Abstract
We aimed to evaluate the correlation among serum parathyroid hormone (PTH) and slow-reflow during primary percutaneous coronary intervention (PCI) and prognosis in patients with ST-segment elevation myocardial infarction (STEMI). A total of 262 patients were enrolled and divided into a slow-reflow group (n = 61) and a control group (n = 201). PTH was an independent risk factor for slow-reflow (P < 0.05), and the regression model had good discrimination and calibration. ROC curve analysis showed that PTH (≥ 63.65 pg/ml) had a predictive value for slow-reflow (P < 0.001). During the 1-year follow-up, the patients were divided into a PTH-h group (≥ 63.65 pg/ml, n = 100) and a PTH-l group (< 63.65 pg/ml, n = 162). Readmission for HF was independently associated with PTH levels (P < 0.05). KM survival analysis suggested that PTH-h had a predictive value for MACEs, especially for readmission for HF (P < 0.05). PTH levels were associated with slow-reflow during PCI and MACEs during follow-up in patients with STEMI.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction (aMI) is a life-threatening disease with a high mortality rate, and primary percutaneous coronary intervention (PCI) is an effective procedure for saving patients’ lives. However, slow-reflow often occurs during the operation, which greatly affects therapeutic effect and even prognosis [1]. The location of myocardial infarction (MI), such as anterior MI, infarction duration, diabetes mellitus (DM), and age are common risk factors for no-reflow and poor prognosis [2, 3]; however, these indicators often lack specificity, and some of them are not quantified. Thus, the identification of novel biomarkers that quantitatively predict adverse events is of great clinical significance. Recently, serum parathyroid hormone (PTH) has become a hot topic in cardiovascular research [4]. Studies have shown that PTH can alter the intracellular and extracellular ionic calcium (Ca2+) gradient and promote Ca2+ influx, thereby enhancing myocardial contractility. Simultaneously, PTH can directly dilate the coronary arteries, increase blood flow, and alter the autorhythmicity of cardiomyocytes, thereby directly affecting cardiac function [5, 6]. However, under pathological conditions, an elevated PTH level not only leads to calcium overload and abnormal autorhythmicity of myocardial cells, inducing malignant arrhythmias [7, 8], it also leads to decreased coronary blood flow reserves and directly affects coronary microcirculation [9]. Serum PTH levels can also independently predict non-ischemic heart failure (HF) and overall HF, determine the timing of hospitalization and discharge, and can be used for risk stratification, individualized treatment, and prognostication of patients with HF [10,11,12,13]. However, whether PTH can predict perioperative slow-reflow and long-term prognosis in patients with acute ST-segment elevation myocardial infarction (STEMI) after primary PCI has not been reported clinically.
Therefore, the present study aimed to investigate the association between serum PTH levels and perioperative slow-reflow, as well as long-term prognosis in patients with STEMI treated with primary PCI.
Methods
Patients
The clinical data of 300 consecutive patients with STEMI treated with primary PCI between January 2016 and December 2020 were collected and retrospectively analyzed, and STEMI was diagnosed based on typical characteristics, including ischemic chest pain, ECG changes, and increased troponin I levels, according to the European Society of Cardiology guidelines for the diagnosis and treatment of acute STEMI [14]. Patients with intraoperative dissection, perforation, or other complications were excluded. Patients with a known medical history of thyroid diseases, primary hyperparathyroidism, chronic kidney disease, cancer, skeletal system diseases, and chronic malnutrition diseases were also excluded. Ultimately, 262 patients were included in this study.
Based on the occurrence of slow-reflow during primary PCI, the patients were divided into two groups: slow-reflow group (n = 61) and control group (n = 201) for the study. A telephone or clinical follow-up was conducted on 262 patients, and all patients were divided into the PTH-h group (n = 100) and the PTH-l group (n = 162) based on the optimal PTH cutoff value for predicting slow-reflow. The major adverse cardiovascular events (MACEs) during the 1-year follow-up included cardiac death (n = 4), in-stent restenosis (ISR, n = 11), readmission for HF (n = 17), and recurrent MI or unstable angina pectoris (n = 23), except for patients with multi-branch lesions who were readmitted to elective PCI as planned after discharge.
Research Methods
Patient data regarding age, sex, height, weight, hypertension, DM, hyperlipidaemia, cigarette smoking status, and alcohol consumption were collected at admission. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in the catheterization laboratory before coronary angiography. Upon arrival at the emergency department, venous blood from patients with STEMI was collected immediately for testing of the levels of blood cell count, serum creatinine (Scr), electrolytes, admission blood glucose (ABG), C-reactive protein (CRP), troponin I, and PTH. Troponin I was assessed using a quantitative immunofluorescence method (troponin assay kit, Getein Biotechnology Co., Ltd.), and serum PTH levels were measured using chemiluminescence method. Access intact PTH assay is a paramagnetic microparticle chemiluminescent immunoassay that applies the access immunoassay system to quantitatively determine the levels of intact PTH in human serum and plasma. Blood sample collection and processing methods are as follows: 5–10 ml of elbow vein blood was collected when the patient was admitted to the emergency department; as for the yellow-headed tube (the serum tube containing coagulant and separating gel), it was sent to the blood biochemical laboratory of our hospital. After centrifugation for 5 min at 3000 rpm/min at 4 °C in a centrifuge (Baiyang Medical, Beijing Baiyang medical device Co., Ltd.), the test tube was stratified into serum, separating gel and blood clot from top to bottom. Determination of serum PTH is as follows: the blood biochemical laboratory of our hospital is equipped with a full-automatic chemiluminescence immunoanalyzer UniCel DxI (Beckman Coulter, Inc., brea, CA 92821, USA). After the intact PTH assay kit (Beckman Coulter, Inc., brea, CA 92821, USA) and the above samples to be tested were put on the machine, the serum PTH levels were determined. Depending on the patient’s wishes, N-terminal pro b-type natriuretic peptide (NT-proBNP) might have been assessed at the same time (NT-proBNP assay kit, Getein Biotechnology Co, Ltd.). In addition, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), lipoprotein(a), apolipoprotein A1, and apolipoprotein B were measured on fasting on the first day of admission using an automatic biochemical analyzer (Olympus, Japan). The estimated glomerular filtration rate (eGFR) was calculated using the following formula: eGFR (ml/min/1.73 m2) = (140 – age) × weight/0.818 × creatinine concentration (µmol/l), and the value for women was scaled to 0.85. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Primary PCI was performed according to the standard PCI method by two or more interventionalists familiar with the patient’s condition. The choice of thrombus aspiration and platelet glycoprotein IIb/IIIa receptor antagonist was determined by the operator according to the degree of thrombus loading. The diameter of the stent was selected according to the normal segment diameter of the culprit vessels (1–1.1:1). Nitroglycerin or sodium nitroprusside (100–200 µg) was routinely injected into the coronary artery after balloon dilation. The blood flow evaluation of infarct-related artery after stent implantation was performed according to the thrombolysis in myocardial infarction (TIMI) flow grade by two PCI experts [15]. TIMI grade 0 meaned no flow beyond the obstruction; grade 1 referred to incomplete arterial visualization beyond obstruction, grade 2 referred to complete but delayed (more than 3 cardiac cycles) arterial opacification, and grade 3 meaned complete and prompt arterial opacification [16]. In the present study, TIMI grades 0–2 were classified as the slow-reflow group, and TIMI grade 3 was classified as the normal flow group. The following information was recorded: time of onset-to-balloon, coronary angiography-related parameters such as the number of diseased vessels, site of MI (left main stem, left anterior descending, left circumflex branch, right coronary artery), stent length and internal diameter, post-dilation frequency, and coronary blood flow in the infarct-related artery after primary PCI. In patients with no contraindications, aspirin (300 mg, followed by 100 mg per day), ticagrelor (180 mg, followed by 90 mg twice a day), β-blockers, statins, and renin-angiotensin system inhibitors (RASi) were administered. All patients were followed up in the clinic or by telephone after discharge.
Calibration Procedures and Blinding
Quality control of biochemical analyzer, chemiluminescence analyzer, and immunofluorescence detector was performed every day to ensure that the results were in control, and then the samples could be tested. Calibration was performed after out-of-control, batch number change, and/or instrument maintenance to ensure that the results were in control, and then the samples could be tested. Regularly participated in municipal, provincial, and national Clinical Laboratory Center external quality assessment, and the results were all qualified. The detection of imaging equipment referred to the Verification Regulation of Medical Diagnostic X-ray Radiation Source for Medical Digital Subtraction Angiography (JJG 1067–2011), and the equipment stability detection cycle was once every month.
In present study, the TIMI blood flow evaluators were unaware of the patient’s clinical information; the data of patients during hospitalization was obtained by a designated data collector, and MACEs during follow-up were obtained by the other dedicated data collector by reviewing hospital databases and outpatient follow-up records and/or by contacting patients or their families via telephone. None of the above personnel was involved in the final statistical analysis.
Statistical Analysis
Continuous variables were expressed as means and standard deviations or medians and quartiles, and differences between groups were compared using analysis of variance and the least significant difference test. Categorical variables were expressed as frequencies and percentages, and differences between groups were compared using the chi-square test. Logistic regression models were used to analyze whether PTH levels were related to the occurrence of slow-reflow during primary PCI. Receiver operating characteristic (ROC) curves were used to evaluate the predictive value of PTH for slow-reflow, and the best PTH cutoff point was determined by selecting the sum of maximum sensitivity and specificity. Multivariate logistic regression analysis and 1000 repeated bootstrap validations were performed to explore the correlation between PTH levels and adverse cardiovascular events during follow-up. To further explore the role of slow-reflow in the correlation between PTH levels and adverse cardiovascular events during follow-up, mediating effect analysis was performed. Kaplan–Meier survival curves were used to evaluate the prognostic value of PTH. The level of statistical significance was set at P < 0.05. All statistical analyses were performed using SPSS software (version 20.0; Chicago, IL, USA).
Results
Patient Characteristics
Three hundred cases of acute STEMI were initially collected, of which four did not undergo coronary angiography due to advanced malignancy; six did not receive PCI treatment due to diffuse coronary artery disease, of which four died during hospitalization; two converted to coronary artery bypass grafting surgery, and one died due to pericardial effusion during PCI. Twenty-two patients had chronic diseases listed in the exclusion criteria, and five refused to sign informed consent. A total of 262 patients (222 males and 40 females, mean age 58.2 ± 13.5 years) were included. A flowchart of the enrollment process is shown in Fig. 1. All patients received dual antiplatelet therapy, statins, RASi, and β-receptor antagonists, except for three patients who did not receive RASi treatment due to intolerance to blood pressure. The median follow-up period was 709 days.
Serum PTH and Slow-Reflow During the Operation
General Data Pairwise Comparison
According to whether slow-reflow occurred during the operation, the patients were divided into two groups, which were named the slow-reflow group (n = 61) and the control group (n = 201). The patients in the slow-reflow group were older, had more smokers and diabetics, and had significantly higher ABG, PTH, eGFR, and other indicators than those in the control group (P < 0.05). There were no significant differences between the two groups in terms of gender ratio, diameter of lesion vessels, number of lesion vessels, BMI, SBP, DBP, hemoglobin, platelet, Scr, calcium, magnesium, phosphorus, CRP, cTnI, NT-proBNP, time from onset to recanalization, medication, thrombus aspiration, stent parameters, and postoperative dilatation frequency (P > 0.05), as shown in Table 1.
Logistic Regression Analysis
According to the general data comparison results, we used P < 0.1 as the criterion and included significant parameters in the univariate logistic regression analysis of general data comparison (gender, diabetes, smoking, age, reperfusion time, number of lesion vessels, PTH, NT-proBNP, eGFR, ABG). The results showed that age, ABG, smoking, admission PTH, eGFR, and diabetes were risk factors for slow-reflow during primary PCI (P < 0.05). Using P < 0.1 as the criterion, we tested for collinearity among the significant parameters in the univariate logistic regression analysis and found that there was no multicollinearity between variables (tolerance much greater than 0.1, variance inflation factor less than 10). Subsequently, we performed multivariate logistic regression analysis, and the results showed that age (OR = 1.031; 95% CI, 1.007–1.057), PTH (OR = 1.022; 95% CI, 1.012–1.032), and ABG (OR = 1.14; 95% CI, 1.014–1.282) were independent related factors for slow-reflow during primary PCI (P < 0.05), as shown in Table 2.
Model Discrimination Test
Prediction model ROC curve (the area under the curve (AUC) = 0.775; 95% CI, 0.71–0.841, P < 0.01): AUC > 0.75 indicates that the predictive model has good discriminative ability.
Model Calibration Test
The Hosmer and Lemeshow test was used to assess the calibration ability of the prediction model, and the results showed that Hosmer–Lemeshow Χ2 = 11.949, P = 0.154 (> 0.05), indicating that there was no significant difference between the predicted values of the model and the actual observed values, and the predictive model has good calibration ability (Fig. 2A and B).
Discrimination ROC graph and calibration graph of multivariate logistic regression analysis of slow-reflow. A Model discrimination ROC graph; B model calibration graph: sort the predicted probabilities of each research object from small to large and divide them into ten groups according to decile. The actual observation value and model predicted value of each group are expressed in the form of coordinate points, and the model calibration ability is judged as a whole. The closer the predicted curve is to the actual observation curve, the better the calibration capability of the model is
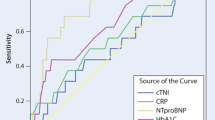
ROC Curve Analysis
The ROC curves revealed that PTH level of ≥ 63.65 pg/ml is optimal for the prediction of slow-reflow during primary PCI, with sensitivity of 78.7%, specificity of 74.1%, and AUC of 0.764 (95% CI, 0.695–0.833; P < 0.001) (Fig. 3).
PTH and Prognosis During follow-up
According to serum PTH levels on admission, all patients were divided into two groups: PTH-l group (PTH < 63.65 pg/ml, n = 162) and PTH-h group (PTH ≥ 63.65 pg/ml, n = 100). The number of patients with hypertension and hyperlipidemia in the PTH-h group was higher than that in the PTH-l group (P < 0.05). In terms of discharge medication, the usage rate of furosemide and spironolactone in the PTH-h group was higher than that in the PTH-l group, and the PTH-h group had significantly higher age, Scr, HDL, CRP, and other indicators than the PTH-l group, and the difference was statistically significant (Table 3).
Multivariate Logistic Regression Analysis and 1000 Repeated Bootstrap Validations
Using adverse cardiovascular events (cardiogenic death, ISR, and readmission for HF, recurrent MI or UA) during follow-up as covariates and PTH-h as the dependent variable, logistic regression analysis was performed to explore the correlation between PTH levels and different outcome events. Since there was high multicollinearity between MACEs and the individual covariates mentioned above, MACEs were not included as covariates. The multivariate logistic regression analysis showed that readmission for HF during follow-up (OR = 6.173; 95% CI, 1.878–20.29, P < 0.001) was independently associated with elevated PTH levels (Table 4). We subsequently adjusted for patients’ baseline characteristics, discharge medication status, and statistically significant parameters (P < 0.05) between the PTH-h and PTH-l groups, and the results all showed that readmission for HF during follow-up was independently correlated with elevated PTH levels (all P < 0.05, Table 4). We then performed 1000 repeated bootstrap validations for all four models, and the results also showed that readmission for HF during follow-up was independently correlated with elevated PTH levels (Table 5).
Mediating Effect Analysis
To further explore the role of slow-reflow in the correlation between PTH levels on admission and readmission for HF during follow-up, mediating effect analysis was performed. The results showed that slow-reflow was an important mediator of PTH levels and readmission for HF during follow-up, and the proportion mediated was approximately 35.362%, which indicating that serum PTH levels might impact readmission for HF during follow-up partially by influencing slow-reflow. More importantly, there was a direct association between elevated PTH levels on admission and readmission for heart failure during follow-up (Table 6).
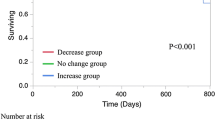
Kaplan–Meier Survival Analysis
Subsequently, Kaplan–Meier survival analysis was used to evaluate the predictive value of PTH-h for MACEs. The results showed that there were significant differences in the risk of occurrence of MACEs and readmission for HF during follow-up between the PTH-h and PTH-l groups (both log rank test P < 0.05, Fig. 4A and B).
Discussion
In patients with STEMI treated with primary PCI, PTH was strongly associated with perioperative slow-reflow. In particular, PTH levels were closely correlated with readmission for HF during long-term follow-up. Even after adjusting for cardiovascular risk factors and other possible confounders, the results remained significant.
Our findings are in line with those of other studies, which found associations between PTH levels and adverse prognosis of acute coronary syndrome [17,18,19]. However, the present study focused on the association of PTH with slow-reflow in this particular cohort receiving primary PCI for STEMI, and followed up for a median time of 709 days to investigate the association of PTH with MACEs. These have not been reported in relevant literatures.
The most common cause of slow-reflow during PCI of aMI is coronary microcirculation disorder, including thrombosis embolism, plaque detachment, and vasospasm, which can cause microcirculation disturbances and then induce slow-reflow [20]. Recently, PTH has also been shown to play a paradoxical and interesting role in cardiovascular diseases. On the one hand, PTH dilates blood vessels via the blocking of L-type calcium channels in smooth muscle cells [21], promotes nitric oxide (NO) production in endothelial cells, and enhances coronary blood flow volume [22]. On the other hand, MI induces elevated serum PTH levels, and elevated PTH can activate adenylate cyclase, promote the translocation of protein kinase C from cytochylema to cytoplasmic membranes, increase intracellular free calcium, cause intracellular calcium overload, activate oxidative stress, and lead to impaired NO synthesis in endothelial cells, thus inducing coronary microcirculation disorders and reducing coronary blood flow reserve [7]. At the same time, PTH and PTH1R interact in the blood, which enhances platelet activity and induces thrombotic events and slow-reflow [23]. In the present study, the higher the PTH level, the higher the incidence of slow-reflow, which is mutually supported and verified with the above findings. Other clinical factors, such as age, diabetes, onset to balloon expansion time, stent length, stent under-expansion, and distal vascular dissection after stent implantation, are also involved in the development of slow-reflow [24, 25]. In our study, patients with slow-reflow were older and had higher blood glucose levels, which is consistent with previous reports [24]. However, in contrast to previous studies [2, 26], onset-to-balloon time, total length of implanted stents, and frequency of post-dilation were not risk factors for slow-reflow in present study. This may be related to factors, such as optimized pre- and in-hospital treatment protocols and the relative simplicity and small number of enrolled cases. TIMI thrombus grade greater than or equal to four was classified as high thrombus load, which was an independent predictor of no-reflow after primary PCI [27]. The subjects of the present study were patients with STEMI, and almost all of whom had completely occlusive blood vessels, i.e., thrombus score of five, so the correlation between thrombus load and slow-reflow was not further analyzed.
Serum PTH is also involved in the pathogenesis of atherosclerosis [28], with elevated PTH levels being positively associated with coronary heart disease events, cardiovascular mortality, and all-cause mortality [29]. In addition to adverse effects on blood pressure, myocardium, coronary blood flow, and arrhythmias, abnormalities of coagulation and fibrinolysis in patients with high PTH levels may also be important risk factors for cardiovascular death events [30]. Heart failure is the most common chronic complication of aMI, and one study demonstrated that PTH had a predictive value in predicting acute HF in STEMI patients within 6 months [18]. The present study, at a longer follow-up, also suggested that PTH was an independent risk factor for readmission due to HF and overall MACEs in patients with STEMI, but not for cardiogenic death, readmission due to recurrent myocardial ischemia or ISR. Interestingly, several studies disagree with the prognostic value of PTH in cardiovascular disease. A prospective study by Folsom et al. conducted a median follow-up of 19 years for 19,392 cases [31]. Their results indicated that PTH levels were not associated with coronary heart disease, stroke, peripheral vascular disease, or atrial fibrillation, but showed weak protective effects on HF and cardiovascular death. They concluded that PTH level was not an independent risk factor for cardiovascular disease. The contrasting clinical conclusion from this study may be related to different PTH detection sequences, long follow-up periods, one-time PTH detection, and cardiovascular event registration, partially or completely dependent on the International Classification of Diseases coding.
No-reflow was an independent predictor of poor outcome in STEMI patients treated by primary PCI and was independent of infarct size [32]. In present study, among the two groups of patients classified based on the optimal PTH cutoff value for predicting slow-reflow, the prognosis of patients in the PTH-h group was worse than that in the PTH-l group. Further, the results of mediating effect analysis also suggested that slow-reflow was an important mediating factor between PTH and readmission for HF during follow-up, and the conclusion of this study is consistent with previous studies. Similarly, mediation analysis also reconfirmed that PTH levels on admission had a direct effect on readmission for HF during follow-up.
Limitations
The present study has several limitations. First, lacking core laboratory support, it utilizes the relatively simple TIMI blood flow grading method to assess blood flow status. Application of the TIMI myocardial perfusion grade or corrected TIMI frame count may improve the accuracy and reproducibility of blood flow assessments. Second, the indicators used in this study were relatively simple. We did not routinely measure NT-proBNP levels because BNP analysis is costly and not covered by medical insurance. However, we believe that our results may be more convincing when using BNP as a control. Third, our sample size was relatively small, and the propensity score matching method was not implemented; therefore, our conclusions may not be generalizable, and most future studies, and even some prospective cohort studies, need to explore the optimal detection point for PTH and how PTH can be regulated to improve the prognosis of patients with STEMI.
Conclusion
PTH levels are associated with slow-reflow during primary PCI and are also closely related to MACEs during 1-year follow-up in patients with STEMI, especially readmission for HF.
Data Availability
For data from this study, please contact the corresponding author.
Abbreviations
- HF:
-
Heart failure
- ISR:
-
In-stent restenosis
- MACEs:
-
Major adverse cardiovascular events
- PCI:
-
Percutaneous coronary intervention
- PTH:
-
Parathyroid hormone
- RASi:
-
Renin-angiotensin system inhibitors
- STEMI:
-
ST-segment elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
- UA:
-
Unstable angina pectoris
References
Gao G, Xu H, Zhang D, Song C, Guan C, Xu B, et al. The predictive value of baseline target lesion SYNTAX score for no-reflow during urgent percutaneous coronary intervention in acute myocardial infarction. J Interv Cardiol. 2021;2021:9987265. https://doi.org/10.1155/2021/9987265.
Tasar O, Karabay AK, Oduncu V, Kirma C. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2019;30(4):270–6. https://doi.org/10.1097/MCA.0000000000000726.
Niu X, Zhang J, Bai M, Peng Y, Sun S, Zhang Z. Effect of intracoronary agents on the no-reflow phenomenon during primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: a network meta-analysis. BMC Cardiovasc Disord. 2018;18(1):3. https://doi.org/10.1186/s12872-017-0722-z.
Isaksson E, Almquist M, Seeberger A, Sterner G. Is low pre-transplant parathyroid hormone a risk marker for cardiovascular disease in long-term follow-up of renal transplant recipients? Clin Exp Nephrol. 2018;22(5):1188–97. https://doi.org/10.1007/s10157-018-1543-9.
Radhakrishnan A, Pickup LC, Price AM, Law JP, Edwards NC, Steeds RP, et al. Coronary microvascular dysfunction: a key step in the development of uraemic cardiomyopathy? Heart. 2019;105(17):1302–9. https://doi.org/10.1136/heartjnl-2019-315138.
Wu GY, Wu T, Xu BD, Shi YC, Cheng ZY, Zhang X, et al. Effect of parathyroid hormone on cardiac function in rats with cardiomyopathy. Exp Ther Med. 2018;16(4):2859–66. https://doi.org/10.3892/etm.2018.6528.
Lombardi G, Ziemann E, Banfi G, Corbetta S. Physical activity-dependent regulation of parathyroid hormone and calcium-phosphorous metabolism. Int J Mol Sci. 2020;21(15):5388. https://doi.org/10.3390/ijms21155388.
Gerbino A, Colella M. The different facets of extracellular calcium sensors: old and new concepts in calcium-sensing receptor signalling and pharmacology. Int J Mol Sci. 2018;19(4):999. https://doi.org/10.3390/ijms19040999.
Osto E, Fallo F, Pelizzo MR, Maddalozzo A, Sorgato N, Corbetti F, et al. Coronary microvascular dysfunction induced by primary hyperparathyroidism is restored after parathyroidectomy. Circulation. 2012;126(9):1031–9. https://doi.org/10.1161/CIRCULATIONAHA.111.081307.
Kolaszko A, Nowalany-Kozielska E, Ceranowicz P, Morawiec B, Kubiak G. The role of parathyroid hormone and vitamin D serum concentrations in patients with cardiovascular diseases. Dis Markers. 2018;2018:5287573. https://doi.org/10.1155/2018/5287573.
Meems LM, Brouwers FP, Joosten MM, LambersHeerspink HJ, de Zeeuw D, Bakker SJ, et al. Plasma calcidiol, calcitriol, and parathyroid hormone and risk of new onset heart failure in a population-based cohort study. ESC Heart Fail. 2016;3(3):189–97. https://doi.org/10.1002/ehf2.12089.
Wu G, Wang X, Wang X, Jiang H, Wang L, Wang T, et al. Serum parathyroid hormone levels predict discharge and readmission for heart failure. Genet Test Mol Biomarkers. 2016;20(6):328–34. https://doi.org/10.1089/gtmb.2015.0285.
Asada S, Yokoyama K, Miyakoshi C, Fukuma S, Endo Y, Wada M, et al. Relationship between serum calcium or phosphate levels and mortality stratified by parathyroid hormone level: an analysis from the MBD-5D study. Clin Exp Nephrol. 2020;24(7):630–7. https://doi.org/10.1007/s10157-020-01879-8.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. https://doi.org/10.1093/eurheartj/ehx393.
Carrick D, Haig C, Ahmed N, Carberry J, Yue May VT, McEntegart M, et al. Comparative prognostic utility of indexes of microvascular function alone or in combination in patients with an acute ST-segment-elevation myocardial infarction. Circulation. 2016;134(23):1833–47. https://doi.org/10.1161/CIRCULATIONAHA.116.022603.
Schwartz BG, Kloner RA. Coronary no reflow. J Mol Cell Cardiol. 2012;52(4):873–82. https://doi.org/10.1016/j.yjmcc.2011.06.009.
Alsancak Y, Kızıltunç E, Sezenöz B, Özkan S, DemirAlsancak A, Gül M, et al. Association between parathyroid hormone levels and the extensiveness of coronary artery disease. Anatol J Cardiol. 2016;16(11):839–43. https://doi.org/10.14744/AnatolJCardiol.2016.6799.
Zarei B, Mousavi M, Mehdizadeh S, Mehrad-Majd H, Zarif M, Erfanian Z, et al. Early effects of atorvastatin on vitamin D and parathyroid hormone serum levels following acute myocardial infarction. J Res Pharm Pract. 2019;8(1):7–12. https://doi.org/10.4103/jrpp.JRPP_18_55.
Baktır AO, Doğan Y, Şarlı B, Şahin Ö, Demirci E, Akpek M, et al. Relationship between serum 25-hydroxyvitamin D levels and the SYNTAX score in patients with acute coronary syndrome. Anatol J Cardiol. 2017;17(4):293–7. https://doi.org/10.14744/AnatolJCardiol.2016.6977.
Konijnenberg LSF, Damman P, Duncker DJ, Kloner RA, Nijveldt R, van Geuns RM, et al. Pathophysiology and diagnosis of coronary microvascular dysfunction in ST-elevation myocardial infarction. Cardiovasc Res. 2020;116(4):787–805. https://doi.org/10.1093/cvr/cvz301.
Zheng MH, Li FX, Xu F, Lin X, Wang Y, Xu QS, et al. The interplay between the renin-angiotensin-aldosterone system and parathyroid hormone. Front Endocrinol (Lausanne). 2020;11:539. https://doi.org/10.3389/fendo.2020.00539.
Zarei B, Mousavi M, Mehdizadeh S, Mehrad-Majd H, Zarif M, Erfanian Z, Moradi A. Early effects of atorvastatin on vitamin D and parathyroid hormone serum levels following acute myocardial infarction. J Res Pharm Pract. 2019;8(1):7–12. https://doi.org/10.4103/jrpp.JRPP_18_55.
Dahlen B, Müller F, Tröbs SO, Heidorn MW, Schulz A, Arnold N, et al. Sex-specific relationship between parathyroid hormone and platelet indices in phenotypes of heart failure-results from the MyoVasc study. Front Cardiovasc Med. 2021;8:682521. https://doi.org/10.3389/fcvm.2021.682521.
Mirbolouk F, Gholipour M, Salari A, Shakiba M, Kheyrkhah J, Nikseresht V, et al. CHA2DS2-VASc score predict no-reflow phenomenon in primary percutaneous coronary intervention in primary percutaneous coronary intervention. J Cardiovasc Thorac Res. 2018;10(1):46–52. https://doi.org/10.15171/jcvtr.2018.08.
Tsukui T, Sakakura K, Taniguchi Y, Yamamoto K, Seguchi M, Jinnouchi H, et al. Factors associated with poor clinical outcomes of ST-elevation myocardial infarction in patients with door-to-balloon time <90 minutes. Plos One. 2020;15(10):e0241251. https://doi.org/10.1371/journal.pone.0241251.
Pries AR, Habazettl H, Ambrosio G, Hansen PR, Kaski JC, Schächinger V, et al. A review of methods for assessment of coronary microvascular disease in both clinical and experimental settings. Cardiovasc Res. 2008;80(2):165–74. https://doi.org/10.1093/cvr/cvn136.
Özbiçer S, Yüksel G, Urgun ÖD, Neşelioğlu S, Erel Ö. Thiols and disulfide levels are correlated with TIMI thrombus grade in non-ST elevation myocardial infarction patients. Biomark Med. 2022;16(4):233–40. https://doi.org/10.2217/bmm-2021-0659.
Seiler-Mussler S, Limbach AS, Emrich IE, Pickering JW, Roth HJ, Fliser D, et al. Association of nonoxidized parathyroid hormone with cardiovascular and kidney disease outcomes in chronic kidney disease. Clin J Am Soc Nephrol. 2018;13(4):569–76. https://doi.org/10.2215/CJN.06620617.
Pilz S, Tomaschitz A, Drechsler C, Ritz E, Boehm BO, Grammer TB, et al. Parathyroid hormone level is associated with mortality and cardiovascular events in patients undergoing coronary angiography. Eur Heart J. 2010;31(13):1591–8. https://doi.org/10.1093/eurheartj/ehq109.
Elbers LPB, Wijnberge M, Meijers JCM, Poland DCW, Brandjes DPM, Fliers E, et al. Coagulation and fibrinolysis in hyperparathyroidism secondary to vitamin D deficiency. Endocr Connect. 2018;7(2):325–33. https://doi.org/10.1530/EC-17-0249.
Folsom AR, Alonso A, Misialek JR, Michos ED, Selvin E, Eckfeldt JH, et al. Parathyroid hormone concentration and risk of cardiovascular diseases: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2014;168(3):296–302. https://doi.org/10.1016/j.ahj.2014.04.017.
Ndrepepa G, Tiroch K, Fusaro M, Keta D, Seyfarth M, Byrne RA, Pache J, Alger P, Mehilli J, Schömig A, Kastrati A. 5-year prognostic value of no-reflow phenomenon after percutaneous coronary intervention in patients with acute myocardial infarction. J Am Coll Cardiol. 2010;55(21):2383–9. https://doi.org/10.1016/j.jacc.2009.12.054.
Funding
This study was funded by the Innovation and Application Project of Medical and Public Health Technology of Wuxi Science and Technology Bureau (grant number N20202035).
Author information
Authors and Affiliations
Contributions
GW and GZ contributed to conception and design of the study. GW and ZW drafted the manuscript. ZW, BX, and SC performed the statistical analysis. GW, ZW, BX, WS, YL, and TW organized the database, implemented the study, and interpreted the data. GW, BX, and GZ critically revised the article. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics Approval
The Medical Ethics Committee of the 904th Hospital of the PLA Joint Logistics Support Force approved this clinical study under protocol No. 20160102. Each patient signed a written consent form, so that their information could be stored in the hospital’s database and used in the analysis.
Conflict of Interest
The authors declare no competing interests.
Additional information
Associate Editor Rupak Mukherjee oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, G., Wu, Z., Xu, B. et al. Slow-Reflow and Prognosis in Patients with High Parathyroid Hormone Levels Undergoing Primary Percutaneous Coronary Intervention for Acute ST-Segment Elevation Myocardial Infarction. J. of Cardiovasc. Trans. Res. 17, 657–668 (2024). https://doi.org/10.1007/s12265-023-10457-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-023-10457-8