Abstract
Background
Late recurrence accounts for nearly half of the recurrences in estrogen receptor (ER)-positive breast cancer and decreases post-recurrence survival in patients with ER-negative breast cancer. Clinicopathological factors and multigene assays have been used for various purposes but their prognostic capacity for late recurrence was limited. This study aimed to determine whether neutrophil to lymphocyte ratio (NLR) taken after primary treatment can be a feasible prognostic factor for late recurrence.
Methods
Patients who were diagnosed with primary breast cancer and completed planned treatment were enrolled; data were retrospectively collected from the Wonju Severance Hospital database of Yonsei University.
Results
496 patients completed planned treatment for their primary breast cancer. 385 were disease free after 5 years of the primary diagnosis and 330 were enrolled for second-look NLR analysis. NLR analysis performed approximately 5 years after the primary diagnosis categorized patients into high and low risk of late recurrence with p < 0.001 and an elevated NLR was found as an independent risk factor for late recurrence (HR 1.448, CI 1.168–1.795, p < 0.001).
Conclusion
A clinically valid biomarker to determine late recurrence is urgently needed to prevent patients from treatment extension with little benefit. Elevated NLR is found as an independent prognostic factor for late recurrence and could be utilized as a reliable, easily accessible, and cost-effective test.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Late recurrence, occurring after ≥ 5 years of primary diagnosis, accounts for nearly half of recurrence in estrogen receptor (ER)-positive breast cancer, although adjuvant chemotherapy and endocrine therapy for early breast cancer considerably affect outcomes [1,2,3]. Moreover, the risk of late recurrence and death never declined to 0, with relatively consistent rates ranging from 0.5 to 3% per year over the succeeding 5–10 years and even persisted for decades [2, 4, 5]. Patients with ER-negative breast cancer also experience decreased post-recurrence survival once they have late recurrent disease, although the number of patients who experience late recurrence is limited [6]. These findings, particularly in endocrine-positive breast cancer, had resulted in extended endocrine therapy beyond the 5-year initial treatment to determine prolonged disease-free and overall survival [7]. However, identifying patients who are at a risk for late recurrences is crucial, because extension of medical care beyond 5 years requires tactful approach [8, 9]. For example, extended hormonal treatment for patients with ER-positive breast cancer can also cause side effects, from life-threatening one to non-lethal but bothersome symptoms [8, 9]. Patients with breast cancer without ER should also be monitored for late recurrences because although late recurrence is uncommon, the risk remains even after decades, like in ER-positive disease [2, 5, 6, 10].
Clinicopathological factors, such as tumor size, nodal metastasis, and tumor grade, have been used as prognostic factors for breast cancer, including late recurrence [11]. However, these factors alone have been known to predict late recurrence inadequately, and one example is a recently reported overview analysis on > 60,000 disease-free women after 5 years of adjuvant endocrine therapy, showing that even patients with T1N0 disease still had 10–17% estimated risk of distant recurrence according to the histologic grade between 5 and 20 years [1]. Multigene expression profiles enhanced the prognostic or predictive power of clinicopathological characteristics, and late recurrence is also one of the areas in which multigene expression profiles could be integrated for better prediction [12, 13]. Although some studies have reported that clinicopathological parameters have a better predictive power than multigene expression assays, some have shown the opposite; however, neither clinicopathological factors nor multigene expression profiling has yielded optimum prediction of late recurrence, unless appropriately combined, which requires other factors to enhance the known prognostic factors [11, 13,14,15].
There is growing body of evidence indicating that biomarkers obtained after planned treatment such as preoperative systemic treatment can be used as prognostic indicator and complete remission after systemic treatment is one of the examples of how a biomarker can be developed using specimen obtained after treatment for individual patients [16].
Increased neutrophil to lymphocyte ratio (NLR) is reported as an independent predictor of survival in patients with breast cancer, and several recent studies have reported the predictive role of NLR in the prognosis of patients with breast cancers [17]. NLR from complete blood count, most commonly performed blood test to monitor patients’ general health and to screen for a variety of disorders, can be utilized as a biomarker reflecting status after treatment [18].
This study primarily aimed to determine whether NLR obtained after completion of primary treatment and 5-year follow-up can predict late recurrence in patients without evidence of breast cancer after 5 years of the primary diagnosis.
Materials and methods
Study cohort
A retrospective cohort was designed with female patients who were diagnosed with primary breast cancer from 2000 to 2010 and completed all phases of treatment at a single institute, Wonju Severance Hospital, Yonsei University, after obtaining approval from the institutional review board (YWMR-13-5-039). Patients who achieved 5-year disease-free survival from this “initial cohort” were included in the second cohort. All records were codified under the IRB data monitoring body and kept by a neutral person who was blinded from this study’s analysis (IC). Survival analysis was based on two databases, one from Wonju Severance Hospital and the other from Korean National Cancer Registry.
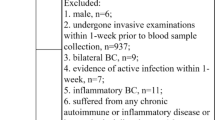
Inclusion and exclusion
Patients with primary invasive breast cancer were included. Patients with incomplete data, known stage IV disease, systemic autoimmune disease, such as systemic lupus erythematous or sclerodermatitis, were excluded from the initial NLR cohort. Patients with pregnancy-related breast cancer were also excluded. For the second cohort, patients who had insufficient data, took hormonal treatment more than 5 years or were not qualified as disease-free survival at 5 years after diagnosis were excluded. Disease-free survival 5-year after diagnosis was determined mainly based on radiologic studies. Patients who experience disease recurrence or death from any cause within 6 months before or after second look were also excluded.
Collection of data: clinicopathologic, laboratory and survival data
From the initial NLR cohort, data on the subjects’ medical history; age; pathologic results, such as tumor size, lymph node status, hormonal receptor status, and human epidermal growth factor receptor 2 (HER2) status; and laboratory data, including complete blood cell count with proportion of white blood cell count, were collected. For the second cohort, another complete blood cell count with proportion of white blood cell count between 4.0 and 6.0 years was collected and used for the second-look NLR. ER and progesterone receptor(PR) states were assessed through immunohistochemistry (IHC) stain and defined as positive when > 10% of tumor cells were stained according to the previous definition of positivity. HER2 status was assessed using IHC staining and defined positive if the score was 3. Fluorescent in situ hybridization was selectively performed when IHC staining score was 2, with the cutoff value being 2.2 times more signal than that of CEP17. NLR was calculated as neutrophil count divided by lymphocyte count. The cutoff value was defined by receiver operating characteristics (ROC) curve and Youden’s index.
Statistical analysis
Late recurrence was defined as any breast cancer-related event 5 years after completion of planned treatment, including local, regional, contralateral and distant recurrence and death from breast cancer, and any non-breast cancer-related death was censored. 5 years or 60 months was used to determine whether the recurrence was early or late. Overall recurrence defined as any recurrence detected at either earlier or later than 5-year time point and included local, regional, contralateral and distant recurrence, regardless of any non-breast cancer-related malignant disease or death. Chi squared or Fisher’s exact tests were used for categorical variables and Students t test was for continuous variables. The cutoff value was defined by receiver operating characteristics (ROC) curve and Youden’s index. The survival curves were calculated using the Kaplan–Meier method with the log-rank test and Cox proportional hazards model was used for multivariable analysis. All statistical tests were two sided and a p value of < 0.05 was considered statistically significant, using SPSS 23.0 (IBM Corp., Armonk, USA).
Results
Study cohort
Among the 496 patients who were diagnosed with breast cancer and completed primary treatment, 471 were included for initial NLR (Fig. 1). 25 patients were excluded from the analysis with various reasons as follows: three patients with past history of systemic disease such as systemic lupus erythematous (n = 2) or sclerodermatitis (n = 1), two patients with pregnancy-related breast cancer, ten patients with second malignancy within 5 years, five patients with only ER records as their follow-up, and five patients with insufficient data. 86 of the 471 patients (18.3%) experienced early recurrences. A total of 385 patients were reported as breast cancer free at the 5-year follow-up; 330 of them were enrolled into the second cohort after excluding 55 patients. 41 patients (85%) returned to their primary physician and three patients have only tentative diagnosis with no further studies: cerebrovascular disease (n = 2) and mandible necrosis (n = 1) were the suspected diseases. Two patients had insufficient data to support disease-free survival at 5 years after diagnosis (Supplementary Fig. 1) and five patients underwent hormonal treatment more than 5 years (Supplementary Table 1). Four patients were missing from any database. Survival data for these 55 patients were available from the National Cancer Registry with only one mortality which was also excluded from this study. Clinicopathological data of each cohort are presented in Table 1. Among the 330 patients enrolled in the second-look cohort, 21 (6.3%) experienced late recurrence.
Study profile. A total of 496 patients who were diagnosed with primary invasive breast cancer and completed the planned treatment were enrolled as the first cohort. Data of 471 patients were analyzed after excluding 25 patients who did not meet the eligibility criteria: past systemic disease history (n = 3), pregnancy-related breast cancer (n = 2), second malignancy within 5 years (n = 10), emergency room (ER) visiting as the only follow-up (n = 5) and insufficient data (n = 5). Among the 471 patients, 86 experienced early recurrence within 5 years, and the remaining 385 were disease free at 5 years after the primary diagnosis. A total of 337 patients were entered into the second cohort after excluding 55 patients with insufficient data for further analysis: return to their primary physician (n = 41), incomplete evidence of disease-free survival at 5-year diagnosis (n = 2), hormonal treatment more than 5 years (n = 5), emergency room records as the only follow-up data (n = 3), data missing (n = 4)
Late recurrence in second-look cohort
A total of 327 patients with subsequent NLR results had relevant disease-free survival after 4–6 years of primary diagnosis and, thus, were available for this study. Second look NLR was significantly correlated with risk of late recurrence. First, cut off value, 2.18 was derived from ROC curve with Youden index (Supplementary Fig. 2 and Supplementary table 1) and patients were divided into two groups according to their second look NLR. Kaplan–Meier estimates of late recurrence of breast cancer showed patients with higher second look NLR had worse prognosis than patients with lower NLR (p = 0.001) (Fig. 2). Cox proportional hazard model indicated that synchronous axillary lymph node metastasis (HR 1.053; 95% CI 1.002–1.114, p = 0.025) and second-look NLR (HR = 1.448; 95% CI 1.168–1.795, p < 0.001) were statistically significant risk factors (Table 2). Initial NLR, sampled ahead of any treatment either systemic or locoregional, was also tested, showing no significant contribution to the risk of late recurrence (HR 0.400; 95% CI 0.400–1.487, p = 0.171) (Table 2). When patients were divided into two groups, higher or lower NLR than 2.18, there were no significantly different clinicopathological characteristics except N stage (Table 3).
Late recurrence-free survival. Kaplan–Meier estimates of late recurrence-free survival after dichotomizing patients into two groups with higher or lower NLR. Blue and Green lines indicate patients with lower (blue) or higher (green) NLR than cutoff value, 2.18, driven from ROC curve with Youden index using SPSS. Patients with NLR of > 2.18 showed worse late recurrence-free survival (p < 0.001). Multivariate analysis with Cox proportional hazard model on factors affecting late recurrence-free survival is found in Table 2
Breast cancer-free survival and initial NLR, difference between two NLR values from each cohort
The initial NLR was related to overall recurrences including either early or late recurrence, and Kaplan–Meier method with log-rank test showed statistically significant poor survival with the cutoff value of 1.8 (Fig. 3a). Cox proportional hazard model indicated that tumor size, axillary lymph node metastasis, and high NLR value of > 2.18 were statistically significant risk factors for recurrences in general (Table 4). However, initial NLR was not different either in early (2.3016 ± 1.12) or late (2.3909 ± 1.51) recurrence groups (p = 0.452), and the Kaplan–Meier curve did not show any survival difference (Fig. 3b, c). NLR difference between the two cohorts also produced fair but less powerful AUC than that of NLR at 5 years after diagnosis (0.765 vs. 0.850).
Overall breast cancer-free survival. Blue and green lines indicate patients with lower (blue) or higher (green) than cutoff value, 2.18. a Kaplan–Meier estimates of breast cancer-free survival by NLR from the initial assay before giving any treatment. A total of 86 early and 21 late recurrences were reported and patients with NLR of > 2.18 showed worse prognosis (p = 0.031). b, c Neither early nor late recurrence-free survival was statistically significant when exclusively assessed. d The NLR values of both early and late recurrence groups were not different
Discussion
This study has shown that patients with high NLR approximately 5 years after the initial diagnosis have statistically significant worse breast cancer-free survival with late recurrence. Given that a relevant question in the current clinical field is who are residually at risk after completing the primary treatment, one of the strengths of this study is that it reflected the time point at 5 years after primary treatment, while most of the multigene expression profiles reflecting the time point not even before treatment had been given [12,13,14]. Indeed, most studies worked with primary tumors before treatment and studies that evaluated any specimen obtained 5 years after the primary treatment as a prognostic marker have been limited. Status of tumor(s) or patients after the primary treatment can be a feasible surrogate marker to predict late recurrence. Complete remission after the preoperative systemic treatment in ER-negative breast cancer is one of the examples, and in estrogen receptor-positive treatment, changes of Ki67 level after preoperative endocrine therapy are another one [19,20,21]. Another example is the circulating tumor cells 5 years after the primary diagnosis, which powerfully stratifies late recurrence with hazard ratio of approximately 13, which was much higher than that of any other expression profiles with hazard ratio range of approximately 2 [22]. Taken together, response after any treatment can be a surrogate marker for recurrence and this study showed the feasibility of NLR 5 years after the initial diagnosis as a prognostic factor for late recurrence. We believe that this study supports the use of specimen or samples obtained at a certain time point after completion of the treatment, which was 5 years after treatment in this study to predict the late recurrence.
Utilizing neutrophils and lymphocytes, factors related to tumor microenvironment are another specific feature of this study. Stratification of patients according to the clinicopathological factors of tumors remains important, and nodal involvement has been consistently reported as a strong prognostic factor of late recurrence [1, 2], which was also one of the independent risk factors of late recurrence in this study. However, a recent meta-analysis with > 60,000 women who remained disease free after 5 years of scheduled endocrine treatment showed risks of distant recurrence stratified according to the nodal status, and the risk was 13%, 20%, and 34% for T1N0, T1N1, and T1N2 patients, respectively [1], which means even N0 disease still has > 10% risk of late recurrence, suggesting that other factors are required for more sophisticated discrimination of late recurrence [5, 10, 12]. Although gene expression-based profiles have enhanced the prognostic ability of clinicopathological factors, these multigene expression assays have shown only a modest risk stratification in terms of late recurrence, and their clinical utility remains controversial [12,13,14, 22]. The importance of neutrophils and lymphocytes has been highlighted by the fact that tumor-infiltrating neutrophils and lymphocytes are strongly correlated with patient’s prognosis, worse prognosis with tumor-infiltrating neutrophils and better with tumor-infiltrating lymphocytes [23]. Neutrophils, the most commonly found immune cells in the blood, are considered to play a role in the development of metastatic disease, and elevated serum NLR is also highlighted by its significant correlation with poor prognosis in many cancers, including breast cancer [17, 24]. Although evidence regarding the mechanism underlying the association between high NLR and poor outcome in cancer patients is limited, neutrophils, early responders to wounds and infection, have been believed to play an inverse role against their protective role as immune cells when they respond tumor [25, 26]. Preclinical animal models showed that neutrophils localized around the primary tumor responding to IL-8 were secreted by tumor cells and eventually modify the extracellular matrix promoting tumor progression [27]. Neutrophils are also believed to localize to the lung and enhance early metastatic process in compliance with the primary tumor through reverse trans-endothelial migration [28, 29]. In another model, neutrophils had moderate antitumor immunity and resulted in more predominant metastatic disease by suppressing the function of the adaptive immune response in tumor microenvironment [30, 31]. However, there is a caveat to understanding the role of neutrophils in cancer: they can provide both protumor and antitumor functions, which still need to be enlightened [27]. Another thing not to be forgotten is that these findings mostly from animal models are not always translated or applicable to clinical data. Thus, this area should be actively investigated to understand and utilize immune-related therapy against late recurrence of breast cancer. This study showed that high NLR at 5 years after the primary treatment showed statistically significant higher risk of late recurrence and is the first research, based on our literature review, reporting that tumor microenvironment markers, i.e., elevated NLR, can be used as a prognostic marker for late recurrence. We believe that large clinical trials can help to confirm the clinical validity of NLR and to elucidate immunologic challenges and responses in patients with breast cancer.
Limitation of this study is small study population considering long-term survival and large number of breast cancer patients. Recent meta-analysis regarding NLR and breast cancer includes 15 studies with two previous meta-analysis, comprising a total of 8563 patients [24] and median number of study population from each study was 316, which was smaller than 1st cohort of this study, suggesting that NLR in breast cancer needs more attention from the academic society considering their capacity as cheaper and easily accessible prognostic factor. Another limitation of this study is 12% of follow-up loss after developing 2nd cohort. Surveillance/follow-up plan was as follows: history and physical examination two times per year as clinically appropriate for 5 years, then annually; Mammography and/or breast ultrasound every 12 months for 5 years, then every 2 years; periodic imaging and/or laboratory studies for metastases screening annually for 5 years, then recommended when there was any clinical sign or symptom suggestive of recurrent disease unless the patients had more than N3 disease, who were recommended annual screening for metastases. However, considering 5-year follow-up plan was standard plan during the study period and Health Insurance Review and Assessment system, Government-run health insurance system in Korea only covered these 5 years, there was no reason for surgical or medical oncologists to hold patients back from their primary physician or taking screening test supported by National Health Insurance Service. This bias from common clinical practice, however, has more chance to include less healthy patients in this study, which can affect the result. Recent studies showing better prognosis with extension of tamoxifen treatment will change medical practice and future study could include patients in a more random way until clinician can choose patients at a higher risk of late recurrence.
Conclusion
In summary, a high NLR at 5 years after initial diagnosis is associated with late recurrence in years 5–10 during follow-up. We believe that NLR can serve as a reliable prognostic biomarker of late recurrence in a cost-effective way.
References
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377(19):1836–46.
Brewster AM, Hortobagyi GN, Broglio KR, Kau SW, Santa-Maria CA, Arun B, et al. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100(16):1179–83.
Early Breast Cancer Trialists’ Collaborative Group. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–84.
Saphner T, Tormey DC, Gray R. Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol. 1996;14(10):2738–46.
Early Breast Cancer Trialists’ Collaborative Group. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–35.
Reddy SM, Barcenas CH, Sinha AK, Hsu L, Moulder SL, Tripathy D, et al. Long-term survival outcomes of triple-receptor negative breast cancer survivors who are disease free at 5 years and relationship with low hormone receptor positivity. Br J Cancer. 2018;118(1):17–23.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
van Hellemond IEG, Geurts SME, Tjan-Heijnen VCG. Current status of extended adjuvant endocrine therapy in early stage breast cancer. Curr Treat Options Oncol. 2018;19(5):19–26.
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2019;15(2):106–7.
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet. 2005;365(9472):1687–717.
Dowsett M, Sestak I, Regan MM, Dodson A, Viale G, Thurlimann B, et al. Integration of clinical variables for the prediction of late distant recurrence in patients with estrogen receptor-positive breast cancer treated with 5 years of endocrine therapy: CTS5. J Clin Oncol. 2018;36(19):1941–8.
Gyorffy B, Hatzis C, Sanft T, Hofstatter E, Aktas B, Pusztai L. Multigene prognostic tests in breast cancer: past, present, future. Breast Cancer Res. 2015;17:11.
Sestak I, Cuzick J. Markers for the identification of late breast cancer recurrence. Breast Cancer Res. 2015;17:10.
Sestak I. Risk stratification in early breast cancer in premenopausal and postmenopausal women: integrating genomic assays with clinicopathological features. Curr Opin Oncol. 2019;31(1):29–34.
Sestak I, Buus R, Cuzick J, Dubsky P, Kronenwett R, Denkert C, et al. Comparison of the performance of six prognostic signatures for estrogen receptor-positive breast cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018;4(4):545–53.
Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30(26):3242–9.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):124.
Agrawal D, Sarode R. Complete blood count or complete blood count with differential: what’s the difference? Am J Med. 2017;130(8):915–6.
Ellis MJ, Suman VJ, Hoog J, Lin L, Snider J, et al. Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2–3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype-ACOSOG Z1031. J Clin Oncol. 2011;29(17):2342–9.
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia J, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26(8):1275–81.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13(8):2329–34.
Sparano J, O’Neill A, Alpaugh K, Wolff AC, Northfelt DW, Dang CT, et al. Association of circulating tumor cells with late recurrence of estrogen receptor-positive breast cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018;4(12):1700–6.
Shen M, Hu P, Donskov F, Wang G, Liu Q, Du J. Tumor-associated neutrophils as a new prognostic factor in cancer: a systematic review and meta-analysis. PLoS One. 2014;9(6):e98259.
Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19(1):2.
Tuting T, de Visser KE. How neutrophils promote metastasis. Science. 2016;352(6282):145–6.
Giese MA, Hind LE, Huttenlocher A. Neutrophil plasticity in the tumor microenvironment. Blood. 2019;133(20):2159–67.
De Larco JE, Wuertz BR, Furcht LT. The potential role of neutrophils in promoting the metastatic phenotype of tumors releasing interleukin-8. Clin Cancer Res. 2004;10(15):4895–900.
Wculek SK, Malanchi I. Neutrophils support lung colonization of metastasis-initiating breast cancer cells. Nature. 2015;528(7582):413–7.
Acharyya S, Massague J. Arresting supporters: targeting neutrophils in metastasis. Cell Res. 2016;26(3):273–4.
Coffelt SB, Kersten K, Doornebal CW, Weiden J, Vrijland K, Hau CS, et al. IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015;522(7556):345–8.
Garcia-Mendoza MG, Inman DR, Ponik SM, Jeffery JJ, Sheerar DS, Van Doorn RR, et al. Neutrophils drive accelerated tumor progression in the collagen-dense mammary tumor microenvironment. Breast Cancer Res. 2016;18(1):49.
Acknowledgements
The authors would like to thank all patients who showed courage against breast cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and for this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Moon, G., Noh, H., Cho, IJ. et al. Prediction of late recurrence in patients with breast cancer: elevated neutrophil to lymphocyte ratio (NLR) at 5 years after diagnosis and late recurrence. Breast Cancer 27, 54–61 (2020). https://doi.org/10.1007/s12282-019-00994-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-019-00994-z