Abstract
Purpose of the Review
Fluconazole prophylaxis (FP) for invasive candidiasis (IC) in preterm newborns is still a debated topic. In this review, we describe the most important papers on the topic, and we discuss pros and cons of the use FP in newborns according to these paper’s findings.
Recent Findings
Since 2001, several studies have been published on the use of FP to prevent IC. While most of them agree on the effectiveness of FP in reducing IC, especially in NICUs with high IC rates, the lack of evidence of decrease in overall mortality, and the risks associated with fluconazole administration both concerning neurodevelopmental impairment and the increase in Candida resistances still pose great concern against the universal implementation of FP.
Summary
A local risk-based selection strategy could represent the best choice to optimize the benefits of FP and minimize the potential long-term toxicity and the development of resistant pathogens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive candidiasis (IC) is a serious infection with significant morbidity and mortality. Central nervous system is involved in around 50% of newborns with IC [1, 2], and up to 60% of survivors may present neurological impairment [3].
The incidence of IC varies according to birth weight and it has been estimated that the risk of IC is threefold higher for infants < 750 g compared to infants with birth weight of 750–1000 g [4]. The immaturity of the immune system of very low birth weight (VLBW) and extremely low birth weight (ELBW) neonates is the most important risk factor [5]; the presence of invasive devices, prior colonization by Candida spp., cross transmission by hands, and use of broad-spectrum antibiotics use, as well as recent abdominal surgery are all considered predisposing conditions [6, 7]. Indeed, the difference in IC incidence between single NICUs reflects the differences in central line policies, infection control, and antimicrobial stewardship programs [7, 8].
Owing to its pharmacokinetic characteristics, fluconazole represents an attractive agent for prophylaxis. It has a good enteral absorption, long half-life, excellent CSF penetration, and it is mostly eliminated unchanged in the urine [9].
Effectiveness of Fluconazole Prophylaxis
There is some evidence supporting fluconazole prophylaxis (FP) as a safe and efficacious strategy to prevent colonization and IC in VLBW and ELBW infants.
The use of fluconazole for prophylaxis was first explored in 2001 by two randomized controlled trials. The first, by Kaufman et al., was a prospective, randomized, double-blind trial of 100 ELBW infants randomly assigned to receive either intravenous fluconazole or placebo for 6 weeks. Although the study had small numbers of neonates included in each arm this trial showed a significant reduction in Candida colonization and a decrease in IC [10]. The second one, conducted by Kicklighter et al., was a single-center randomized control trial investigating if FP administration for the first 28 days of life could result in a reduced incidence of Candida colonization in the VLBW infant. This trial, that involved 103 patients, showed that FP is safe and able to decrease the risk of rectal colonization by Candida species [11].
In 2007 Manzoni et al. conducted a robust multicenter, randomized, double-blind, placebo-controlled trial regarding fluconazole prophylaxis including 322 VLBW infants. Patients were randomly assigned to receive either fluconazole (at a dose of either 6 mg or 3 mg/kg) or placebo, from birth until day 30 (if VLBW) or day 45 of life (if ELBW). In this case, a significant reduction in both colonization and IC in the fluconazole arms was reported.
In addition to this evidence, other retrospective comparative studies with pre- and post-exposure analysis support the use of FP [12]. Healy et al., in 2008 reported a reduction of IC from 0.6% (19/3012) to 0.3% (22/6393) with the use of FP, with a 3.6-fold decrease in ELBW infants in particular. Similarly, Rueda and colleagues in 2010 published a study that described a reduction in the incidence of IC among VLBW neonates, from 7.7% (21/271) in the pre-FP period to 1.1% (3/252) in the post-FP period [13].
On the other hand, some studies question the effectiveness of FP in preventing neonatal IC. A randomized, double-blind placebo-controlled study conducted by Parikh et al. in 2007 [14], reported no difference between the incidence of IC between intervention and placebo groups. Likewise, a retrospective analysis by Lee and colleagues on 423 children, reported no reduction of incidence in IFIs in ELBW infants receiving FP [15].
In 2014 Benjamin et al., conducted a multicenter randomized blinded, placebo-controlled trial of fluconazole in premature infants including 361 infants weighing less than 750 g at birth [16]. The aim of the study was to evaluate the safety and efficacy of fluconazole in preventing IC or death among ELBW infants and to determine the effect of FP on neurodevelopment in surviving infants. They concluded that among infants with a birth weight of less than 750 g, FP compared with placebo was not associated with a statistically significant difference in the incidence of the composite outcome of death or IC. These findings do not support the universal use of prophylactic fluconazole in extremely low birth weight infants [16] (Table 1).
The lack of consistency in these results may be a consequence of differences in baseline incidence of colonization and IC: many studies reporting an effective reduction of IC come from centers with high incidence of IC (15–20%), while it is unclear if FP has a real impact in low incidence settings [24].
Moreover, as underlined by Ericson and Benjamin in their review, all studies regarding FP that used historical controls as comparator group are affected by other factors (e.g., central line policies) that might have changed over time, and it is impossible for these studies to fully determine the effect of fluconazole on the incidence of IC. In fact, a reduction in the incidence of Candida central line-associated bloodstream infections has been reported even in birth weight cohorts that are not considered for FP (e.g., > 1000 or > 1500 g birth weight) [24].
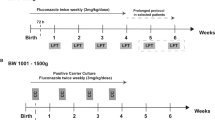
As a consequence, universal FP is not recommended for all neonates. Current recommendations include the use of FP only for infants with a birth weight of less than 1000 g in NICUs with high rates of IC [25, 26]. However, differences in the threshold for starting a FP still persist. Indeed, ESCMID guidelines suggest a cut-off IC rate of 2% [26] differently from the 5% proposed by the IDSA guidelines [25]. Moreover, the lack of evidence of decrease in overall mortality, and the risks associated to fluconazole administration both concerning neurodevelopmental impairments and an increase in Candida resistances still represent important concerns against the use of FP.
Open Issues
Reduction of Mortality
Literature findings reporting a reduction of mortality associated with IC in neonates receiving FP are scarce. A recent review conducted by Ferrera da Silva Rios et al. [27], included 12 original articles on antifungal prophylaxis in premature infants. They identified six studies that assessed IC-related mortality: four comparative studies with pre-prophylaxis period and FP period, [13, 18, 19, 22] and two trials comparing fluconazole to placebo [10, 14]. They found that in only one of these studies [13], there was a significant reduction of IC-associated deaths, with 21% mortality in the pre-prophylaxis group versus no deaths in the post-prophylaxis group.
Similarly, a metanalysis conducted in 2015 by Clerihew et al., including data from four trials comparing FP to placebo did not demonstrate any statistically significant effect on overall mortality rate, even if with a wide confidence interval (95%) [28].
Neurodevelopmental Disorders
Other concerns regarding widespread application of FP are long-term consequences of fluconazole administration and neurodevelopmental impairment. To our knowledge, two studies assessed neurodevelopmental consequences in neonates receiving FP.
The first one is the aforementioned trial conducted by Benjamin et al. [2] that evaluated neurodevelopment at 18–22 months of age in 118 infants who were randomized to use FP or placebo. The authors concluded that the use of fluconazole did not impair the neurodevelopment of these neonates. However, as stated in the study, these results are biased, since many factors affected neurodevelopmental impairment in preterm neonates, and the study was not powered for differences in neurodevelopmental impairment alone.
The second study, by Kaufmann et al. [29•], assessed long-term consequences, considering neurodevelopmental and behavioral impairments at 8–10 years of age. The complete follow-up and assessment was possible only for 20 children who had received fluconazole as infants, and it showed that outcomes of the children who received fluconazole was not different from the ones who did receive placebo. Even if this result is encouraging, the high number of patients lost in follow-up, as well as the possible biases related to the long period of follow-up represent significantly limit the strength of the evidence.
Moreover, while these results show that FP administration does not result in neurodevelopmental impairments, they also show that it provides no advantage compared to placebo either.
Antifungal Resistances
Although it has not been reported in NICUs yet, resistance to fluconazole has appeared in recent years, with some centers reporting ~ 8% of resistance among Candida isolates both in adults and children [30]. Furthermore, it has been demonstrated that the application of non-targeted FP leads to a change in the distribution of the different species of Candida, resulting in a decrease of C. albicans, and an increase of C. krusei, which is inherently resistant to fluconazole, and C. glabrata, that has resistance rates > 50% [31, 32]. Indeed, the aforementioned study by Lee et al. [15], reported an increase in incidence of invasive infections involving fluconazole-resistant C. parapsilosis even though it was not statistically significant (41.7 vs. 0%, P = 0.11).
On the other hand, a single-centered study conducted by Manzoni et al. over a 5-year period, found no increase in fluconazole inherently resistant Candida species after the implementation of routine FP for VLBW infants [33]. Likewise, a study by Healy and colleagues [13], compared resistance patterns of isolates causing IC before and after the implementation of FP, and showed no difference in the epidemiology in the two study periods.
However, both these are single-center studies, and have relatively small number of patients and short duration, and the effect of FP on larger scale and longer period is yet to be evaluated.
In addition to the concerns about current resistances, there is rising attention about the emergence of a new, highly resistant species, Candida auris, that is a new species that was first described in 2009 and has been demonstrated to be multidrug resistant, with fluconazole resistance rates > 90%. Even if the report of C. auris are still occasional, it is interesting to underline that among the 12 first reported cases in India, 3 were neonates, as reported by Chowdhary et al. [34].
One last factor to consider is the cost-effectiveness of FP: according to Swanson et al. [35], if the incidence of IC is below 2.8%, FP loses its cost-effectiveness in NICU. However, as indicated by the authors, many factors affect the incidence of IC in NICUs, and in low incidence centers the cost-benefit may only be seen in selected population (i.e., < 27 weeks gestation or < 750 g). This analysis provides evidence of the need for targeted use of FP in preventing IC.
Targeted Prophylaxis
To optimize the benefits of FP in preterm neonates, some authors proposed a risk-stratification strategy.
In an observational study by Bertini et al. [17], FP was administered only to VLBW infants with a central venous line. A reduction of fungal infection was reported in the fluconazole group in comparison to the baseline group (9/119 vs. 0/136, P = 0.003).
In 2006, Uko et al. conducted an observational study of two subsequent periods of inborn VLBW and ELBW infants, one before and one after targeted-FP implementation. In this study, the main factor for starting a FP in VLBW and ELBW infants was a concomitant broad-spectrum antibiotic therapy for more than 3 days. IFI was observed in 6.3% (13/206) in the control period and 2/178 (1.1%) after targeted-FP implementation, with a common odds ratio of 0.166. Moreover, this intervention was cost-effective and the number needed to treat to prevent 1 IFI was 10 [18]. Differently, McCrossan et al. suggested few conditions which could request a FP in VLBW babies [20]. In their analysis, the additional risk factors were colonization of Candida species from surface sites with a central venous catheter, third-generation cephalosporin treatment, or total duration of antibiotic treatment > 10 days. The results showed that selective FP reduced invasive fungal sepsis without evidence of fluconazole resistance emerging [20].
Martin et al. in 2012 further stratified the high-risk population proposing targeted FP to all VLVW infants who had received broad-spectrum antibiotics for more than 2 days and having at least one additional risk factor for IC. The authors reported a significant decrease in IC from 15.3 to 6.2% during the FP period [36].
Another study, by Weitkamp et al. applied a different targeted approach to FP, including only < 750 g birth weight or < 26 weeks gestational age with a central line in the prophylaxis group. Again, a reduction in IFI was demonstrated, in comparison with historic controls (9/44 vs. 0/42, p = 0.004), with no significant rates of adverse effect recorded. In addition, the targeted approach allowed to reduce the number of infants > 1000 g requiring prophylaxis from 80 to 42 (48% reduction), without missing any preventable infection [21].
One more recent analysis was conducted by Rolnitsky et al., 2012, in Israel. In their retrospective cohort study with historical controls, they categorized many different risk factors into major (birth weight < 1000 g, corrected gestational age < 28 weeks, and use of broad-spectrum antibiotics) and minor (the presence of a central venous line, respiratory support, inotropic support, use of parenteral nutrition, use of a histamine-2 blocker or systemic steroids, confirmed necrotizing enterocolitis, or recent abdominal surgery), and applied FP only to neonates presenting with one major or two minor criteria. With this approach, they reported a significant reduction in the rate of fungal infections in the fluconazole prophylaxis group (1 of 130 vs. 19 of 319, p = 0.016). Furthermore, they calculated that this selective approach reduced the number of infants treated from 247 to 130 [23].
Alternatives to Fluconazole Prophylaxis
Oral nystatin prophylaxis was the first antifungal studied in preventing IC, and many studies report its efficacy [37,38,39]. FP is preferred because of its greater efficacy and cost-benefit, but nystatin prophylaxis has been proven to reduce mortality as well as IC [38].
Furthermore, since many factors impact IC incidence in NICUs, other infection control measures may reduce IC and IC-related mortality. In their study, Chen et al. [40], evaluated the effect of integrated measures (with a particular emphasis on hand hygiene), in reducing IC in a Chinese hospital’s NICU. They found that integrated measures, combined to FP can be much more effective than FP only: the reported incidence of IC in the group to which integrated measures (together with FP) were applied was 2.9% (2/68), while in the group that received only FP it was 18.2% (18/99) and in the control group was 22.3% (22/94).
Conclusion
Currently, many studies suggest efficacy of FP in reducing IC and colonization by Candida species; however, literature findings are not consistent with recommending universal use of FP, and many aspects of this topic need to be further clarified by scientific evidence.
From what we know at this moment, FP should be implemented in NICUs with an IC rate > 5%, while in those with IC rate between 2 and 5% an approach based on additional risk factors seems to the best choice to optimize the benefits of FP and to minimize the potential long-term toxicity and the development of resistance.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Wynn JL, Benjamin DK Jr, Benjamin DK, Cohen-Wolkowiez M, Clark RH, Smith PB. Very late onset infections in the neonatal intensive care unit. Early Hum Dev. 2012;88(4):217–25. https://doi.org/10.1016/j.earlhumdev.2011.08.009.
Benjamin DK Jr, Stoll BJ, Fanaroff AA, McDonald SA, Oh W, Higgins RD, et al. Neonatal candidiasis among extremely low birth weight infants: risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics. 2006;117(1):84–92.
Adams-Chapman I, Bann CM, Das A, Goldberg RN, Stoll BJ, Walsh MC, et al. Neurodevelopmental outcome of extremely low birth weight infants with Candida infection. J Pediatr. 2013;163(4):961–7.e3. https://doi.org/10.1016/j.jpeds.2013.04.034.
Saiman L, Ludington E, Pfaller M, Rangel-Frausto S, Wiblin RT, Dawson J, et al. Risk factors for candidemia in neonatal intensive care unit patients. The National Epidemiology of Mycosis Survey study group. Pediatr Infect Dis J. 2000;19(4):319–24.
Ghazal P, Dickinson P, Smith CL. Early life response to infection. Curr Opin Infect Dis. 2013;26(3):213–8. https://doi.org/10.1097/QCO.0b013e32835fb8bf.
Brady MT. Health care-associated infections in the neonatal intensive care unit. Am J Infect Control. 2005;33(5):268–75.
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK, et al. The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics. 2006;118:717–22.
Donà D, Mozzo E, Mardegan V, Trafojer U, Lago P, Salvadori S, et al. Antibiotics prescriptions in the neonatal intensive care unit: how to overcome everyday challenges. Am J Perinatol. 2017;34(12):1169–77. https://doi.org/10.1055/s-0037-1602426.
Brammer KW, Coates PE. Pharmacokinetics of fluconazole in pediatric patients. Eur J Clin Microbiol Infect Dis. 1994;13(4):325–9.
Kaufman D, Boyle R, Hazen KC, Patrie JT, Robinson M, Donowitz LG. Fluconazole prophylaxis against fungal colonization and infection in preterm infants. N Engl J Med. 2001;345(23):1660–6.
Kicklighter SD, Springer SC, Cox T, Hulsey TC, Turner RB. Fluconazole for prophylaxis against candidal rectal colonization in the very low birth weight infant. Pediatrics. 2001;107:293–8.
Manzoni P, Stolfi I, Pugni L, Decembrino L, Magnani C, Vetrano G, et al. A multicenter, randomized trial of prophylactic fluconazole in preterm neonates. N Engl J Med. 2007;356:2483–95.
Healy CM, Campbell JR, Zaccaria E, Baker CJ. Fluconazole prophylaxis in extremely low birth weight neonates reduces invasive candidiasis mortality rates without emergence of fluconazole-resistant Candida species. Pediatrics. 2008;121:703–10.
Parikh TB, Nanavati RN, Patankar CV, Rao S, Bisure K, Udani RH, et al. Fluconazole prophylaxis against fungal colonization and invasive fungal infection in very low birth weight infants. Indian Pediatr. 2007;44(11):830–7.
Lee J, Kim HS, Shin SH, Choi CW, Kim EK, Choi EH, et al. Efficacy and safety of fluconazole prophylaxis in extremely low birth weight infants: multicenter pre-post cohort study. BMC Pediatr. 2016 May 16;16:67. https://doi.org/10.1186/s12887-016-0605-y.
Benjamin DK Jr, Hudak ML, Duara S, Randolph DA, Bidegain M, Mundakel GT, et al. Effect of fluconazole prophylaxis on candidiasis and mortality in premature infants: a randomized clinical trial. JAMA. 2014;311(17):1742–9. https://doi.org/10.1001/jama.2014.2624.
Bertini G, Perugi S, Dani C, Filippi L, Pratesi S, Rubaltelli FF. Fluconazole prophylaxis prevents invasive fungal infection in high-risk, very low birth weight infants. J Pediatr. 2005;147:162–5.
Uko S, Soghier LM, Vega M, Marsh J, Reinersman GT, Herring L, et al. Targeted short-term fluconazole prophylaxis among very low birth weight and extremely low birth weight infants. Pediatrics. 2006;117(4):1243–52.
Manzoni P, Arisio R, Mostert M, Leonessa M, Farina D, Latino MA, et al. Prophylactic fluconazole is effective in preventing fungal colonization and fungal systemic infections in preterm neonates: a single-center, 6-year, retrospective cohort study. Pediatrics. 2006;117:e22–32.
McCrossan BA, McHenry E, O'Neill F, Ong G, Sweet DG. Selective fluconazole prophylaxis in high-risk babies to reduce invasive fungal infection. Arch Dis Child Fetal Neonatal Ed. 2007;92(6):F454–8.
Weitkamp JH, Ozdas A, LaFleur B, Potts AL. Fluconazole prophylaxis for prevention of invasive fungal infections in targeted highest risk preterm infants limits drug exposure. J Perinatol. 2008;28(6):405–11. https://doi.org/10.1038/sj.jp.7211914.
Rueda K, Moreno MT, Espinosa M, Sáez-Llorens X. Impact of routine fluconazole prophylaxis for premature infants with birth weights of less than 1250 grams in a developing country. Pediatr Infect Dis J. 2010;29(11):1050–2. https://doi.org/10.1097/INF.0b013e3181e9dea2.
Rolnitsky A, Levy I, Sirota L, Shalit I, Klinger G. Targeted fluconazole prophylaxis for high-risk very low birth weight infants. Eur J Pediatr. 2012;171(10):1481–7.
Ericson JE, Benjamin DK Jr. Fluconazole prophylaxis for prevention of invasive candidiasis in infants. Curr Opin Pediatr. 2014;26(2):151–6. https://doi.org/10.1097/MOP.0000000000000060.
Pappas PG, Kauffman CA, Andes D, Benjamin DK J, Calandra TF, Edwards JE Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35.
Hope WW, Castagnola E, Groll AH, Roilides E, Akova M, Arendrup MC, et al. European Society of Clinical Microbiology and Infectious Diseases guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clin Microbiol Infect. 2012;18(Suppl 7):38–52.
Rios JFDS, Camargos PAM, Corrêa LP, Romanelli RMC. Fluconazole prophylaxis in preterm infants: a systematic review. Braz J Infect Dis. 2017;21(3):333–8. https://doi.org/10.1016/j.bjid.2017.01.008.
Clerihew L, Austin N, McGuire W. Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants. Cochrane Database Syst Rev. 2007 (4):CD003850.
• Kaufman DA, Cuff AL, Wamstad JB, et al. Fluconazole prophylaxis in extremely low birth weight infants and neurodevelopmental outcomes and quality of life at 8 to 10 years of age. J Pediatr. 2011;158:759–65. This long-term follow-up study of VLBW infants given fluconazole
Cleveland AA, Farley MM, Harrison LH, Stein B, Hollick R, Lockhart SR, et al. Changes in incidence and antifungal drug resistance in candidemia: results from population-based laboratory surveillance in Atlanta and Baltimore, 2008-2011. Clin Infect Dis. 2012 Nov 15;55(10):1352–61. https://doi.org/10.1093/cid/cis697.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373(15):1445–56. https://doi.org/10.1056/NEJMra1315399.
Pfaller MA, Messer SA, Hollis RJ, Boyken L, Tendolkar S, Kroeger J, et al. Variation in susceptibility of bloodstream isolates of Candida glabrata to fluconazole according to patient age and geographic location in the United States in 2001 to 2007. J Clin Microbiol. 2009;47(10):3185–90. https://doi.org/10.1128/JCM.00946-09.
Manzoni P, Leonessa M, Galletto P, Latino MA, Arisio R, Maule M, et al. Routine use of fluconazole prophylaxis in a neonatal intensive care unit does not select natively fluconazole-resistant Candida subspecies. Pediatr Infect Dis J. 2008;27:731–7.
Chowdhary A, Anil Kumar V, Sharma C, Prakash A, Agarwal K, Babu R, et al. Multidrug-resistant endemic clonal strain of Candida auris in India. Eur J Clin Microbiol Infect Dis. 2014 Jun;33(6):919–26. https://doi.org/10.1007/s10096-013-2027-1.
Swanson JR, Vergales J, Kaufman DA, Sinkin RA. Cost analysis of fluconazole prophylaxis for prevention of neonatal invasive candidiasis. Pediatr Infect Dis J. 2016;35(5):519–23. https://doi.org/10.1097/INF.0000000000001068.
Martin A, Pappas A, Lulic-Botica M, Natarajan G. Impact of ‘targeted’ fluconazole prophylaxis for preterm neonates: efficacy of a highly selective approach? J Perinatol. 2012;32(1):21–6. https://doi.org/10.1038/jp.2011.27.
Ozturk MA, Gunes T, Koklu E, Cetin N, Koc N. Oral nystatin prophylaxis to prevent invasive candidiasis in Neonatal Intensive Care Unit. Mycoses. 2006;49(6):484–92.
Ganesan K, Harigopal S, Neal T, Yoxall CW. Prophylactic oral nystatin for preterm babies under 33 weeks’ gestation decreases fungal colonisation and invasive fungaemia. Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94(4):F275–8. https://doi.org/10.1136/adc.2008.145359.
Howell A, Isaacs D, Halliday R, Australasian Study Group for Neonatal Infections. Oral nystatin prophylaxis and neonatal fungal infections. Arch Dis Child Fetal Neonatal Ed. 2009;94(6):F429–33. https://doi.org/10.1136/adc.2008.157123.
Chen J, Yu X, Zhou Y, Zhang Y, Zhu J, Xie L, et al. Integrated measures for prevention of invasive Candida infections in preterm infants in a Chinese neonatal intensive care unit. Am J Infect Control. 2015;43(12):1321–5. https://doi.org/10.1016/j.ajic.2015.07.011.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of Topical Collection on Pediatric Fungal Infections
Rights and permissions
About this article
Cite this article
Donà, D., Luise, D., Baraldi, E. et al. Prevention of Invasive Candidiasis in Premature Neonates: Administering Fluconazole or Not?. Curr Fungal Infect Rep 12, 86–91 (2018). https://doi.org/10.1007/s12281-018-0312-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-018-0312-2