literature demonstrates that chronic exposure to mu-opiate agonists leads to heightened taste preference for high-sugar foods [15]. The preference for sugary foods resulting from opiate administration may lead to increased consumption of such foods, and possibly accumulation of excess body fat and weight gain. Current study also observed a significant difference (p < 0.0001) in the FBS levels of the study groups in one way ANOVA, with highest FBS observed in the opiate + tobacco chewer group (Table 1). The increase in the FBS was linked with a significant increase in fasting insulin in the opiate abusers as compared to HCs (Table 1). Similar observations were made by Gozashti et al. [16] however they reported lower fasting insulin.
The relationship between the substance abuse and MS is complex with scarce literature. There is an increased risk of MS and diabetes in people with substance abuse and most studies have been performed in alcoholics and nicotine dependence. A study from northern India reports 29.3% prevalence of MS in opiate dependence and included subjects with opiate dependence along with tobacco and smoking co-dependence [17]. However, current study reports for the first time opiate in combination with tobacco and smoking groups independently and observed significant difference in the FBS of these three groups, with highest in opiate with smoking (Table 1). The prevalence of MS in the current study was detected using ATP III criteria with highest recorded in opiate with tobacco chewer, followed by opiate with smoking, then pure opiate group and least in HCs. The higher prevalence of MS in both opiate with (tobacco chewers or tobacco smokers) may be due to enhance inflammation as reported in earlier studies [18,19,20,21]. Further significantly higher serum insulin levels were observed in the opiate abusers as compared to the control group. This is in congruence with the observations that administration of naloxone (opioid antagonist) in obese subjects inhibited the responses of insulin and C-peptide to glucose administration and therefore possibly endogenous β-endorphins increase the responsiveness of pancreatic β cells. This may suggest that exogenous opioid administration may contribute to hyperinsulinemia [22].
Oxidative stress has been recently reported as key mechanism of developing IR [23]. Opioid drugs also adversely affect the activity of antioxidant systems, as observed by decrease in the TAC in the blood of human heroin addicts when compared to the control groups [24]. In experimental mice exposed to heroin, there was a decrease in the activity of antioxidant enzymes in the brain such as superoxide dismutase (SOD), catalase and glutathione peroxidase (GPx) and administration of antioxidants alleviated the oxidative stress [25]. Multiple linear regression analysis of opiate abusers with MS showed that low grade chronic inflammation was predicted by increasing adiposity, BP, insulin, HOMA-IR, TC, HDL and LDL [26]. Inflammation is recognized as a major etiologic determinant of multiple disease states including myocardial infarction, stroke, diabetes, MS and individuals with elevated levels of the inflammatory biomarkers such as Hs-CRP are at increased risk of mortality and morbidity from these conditions [27]. The current study also showed that oxidative stress significantly differed in the opiate abusers and was highest in group IV. This shows that opiate abuse along with smokeless tobacco dependence caused maximum oxidative stress. On adjusting for age, dependence years and basic biochemical profile, oxidative stress was independently predicted by the BMI and the serum insulin level of the opiate abusers. Further the correlation analysis of TAC showed that oxidative stress was negatively, significantly associated with dependence years, FBS, insulin and HOMA-IR. There are reports of heroin dependence being associated with increased IR in hepatitis C virus seronegative heroin abusers. Prolonged heroin abuse has been reported as associated with reduction of basal β-cell pancreatic function with decreased IR controlled for waist circumference, but still inducing significantly decreased basal insulin sensitivity [28].
Conclusion
We conclude that chronic opiate abuse is not benign for male abusers and there should be public awareness regarding the harmful effects of opiate abuse. Such subjects are a unique group with significant low grade inflammation and oxidative stress that drives for insulin resistance, even in the absence of co-morbidities like diabetes or hypertension. The consumption of opiates with smoking further adds to this risk. We recommend screening of opiate abuse patients for routine cardiometabolic profile.
References
Masoomi M, Ramezani MA, Shahriari S, Shahesmaeeli A, Mirzaeepour F. Is opium addiction a risk factor for deep vein thrombosis? A case–control study. Blood Coagul Fibrinolysis. 2010;21:109–12.
Roohafza HR, Talaei M, Sadeghi M, Haghani P, Shokouh P, Sarrafzadegan N. Opium decreases the age at myocardial infarction and sudden cardiac death: a long- and short-term outcome evaluation. Arch Iran Med. 2013;16(3):154–60.
Davoodi G, Sadeghian S, Akhondzadeh S, Darvish S, Alidoosti M, Amirzadegan A. Comparison of specifications, short-term outcome and prognosis of acute myocardial infarction in opium dependent patients and non-dependents. Ger J Psychiatry. 2005;8:33–7.
Azod L, Rashidi M, Afkhami-Ardekani M, Kiani G, Khoshkam F. Effect of opium addiction on diabetes. Am J Drug Alcohol Abuse. 2008;34:383–8.
Mami S, Eghbali M, Cheraghi J, Mami F, Broujeni MP, Salati AP. Effect of opium addiction on some serum parameters in rabbit. Glob Vet. 2011;7:310–4.
Najafi M, Sheikhvatan M. Plausible impact of dietary habits on reduced blood sugar in diabetic opium addicts with coronary artery disease. Iran Cardiovasc Res J. 2012;6:75–8.
Asgary S, Sarrafzadegan N, Naderi G, Rozbehani R. Effect of opium addiction on new and traditional cardiovascular risk factors: do duration of addiction and route of administration matter? Lipids Health Dis. 2008;7:42.
Olson GA, Olson RD, Kastin AJ. Endogenous opiates. Peptides. 1996;17(8):1421–66.
Abu Bakar NH, Hashim SN, Mohamad N, Husain R, Mohd Adnan LH, Shariff H, et al. Role of oxidative stress in opiate withdrawal and dependence: exploring the potential use of honey. J Appl Pharm Sci. 2015;5(12):159–61.
Grundy SM, Cleema JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735–52.
World Health Organization. The ICD-10 classification of mental and behavioural disorders—clinical descriptions and diagnostic guidelines. Geneva: WHO; 1992.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Phillips GT, Gossop MR, Edwards G, Sutherland G, Taylor C, Strang J. The application of the SODQ to the measurement of the severity of opiate dependence in a British sample—severity of alcohol dependence questionnaire. Br J Addict. 1987;82(6):691–9.
Davis C, Zai C, Levitan RD, Kaplan AS, Carter JC, Reid-Westoby C, et al. Opiates, overeating and obesity: a psychogenetic analysis. Int J Obes (Lond). 2011;35(10):1347–54.
Dum J, Gramsch CH, Herz A. Activation of hypothalamic B-endorphin pools by reward induced by highly palatable food. Pharmacol Biochem Behav. 1983;18:443–7.
Gozashti MH, Yazdi F, Salajegheh P, Dehesh MM, Divsalar K. Fasting blood glucose and insulin level in opium addict versus non-addict individuals. Addict Health. 2015;7(1–2):54–9.
Mattoo SK, Chakraborty K, Basu D, Ghosh A, Vijaya Kumar KG, Kulhara P. Prevalence & correlates of metabolic syndrome in alcohol & opioid dependent inpatients. Indian J Med Res. 2011;134:341–8.
Dwivedi S, Goel A, Khattri S, Mandhani A, Sharma P, Pant KK. Tobacco exposure by various modes may alter pro-inflammatory (IL-12) and anti-inflammatory (IL-10) levels and affects the survival of prostate carcinoma patients: an explorative study in North Indian population. Biomed Res Int. 2014;2014:158530.
Dwivedi S, Singh S, Goel A, Khattri S, Mandhani A, Sharma P, Misra S, Pant KK. Pro-(IL-18) and anti-(IL-10) inflammatory promoter genetic variants (intrinsic factors) with tobacco exposure (extrinsic factors) may influence susceptibility and severity of prostate carcinoma: a prospective study. Asian Pac J Cancer Prev. 2015;16(8):3173–81.
Dwivedi S, Goel A, Khattri S, Sharma P, Pant KK. Aggravation of inflammation by smokeless tobacco in comparison of smoked tobacco. Indian J Clin Biochem. 2015;30(1):117–9.
Dwivedi S, Goel A, Mandhani A, Khattri S, Pant KK. Tobacco exposure may enhance inflammation in prostate carcinoma patients: an explorative study in North Indian population. Toxicol Int. 2012;19(3):310–8.
Giugliano D, Salvatore T, Cozzolino D, Ceriello A, Torella R, D’Onofrio F. Sensitivity to beta-endorphin as a cause of human obesity. Metabolism. 1987;36:974–8.
Hurrle S, Hsu WH. The etiology of oxidative stress in insulin resistance. Biomed J. 2017;40(5):257–62.
Pereska Z, Dejanova B, Bozinovska C, Petkovska L. Pro-oxidative/antioxidative homeostasis in heroin addiction and detoxification. Bratisl Lek Listy. 2007;108(9):393–8.
Xu B, Wang Z, Li G, Li B, Lin H, Zheng R, Zheng Q. Heroin-administered mice involved in oxidative stress and exogenous antioxidant-alleviated withdrawal syndrome. Basic Clin Pharmacol Toxicol. 2006;99(2):153–61.
Purohit P, Nebhinani N, Sharma P. Evaluation of antioxidant status, high sensitivity C-reactive protein, and insulin resistance in male chronic opiate users without comorbidities. Indian J Psychol Med. 2017;39(3):299–305.
Ridker PM. Inflammatory biomarkers and risks of myocardial infarction, stroke, diabetes, and total mortality: implications for longevity. Nutr Rev. 2007;65(12Pt 2):S253–9.
Guzman DC, Vazquez IE, Brizuela NO, Alvarez RG, Mejia GB, Garcia EH, et al. Antioxidant activity of Portuguese honey samples: different contributions of the entire honey and phenolic extract. Food Chem. 2009;114:1438–43.
Acknowledgements
We acknowledge the support of technical staff at Department of Biochemistry, AIIMS Jodhpur and NGO Manklao de-addiction Centre for the constant support.
Funding
This work was supported by All India Institute of Medical Sciences Jodhpur intramural funding Grant No AIIMS/RES9010/2014/0000038.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Dwivedi, S., Purohit, P., Nebhinani, N. et al. Effect of Severity of Opiate Use on Cardiometabolic Profile of Chronic Opiate Dependents of Western Rajasthan. Ind J Clin Biochem 34, 280–287 (2019). https://doi.org/10.1007/s12291-018-0759-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-018-0759-5