Abstract
Background
Fertility is one of the key aspects of quality of life for breast cancer patients of childbearing age. The objective of this study was to describe fertility-related practice for young breast cancer patients in Japan and to identify healthcare provider factors that contribute to physicians’ behavior towards fertility preservation.
Methods
A cross-sectional survey was developed in order for Japanese breast cancer specialists (n = 843) to self-evaluate their knowledge, attitude, and behavior regarding fertility preservation. Survey items included questions regarding knowledge of and attitude toward fertility issues in cancer patients, fertility-related practice, potential barriers for the discussion of fertility with patients, and responding physicians’ socio-demographic background.
Results
Four hundred and thirty-four (52%) breast oncologists responded to the survey. Female and younger oncologists (age less than 50 years) had significantly higher probability of referring patients to reproductive specialists. Physicians who had better knowledge score and positive attitudes toward fertility preservation were more likely to discuss potential fertility issues with cancer patients. This was significantly associated with consultation and referral to reproduction specialists when encountering fertility issues with cancer patients. Risk of recurrence, lack of collaborating reproductive specialists, and time constraints in the clinic were identified as major barriers to discussion of fertility preservation with breast cancer patients.
Conclusion
Female and younger physicians as well as physicians working in a multidisciplinary environment had positive attitudes and behavior towards fertility preservation in breast cancer patients. The development of comprehensive and interdisciplinary programs for healthcare providers is necessary to meet the expectations and fertility needs of breast cancer patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With improvement of cancer prognosis, fertility has become one of the key aspects of quality of life for breast cancer patients of childbearing age. Distress about interrupted childbearing is likely to persist in long-term female cancer survivors [1]. The American Society of Clinical Oncology (ASCO) has developed guidance for oncologists regarding available fertility preservation methods and related issues [2]: oncologists should address the possibility of infertility with patients during their reproductive years and be prepared to discuss possible fertility preservation options or refer appropriate and interested patients to reproductive specialists as early as possible during treatment planning.
However, previous studies have shown that only 23% of the patients younger than 40 years of age were informed of potential infertility after cancer treatment in a single institution in Japan and less than half of oncologists were following the ASCO guideline in the USA [3, 4]. The practice of oncologists regarding fertility preservation in cancer patients of reproductive age may depend on multiple factors: the patient’s medical and psychosocial condition [5, 6], the patient’s knowledge [7], and physicians’ knowledge about fertility preservation [8].
We have previously analyzed the decision-making process for adjuvant treatment in young breast cancer patients of reproductive age [3]. Significantly less patients expressed interest in fertility when they had children or advanced disease. Less aggressive treatment (without chemotherapy) was recommended by oncologists for patients who voluntarily expressed an interest in preserving fertility [3]. Nearly one-third of the patients who expressed an interest in fertility selected a different adjuvant treatment from the primary recommendation of the oncologist because of their concern for preserving fertility, whereas the majority of patients who did not express an interest in preserving fertility followed the oncologists’ primary recommendation [3].
The awareness and attitude of patients in the clinic might reflect the ability of healthcare providers to provide an environment in which patients could bring up fertility issues. The objectives of this study include describing fertility-related practice for breast cancer patients in a variety of clinical settings in Japan and identifying healthcare provider factors that contribute to physicians’ behavior regarding fertility preservation in young breast cancer patients.
Methods
Selection of participant
A cross-sectional survey was developed in order for board-certified breast oncologists of the Japanese Breast Cancer Society (JBCS), who are the main physicians treating breast cancer patients in Japan, to self-evaluate their knowledge, perception, and behavior regarding fertility issues in young breast cancer patients.
Measures
The survey consisted of 49 items including questions regarding knowledge of and attitudes towards fertility in cancer patients, practice behavior of fertility-related discussions with patients, potential barriers for these discussions, and demographic background of the practitioners (Table 1). Survey items were derived from existing literature and multidisciplinary discussion. Physicians were asked to evaluate their agreement with the statements using a five-grade system (1, strongly agree; 2, agree; 3, cannot decide; 4, disagree; 5, strongly disagree).
-
1.
Knowledge about fertility issues in breast cancer patients
To evaluate the accuracy of knowledge about fertility issues in breast cancer patients, the statements were developed from the latest JBCS treatment guideline [5]. For statements A-1 and A-4, the respondents were considered to have more accurate knowledge when the score was lower. For statements A-2 and A-3, the respondents were considered to have more accurate knowledge when the score was higher. Then the sum of (5 − “score for A-1”) + (“score for A-2”) + (“score for A-3) + (5 − “score for A-4”) was calculated. The respondents with a higher sum were considered to have more accurate overall knowledge. A-5 was not used to evaluate the accuracy of knowledge because of lack of definite evidence, but correlated with the use of LHRH agonist for fertility preservation.
-
2.
Practice behavior for breast cancer patients of reproductive age
Practice behavior statements consisted of 13 items including statements used in the US oncologist survey with some modifications to adapt to Japanese practice setting. The statements “I discuss the impact of cancer treatment on future fertility with my patients”, “I consult reproductive specialists with questions about fertility issues in my patients”, and “I refer patients who have questions about fertility to reproductive specialists” were considered the most important behavior according to the ASCO guideline [2].
-
3.
Potential barriers for discussing fertility issues with breast cancer patients
Among seven potential barriers asked in the questionnaire, four were similar to statements used in the US survey [4]. We put three additional statements (patients’ voluntary expression of interest, existence of spouse/partner, and support from co-medical staff) that were created by findings from our previous study [2] and by considering Japanese culture. In addition, we asked the participant to describe the greatest difficulty in discussing fertility in an open question.
-
4.
Attitude towards fertility preservation of cancer patients
Five statements were selected from the US survey [4]. Because the hereditary aspect of breast cancer was considered to be not genuinely linked with perception of fertility preservation, the item was not included in our analysis. Participants were considered to be positive toward fertility preservation if the sum of scores was higher than 3. The sum of scores for statements from D-1 through D-5 was calculated and the respondents with higher total score were considered as physicians with a “positive attitude” towards fertility preservation.
-
5.
Individual and institutional background
The items included physicians’ gender, age, religious background, length of professional career, and specialty. We also asked for a description of the practicing institution: the number of breast surgeries, the number of young breast cancer patients, presence of female colleagues in the team, the presence of one or more medical oncologist(s), breast cancer certified clinical nurse specialist (CNS), and board-certified pharmacists in the institution.
Procedures
The study was carried out according to the National Guideline for Epidemiological Studies. The names of study participants and the institutions of breast oncologists were obtained from the JBCS website. After confirmation of each physician’s affiliation, anonymous paper surveys were sent out to all 843 breast oncologists by mail with a return postage-paid envelope. The survey was sent out on 28 May 2010 and the mailed surveys postmarked by 31 July were included in the analysis. The consent from the participants was waived because of the anonymity of the survey. No honorarium was offered for completing the survey.
Data analysis
All analyses were conducted using IBM SPSS statistics version 18. Accuracy of knowledge about fertility was scored on the basis of four questions (A-1, 2, 3, 4, Table 1) concerning the standard knowledge about chemotherapy and the effect of chemotherapy on fertility. Respondents with appropriate knowledge were considered “accurate”. Four questions (D-1, 2, 3, 5, Table 1) concerning the perspective and opinion about the fertility preservation were asked and scored as attitude score. Respondents were divided into “positive attitude group” and “negative attitude group” depending on the attitude score. Chi-square test was applied for correlation analysis between physician knowledge, attitude, and background. Physicians’ background demographics, knowledge, and attitude regarding fertility issues were associated with physicians’ practice behavior regarding fertility issues. Odds ratios (OR) and their 95% confidence interval (CI) were estimated to compare physician background factors, knowledge, and attitude with physician practice pattern, using simple and multivariable logistic regression models. All p values are two sided, and the statistical significance level was set at p < 0.05. No adjustments for multiple comparisons were considered because of the exploratory nature of this study.
Results
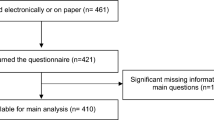
Response rate
The response rate was calculated as the number of breast oncologists completing the survey (n = 434) divided by the initial sample size minus undeliverable (843 − 8 = 835): this yielded a 52% response rate. This is higher than the previous survey on fertility preservation referral targeting oncology specialists in the USA [4].
Demographic and characteristics of responding breast oncologists
The background of respondents is shown in Table 2. A total of 16.6% of the respondents were female. More than 95% of the respondents were experienced physicians reflecting the requirement of basic board certification in general medicine, surgery, radiation oncology, or pathology in order to obtain JBCS Breast Oncologists certification. The majority was surgeons. Less than half responded that they have medical oncologists in their institutions. About 70% were the institutions in which they operated on less than five breast cancer patients per week (less than approximately 200 cases per year).
Association between knowledge, attitude, and physician background
Two hundred and seventy-nine (64%) respondents were considered to have accurate knowledge. Accuracy of knowledge about fertility was correlated with the number of young breast cancer patients treated (p = 0.006), presence of children of the physician (p = 0.01), age of the physician (p = 0.019), and the presence of female colleagues (p = 0.019).
The existence of a spouse/partner (p = 0.011), age (p = 0.032), and gender (p = 0.023) of the physician were the factors significantly correlated with a positive attitude toward fertility considerations of breast cancer patients. Physicians who have a spouse/partner, physicians who are younger than 50 years, and female physicians had more positive attitudes toward fertility issues for breast cancer patients.
Practice of fertility issues among breast oncologists
A total of 83% of the participants responded that they were positive in discussing fertility issues with young breast cancer patients.
Twenty-one percent responded that patients voluntarily bring up fertility issues in the clinic. Physicians who treat two or more young patients per week perceived that patients voluntarily express their concern in the clinic compared to physicians who treat fewer (OR 1.84, 95% CI 1.13–3.00, p = 0.008). Physicians who treat two or more young patients per week (OR 1.30, 95% CI 1.05–2.45, p = 0.023), who have board-certified nurse colleagues (OR 1.55, 1.19–2.03, p < 0.001) and have more than six breast surgeries per week (OR 1.20, 1.02–1.41, p = 0.014) responded that they perceived that patients talk to co-medical staff about their concerns about fertility. A total of 24% of the respondents consulted reproductive specialists when they encountered fertility problems in their patients and 42% referred patients to reproductive specialists when patients expressed concerns regarding fertility.
The association between physicians’ behavior related to fertility issues and their knowledge, attitude, and background demographics are shown in Table 3. Fair knowledge had the strongest impact on physicians’ positive behavior towards discussing fertility issue with patients. Positive attitude, presence of breast cancer-specialized CNS, young age, and female gender were also significant factors associated with positivity towards the discussion. Female oncologists and medical oncologists were more likely to take into account patients’ social backgrounds such as history of childbirth, presence of a spouse/partner, and patients’ economic status when discussing fertility issues.
Physicians with a positive attitude, physicians younger than 50 years, and female physicians were more likely to discuss fertility issues with patients with poorer prognoses. Positive attitude was the strongest factor related to consultation and referral to reproductive specialists.
Barriers for discussion with patients
High risk of disease recurrence (51%), lack of reproductive specialists or infertility clinic for referral (45%), and time constraints in the clinic (45%) were regarded as major barriers for discussing fertility issues. When only physicians who were negative in discussing fertility issues (n = 69) were analyzed, high risk of recurrence (57%), no signal of interest in fertility from patients (49%), and lack of reproductive specialists or infertility clinic for referral (38%) were the major causes for them not to discuss fertility with patients.
Discussion
This study describes the attitude of the main providers of breast cancer treatment in Japan towards fertility issues in young breast cancer patients. The high response rate to our survey in a relatively short time indicates the interest of breast oncologists in fertility issues. More than 80% of the participants responded that they had a positive attitude when discussing fertility issues in the clinic, but this result may be biased by the respondents’ interest in fertility issues. The recent awareness of fertility issues among Japanese breast oncologists may be related to the publication of the ASCO guideline in 2006 and the inclusion of fertility-related contents in JBCS patient guideline 2009 [2, 9]. Indeed, the JBCS treatment guideline, the standard textbook for board certification of Breast Oncologists, updated its contents to cover fertility-related issues in July 2010 [10].
The physicians with a positive attitude and working in institutions with medical oncologists and/or female colleagues had a higher likelihood of consultation or referral to reproductive specialists. The likelihood of referring to reproductive specialists was slightly higher in female physicians, which was consistent with the results of the survey in the USA [4]. These results indicate that participation of female healthcare providers in the team and a multidisciplinary working environment might enhance physicians’ awareness of and behavior toward fertility-related issues. Because knowledge and attitude seem to be influenced by gender, personal experience, and the working environment of the physicians, we think that outreach with educational materials and systematic learning opportunities for healthcare providers would be helpful in expanding knowledge and performance regarding fertility issues in young breast cancer patients.
High risk of disease recurrence was considered the greatest barrier for physicians, similar to the results of other studies [5, 6]. In our previous study, patients’ with higher risk of disease recurrence did not voluntarily express their concerns regarding fertility when compared to patients of lower risk of disease recurrence [3]. Both patients and physicians may refrain from discussing future fertility when the estimation of prognosis of the cancer is poor. Although early referral to reproductive specialists might increase the patients’ likelihood of receiving reproductive intervention and improve the fertility outcome [11, 12], fertility preservation techniques such as embryo preservation and oocyte preservation connote ethical issues especially in patients with poor prognosis [13]. Ethical and psychosocial support is necessary in the shared decision-making process among patients, families, and physicians.
A lack of reproductive specialists or infertility clinic for referral is a real problem. A survey in the USA showed that many breast cancer clinicians reported that they do not have knowledge of or resources for fertility preservation [8, 14]. Interdisciplinary communication between reproductive specialists and oncologists is necessary.
Early case–control studies suggest that pregnancy after primary treatment of breast cancer does not have a negative impact on cancer prognosis, although “healthy mother” bias might exist [15]. Because prognostication of breast cancer has become individualized using genetic biomarkers [16, 17], further investigations to clarify the impact of pregnancy after primary treatment on an individual basis is needed so that patients can personalize their decision-making regarding both cancer treatment and fertility.
In conclusion, Japanese breast oncologists were in general positive in discussing fertility issues with young breast cancer patients. Female and younger physicans as well as physicians working in a multidisciplinary environment had more positive attitudes and behavior towards fertility preservation. The development of multidisciplinary and interdisciplinary programs is necessary to meet the fertility needs of breast cancer patients.
References
Canada AL, Schover LR. The psychosocial impact of interrupted childbearing in long-term female cancer survivors. Psychooncology. 2010 (Epub ahead of print).
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;2429:17–2931.
Kubo A, Koido K, Sawada M, Ryushima Y, Shimizu C, Kato T, Ando M, et al. Survey on oncologists provided information on treatment-related infertility to breast cancer patients. Gan to Kagakuryoho (Cancer Chemother). 2011 (in press).
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Belper G, Lancaster J, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–7.
Arafa MA, Rabah DM. Attitudes and practices of oncologists toward fertility preservation. J Pediatr Hematol Oncol. 2011;33:203–7.
Collins IM, Fay L, Kennedy MJ. Strategies for fertility preservation after chemotherapy: awareness among Irish cancer specialists. Ir Med J. 2011;104:6–9.
Peate M, Meiser B, Friedlander M, Zorbas H, Rovelli S, Sansom-Daly U, et al. It’s now or never: fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer—an Australian Fertility Decision Aide Collaborative Group Study. J Clin Oncol. 2011 (Epub ahead of print).
Quinn GP, Vadaparamil ST, King L, Miree CA, Wilson C, Raj O, et al. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009;77:338–43.
Japanese Breast Cancer Society. Breast cancer treatment guideline for patients 2009. Tokyo: Kanehara Shoten; 2010 (Japanese).
Japanese Breast Cancer Society. Breast cancer treatment guideline 2010. Tokyo: Kanehara Shoten; 2010 (Japanese).
Lee S, Heytens E, Moy F, Ozkavukcu S, Otkay K. Determinants of access to fertility preservation in women with breast cancer. Fertil Steril. 2011;95:1932–6.
Lee S, Ozkavukcu S, Heytens E, Moy F, Otkay K. Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol. 2010;28:4683–6.
Gerber B, Dieterich M, Muller H, Remer T. Controversies in preservation of ovary function and fertility in patients with breast cancer. Breast Cancer Res Treat. 2008;108:1–8.
Goldfarb S, Dickler M, McCabe M, Thom B, Jia X, Hudis C, et al. Oncology clinicians knowledge, attitude and practices regarding fertility preservation. J Clin Oncol. 2010;28(15 Suppl):e19525.
Kranick MA, Schaefer C, Rowell S, Desai M, Petrek JA, Hiatt RA, Senie RT. Is pregnancy after breast cancer safe? Breast J. 2010;16:404–11.
Oakman C, Santarpia L, Di Leo A. Breast cancer assessment tools and optimizing adjuvant therapy. Nat Rev Clin Oncol. 2010;7:725–32.
Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thurlimann B, Senn HJ, Panel Members. Thresholds for therapies: highlights of the St Galln International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol. 2009;20:1319–29.
Acknowledgments
This study was supported by the Ministry of Health, Science and Welfare, Grant-in-Aid for Clinical Research in Cancer (H21-021). There were no financial disclosures from any authors. We thank Professor Richard Theriault of the University of Texas M. D. Anderson Cancer Center for his editorial assistance in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shimizu, C., Bando, H., Kato, T. et al. Physicians’ knowledge, attitude, and behavior regarding fertility issues for young breast cancer patients: a national survey for breast care specialists. Breast Cancer 20, 230–240 (2013). https://doi.org/10.1007/s12282-011-0328-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-011-0328-8