Abstract
Background
Microinvasive breast cancer is a rare entity in which an invasive component not exceeding 1 mm is found, mostly in a ductal carcinoma in situ setting. Its diagnosis can be difficult and must rely upon immunohistochemistry markers. Many studies have analyzed pathological characteristics of this cancer to delineate its biological profile and possibly identify risk factors of axillary lymph nodes infiltration, which might be present and therefore clinically relevant. Starting from a relative large number of cases we aimed to analyze pathological data, cancer subtypes distribution, and their correlation to nodal metastasis, comparing our results to the existing recent literature.
Methods
All cases of microinvasive breast cancer were retrieved from institutional database from 1992 to 2014. Pathological parameters were analyzed for entire cohort. Moreover, cases submitted to standardized sentinel node biopsy in a restricted period, 2000–2014, were selected to correlate pathology and cancer subtype to axillary lymph nodes status.
Results
174 cases (1.4 % of operated breast cancers) were evaluated in the larger period, 1992–2014. Neither specific pathological parameters were expressed nor a peculiar cancer subtype was represented. 126 cases were selected for axillary staging analysis. Eighteen cases (14.3 %) had lymph nodes metastasis, 10 ITCs (7.9 %), 3 micrometastases (2.4 %), and 5 macrometastases (4 %). An associated intraductal component of carcinoma over 20 mm in maximum dimension resulted significant at multivariate analysis, but only if including ITCs, while this risk factor was not reproduced for micro- and macrometastases only.
Conclusions
Microinvasive breast cancer does not seem to have specific pathological and biological traits. An associated intraductal component of carcinoma >20 mm in size is a specific risk factor for ITCs nodal metastasis. Its clinical significance is anyway limited and therefore sentinel node biopsy should be performed case by case and not routinely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “microinvasive” was used for breast cancer (BC) by Lagios in 1982 for the first time [1], as synonymous of an extent of invasion lesser than 1 mm. Many different definitions have been used throughout the past decades. The most common is reported in the 7th edition of the AJCC cancer staging manual [2], as an invasive breast cancer with the greatest focus not exceeding 1 mm in its dimensions. A more comprehensive definition is present in the World Health Organization Classification of Tumors of the Breast, where a microinvasive breast carcinoma (MIBC) is characterized “by one or more clearly separate microscopic foci of infiltration of tumor cells into the mammary stroma, each ≤1 mm in size.” No further extension beyond the specialized intralobular stroma is required, the number of invasive foci and their percentage among all the carcinoma cells are irrelevant and sizes of different foci are not to be added together [3].
MIBC is frequently found in a high nuclear grade-comedo ductal carcinoma in situ (DCIS) setting, less frequently with other types of DCIS or lobular carcinoma in situ (LCIS) [4]. The sole presence of an invasive breast carcinoma 1 mm or less, without any in situ background, is very rare and should be better regarded as an invasive carcinoma of that specific diameter [5].
Diagnosis of MIBC is another crucial issue, since it might become very challenging for a pathologist. Many artifacts can mimic a microinvasion leading to overdiagnosis [6]. On the other hand, a poor tissue sampling without serial macroscopic sectioning, which is highly recommended [7], can cause an underdiagnosis problem.
Immunohistochemistry (IHC) is of utmost importance in the pathological diagnostic process. Basement membrane components such as laminin and type IV collagen are useful but IHC is technically difficult for these markers in formalin-fixed, paraffin-embedded tissue [6]. Moreover, invasive tumors cells can still synthesize the aforementioned basement membrane components, thus limiting their use in invasion distinction [8].
Myoepithelial cells surrounding nests of carcinoma cells specify an in situ neoplasia, while their absence defines invasion [9]. Many markers are used to detect myoepithelial cells, the most reliable ones are smooth muscle myosin heavy chain (SMM-HC), Calponin, and p-63 [8, 10].
Once a correct diagnosis has been made, some histological and biological features might be useful for planning a right treatment of MIBC. Particularly, axilla management and adjuvant therapies are frequent issues in the everyday clinical practice of MIBC. Some recent studies are present in literature dealing with the pathological and biological profiling of MIBC in order to find traits which might lead to higher risk cases and clinical implications [11–14]. So far there are many conflicting results in literature and it is difficult to distinguish higher risk groups for axillary involvement among MIBC patients.
Starting from a relative large number of cases for this rare BC subgroup, we conducted a retrospective observational study. The aim of the present study is to describe pathological features and BC subtypes distribution for all MIBC cases. Furthermore, we tried to identify risk factors for axillary lymph nodes metastasis in order to find specific indications for sentinel lymph node biopsy (SLNB) staging in case of MIBC.
Materials and methods
All cases of MIBC diagnosed and treated from 1992 to March 2014 at our institution were retrieved from our prospectively collected database.
Pathology and surgery reports were thoroughly revised. Patients’ baseline and clinical characteristics were extracted along with surgical and pathologic details. Study design and all required documents were presented and approved by the Local Ethical Committee.
We primarily analyzed the entire cohort of MIBC cases, describing baseline characteristics, pathologic features, and cancer subtype distribution, in order to find any peculiar profile of this rare tumor. The parameters we used were intraductal component of carcinoma size, intraductal component of carcinoma and MIBC tumor grade, MIBC multifocality, intraductal and invasive histologic type. Thereafter, specifically for the MIBC component, we reported LVI, Ki-67 stain percentage, hormones receptor status, HER-2 status, and cancer biologic subtype. A secondary analysis was performed to evaluate risk factors of lymph nodes involvement. For such evaluation, we considered only those cases of MIBC submitted to SLNB and specifically those diagnosed and treated between January 2000 and March 2014, when SLNB technique was standardized at our institution and always performed by means of Technetium 99 radionuclide sulfur colloid. We therefore divided up our cohort into two groups, those with any type of axillary lymph nodes (ALN) metastasis and those without any lymph node metastasis. The two groups were hence compared in terms of the aforementioned pathological features and biologic subtype to find out any significant difference.
Pathological and immunohistochemical analysis
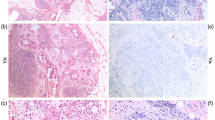
Every case of MIBC was diagnosed by specialized pathologists, dedicated to breast diseases. Diagnosis was made according to the AJCC and WHO criteria. Starting from macroscopic examination, in order to correctly diagnose possible site/s of microinvasion in a background of intraductal carcinoma, handling of surgical specimens included “bread-slicing” method: mastectomies specimens were serially sectioned at 1.5–2 mm intervals from superficial to deep aspects, and wide excision specimens, after ink application for margins assessment, were serially sectioned at 1.5–2 mm intervals from medial to lateral aspects. Tissue sections were chosen for microscopic examination on corresponding mammographic patterns in case of mastectomy and on surgical specimen radiography in case of wide excision. Focus or foci of microcalcifications were completely and sequentially submitted to histological examination. Because microcalcifications are sometimes present in part of the cancer only, randomly chosen areas of fibrous parenchyma were also submitted to histological examination. In cases of diffuse microcalcifications, specimens were extensively sampled in order to identify areas of carcinoma and possibly microinvasion.
IHC for SMM-HC, Calponin, and p-63 was adopted to confirm foci of infiltration. Cancer subtype (Luminal A, Luminal B HER-2 negative, Luminal B HER-2 positive, HER-2 positive and Triple Negative) was determined by ER, PR receptors, and HER-2 status. Ki-67 stain was used for distinction of Luminal A and B. An MIBC was deemed Luminal A when ER and/or PR receptors were positive, HER-2 status was negative and Ki-67 was <20 %. Otherwise with Ki-67 ≥20 % the same tumor would have been categorized as Luminal B HER-2 negative. A Luminal B HER-2 positive, on the other hand, is ER and/or PR receptors positive and HER-2 positive independently of Ki-67 percentage. Hormone receptor status was reported as negative when <1 % of tumors cells stained at IHC. HER-2 status was determined only by IHC in cases scored as 0 or 1+ (negative) and 3+ (positive). Fluorescence in situ hybridization (FISH) was used in 2+ cases when a chemotherapy regimen was an option for the patient, otherwise it was not performed. Those 2+ cases in which FISH test was not adopted, because deemed clinically irrelevant, were considered “unknown” as for HER-2 status. Tumor cells replication rate was always evaluated by means of Ki-67 stain using MIB-1 antibody. In some cases, receptor status and Ki-67 stain were determined for the BC in situ component alone, due to MIBC focus/i dimensions. An almost complete concordance has been previously demonstrated between the microinvasive component and the in situ background [12, 15]. Recorded histologic features of MIBC were type, grade, number/dimensions of foci, and distance from inked margins. The associated intraductal component was characterized by type, grade, extension, and margins as well. Grade was scored according to the Nottingham histologic score system (the Elston-Ellis modification of Scarff-Bloom–Richardson grading system).
Lymph nodes metastasis was described as isolated tumor cells (ITCs) when tumor deposit was ≤0.2 mm, micrometastasis when >0.2 and ≤2 mm, and macrometastasis when >2 mm. Unless metastasization was clearly evident by hematoxylin and eosin staining, as for macrometastases, IHC was always used to confirm nodal involvement, particularly for micrometastases and in every case for ITCs.
Statistical analysis
Pearson’s Chi square test and Fisher exact test, where appropriate, were used to assess differences in clinical and biological characteristics between ALN positive/negative subgroups. Significant factors, found in univariate analyses, were further analyzed by logistic regression analysis to identify the independent factors associated with ALN infiltration. Exact logistic regression test and Firth logistic regression test were used in order to solve the phenomenon of separation [16]. Significance was defined as 2-tailed p < .05. All statistical analyses were performed using STATA software, version 12.1.
Results
Among 12,152 cases of breast cancer operated on at our Institution between 1992 and March 2014, and prospectively collected in a database, a total count of 174 (1.4 %) cases of MIBC (T1mi) was extracted. In the same time span, Tis cases were 2223 (18.3 %), while T1a BC were 1227 (10.1 %). Table 1 shows distribution of baseline characteristics, pathological and biological features of all these cases. No specific biomarkers or histologic features stand out as particularly expressed in MIBC cases. Cancer subtypes distribution is also in line with invasive cancers.
Limiting the analysis to MIBC patients submitted to SLNB after 2000, 126 cases were identified. Characteristics of this cohort are shown in Table 2. Eighteen cases (14.3 %) had lymph nodes metastasis, namely 10 ITCs (7.9 %), 3 micrometastases (2.4 %), and 5 macrometastases (4 %).
Two parameters were statistically significant as risk factors for ALN metastasis: LVI and an associated intraductal component of carcinoma dimension over 20 mm. At multivariate analysis, using Firth logistic regression test as well, only intraductal component of carcinoma dimension over 20 mm remained significant. If we look in detail into this parameter we can find that this is true only for ITCs. In fact, out of 10 cases with ITCs on SLNB a total of 7 cases had intraductal component of carcinoma dimension >20 mm, 1 case was ≤20 mm, and 2 were unknown. Instead, we recorded 1 case >20 mm, 1 case ≤20 mm, 1 case unknown among micrometastases, and 2 cases >20 mm and 3 cases ≤20 mm among macrometastases. Even changing the cutoff to 30 mm, intraductal component of carcinoma dimension remains a significant risk factor for ALN metastasis, but, once again, for ITCs only. On the contrary, lowering the cutoff to 10 mm would eliminate any significant difference.
Furthermore, six patients had a completion axillary lymph nodes dissection. Five were those with macrometastases at SLNB and one was a patient with ITCs at SLNB. Only 1 case, in the group of macrometastases, had a single non-sentinel positive (macrometastatic) node.
Discussion
This study is a contribution to the existing literature on MIBC. So far many cancer subtype features and many risk factors for nodal metastasis have been proposed for the MIBC subgroup of breast cancers.
Breast cancer (BC) subtypes, expressed by estrogen (ER) and/or progesterone (PR) receptor status and by HER-2 status as well, have proved to be significant for local and distant recurrence both after mastectomy and breast conserving surgery (BCS) in cases of invasive BC [17, 18]. Therefore, hypothetically, such a consideration might be applied to MIBC as well.
Yu et al. [11] found that DCIS, DCIS with microinvasion (DCIS-Mi), and DCIS with an invasive component greater than 1 mm (DCIS-I) can be considered as entities with progressive different biological features, due to subtypes distribution like a spectrum with hormone receptors loss (ER 50 % positive in DCIS-Mi) and HER-2 positivity (37 % in DCIS-Mi) more pronounced as invasion increased.
In a study by Margalit [12], MIBC was found to be ER positive in 61 % of cases and HER-2 positive in 49 % (subtype Luminal B), which is significantly higher than for the in situ and invasive counterparts [15, 19]. In the same study, no correlation was found between biologic subtype, number of foci, and axillary metastases, due to the very small number of these (4 %, micrometastases only).
Also another recent study [13] could not find any association between subtype, foci, and lymph nodes metastasis, because of the small sample size, 1 micrometastasis and 1 macrometastasis among 35 cases.
In a 2008 review, a nodal metastasis rate ranging from 0 to 28 % is reported and axillary staging is deemed mandatory in case of microinvasion [20]. In a recent review and meta-analysis of Sentinel Lymph Node (SLN) metastasis, an overall macrometastasis rate of 3.2 % and micrometastasis rate of 4.0 % were reported considering 756 patients from 18 different studies [14]. In 47 patients with SLN macrometastasis, a rate of 29.7 % of non-SLN positivity was found on further axillary dissection.
Based on these numbers, authors conclude that SLNB should not be performed as standard practice in MIBC, but rather proposed to individualized higher risk cases.
In the study of the Rome Breast Cancer Study Group [21], cited in the meta-analysis, incidence of SLN metastases was 4 % in pT1a tumors and 7.8 % in pT1mic. Authors speculate that this might reflect a more aggressive nature of this subgroup, from the very beginning, as previously reported in another publication [22].
In a Korean study with 293 cases, which is not included in the aforementioned meta-analysis, lymph nodes macrometastases were found in 4 cases, micrometastases in 12, and ITCs in 6 patients [23]. At a multivariate analysis, lymphatics invasion and positive ER status were found independent predictors of lymph nodes metastases. HER-2 status was not tested by FISH in any case. Authors conclude that SLNB might be considered only in these selected, at risk, cases.
The most recent and largest study on this topic, with 414 cases, was not able to find any correlation between nodal metastasis at SLNB and MIBC multifocality, dividing up all cases into two cohorts: one single focus of infiltration and 2 or more, as surrogates of infiltrating tumor load. In this study from MSKCC [24], rates of 1.4 and 6.3 % were found for macro- and micrometastases, respectively, with LVI being the only pathologic factor associated with a positive SLNB. Compared to our study, it did not consider ITCs in the nodal metastasis evaluation and it did not include the associated intraductal component of carcinoma dimensions, histotype and grade, and MIBC (T1mi) Ki-67 as pathological factors in the risk factors analysis. A previous smaller study from a different institution [25] had found a trend toward higher risk of nodal metastasis in case of MIBC multifocality, although not a statistical significant level, while negative ER status was significantly associated with nodal infiltration in contrast with the Korean study results.
To our knowledge, our study is the third largest series of SLN status in MIBC cases, with the current AJCC definition. Considering the entire cohort of cases, our results show that no pathological parameter or a cancer subtype is specifically expressed in MIBC. We were not able to find a trait that could let us speculate on a possible more aggressive nature of MIBC. From our results, MIBC is only a different entity in terms of T staging and not of biology. Differences from other studies might be the effect of different patients’ populations (genetic and environmental factors) and of the intrinsic technical difficulty of analyzing all parameters in small samples like the MIBC cases, with different laboratory diagnostic methodologies. As for ALN positivity at SLNB, we found out that among 126 patients only 5 (4 %) had macrometastases, 3 (2.4 %) had micrometastases, and 10 (7.9 %) had ITCs. An associated intraductal component of carcinoma with at least 20 mm in diameter resulted to be the only risk factor at multivariate analysis. This is confirmed only if including ITCs among nodal metastases in the analysis. Micro- and macrometastases alone did not have any specific risk factor. We were not able to confirm LVI as a risk factor as in the Korean and MSKCC studies. Hence, an associated intraductal component of carcinoma >20 mm can be reliable as a risk factor for ITCs ALN metastasis in our study. Since MIBC diagnosis is usually made “ex post,” meaning post-operative, the decision to perform or not a delayed SLNB is sometimes debated. Therefore, unless a SLNB has already been performed because of a large and suspicious DCIS or in case of mastectomy, only risk factors can guide the surgeon in advising a delayed SLNB to a woman with MIBC.
Moreover it is worth to be considered that the decision of a delayed SLNB should be taken only for a staging purpose, in order to schedule adjuvant systemic therapies. There is no reason to perform a SLNB in case of MIBC for a possible completion ALN dissection (CALND) for local disease control. According to St. Gallen International Expert Consensus 2011, “isolated tumor cells, and even metastases up to 2 mm (micrometastases) in a single sentinel node, were not considered to constitute an indication for axillary dissection regardless of the type of breast surgery carried out” [26]. The IBCSG 23-01 trial showed no benefit of axillary dissection in case of one or more micrometastatic sentinel nodes [27]. And eventually, along with the ACOSOG Z0011 trial, even in selected cases with one or two macrometastatic sentinel lymph nodes, CALND can be omitted if whole breast radiation therapy is planned [28]. Thus, the surgical clinical relevance of SLNB in MIBC, for a possible CALND, would be present only in mastectomy cases with macrometastatic SLN, when chest wall radiation therapy is not planned. Moreover, we found out that only in one patient, out of 5 macrometastatic cases submitted to CALND in our series, only one single non-sentinel infiltrated node was found.
Thus, in the decision-making process of performing SLNB to correctly stage a MIBC case for possible adjuvant therapies, the knowledge of confirmed risk factors, such as LVI from the American and Korean studies and intraductal component of carcinoma dimension >20 mm from our study, could be a precious guidance.
There are some limitations in our study which we should mention. First of all it is a retrospective study. Moreover, the study time period is quite long, from 1992 to 2014 for entire cohort and from 2000 to 2014 for the SLNB group. Obvious technical improvements throughout all this time, either in pathology or in surgical procedures, might bias the results.
In conclusion, we can state that our study is a thorough focus on the pathological nature of MIBC and its surgical implications in terms of SLNB. We performed a broad analysis of any pathological parameter of the MIBC tumor and its associated intraductal component, of the cancer subtypes distribution and eventually of their correlation to nodal metastasis, considering ITCs as well. We were not able to find any significantly expressed parameter or cancer subtype in our MIBC population. Lymph nodes micro- or macrometastases are a rare event. None of the analyzed pathologic features or cancer biologic subtype resulted as a specific statistical significant risk factor for such metastases. On the other hand, the associated intraductal component of carcinoma dimensions over 20 mm was a significant risk factor for nodal ITCs metastasis. Therefore, axillary staging by means of SLNB could not be performed on a routine basis for MIBC cases, but rather discussed case by case on a multidisciplinary level, whenever a risk factor is present and it might add staging information for adjuvant therapy options.
References
Lagios MD, Westdahl PR, Margolin FR, Rose MR. Duct carcinoma in situ. Relationship of extent of noninvasive disease to the frequency of occult invasion, multicentricity, lymph node metastases, and short-term treatment failures. Cancer. 1982;50(7):1309–14.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. American Joint Committee on Cancer. AJCC cancer staging manual, vol. VIII. 7th ed. New York: Springer; 2010. p. 345–77.
Pinder SE, Ellis IO, Schnitt SJ, Tan PH, Rutgers E, Morrow M. Microinvasive carcinoma. In: Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, Van de vijvair MJ, editors. WHO classification of tumors of the breast. Lyon: IARC Press; 2012. p. 96–7.
Nemoto T, Castillo N, Tsukada Y, Koul A, Eckhert KH Jr, Bauer RL. Lobular carcinoma in situ with microinvasion. J Surg Oncol. 1998;67:41–6.
Bianchi S, Vezzosi V. Microinvasive carcinoma of the breast. Pathol Oncol Res. 2008;14:105–11.
Schnitt SJ. Microinvasive carcinoma of the breast: a diagnosis in search of a definition. Adv Anat Pathol. 1998;5:367–72.
Olivotto I, Levine M. Steering committee on clinical practice guidelines for the care and treatment of breast cancer. Clinical practice guidelines for the care and treatment of breast cancer: the management of ductal carcinoma in situ (summary of the 2001 update). CMAJ. 2001;165:912–3.
Yaziji H, Gown AM, Sneige N. Detection of stromal invasion in breast cancer: the myoepithelial markers. Adv Anat Pathol. 2000;7(2):100–9.
Damiani S, Ludvikova M, Tomasic G, Bianchi S, Gown AM, Eusebi V. Myoepithelial cells and basal lamina in poorly differentiated in situ duct carcinoma of the breast: an immunocytochemical study. Virchows Arch. 1999;434:227–34.
Werling RW, Hwang H, Yaziji H, Gown AM. Immunohistochemical distinction of invasive from noninvasive breast lesions: a comparative study of p63 versus calponin and smooth muscle myosin heavy chain. Am J Surg Pathol. 2003;27(1):82–90.
Yu KD, Wu LM, Liu GY, Wu J, Di GH, Shen ZZ, et al. Different distribution of breast cancer subtypes in breast ductal carcinoma in situ (DCIS), DCIS with microinvasion, and DCIS with invasion component. Ann Surg Oncol. 2011;18(5):1342–8.
Margalit DN, Sreedhara M, Chen YH, Catalano PJ, Nguyen PL, Golshan M, et al. Microinvasive breast cancer: ER, PR and HER-2/neu status and clinical outcomes after breast-conserving therapy or mastectomy. Ann Surg Oncol. 2013;20(3):811–8.
Shatat L, Gloyeske N, Madan R, O’Neil M, Tawfik O, Fan F. Microinvasive breast carcinoma carries an excellent prognosis regardless of the tumor characteristics. Hum Pathol. 2013;44:2684–9.
Gojon H, Fawunmi D, Valachis A. Sentinel lymph node biopsy in patients with microinvasive breast cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2014;40:5–11.
Burkhardt L, Grob TJ, Hermann I, Burandt E, Choschzick M, Jänicke F, et al. Gene amplification in ductal carcinoma in situ of the breast. Breast Cancer Res Treat. 2010;123(3):757–65.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21:2409–19.
Kyndi M, Sørensen FB, Knudsen H, Overgaard M, Nielsen HM, Overgaard J. Danish Breast Cancer Cooperative Group. Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol. 2008;26(9):1419–26.
Nguyen PL, Taghian AG, Katz MS, Niemierko A, Abi Raad RF, Boon WL, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol. 2008;26(14):2373–8.
Owens MA, Horten BC, Da Silva MM. HER2 amplification ratios by fluorescence in situ hybridization and correlation with immunohistochemistry in a cohort of 6556 breast cancer tissues. Clin Breast Cancer. 2004;5(1):63–9.
Guth AA, Mercado C, Roses DF, Darvishian F, Singh B, Cangiarella JF. Microinvasive breast cancer and the role of sentinel node biopsy: an institutional experience and review of the literature. Breast J. 2008;14(4):335–9. doi:10.1111/j.1524-4741.2008.00594.x.Review.
Fortunato L, Santoni M, Drago S, Gucciardo G, Farina M, Cesarini C, et al. Rome Breast Cancer Study Group. Sentinel lymph node biopsy in women with pT1a or “microinvasive” breast cancer. Breast. 2008;17:395–400.
Adamovich TL, Simmons RM. Ductal carcinoma in situ with microinvasion. Am J Surg. 2003;186:112–6.
Ko BS, Lim WS, Kim HJ, Yu JH, Lee JW, Kwan SB, et al. Risk factors for axillary lymph node metastases in microinvasive breast cancer. Ann Surg Oncol. 2012;19:212–6. doi:10.1245/s10434-011-1812-2.
Matsen CB, Hirsch A, Eaton A, Stempel M, Heerdt A, Van Zee KJ, et al. Extent of microinvasion in ductal carcinoma in situ is not associated with sentinel lymph node metastases. Ann Surg Oncol. 2014;21(10):3330–5. doi:10.1245/s10434-014-3920-2.
Kapoor NS, Shamonki J, Sim MS, Chung CT, Giuliano AE. Impact of multifocality and lymph node metastasis on the prognosis and management of microinvasive breast cancer. Ann Surg Oncol. 2013;20(8):2576–81. doi:10.1245/s10434-013-2924-7.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B. Senn HJ; Panel members. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22(8):1736–47. doi:10.1093/annonc/mdr304.
Galimberti V, Cole BF, Zurrida S, Viale G, Luini A, Veronesi P, et al. International Breast Cancer Study Group Trial 23-01 investigators. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14(4):297–305. doi:10.1016/S1470-2045(13)70035-4.
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252(3):426–32. doi:10.1097/SLA.0b013e3181f08f32.
Acknowledgments
We thank Monica Macguire for English proofreading. Authors themselves and Institutional University Hospital funds covered all the expenses for the present study. No third party funding was received.
Conflict of interest
All the authors disclaim any conflict of interest.
Ethical standards
Study protocol and related documentation have been approved by the appropriate hospital ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Orzalesi, L., Casella, D., Criscenti, V. et al. Microinvasive breast cancer: pathological parameters, cancer subtypes distribution, and correlation with axillary lymph nodes invasion. Results of a large single-institution series. Breast Cancer 23, 640–648 (2016). https://doi.org/10.1007/s12282-015-0616-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-015-0616-9